Abstract
Aims
The coronavirus disease (COVID)-19 pandemic forced an unprecedented period of challenge to the NHS in the UK where hip fractures in the elderly population are a major public health concern. There are approximately 76,000 hip fractures in the UK each year which make up a substantial proportion of the trauma workload of an average orthopaedic unit. This study aims to assess the impact of the COVID-19 pandemic on hip fracture care service and the emerging lessons to withstand any future outbreaks.
Methods
Data were collected retrospectively on 157 hip fractures admitted from March to May 2019 and 2020. The 2020 group was further subdivided into COVID-positive and COVID-negative. Data including the four-hour target, timing to imaging, hours to operation, anaesthetic and operative details, intraoperative complications, postoperative reviews, COVID status, Key Performance Indicators (KPIs), length of stay, postoperative complications, and the 30-day mortality were compiled from computer records and our local National Hip Fracture Database (NHFD) export data.
Results
Hip fractures and inpatient falls significantly increased by 61.7% and 7.2% respectively in the 2020 group. A significant difference was found among the three groups regarding anaesthetic preparation time, anaesthetic time, and recovery time. The mortality rate in the 2020 COVID-positive group (36.8%) was significantly higher than both the 2020 COVID-negative and 2019 groups (11.5% and 11.7% respectively). The hospital stay was significantly higher in the COVID-positive group (mean of 24.21 days (SD 19.29)).
Conclusion
COVID-19 has had notable effects on the hip fracture care service: hip fracture rates increased significantly. There were inefficiencies in theatre processes for which we have recommended the use of alternate theatres. COVID-19 infection increased the 30-day mortality and hospital stay in hip fractures. More research needs to be done to reduce this risk.
Cite this article: Bone Joint Open 2020;1-9:530–540.
Introduction
In early 2020, the COVID-19 pandemic prompted exceptional crisis measures in NHS hospitals in the UK, reformulating numerous regular treatment protocols.1,2
Hip fractures are a major public health issue due to an ever-increasing ageing population. Approximately 76,000 hip fractures occur each year and the annual cost for all UK hip fracture cases is about £1 billion (excluding social care). Hip fractures are the subject of National Institute for Health and Care Excellence (NICE) guidance and a Best Practice Tariff is applied for performance, with the individual hospital and national outcomes recorded on the National Hip Fracture Database (NHFD).3,4 Elderly patients with hip fractures are a particularly vulnerable group during the pandemic. It is widely recognized that expedited surgical management is associated with a reduction in morbidity and mortality. The 30-day mortality rate of people with a hip fracture is 6.1% which increases to around 30% within 12 months.3,4
Our hospital provides medical and surgical services for over 350,000 people living in its catchment area. Our local NHFD export data revealed 334 hip fractures treated last year with an average time to surgery of 27.6 hours. Our local hip fracture protocol has a structured approach to optimize the perioperative management of patients. This involves a fast-track pathway from the emergency department (ED) to the orthopaedic ward within four hours. There is a dedicated orthogeriatric team that reviews patients preoperatively and takes over care postoperatively; coordinating the multidisciplinary team postoperative management and ensuring prompt and safe discharge. There is usually the provision of 13 sessions of trauma lists: two sessions daily and one on Sunday morning.
The purpose of this study is to:
1- Provide an overview of the impact caused by the COVID-19 pandemic on hip fracture care and the short-term postoperative outcomes by comparing it to our performance last year.
2- Identify areas for improvement in preparation for the persistence or resurgence of this COVID-19 pandemic, and planning for future pandemics.
Methods
Study design and participants
This was an observational, descriptive, retrospective study conducted at a single NHS hospital trust. This study was approved by our Trust Audit Committee as a service improvement activity. Included participants were all patients ≥ 60 years of age diagnosed with a proximal femoral fracture. These include intracapsular, extracapsular, peri-trochanteric, and sub-trochanteric fractures. Two groups were studied. The first group represented the period from 1 March, 2020 until 31 May, 2020. The second group corresponded to the same dates in the previous year. The 2020 group was further subdivided according to COVID status: COVID-negative and COVID-positive. Patients with polytrauma; femoral shaft, open, pathological, periprosthetic, or peri-implant fractures were excluded.
Data collection
Demographic, treatment, and outcome data were compiled from electronic medical records and most of 2019 data were obtained from our NHFD export data. Incomplete, inconsistent, or implausible data were queried and checked against electronic medical records for accuracy. The primary outcome of this study was the assessment of the 30-day mortality rate.
Patient pathway
Our local orthopaedic pathway consists of structured steps and checklists to ensure that neck of femur (NOF) cases are optimized preoperatively to facilitate safe surgery within 36 hours from registration.
Once a patient with a NOF fracture is identified via radiography in the ED, a NOF bleep is put out. This alerts the orthopaedic on-call team, patient flow manager, and the ward nurse in charge that a NOF bed is required on the designated orthopaedic ward. The ED then performs rapid targeted assessment, investigations, and pain management to ensure that the patient is safe for early transfer to the orthopaedic ward. The patient is then clerked, and a nursing and orthopaedic checklist is completed, checked, and signed by the orthopaedic registrar on-call. If a patient has a Nottingham Hip Fracture Score (NHFS) score of ≥ 6 the on-call anaesthetist is contacted to review the patient as soon as feasibly possible, otherwise they are reviewed on the morning of surgery.5
In the following trauma meeting, the patient is discussed with the orthogeriatric team present. Once called for theatres, the patient is taken into the holding bay, and then the anaesthetic room where anaesthesia is induced before they proceed to have surgery. Postoperatively, they are recovered in the recovery area until they are deemed safe to return to the ward.
One of the changes during the COVID-19 pandemic include the orthopaedic registrar independently clerking the patient and completing the checklist. As well as this, due to the shortage of regular nurses, there was difficulty in achieving the nursing checklist compliance. Moreover, the anaesthetists would only assess in theatres regardless of the NHFS score. We assumed all patients were COVID-19 positive and had a single theatre pathway. Hence, all patients were recovered in the same operating theatre.
Availability of dedicated orthopaedic trauma lists varied. Provision of dedicated trauma lists ceased for four days during the peak period of COVID-19 (23 March, 28 March, 30 March, and 4 April, 2020), and therefore, Trauma and Orthopaedics had to share the emergency operating list with other surgical specialities. This arrangement rapidly became incompatible with the volume of daily trauma cases, resulting in a high number of trauma patients awaiting surgery.
Due to doctors being redeployed, the orthogeriatric team took care of patients operated with only one registrar and junior doctor.
Variables
A total of 32 variables were studied:
-
Demographic data: age, sex, and type of fracture.
-
COVID status: this was applied to the 2020 group. We also assessed its relation against the NHFS.5
-
Preoperative assessment - this included:
-
Time to imaging: time from ED registration or from inpatient fall until the imaging was performed.
-
Four-hour target: time from ED registration until arrival on the orthopaedic ward.
-
Checklist compliance: our pathway involves completion of a 15-point checklist of preoperative measures to ensure patients are fit for surgery to achieve the 36 hour best practice tariff target (Figure 1).
-
Hours to operation: time from ED registration until arrival in theatre.
-
-
Theatre management:
-
Sending time: time from calling the ward to send the patient until the patient arrives in theatres.
-
Holding bay time: time from the arrival of the patient in theatres holding bay until arrival in the anaesthetic room.
-
Anaesthetic preparation time: time from the arrival of the patient in the anaesthetic room until induction of anaesthesia. This time included donning of the personal protective equipment (PPE) by the anaesthetic team in all 2020 group either COVID-positive or -negative.
-
Anaesthesia time: time from induction of anaesthesia until knife to skin.
-
Operation time: time taken from knife to skin until completion of skin closure.
-
Recovery time: time of the patient in the recovery room until patient arrival back on the ward. Due to COVID regulations, recovery was done in theatres in the 2020 group.
-
Type of anaesthesia.
-
Intraoperative complications.
-
-
Postoperative review:
-
Day zero review: medical and surgical review of the patient within 12 hours after operation.
-
Day one postoperative review by Orthopaedic Consultant.
-
Nutrition assessment: malnutrition universal screening tool calculation to assess if a patient is malnourished.
-
Bone health assessment: osteoporosis screen.
-
-
KPIs3: The KPIs set by NHFD measure performance against guidance and clinical standards for hip fracture care from NICE. These include:
-
KPI 1 – Prompt orthogeriatric assessment: percentage of hip fracture patients assessed by a Senior Orthogeriatrician within 72 hours.
-
KPI 2 – Prompt surgery: percentage of patients receiving hip fracture surgery by the day following admission.
-
KPI 3 – NICE compliant surgery: percentage of patients who received a NICE compliant surgical approach to their hip fracture surgery.
-
KPI 4 – Prompt mobilization after surgery: percentage of patients mobilized by the day following hip fracture surgery.
-
KPI 5 – Not delirious when tested after surgery: percentage of patients who were assessed and found not to be delirious after their surgery.
-
KPI 6 – Return to original residence by 120 days: percentage of patients known to have returned to their original residence by 120 days after their hip fracture.
-
-
Postoperative complications:
-
Wound infection.
-
Reoperation rate.
-
Inpatient falls: any fall the patient experienced postoperatively during their hospital stay.
-
-
30-day mortality.
-
Length of the hospital stay.
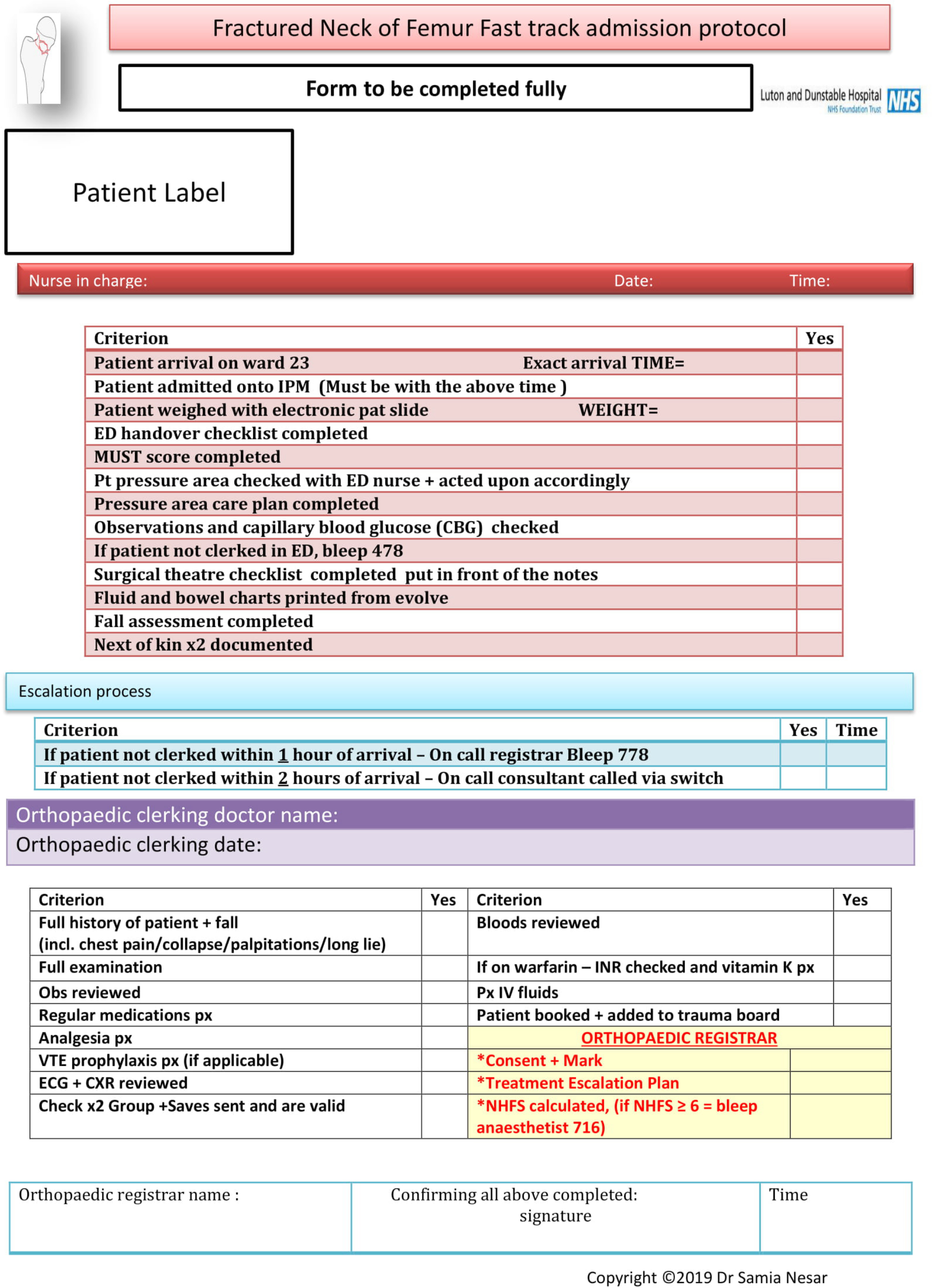
Fig. 1
Checklist for fracture neck of femur fast-track admission protocol, courtesy of Dr S. Nesar. CXR, chest x-ray; ED, emergency department; IPM, in-patient management; INR, international normalized ratio; IV, intravenous; MUST, malnutrition universal screening tool; VTE, venous thromboembolism.
Statistical analysis
Data were entered into the computer and analyzed using International Business Machines Statistical Package for the Social Sciences (IBM SPSS) software package version 20.0 (IBM; Armonk, New York, USA). Qualitative data were described using the number and percentage. The Kolmogorov-Smirnov test was used to verify the normality of distribution. Quantitative data were described using range (minimum and maximum), mean, SD, median, and interquartile range (IQR). A p-value ≤ 0.05 was considered statistically significant.
The following statistical tests were:
-
Chi-squared test: for categorical variables, to compare between different groups.
-
Fisher’s exact test or Monte Carlo correction: correction for chi-squared when more than 20% of the cells have expected count less than five.
-
Independent-samples t-test: For normally distributed quantitative variables, to compare between two studied groups.
-
Mann-Whitney U test: for abnormally distributed quantitative variables, to compare between two studied groups.
-
F-test (analysis of variance (ANOVA)): for normally distributed quantitative variables, to compare between more than two groups, and post hoc Tukey test for pairwise comparisons.
-
Kruskal Wallis test: for abnormally distributed quantitative variables, to compare between more than two studied groups and post hoc (Dunn's multiple comparisons test) for pairwise comparisons.
Results
Demographic data
A total of 157 records were identified. During the COVID-19 pandemic, there was a significant increase in the number of hip fractures. We had 37 more hip fractures in 2020 compared to 2019, equivalent to an increase of 61.7%. In all, 67 patients (69%) in 2020 group were tested for COVID-19, 17 (17.5%) of whom had a confirmed positive test; we believed two patients (2%) had a false negative test, as although their swab tests were negative, their clinical and radiological findings indicated the presence of COVID-19: these were therefore also considered COVID-positive (Figure 2). There were no statistically significant differences in mean age, sex, or fracture types among the three groups (Table I). Six patients (two in COVID-positive, one in COVID-negative, and three in the 2019 group) were medically unfit for surgery and died preoperatively. Two patients in the 2020 group underwent conservative management, though they failed and needed surgery.
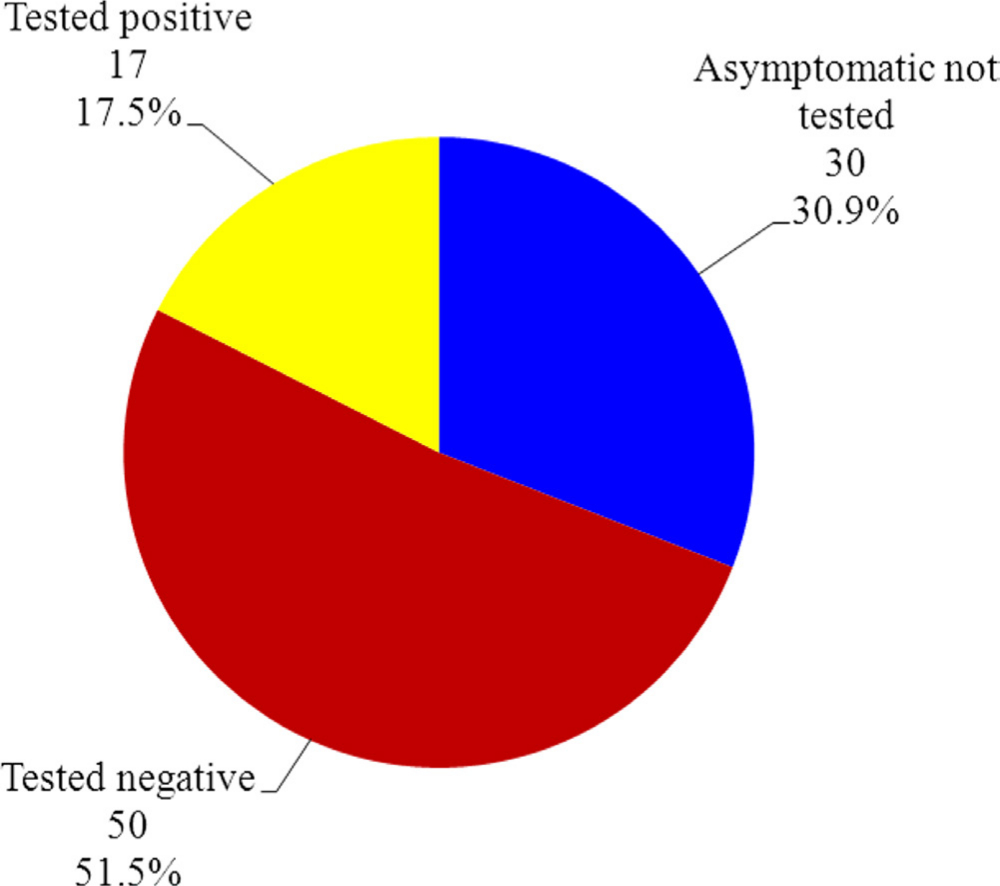
Fig. 2
COVID-19 test status of hip fractures in 2020 group.
Table I.
Comparison between the three studied groups according to demographic data.
| Characteristic | Group 2019 (n = 60), n (%) |
Group 2020 | p-value | |
|---|---|---|---|---|
| COVID-negative (n = 78), n (%) |
COVID-positive (n = 19), n (%) |
|||
| Sex | 0.225* | |||
| Male | 19 (31.7) | 21 (26.9) | 9 (47.4) | |
| Female | 41 (68.3) | 57 (73.1) | 10 (52.6) | |
| Age (yrs) | 0.288† | |||
| Range | 60 to 100 | 60 to 99 | 68 to 96 | |
| Mean (SD) | 83.33 (8.28) | 83.05 (7.64) | 86.21 (7.71) | |
| Median (IQR) | 84.0 (79.0 to 90.0) | 83.50 (79.0 to 87.0) | 90.0 (82.0 to 91.50) | |
| Fracture type, n | 0.418* | |||
| IC | 43 (71.7) | 49 (62.8) | 11 (57.9) | |
| EC | 17 (28.3) | 29 (37.2) | 8 (42.1) |
-
*
Chi-squared test.
-
†
F-test for analysis of variance (ANOVA).
-
EC, extracapsular; IC, intracapsular; IQR, interquartile range
Preoperative assessment
The checklist compliance was statistically significant, however the time to imaging, four-hour target, and the mean hour to operation variables were not (Table II) (Figure 3).
Table II.
Comparison between the three studied groups according to preoperative assessment.
| Variable | Group 2019 (n = 60) |
Group 2020 | p-value | |
|---|---|---|---|---|
| COVID-negative (n = 78) |
COVID-positive (n = 19) |
|||
| Timing of radiograph, mins | 0.606* | |||
| Range | 7 to 354 | 1 to 571 | 1 to 117 | |
| Mean (SD) | 50.03 (57.92) | 51.74 (69.76) | 47.95 (33.88) | |
| Median (IQR) | 26.0 (16.50 to 57.50) | 37.0 (23.0 to 58.0) | 36.0 (21.0 to 74.50) | |
| Four hours target | 0.513† | |||
| No, n (%) | 30 (50.0) | 33 (42.3) | 7 (36.8) | |
| Yes, n (%) | 30 (50.0) | 45 (57.7) | 12 (63.2) | |
| Checklist compliance | < 0.001† | |||
| No, n (%) | 27 (45.0) | 13 (16.7) | 6 (31.6) | |
| Yes, n (%) | 33 (55.0) | 65 (83.3) | 13 (68.4) | |
| Hours to operation | 0.066* | |||
| Range | 5.07 to 68.03 | 10.0 to 390.0 | 12.0 to 49.0 | |
| Mean (SD) | 24.96 (15.43) | 28.96 (47.85) | 28.59 (10.23) | |
| Median (IQR) | 19.08 (13.02 to 35.10) | 20.0 (16.0 to 24.0) | 26.0 (22.0 to 35.0) |
-
*
H for Kruskal Wallis test.
-
†
Chi-squared test.
-
IQR, interquartile range
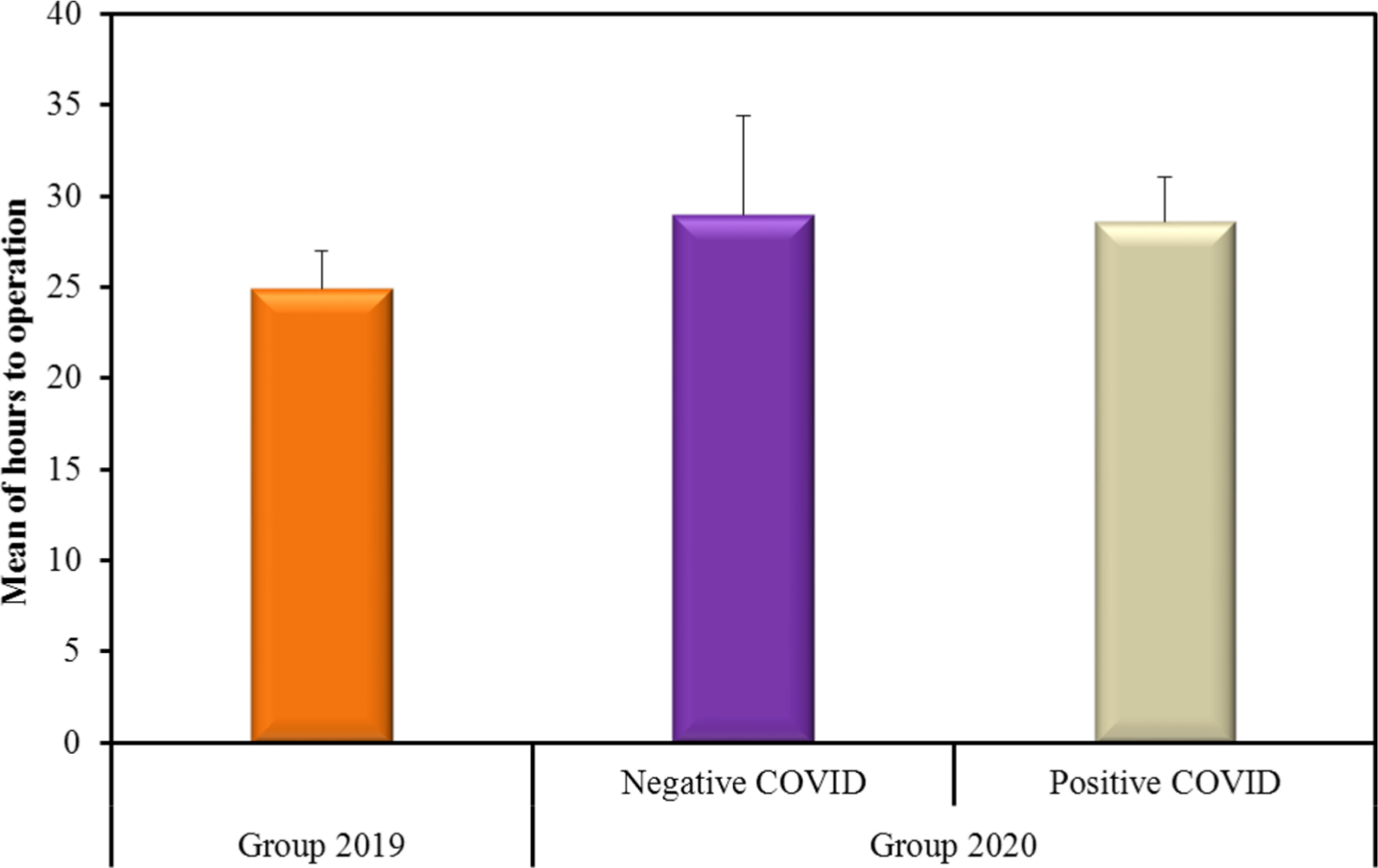
Fig. 3
Comparison between the three studied groups according to hours to operation.
Theatre management
The COVID-positive group showed a significant delay in the mean anaesthetic preparation and anaesthetic times (14.06 and 68.88 minutes, respectively). The mean recovery time, however, was significantly shorter (76.71 minutes, p = 0.010, Kruskal-Wallis test). This was being performed in theatres during the pandemic. Nevertheless, all other timings showed no statistical difference (Figure 4). There was no difference regarding the type of anaesthesia and intraoperative complications (Table III).
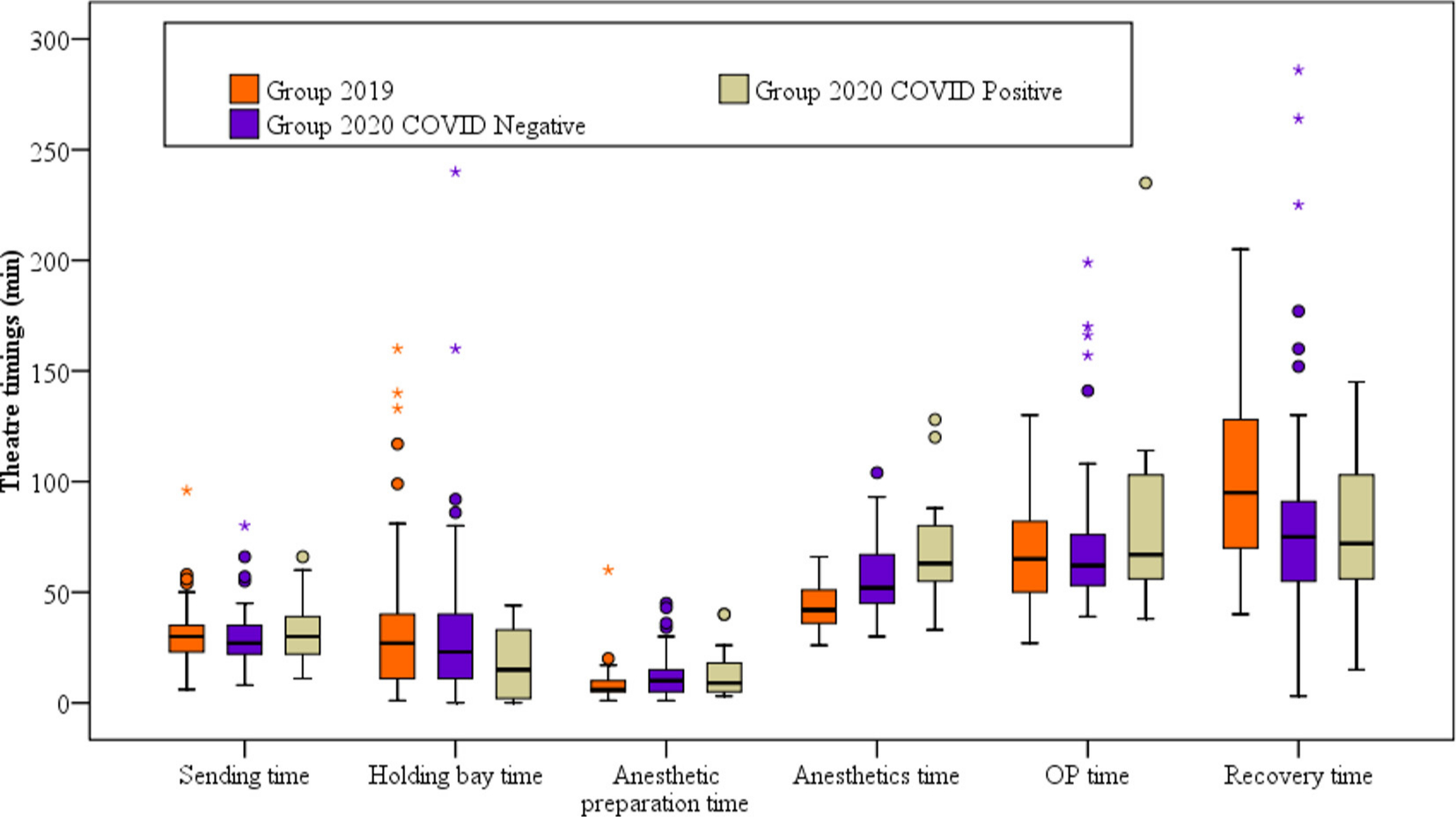
Fig. 4
Comparison between the three studied groups according to theatre timings. Asterisks indicate outliers.
Table III.
Comparison between the three studied groups according to types of anaesthesia and intraoperative complications.
| Variable | Group 2019 (n = 57), n (%) |
Group 2020 | p-value* | |
|---|---|---|---|---|
| COVID-negative (n = 77), n (%) |
COVID-positive (n = 17), n (%) |
|||
| Type of anaesthesia | 0.557 | |||
| General | 24 (42.1) | 39 (50.6) | 9 (52.9) | |
| Spinal | 33 (57.9) | 38 (49.4) | 8 (47.1) | |
| Intraoperative complications | MC0.721 | |||
| No | 55 (96.5) | 74 (96.1) | 16 (94.1) | |
| Yes | 2 (3.5) | 3 (3.9) | 1 (5.9) | |
-
*
Chi-squared test, with Monte Carlo (MC) correction where more than 20% of the cells have an expected count of less than five.
Postoperative review
The three groups showed no statistical difference across all parameters except for the day one postoperative review by the orthopaedic consultant, which showed significant improvement in the 2020 group (Table IV).
Table IV.
Comparison between the three studied groups according to postoperative reviews.
| Postoperative review | Group 2019 (n = 57), n (%) |
Group 2020 | p-value* | |
|---|---|---|---|---|
| COVID-negative (n = 77), n (%) |
COVID-positive (n = 17), n (%) |
|||
| Day 0 review | MC0.312 | |||
| No | 6 (10.5) | 4 (5.2) | 0 (0.0) | |
| Yes | 51 (89.5) | 73 (94.8) | 17 (100.0) | |
| Day 1 postop review by Ortho cons | < 0.001† | |||
| No | 33 (57.9) | 10 (13.0) | 4 (23.5) | |
| Yes | 24 (42.1) | 67 (87.0) | 13 (76.5) | |
| Nutrition assessment | MC0.374 | |||
| No | 2 (3.5) | 4 (5.2) | 2 (11.8) | |
| Yes | 55 (96.5) | 73 (94.8) | 15 (88.2) | |
| Bone health assessment | N/A | |||
| No | 0 (0.0) | 0 (0.0) | 0 (0.0) | |
| Yes | 57 (100.0) | 77 (100.0) | 17 (100.0) | |
-
*
Chi-squared test, with Monte Carlo (MC) correction where more than 20% of the cells have an expected count of less than five.
-
†
Statistically significant at p ≤ 0.05.
-
N/A, not applicable.; Ortho cons, orthopaedic consultant
KPIs
The differences in KPIs were statistically insignificant, but they showed a decrease in the number of patients who returned to original residence among the COVID-positive which was as low as 58.8% (Table V). The reasons for the delay in surgery are outlined in Figure 5.
Table V.
Comparison between the three studied groups according to the key performance indicators (KPIs).
| KPI | Group 2019 (n = 57), n (%) |
Group 2020 | p-value* | |
|---|---|---|---|---|
| COVID-negative (n = 77), n (%) | COVID-positive (n = 17), n (%) |
|||
| Prompt orthogeriatric review | MC0.211 | |||
| No | 0 (0.0) | 1 (1.3) | 1 (5.9) | |
| Yes | 57 (100.0) | 76 (98.7) | 16 (94.1) | |
| Prompt surgery | 0.389 | |||
| No | 13 (22.8) | 11 (14.3) | 4 (23.5) | |
| Yes | 44 (77.2) | 66 (85.7) | 13 (76.5) | |
| NICE-compliant surgery | 0.260 | |||
| No | 11 (19.3) | 18 (23.4) | 1 (5.9) | |
| Yes | 46 (80.7) | 59 (76.6) | 16 (94.1) | |
| Prompt mobilization | MC0.351 | |||
| No | 2 (3.5) | 0 (0.0) | 0 (0.0) | |
| Yes | 55 (96.5) | 77 (100.0) | 17 (100.0) | |
| Not delirious postop | 0.565 | |||
| No | 13 (22.8) | 12 (15.6) | 3 (17.6) | |
| Yes | 44 (77.2) | 65 (84.4) | 14 (82.4) | |
| Return to original residence | 0.197 | |||
| No | 13 (22.8) | 16 (21.8) | 7 (41.2) | |
| Yes | 44 (77.2) | 61 (78.2) | 10 (58.8) | |
-
*
Chi-squared test, with Monte Carlo (MC) correction where more than 20% of the cells have an expected count of less than five.
-
NICE, National Institute for Health and Care Excellence; postop, postoperative
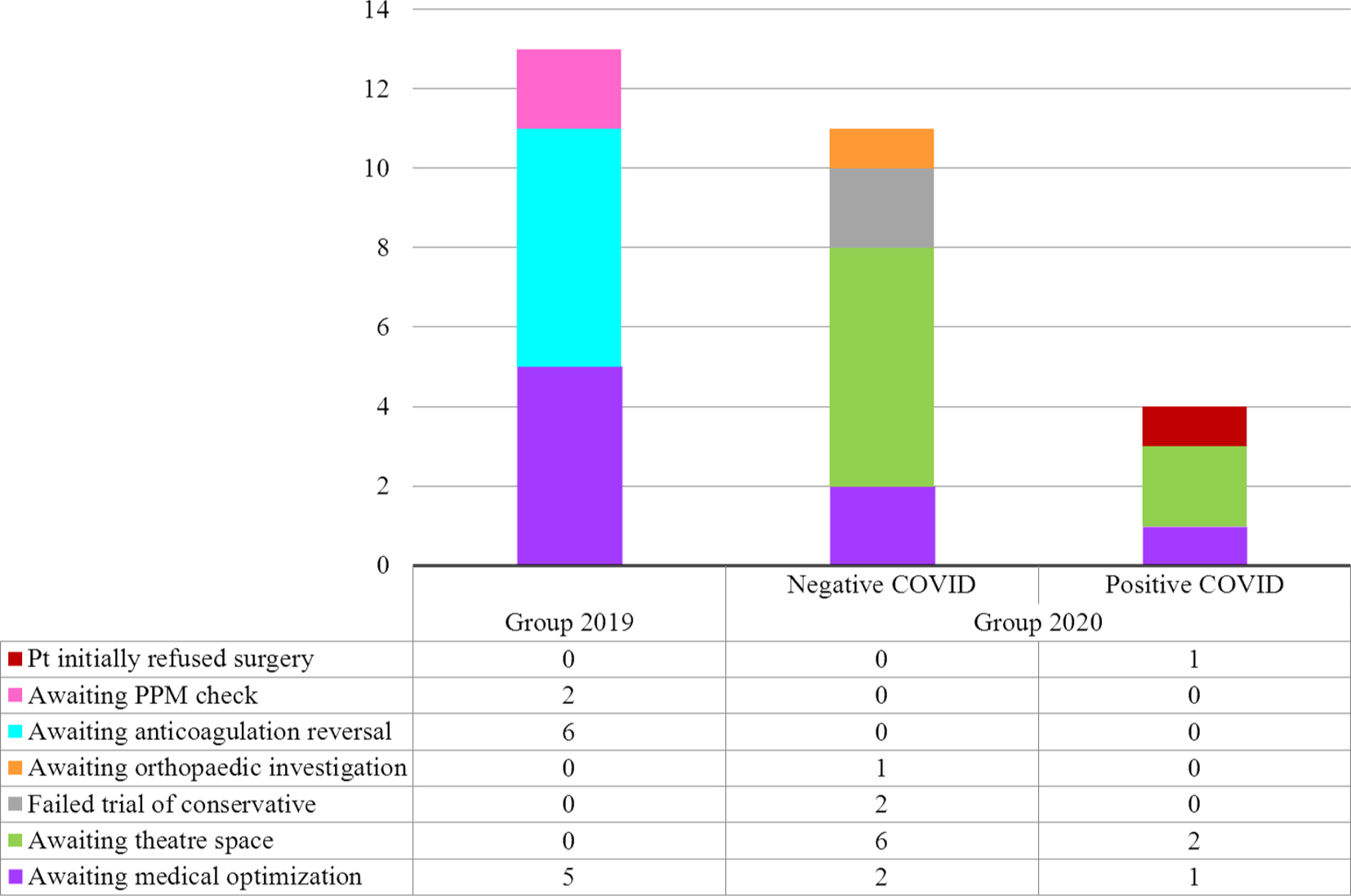
Fig. 5
Reasons for delay in surgery. PPM, permanent pacemaker; Pt, patient.
Postoperative complications
There were no statistically significant differences except for inpatient falls which were significantly higher in the 2020 group (7.2%) compared to 2019 group (0%) (Table VI). One patient was reoperated due to hemiarthroplasty dislocation in 2019, while two patients in the 2020 group were reoperated due to hemiarthroplasty dislocation and wound dehiscence.
Table VI.
Comparison between the three studied groups according to postoperative complication.
| Postoperative complication | Group 2019 (n = 57), n (%) |
Group 2020 | MCp-value | |
|---|---|---|---|---|
| COVID-negative (n = 77), n (%) |
COVID-positive (n = 17), n (%) |
|||
| Wound infection | 0.492* | |||
| No | 56 (98.2) | 77 (100.0) | 17 (100.0) | |
| Yes | 1 (1.8) | 0 (0.0) | 0 (0.0) | |
| Inpatient falls | 0.012‡ | |||
| No | 57 (100.0) | 73 (94.8) | 14 (82.4) | |
| Yes | 0 (0.0) | 4 (5.2) | 3 (17.6) | |
| Reoperation | 1.000* | |||
| No | 56 (98.2) | 75 (97.4) | 17 (100.0) | |
| Yes | 1 (1.8) | 2 (2.6) | 0 (0.0) |
-
Monte Carlo (MC) correction used where more than 20% of the cells have an expected count of less than five.
-
*
Chi-squared test
-
†
Fisher's exact test
-
‡
Statistically significant at p ≤ 0.05
30-day mortality
The 30-day mortality was significantly higher in the 2020 COVID-positive group (7/19 patients, 36.8%) than the 2020 COVID-negative and 2019 groups ((7/78 patients (11.5%) and 7/60 patients (11.7%), respectively); p = 0.014, chi-squared test). The causes of death are outlined in Figure 6. There were two patients of the COVID-negative group who were discharged and re-admitted within 30 days under the care of the Department of Medicine for the Elderly (DME) and subsequently died with COVID pneumonia.
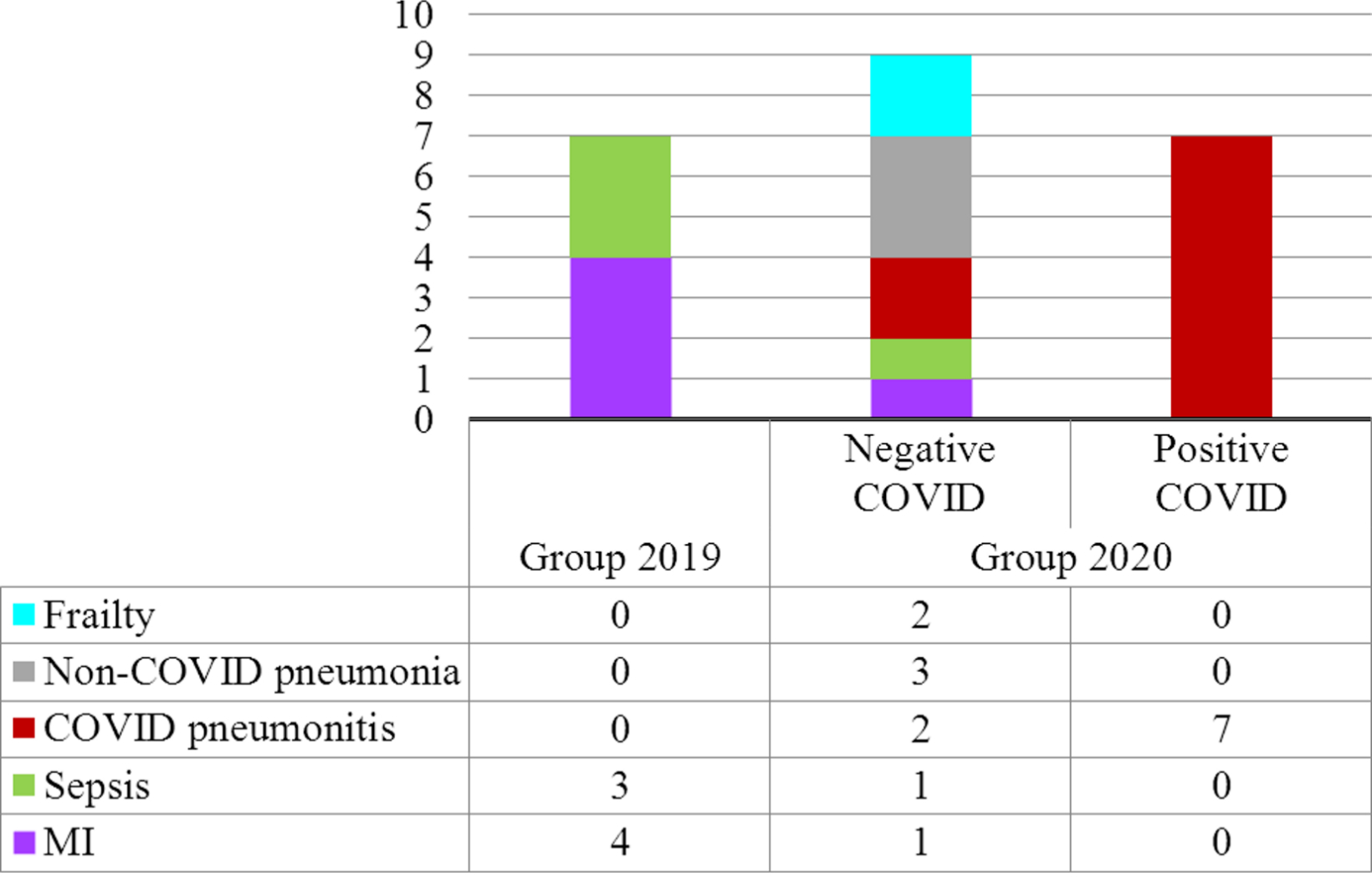
Fig. 6
Comparison between the three studied groups according to causes of death. MI, myocardial infarction.
The length of hospital stay
The mean length of hospital stay was significantly longer in the COVID-positive group compared to the other two groups (Figure 7). Though not statistically significant (p = 0.068, independent-samples t-test), the mean NHFS was higher in the COVID-positive group of 19 patients (5.79 (SD 1.08)) compared to the COVID-negative group of 78 patients (5.10 (SD 1.53)) .
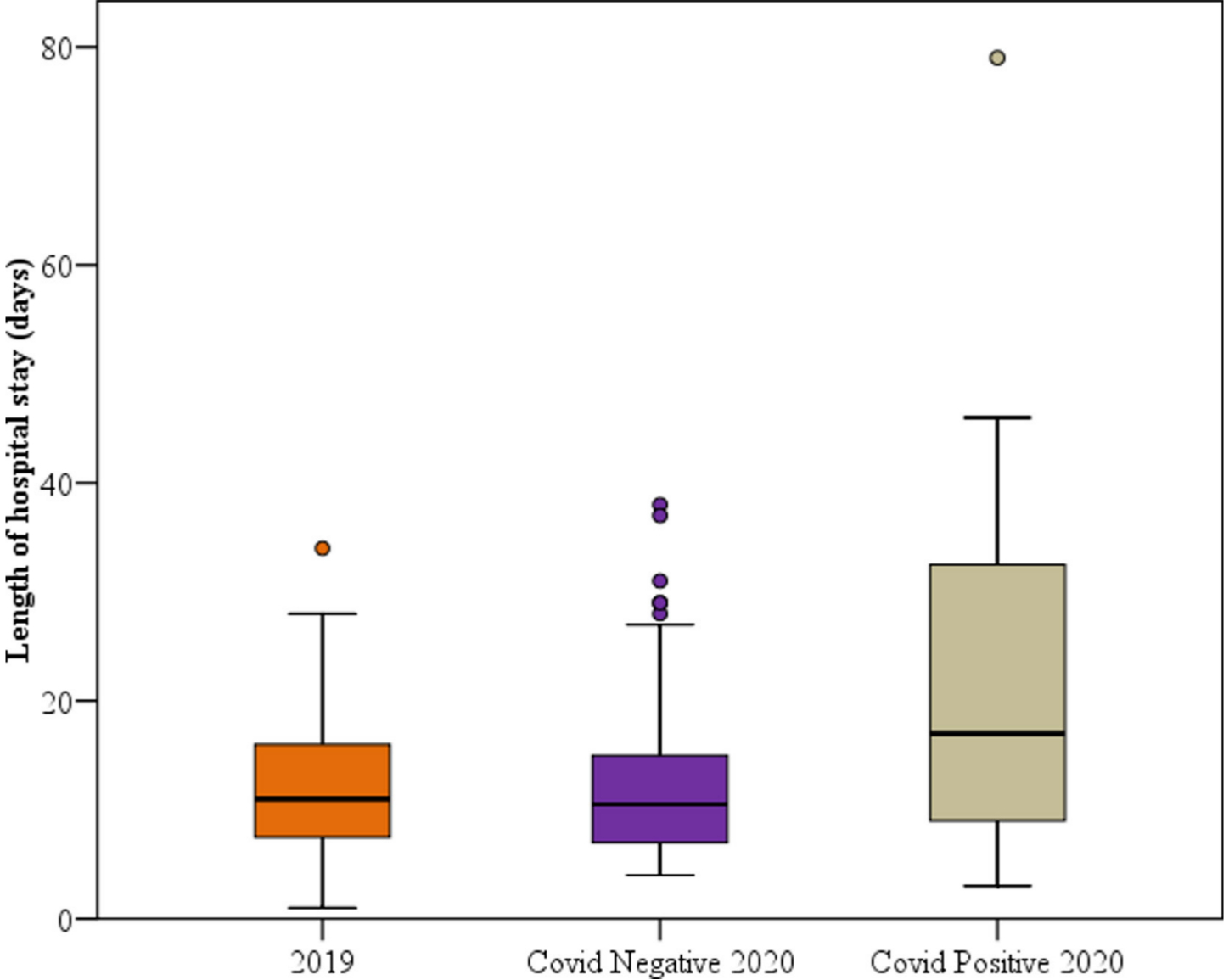
Fig. 7
Comparison between the three studied groups according to length of hospital stay.
Discussion
The COVID-19 pandemic caused unprecedented challenges to hospitals in the UK. Numerous changes and adaptations to service delivery, patient pathways, and work patterns were introduced in response to the influx of COVID-19 patients. A mandate from the government was issued to suspend all elective surgeries on the 17 March 2020 to expand service capacity to cover the surge of COVID-19 patients. Most of the theatre staff (mainly anaesthetists, Operating Department Practitioners, and theatrepractitioners) was redeployed to the intensive care unit (ICU). The unfamiliarity of the pandemic protocols, including PPE, resulted in decreased theatre turnaround times, negatively affecting Trauma and Orthopaedics’ efficiency.
Hip fracture surgery is one of the most common major operations undertaken in any trauma unit. Elderly people are more prone to these fractures due to frailty, osteoporosis, and associated medical comorbidities which make them more adversely affected by COVID-19 infections, due to their diminished functional reserves and weakened immune systems.6
The analysis of our data shows a significant increase in the number of admitted hip fractures. Despite national lockdown and traffic restrictions, the number of older patients with hip fractures significantly increased. One can assume that due to the social isolation policy, support obtained from relatives and carers may have been reduced for these individuals; this could have inadvertently been a cause of the increased hip fractures occurring at home.2 This contrasts with the decrease in the number of hip fractures as revealed in the data from Maniscalco et al7 (decrease from 169 to 121) and Malik-Tabassum et al8(decrease from 84 to 68).
The rates of checklist compliance were much higher during the pandemic. This could be due to the fact that more senior doctors were on the shop floor and staff members were more cautious in ensuring protocol was followed in order to avoid unnecessary delays or loss of valuable theatre space.
The mean hours to operation, though not significant, was higher in the 2020 group (28.59 (SD 10.23)) in comparison to the 2019 group (24.96 (SD 15.43)). This was better than data revealed from the Spanish study by Muñoz Vives et al9 which showed a mean delay to surgery of 2.4 days. However, our data contrast to the data revealed by Malik-Tabassum et al8 which showed a reduction in the mean hours to operation (21.8 hours) in a similar period, but their study only comprised one COVID-positive patient compared to 19 in our study. The theatre delays were mostly due to administrative issues (awaiting theatre space) which were exacerbated by the COVID-19 pandemic.
There was a significant difference in theatre times among the three groups due to the PPE donning and doffing requirements and staffing issues. However, in hindsight, this could have been improved through the use of alternative theatres to improve turnaround times. Additional theatre space was not an issue as all elective activity had ceased.
This study showed that despite severe disruptions to the acute trauma services at our hospital, the KPIs for hip fracture patients did not show a significant difference. Our team continued to adhere to strict protocols set on existing NOF templates.
The mean length of hospital stay in the COVID-positive group was significantly higher than the other two groups while Malik-Tabassum et al8 revealed a mean length of stay as 8.6 days. This difference may be due to barriers to discharge planning, including awaiting COVID-positive patients to become COVID-negative; this factor is not applicable for Malik-Tabassum et al8 who only had one COVID-positive patient who died four days following their admission.
The rate of inpatient falls was noticeably higher in the 2020 group (7.2%) compared to the 2019 group (0%). This can be attributed to the lack of staff, isolation of COVID-positive or symptomatic patients, and the time taken to comply with PPE precautionary measures before being able to assist the patient.
The postoperative wound infection rate remained 0% in the 2020 group despite the modified intraoperative measures taking place in response to COVID-19. This includes the limited use of diathermy, lack of the pulsed lavage, use of a nibbler instead of the saw to level the neck cut, and use of absorbable subcuticular sutures instead of skin clips. As a department, we made these choices to minimize droplet and aerosol formation and reduce the need for direct future patient contact (e.g. suture removal). Taking into account the small size of this study’s population, these measures may not necessarily be routinely used for future pandemics. Nevertheless, it is undoubtedly a good area for further multicentre research.
The 30-day mortality in the COVID-positive group (36.8%) was higher than the 22.2% 30 day-mortality revealed by Archer et al10 in their study examining a similar cohort of 18 patients. Another study from Spain reported mortality in this cohort as high as 30.4%9 whilst Malik-Tabassum et al8 reported an 8.8% mortality, but it must be taken into account that this study only had one COVID-positive patient. The high percentage of mortality in these patients can be explained by their old age and associated medical comorbidities which make them more vulnerable to COVID-19 infection complications. However, this should not affect the decision to perform expedited surgery as the surgery itself can contribute to the overall stability of the patient, improvement of physiological ventilation, and respiratory parameters as noted in 12 COVID-19 positive patients who underwent surgical treatment of proximal femoral fractures by Catellani et al.11
Additionally, two patients from the COVID-negative group were readmitted under the DME after becoming COVID-positive following discharge back to their care homes, and subsequently died. This leads us to believe that extra precautions should be undertaken with these patients after their discharge, especially those classed as ‘vulnerable’.
Based on the NHS England guide for management of fragility fractures during this pandemic,2 two patients with intracapsular fractures in the 2020 group were selected for nonoperative management. It was noted that both failed and needed surgery. Although these measures were taken in an attempt to reduce the operative burden and free more beds, they were counter-productive; therefore, the department rapidly resorted to our previous management strategy of early intervention.
Our data show a significant increase in hip fractures during this pandemic. Therefore, given the future risk of a ‘second wave’ or future pandemics, it is vital that stakeholders understand the impact of the pandemic on major public health concerns such as NOF fractures and provision needs to be made for these in planning. There were inefficiencies in theatre processes which could have been improved by continuing to utilize an operative approach and alternate theatres to ensure improved efficiency and reduced recovery times.
While we appreciate the need for staff redeployment, it is very important that wards or areas of identified high-risk patients remain adequately staffed. Unfortunately, due to the limited evidence-based research about COVID-19 and lack of proven management strategies at the time, this resulted in an expected mortality spike. We advise for a faster response that aims to improve the infrastructure for swifter screening tests, facilitate early discharge, and reduce hospital stay. We should also aim to dedicate more resources while facing a possible second wave or future pandemics in this highly vulnerable patient group with NOF fractures.
The limitations of our study include its retrospective observational design, single-centred nature, and relatively small sample. A larger multicentre study would be beneficial. There may be confounding variables of which we are not yet aware.
References
1. British Orthopaedic Association . Emergency BOAST: management of patients with urgent orthopaedic conditions and trauma during the coronavirus pandemic . 2020 . https://www.boa.ac.uk/resources/COVID-19-boasts-combined.html (date last accessed 1 July 2020 ). Google Scholar
2. NHS England . Clinical guide for the perioperative care of people with fragility fractures during the coronavirus pandemic . 2020 . https://www.england.nhs.uk/coronavirus/wp-content/uploads/sites/52/2020/03/C0086_Specialty-guide-_Fragility-Fractures-and-Coronavirus-v1-26-March.pdf (date last accessed 1 July 2020 ). Google Scholar
3. Royal College of Physicians . National hip fracture database annual report 2019 . London : RCP , 2019 . Google Scholar
4. National Institute for Clinical Excellence . Hip fracture: management CG124 . 2017 . https://www.nice.org.uk/guidance/cg124 (date last accessed 16 July 2020 ). Google Scholar
5. Moppett IK , Parker M , Griffiths R , Bowers T , White SM , Moran CG . Nottingham hip fracture score: longitudinal and multi-assessment . Br J Anaesth . 2012 ; 109 ( 4 ): 546 – 550 . Crossref PubMed Google Scholar
6. Chen N , Zhou M , Dong X , et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study . Lancet . 2020 ; 395 ( 10223 ): 507 – 513 . Crossref PubMed Google Scholar
7. Maniscalco P , Poggiali E , Quattrini F , et al. Proximal femur fractures in COVID-19 emergency: the experience of two Orthopedics and Traumatology Departments in the first eight weeks of the Italian epidemic . Acta Biomed . 2020 ; 91 ( 2 ): 89 – 96 . Crossref PubMed Google Scholar
8. Malik-Tabassum K , Crooks M , Robertson A , To C , Maling L , Selmon G . Management of hip fractures during the COVID-19 pandemic at a high-volume hip fracture unit in the United Kingdom . J Orthop . 2020 ; 20 : 332 – 337 . Crossref PubMed Google Scholar
9. Muñoz Vives JM , Jornet-Gibert M , Cámara-Cabrera J , et al. Mortality rates of patients with proximal femoral fracture in a worldwide pandemic: preliminary results of the Spanish HIP-COVID observational study . J Bone Joint Surg Am . 2020 ; 102-A ( 13 ): e69 . Crossref PubMed Google Scholar
10. Archer JE , Kapoor S , Piper D , Odeh A . The impact of COVID-19 on 30-day mortality in patients with neck of femur fractures . Bone Joint Open . 2020 ; 1-7 : 326 – 329 . Google Scholar
11. Catellani F , Coscione A , D'Ambrosi R , Usai L , Roscitano C , Fiorentino G . Treatment of proximal femoral fragility fractures in patients with COVID-19 during the SARS-CoV-2 outbreak in northern Italy . J Bone Joint Surg Am . 2020 ; 102 ( 12 ): e58 . Crossref PubMed Google Scholar
Author contributions
M. Arafa: Collected the data, Wrote and revised the manuscript.
S. Nesar: Collected the data, Wrote the manuscript.
H. Abu-Jabeh: Collected the data, Wrote the manuscript.
M. O. R. Jayme: Collected the data, Wrote the manuscript.
Y. Kalairajah: Wrote and revised the manuscript.
Funding statement
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
ICMJE COI statement
None declared.
Acknowledgements
We would like to thank all the staff of our trauma & orthopaedic department and orthogeriatric team in Luton and Dunstable hospital and in particular our trauma coordinator Anne Barker.
© 2020 Author(s) et al. This is an open-access article distributed under the terms of the Creative Commons Attributions licence (CC-BY-NC-ND), which permits unrestricted use, distribution, and reproduction in any medium, but not for commercial gain, provided the original author and source are credited.









