Abstract
Post-traumatic elbow stiffness is a disabling condition that remains challenging for upper limb surgeons. Open elbow arthrolysis is commonly used for the treatment of stiff elbow when conservative therapy has failed. Multiple questions commonly arise from surgeons who deal with this disease. These include whether the patient has post-traumatic stiff elbow, how to evaluate the problem, when surgery is appropriate, how to perform an excellent arthrolysis, what the optimal postoperative rehabilitation is, and how to prevent or reduce the incidence of complications. Following these questions, this review provides an update and overview of post-traumatic elbow stiffness with respect to the diagnosis, preoperative evaluation, arthrolysis strategies, postoperative rehabilitation, and prevention of complications, aiming to provide a complete diagnosis and treatment path.
Cite this article: Bone Joint Open 2020;1-9:576–584.
Introduction
Post-traumatic elbow stiffness (PTES) is a well-known complication of elbow trauma; it causes upper limb disabilities and severely affects daily activities, mainly due to the formation of heterotopic ossification (HO)1 and soft tissue adhesion and contracture.2 A loss of 50° in the arc of motion can cause up to 80% loss of function.3 Treatment goals for PTES involve regaining a stable, painless elbow with functional range. Generally, conservative therapy such as static or dynamic splinting is the first choice within six months after trauma.4 Thereafter, surgery can be performed if the patient is dissatisfied with the range of movement (ROM) and desires to improve function. There are three main operating methods for PTES: arthroscopic release, open elbow arthrolysis (OEA), and arthroplasty. Among these, though more complex release can be performed with greater experience, arthroscopic release is usually only considered for simple elbow stiffness;5 total elbow arthroplasty may be considered in less active and older patients only if no other treatment options are available.6 Therefore, OEA is still the commonest operative method for PTES.
In 1944, Wilson7 first reported treatment of PTES caused by supracondylar fracture of the humerus by capsule excision. In the following 70 years, significant improvements have occurred in OEA.8-10 A systematic review of 637 patients showed a mean increase of 51° in ROM and a 23% rate of complications after OEA; however, the treatment regimen and efficacy varied.8
Due to poor understandings of the treatment principles, nonstandard surgical procedures and insufficient prevention of complications for some surgeons, the therapeutic effect of OEA is often unsatisfactory. As Morrey11 noted, “loss of joint motion is a common complication of elbow trauma. Dealing with post-traumatic elbow stiffness is a challenging task for the orthopaedic surgeon”. Therefore, in this article, we review the complete diagnosis and treatment path of OEA for treating PTES, including diagnosis, preoperative evaluation, arthrolysis strategies, postoperative rehabilitation, and prevention of complications.
Definition and diagnosis
Based on a 3D optical tracking technology, functional elbow motion necessary for contemporary and modern tasks such as using a cellular telephone or keyboard is wider than the traditional “double 100°” reported by Morrey.3 Currently a ROM of approximately 120° in flexion and extension and 140° in forearm rotation arc (FRA) are required.12 Further functional improvement is also needed if patients cannot complete the actions required by their occupation or interests, even if the above range is met. Therefore, the existing definition of elbow stiffness (flexion < 120°, extension > 30°, or rotation < 45° in either direction13) should be updated to “range of elbow motion or rotation not meeting patient needs in entertainment, work, and daily life”.
When a patient reports with PTES, injury history and limited elbow mobility are the main complaints. Injuries include elbow dislocation, fractures (such as distal humerus, olecranon, radial head, and terrible triad injury), brain trauma, and burns. Limited mobility manifests as restricted elbow extension or flexion, and pronation or supination. Additional symptoms commonly include pain and neurological symptoms (sensory and motor dysfunction); less commonly, muscle atrophy, osteoporosis, and joint degeneration are seen.
Preoperative evaluations
ROM measurement
The universal goniometer, a simple and easy-to-use instrument with 360° scale (1° increments), is most used for elbow ROM measurement. One study described the three bony landmarks in detail: the lateral epicondyle (centres), the tip of acromion process (stationary arm points), and the middle portion of wrist (mobile arm points).14 The intraclass correlation coefficients for goniometric measurement of the elbow ranged from 0.945 to 0.973, indicating good reliability.14 The usual practice is to round the values to 5° steps up or down. Although this seems precise enough, a recent study showed that the accuracy of statistical tests performed on rounded ROM data is limited, referred to as “rounding error”, and they proposed a p-value (α) correction for tests on rounded ROM data.15
Imaging, laboratory, and electrodiagnostic examination
Radiographs are necessary to assess the joint anatomy, articular congruity, and presence and location of loose bodies, HOs, and osteophytes that may limit motion. Calculated tomography (CT) with 3D reconstruction is helpful for accurate localization of blocks and further detail of the articular surface. A recent study demonstrates that CT can also determine the path and spatial relationship to HO of the radial and median nerves at the elbow.16
Measurement of inflammatory markers, such as C-reactive protein and erythrocyte sedimentation rate, help detect infection or inflammatory conditions. Elevated serum alkaline phosphatase levels help predict the occurrence or recurrence of HO, especially in children.17
The presence of nerve compression can be confirmed by findings of sensory loss, motor weakness, or nerve hypersensitivity. Moreover, electromyography and nerve conduction velocity studies can be useful as confirmatory studies.18
Classification
Several classifications are used to describe elbow stiffness. The commonly used three-type Morrey’s classification19 allows better understanding of the cause: intrinsic components involve intra-articular adhesions, articular malalignment, and cartilage loss; extrinsic components involve capsular and ligamentous contracture and HO; in reality, most are a combination of both. Mansat’s classification20 has four parts based on ROM (mild, ROM > 90°; moderate, 60°< ROM ≤ 90°; severe, 30°< ROM ≤ 60°; and very severe, ROM ≤ 30°). Recently, a new classification – the Fan’s classification, comprising four types of flexion-extension dysfunction (tethers alone, tethers with blocks, articular malformation, and bony ankylosis) and three types of forearm rotation dysfunction (contracture alone, radial head malunion or nonunion, and proximal radioulnar bony ankylosis), was introduced to specify and standardize the operative approaches and arthrolysis steps.21
Hastings and Graham22 divide elbow HO into three types: I, radiologically evident without functional limitation; II, radiologically evident with functional limitation, and subdivided into IIA (limitation of flexion-extension), IIB (limitation of pronation-supination) and IIC (limitation in both); and III, ankylosis. The Brooker classification23 originally described for HO around the hip is also used for the elbow: I, islands of bone within the soft tissue; II, bone spurs extending from proximal or distal to the joint but with > 1 cm between the opposing surfaces; III, bone spurs with < 1 cm between the nearest opposing ends; and IV, ankylosis.24
Functional scores
Multiple functional scores are reported for elbow function evaluation, such as American Shoulder and Elbow Surgeons-Elbow (ASES), Disabilities of the Arm, Shoulder and Hand Score (DASH), and Oxford Elbow Score.25,26 Among them, the Mayo Elbow Performance Index (MEPI), developed by Morrey27 in 1992, is most widely used,28 and includes elbow pain (45%), motion (20%), stability (10%), and daily function (25%; ability to comb hair, feed, perform personal hygiene tasks, on shirt and put on shoes), with a categorical rank of poor (0 to 59), fair (60 to 74), good (75 to 89), and excellent (90 to 100). Recently a new functional score, the Shanghai Elbow Dysfunction Score29 (SHEDS), comprising three portions: elbow motion capacities (48%, eight-item daily activity form), elbow-related symptoms (42%, pain, nerve function, strength, and stability), and patient satisfaction level (12%), is the first validated system for elbow stiffness, with good reliability, validity, and sensitivity. A minimal clinically important difference (MCID) of 15 points in MEPI was reported for rheumatoid arthritis after arthroplasty or synovectomy;30 however, to our knowledge, there is no MCID in any functional score for elbow stiffness.
Arthrolysis strategies
Time point
The timing of OEA is important. Too early likely causes HO recurrence, while too late poses risks such as progressive soft tissue fibrosis, exacerbation of neurological symptoms, and secondary cartilage degeneration. Garland31 suggested six months for limb trauma, one year for spinal cord injury, and 1.5 years for brain trauma. Generally, HO maturity requires three to six months1. One study found no significant difference in HO recurrence (p = 0.942) between early excision (mean six months after initial trauma) and control group (23 months).32 No significant differences with respect to ROM (p = 0.067), MEPI (p = 0.350), and complications (all p > 0.05) were found among early (six to ten months), median (11 to 20 months), and late ( > 20 months) release groups.33 Thus, if imaging shows maturity, and there are no symptoms like pain, swelling, or local tenderness, early arthrolysis can be performed within six to ten months.
Approach
There are several approaches for OEA, including anterior,34 posterior,35 lateral,20 and medial.36 The preferred approach depends on prior elbow incision, location, and extent of HO and need for ulnar nerve decompression. The anterior approach is not advocated due to the high risk of neurovascular injury. An isolated medial or lateral approach may not be sufficient for extensive HO. A single posterior or combined medial-lateral approach is most common. The posterior approach with elevated broad medial and lateral skin flaps can provide extensive surgical exposure through a single incision, but postoperative haematoma or seroma may develop due to the space under the flaps. Traction across the posterior wound during flexion may interfere with rehabilitation and even cause wound-healing complications. O’Driscoll37 advocates the combined medial-lateral approach to avoid haematoma and enable early postoperative exercises with fewer wound-healing problems. The combined approach is also supported by the Fan’s classification21 (depicted above), in which the lateral approach for anterior tethers and blocks, and medial approach for posterior tethers and blocks.
Release step
Generally, the factors affecting elbow mobility can be divided into tethers and blocks. Posterior tethers (e.g. thickened posterior capsule and contracted triceps) or anterior blocks (e.g. HO, free body in the radial fossa, and osteophyte around coronoid) can cause flexion loss. Similarly, anterior tethers or posterior blocks may cause extension deficiency. Release steps are generally similar for various kinds of PTES. For tethers, release and excision of scarred or ossified soft tissue in the anterior/posterior elbow is indicated in the lateral/medial approach; for blocks, clearing HO, scar, osteophyte, or loose body in the anterior/posterior elbow is recommended from a lateral/medial approach.21
Medially, the triceps is elevated off distal humerus, and the posterior bundles of medial collateral ligament are resected to expose the posterior elbow for debridement. The posterior capsule is resected if a contracture has formed as a posterior tether. Excision of HO and clearance of the olecranon fossa under direct visualization are performed to remove blocks. A 5 mm to 10 mm shortened olecranon tip osteotomy is performed when osteophytes have formed around the olecranon to achieve more extension. A pie-crusting triceps release (Figure 1, as a tether factor) is sometimes performed to improve flexion contracture.38
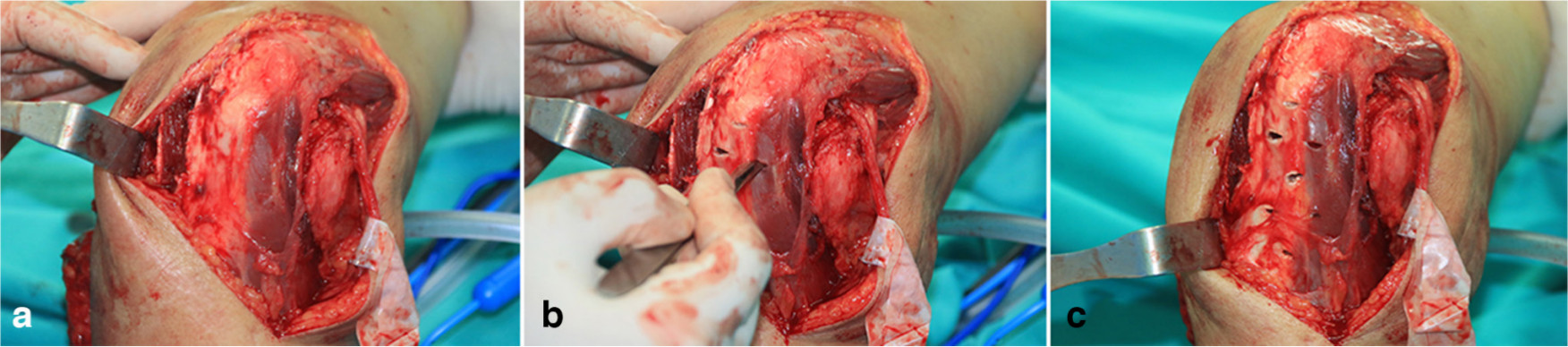
Fig. 1
Pie-crusting contracted triceps (tether release). Multiple stab incisions are made in the triceps tendon in the medial-to-lateral and distal-to-proximal directions via the medial approach.
Laterally, the extensor origins of brachioradialis and extensor carpi radialis longus are elevated from the lateral epicondyle to expose the anterior elbow for debridement. As an anterior tether, hypertrophic anterior capsule excision is performed. HO is excised (Figure 2, as a block factor), and the radio-humeral joint and coronoid fossa are cleared under direct visualization to remove blocks. If present, osteophytes on the tip of the coronoid are removed to improve flexion.
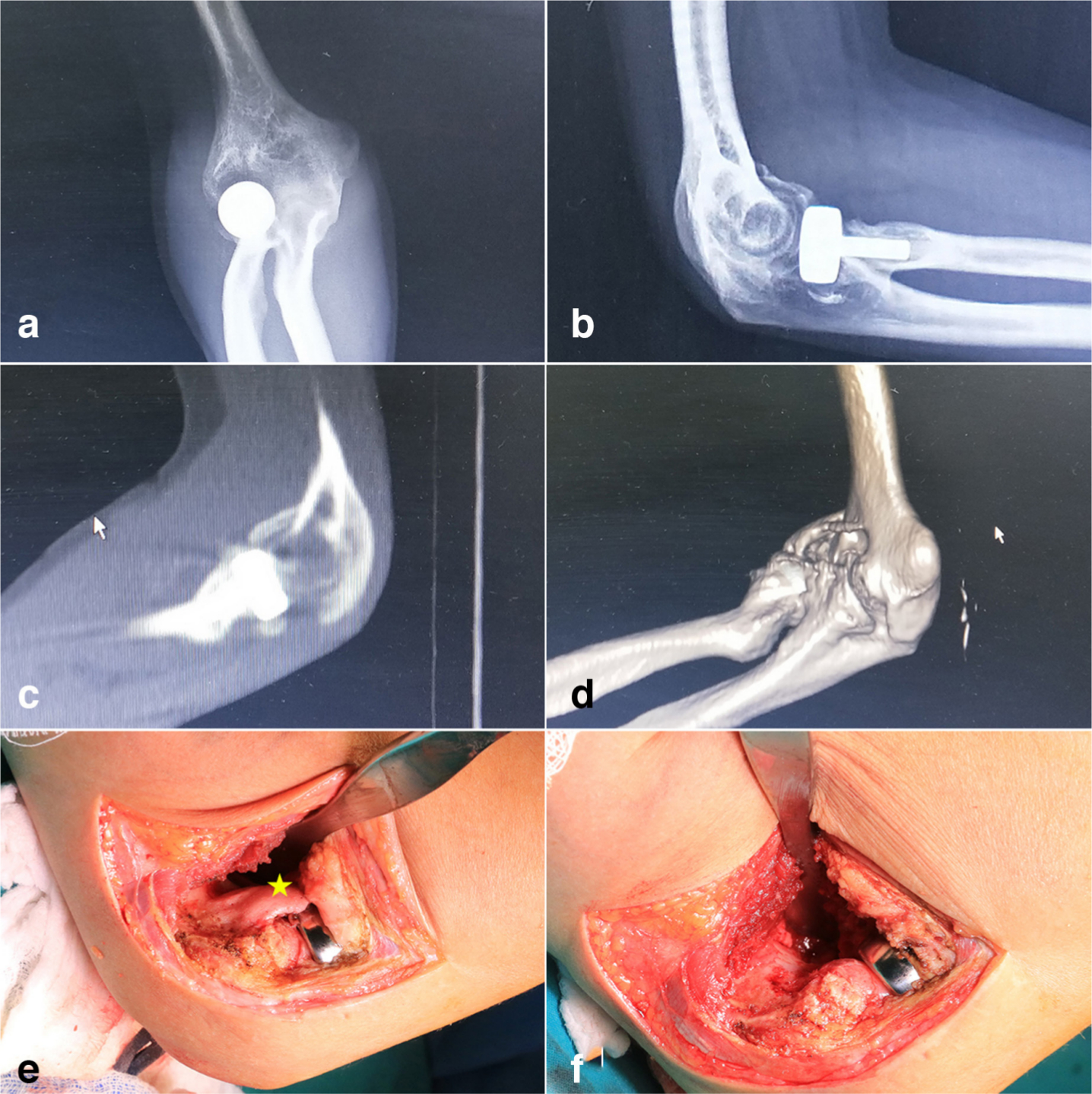
Fig. 2
Anterior ectopic bone excision (block removal). a,b) Radiograph, c) sagittal view of calculated tomography (CT), and d) 3D CT reconstruction show heterotopic ossification (HO) in the anterior elbow. e) An irregularly shaped HO (*, yellow) originated from distal humerus can be seen in the anterior elbow from the operative field. f) The ectopic bone is excised under direct visualization intraoperatively.
Rotational stiffness caused by an abnormal proximal radioulnar joint can be managed in the same OEA (Figure 3); otherwise, separate treatment is recommended, if the stiffness is caused by forearm interosseous membrane, distal radioulnar joint, and wrist joint. Scars and adhesions around the radial head and annular ligament are the primary causes, and contracture release is performed. Approximately half of the patients have rotational loss due to periradial head HO,39 which should be managed. Reconstruction is performed for radial head malunion or nonunion limiting rotation after elbow trauma, including prosthetic arthroplasty and head resection.40
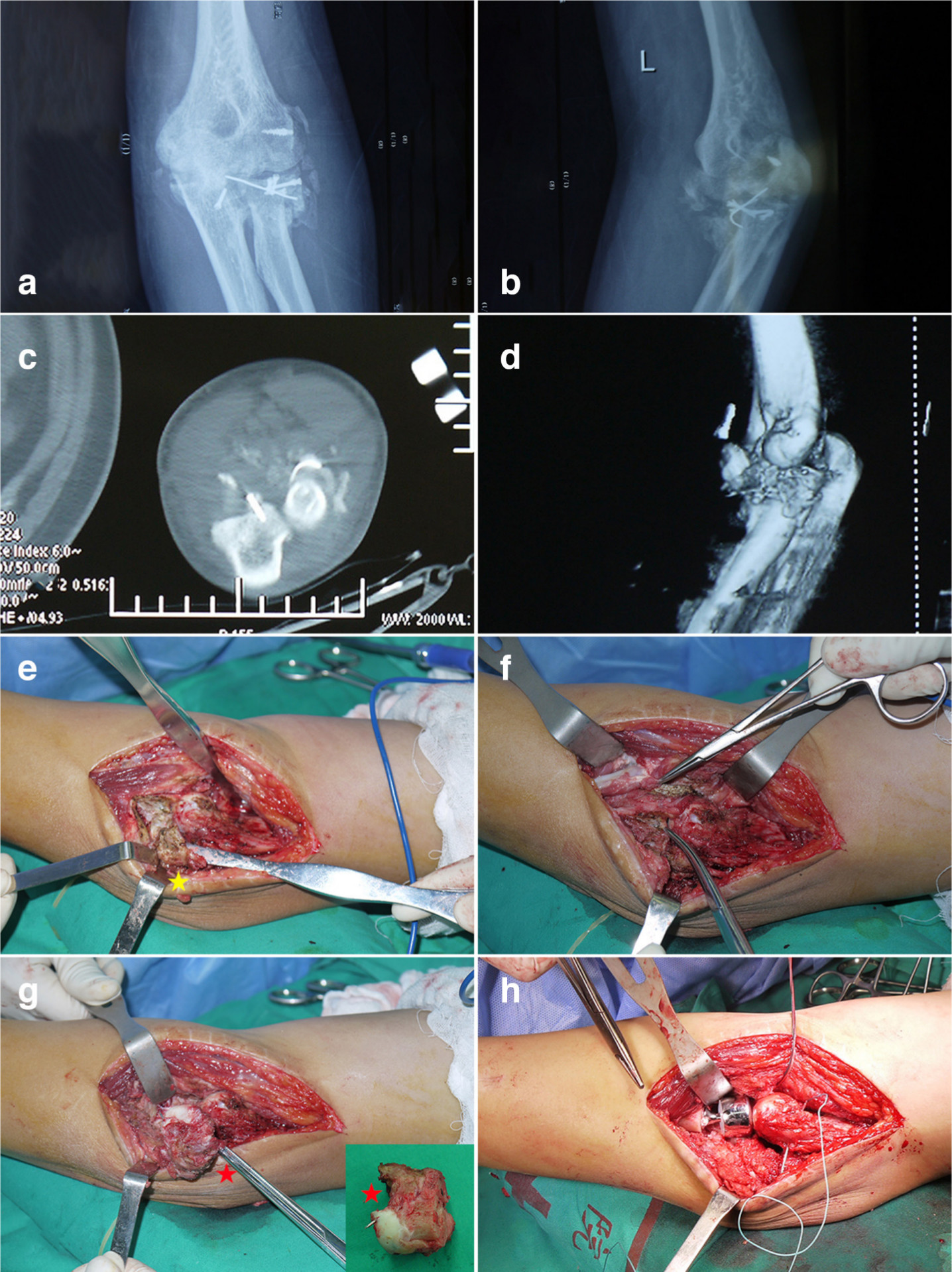
Fig. 3
Rotational function reconstruction. a, b) Radiograph, c) horizontal view of calculated tomography (CT), and d) 3D CT reconstruction show heterotopic ossification (HO) around the malformed radial head. e) An irregularly shaped HO (*, yellow) can be seen around the lateral side of annular ligament and radial head from the operative field, and f) is excised under direct visualization intraoperatively. g) The post-traumatic malformed radial head (*, red) can be seen from the operative field, and h) radial head arthroplasty is performed.
Outcomes
Figure 4 is an example of a 37-year-old woman with limited ROM after elbow trauma, who was treated by OEA and had regained ROM at follow-up. A systematic review involving 637 patients reported a mean preoperative and postoperative ROM after OEA of 52° and 103°, respectively, with an average increase of 51°.8Table I summarises OEA outcomes in the last five years (from 2016 to 2020), including (increased) ROM and FRA, and functional scores.21,41–54 To our knowledge, the largest case series of OEA in the English literature was in 2016 from the Shanghai Sixth People’s Hospital involving 260 patients.54 The mean ROM was 39° preoperatively and 117° at follow-up, with an increase of 78°. The clinical centre also reported medium-term outcomes ( > 5 years) of OEA with hinged external fixation for 49 severe PTES.47 Their satisfactory results showed significant improvements in ROM (from 27° preoperatively to 131° postoperatively), MEPI (54 to 95 points, 100% of good-excellent rate), and DASH (48 to 8 points). A novel technique, olecranon osteotomy-facilitated elbow release (OFER) procedure, was introduced in 35 patients; the mean ROM increased to 110°, with an improvement of 77°, and DASH score decreased to 11 points.50 However, almost of them were grade III and IV. In the future, high-level evidence-based clinical research is needed.
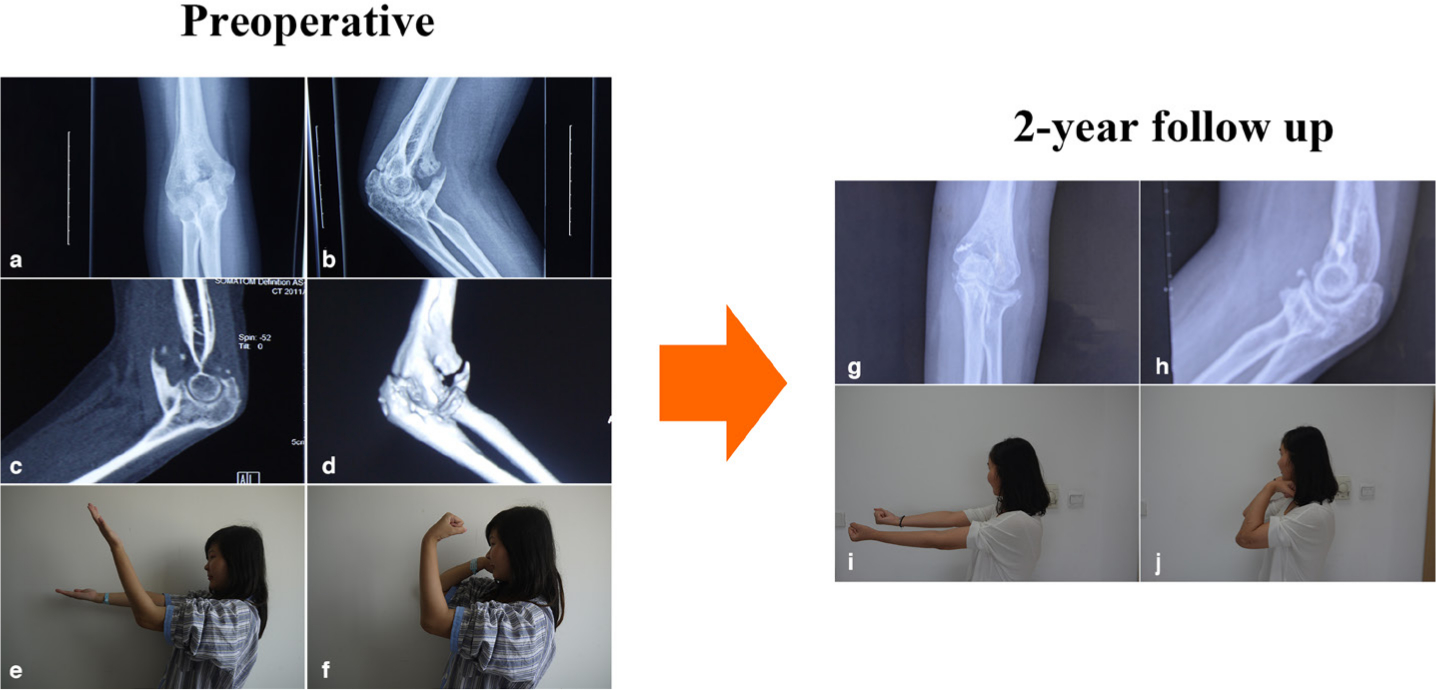
Fig. 4
An example of a 37-year-old woman with post-traumatic elbow stiffnes treated with open elbow arthrolysis. a, b) Preoperative radiograph, c) sagittal view of calculated tomography (CT), and d) 3D CT reconstruction showed massive heterotopic ossification around the elbow. Before arthrolysis, the range of movement (ROM) was 35°, with e) extension of 50° and f) flexion of 85°. g, h) Radiographs at two-year follow-up showed no obvious blocks around the elbow, and the ROM recovered to 130°, with i) extension of 0° and j) flexion of 130°.
Table I.
Reported outcomes following open elbow arthrolysis within the last five years.
| Author | Year | Journal | Patients, n | Age, yrs | FU, month | FU ROM, ° |
Increased ROM, ° |
FU FRA, ° |
Increased FRA, ° |
FU functional scores, points |
|---|---|---|---|---|---|---|---|---|---|---|
| Guglielmetti 41 | 2020 | J Shoulder Elbow Surg | 15 | 35 | 6 | 108 | 41 | 134 | 21 | MEPI: 77; DASH: 28 VAS: 3.9 |
| Freibott 42 | 2020 | J Shoulder Elbow Surg | 30 | 44 | 19 | 106 | 28 | 138 | 73 | N/A |
| Zhang 43 | 2020 | J Shoulder Elbow Surg | 61 | 40 | 27 | 112 | 84 | 154 | 46 | MEPI: 87 |
| Schemitsch 44 | 2020 | Injury | 42 | 47 | 54 | 96 | 33 | N/A | N/A | MEPI: 82, 77%*; DASH: 21 |
| Sun 21 | 2020 | J Shoulder Elbow Surg | 216 | 37 | 18 | 118 | 78 | 128 | 52 | MEPI: 91, 95%* VAS: 0.9 |
| Giannicola 45 | 2020 | J Shoulder Elbow Surg | 12 | 46 | 21 | 116 | 31 | 123 | 123 | MEPI: 89, 100%*; m-ASES: 83; quick-DASH: 19 |
| Kwak 46 | 2019 | J Shoulder Elbow Surg | 31 | 40 | 33 | 96 | 44 | N/A | N/A | MEPI: 80 VAS: 2.2 |
| Sun 47 | 2019 | Clin Orthop Relat Res | 49 | 36 | 69 | 131 | 104 | 145 | 30 | MEPI: 95, 100%*; DASH: 8 VAS: 0.4 |
| Brewley 48 | 2019 | J Shoulder Elbow Surg | 21 | 41 | 39 | 98 | 54 | N/A | N/A | MEPI: 84, 81%* |
| Haglin 49 | 2018 | J Shoulder Elbow Surg | 103 | 45 | 15 | 112 | 52 | 139 | 36 | N/A |
| Edwards 50 | 2017 | J Bone Joint Surg Am | 35 | 40 | 37 | 110 | 77 | N/A | N/A | DASH: 11 VAS: 1.4 |
| Gundes 51 | 2017 | Acta Orthop Traumatol Turc | 77 | 35 | 44 | 110 | 65 | 180 | 10 | MEPI: 85 |
| Kruse 52 | 2016 | J Shoulder Elbow Surg | 36 | 39 | 38 | 109 | 57 | N/A | N/A | MEPI: 91 VAS: 0.4 |
| Pettersen 53 | 2016 | BMC Musculoskelet Disord | 43 | 47 | 41 | 106 | 56 | 139 | 19 | MEPI: 85; quick-DASH: 20 |
| Cai 54 | 2016 | J Shoulder Elbow Surg | 260 | 37 | 14 | 117 | 78 | N/A | N/A | N/A |
-
*
Excellent-good rate of MEPI
-
DASH, Disability of Arm Shoulder and Hand Questionnaire; FRA, forearm rotational arc; FU, follow-up; m-ASES, modified American Shoulder and Elbow Surgeons score; MEPI, Mayo Elbow Performance Index; N/A, not available; ROM, range of movement; VAS, visual analogue score.
Good efficacy can also be achieved in patients with flexion-extension or rotation ankylosis. Massachusetts General Hospital evaluated 18 patients who had surgical release of complete bony ankylosis and found an average increase of 95° in ROM.55 The mean Broberg and Morrey scores were 81 points, with a good-excellent rate of 61%. Shanghai Sixth People’s Hospital showed a mean improvement of 112° in 41 patients.56 The mean MEPI were 84 points and the good-excellent rate is 83%. Sapienza University of Rome reported 12 patients with proximal radioulnar synostosis who underwent surgical resection, and found an average increase of 123° in FRA, with 89 points of MEPI and 100% of good-excellent rate.45
OEA can effectively reduce elbow pain.21,46,47,50,57 In 81 patients from the Glasgow Royal Infirmary, the visual analogue score (VAS) decreased from 2.0 points preoperatively to 1.0 point at follow-up,57 which was similar to the results from the Shanghai Sixth People’s Hospital.21 The medium-term outcomes also showed a mean VAS of 2.5 points pre-operatively and 0.4 points at follow-up.47 Life qualities also improve significantly, as per the increased 36- Item Short Form Survey (SF-36).21,47,58
Nerve management
Proper nerve management is vital during OEA. The ulnar nerve is prone to elongation, and is at high risk for dysfunction due to reasons such as increased elbow flexion after OEA; therefore, most authors advocate routine exposure and release in the medial approach. However, whether anterior transposition of the ulnar nerve should be performed remains controversial. Some authors suggest keeping it in-situ to protect the concomitant vessels and reduce nerve stimulation and surgery time.59 A study found that ulnar nerve function (Amadio score: 8.22 points, ulnar nerve symptoms: 8.1%) in the anterior subcutaneous transposition group was significantly better than that in the simple decompression group (7.62 points and 18.9%) after OEA; the authors recommend anterior transposition in patients with preoperative ulnar nerve symptoms or preoperative flexion < 100°.60 Additionally, radial nerve exploration and release is necessary when the patient has severe extension deformity, long disease duration, childhood injury, extensive anterolateral HO, or preoperative symptoms. The posterior interosseous nerve should be explored and protected when manipulating the radiohumeral and proximal radioulnar joint.
Internal fixator
The implant can be removed only if the time interval between the previous fixation and the index procedure is long enough to allow fracture union, and the preoperative radiographs and clinical symptoms show solid fracture union. To avoid iatrogenic fracture, the principle of “release first, removal next” (i.e. implant removal after complete release) should be followed.
Hinged external fixation
It remains controversial whether using hinged external fixation after OEA is effective. In a retrospective study of 42 patients with ROM ≤ 40°, the average ROM gain was 11° higher in patients treated with a hinge than those without;61 another study including 26 patients with very severe stiffness found an improvement in mean ROM from 16° preoperatively to 102° at follow-up.62 External fixation application has several advantages: maintaining elbow instability after complete release, protecting repaired collateral ligament, and fixing the elbow at the maximum flexion and extension positions to maintain the release effect and facilitate postoperative rehabilitation. A recent study selected the radial facet of the distal radius instead of the traditional middle ulna for distal pins.63 The authors stated that this procedure can reduce the incidence of iatrogenic fracture during passive manipulation in rehabilitation as the distal radius is much thicker and stronger than the middle ulna. No broken ulna or radius was reported in their study. Along with daily rotation exercise, the final rotation recovery was not influenced, with a mean ROM of 126° and FRA of 153°.
Postoperative rehabilitation
Postoperative rehabilitation is aimed at preserving ROM obtained in surgery to achieve a satisfactory final outcome. Early mobilization after arthrolysis is important and the rehabilitation is routinely started on the first postoperative day. Splinting, continuous passive motion (CPM), and external fixation are the three popular selections.
Splinting
Stretching produces plastic elongation of contracted tissue, which is based on viscoelastic properties of soft tissue including creep and stress relaxation.64 The two main types are static progressive and dynamic splints. Previous studies have demonstrated no significant difference between the two protocols for PTES.65 However, static progressive splinting is preferred for better toleration and shorter utilization periods; moreover, dynamic splinting is more likely to cause inflammation.66 Generally, a three to four month period of splinting is enough, but adjustment is necessary for individual.
Continuous passive motion
The application of CPM device reduces intra-articular bleeding and periarticular oedema through a sinusoidal change of intra- and periarticular pressure;67 however, its efficacy is still controversial. In one compared cohort of patients who received CPM device after elbow arthrolysis versus those that did not use, no differences in ROM (p = 0.56) and MEPI (p = 0.29) were found.68 This fact, plus changes in length of hospital stay, limited availability of portable machines and their difficulty of use, and problems with reimbursement, have restricted CPM application.
External fixation
The advantages and effectiveness of external fixation have been introduced in the preceding paragraph. Shanghai Sixth People’s Hospital has introduced a three-step rehabilitation programme for external fixation after elbow arthrolysis.47 In the first postoperative six weeks, patients are instructed to perform “active, assisted and passive” cycles of flexion-extension exercises (30 on the first day, increased by 30 per day until 300 were achieved) and forearm rotation exercises (at least twice daily) under close supervision by physical therapist or family members. The fixator is locked at the extreme position of elbow extension or flexion after each session of ROM exercise as well as in sleep. Generally, fixator removal is performed at six weeks in the outpatient operating room.
Prevention of complications
The complication rate of OEA is approximately 23%.8 The complications most reported are new-onset or exacerbated ulnar nerve symptoms, HO recurrence, and postoperative infection. Compared to treatment, prevention is key to reduce complications.
Ulnar nerve symptoms
Iatrogenic injury during surgery, increased nerve length, and intraneural pressure associated with improved ROM after OEA increase the risk of neuropathy and nerve palsy.69 Prophylactic ulnar nerve decompression and transposition are indicated in cases of severe preoperative flexion deficiency. Careful release, blood vessel protection, and reduction of nerve stimulation during OEA are also important. One study reported 5% new-onset ulnar nerve symptoms without exacerbation after routine transposition during OEA; the authors also revealed that preoperative HO was an independent risk factor, especially on the medial side.54
HO recurrence
Recurrent HO is the main reason for failed arthrolysis. Non-steroidal anti-inflammatory drugs (NSAIDs) and radiotherapy help prevent HO formation. The mechanism of NSAIDs is attenuating the bone morphogenetic pathway and reducing local inflammatory responses, and the commonest drug used is indomethacin.70 Celecoxib, a selective cyclo-oxygenase-2 inhibitor, can also effectively inhibit HO formation after OEA.71 It has gained popularity because of the lower incidence of gastrointestinal side effects, while having similar efficacy as indomethacin.70 Radiation can suppress the pluripotent mesenchymal cell from transforming into osteoprogenitor cells and osteoblasts.72 However, the overall effects of radiotherapy remain controversial and are supported by weak evidence:73 the only randomized controlled trial was terminated before completion because of unacceptably high numbers of adverse events; the only case-control study showed no efficacy; and only a few case series and reports showed positive results.
Post-operative infection
Long operation time, large surgical field, and local haematoma or seroma that may be inaccessible to systemically administered antibiotics, increase risk for infection. Local antibiotic delivery is suitable for wound infection prophylaxis because high concentrations are achieved directly at the wound site and systemic toxicity is limited.74 One study found that local application of vancomycin powder can significantly decrease the infection rate following OEA (0% vs 6.5%, p = 0.003); no adverse effects were documented, showing a promising means to prevent post-OEA infection.75
Summary
OEA can yield sustained improvement in elbow mobility, function, pain relief, and life quality. A clear understanding of the complete diagnosis and treatment path of OEA is paramount to achieving optimal results, from diagnosis, evaluation, operation, rehabilitation to prevention. Future research will need to focus on high-quality clinical evidence of treatment method and rehabilitation programmes.
References
1. Ranganathan K , Loder S , Agarwal S , et al. Heterotopic ossification: Basic-Science principles and clinical correlates . J Bone Joint Surg Am . 2015 ; 97-A ( 13 ): 1101 – 1111 . Crossref PubMed Google Scholar
2. Doornberg JN , Bosse T , Cohen MS , Jupiter JB , Ring D , Kloen P . Temporary presence of myofibroblasts in human elbow capsule after trauma . J Bone Joint Surg Am . 2014 ; 96-A ( 5 ): e36 – 1 . Crossref PubMed Google Scholar
3. Morrey BF , Askew LJ , Chao EY . A biomechanical study of normal functional elbow motion . J Bone Joint Surg Am . 1981 ; 63-A ( 6 ): 872 – 877 . PubMed Google Scholar
4. Lindenhovius ALC , Doornberg JN , Brouwer KM , Jupiter JB , Mudgal CS , Ring D . A prospective randomized controlled trial of dynamic versus static progressive elbow splinting for posttraumatic elbow stiffness . J Bone Joint Surg Am . 2012 ; 94-A ( 8 ): 694 – 700 . Crossref PubMed Google Scholar
5. Jupiter JB , O'Driscoll SW , Cohen MS . The assessment and management of the stiff elbow . Instr Course Lect . 2003 ; 52 : 93 – 111 . PubMed Google Scholar
6. Iyidobi EC , Nwadinigwe CU , Ekwunife RT , et al. Early outcome after the use of the triceps fascia flap in interposition elbow arthroplasty: a novel method in the treatment of post-traumatic elbow stiffness . Sicot J . 2020 ; 6 : 8 . Crossref PubMed Google Scholar
7. Wilson PD . Capsulectomy for the relief of flexion contractures of the elbow following fracture. 1944 . Clin Orthop Relat Res . 2000 ; 1 ( 370 ): 71 – 86 . Crossref PubMed Google Scholar
8. Kodde IF , van Rijn J , van den Bekerom MPJ , Eygendaal D . Surgical treatment of post-traumatic elbow stiffness: a systematic review . J Shoulder Elbow Surg . 2013 ; 22 ( 4 ): 574 – 580 . Crossref PubMed Google Scholar
9. Lee EK , Namdari S , Hosalkar HS , Keenan MA , Baldwin KD . Clinical results of the excision of heterotopic bone around the elbow: a systematic review . J Shoulder Elbow Surg . 2013 ; 22 ( 5 ): 716 – 722 . Crossref PubMed Google Scholar
10. Attum B , Obremskey W . Posttraumatic elbow stiffness: a critical analysis review . JBJS Rev . 2016 ; 4 ( 9 ): 4 – 9 . Crossref PubMed Google Scholar
11. . In : Morrey BF , Sanchez-Sotelo J , Moorey ME . Morrey's the elbow and its disorders . Fifth edition . Amsterdam : Elsevier , 2018 . Google Scholar
12. Sardelli M , Tashjian RZ , MacWilliams BA . Functional elbow range of motion for contemporary tasks . J Bone Joint Surg Am . 2011 ; 93-A ( 5 ): 471 – 477 . Crossref PubMed Google Scholar
13. Sojbjerg JO . The stiff elbow . Acta Orthop Scand . 1996 ; 6 : 626 – 631 . Crossref PubMed Google Scholar
14. Chapleau J , Canet F , Petit Y , Laflamme G-Y , Rouleau DM . Validity of goniometric elbow measurements: comparative study with a radiographic method . Clin Orthop Relat Res . 2011 ; 469 ( 11 ): 3134 – 3140 . Crossref PubMed Google Scholar
15. Zdravkovic V , Jost B . Rounded data have a high potential for false comparative statistical results as shown with elbow Arc of motion . J Shoulder Elbow Surg . 2018 ; 27 ( 2 ): 276 – 281 . Crossref PubMed Google Scholar
16. Bachman DR , Kamaci S , Thaveepunsan S , Park SE , Vasileiadis GI , O'Driscoll SW . Preoperative nerve imaging using computed tomography in patients with heterotopic ossification of the elbow . J Shoulder Elbow Surg . 2015 ; 24 ( 7 ): 1149 – 1155 . Crossref PubMed Google Scholar
17. Ploumis A , Donovan JM , Olurinde MO , et al. Association between alendronate, serum alkaline phosphatase level, and heterotopic ossification in individuals with spinal cord injury . J Spinal Cord Med . 2015 ; 38 ( 2 ): 193 – 198 . Crossref PubMed Google Scholar
18. Eberlin KR , Marjoua Y , Jupiter JB . Compressive neuropathy of the ulnar nerve: a perspective on history and current controversies . J Hand Surg Am . 2017 ; 42-A ( 6 ): 464 – 469 . Crossref PubMed Google Scholar
19. Morrey BF . Post-Traumatic contracture of the elbow. operative treatment, including distraction arthroplasty . J Bone Joint Surg Am . 1990 ; 72-A ( 4 ): 601 – 618 . PubMed Google Scholar
20. Mansat P , Morrey BF . The column procedure: a limited lateral approach for extrinsic contracture of the elbow . J Bone Joint Surg Am . 1998 ; 11-A : 1603 – 1615 . PubMed Google Scholar
21. Sun Z , Li J , Cui H , Ruan H , Wang W , Fan C . A new pathologic classification for elbow stiffness based on our experience in 216 patients . J Shoulder Elbow Surg . 2020 ; 29 ( 3 ): e75 – e86 . Google Scholar
22. Hastings H , Graham TJ . The classification and treatment of heterotopic ossification about the elbow and forearm . Hand Clin . 1994 ; 10 ( 3 ): 417 – 437 . PubMed Google Scholar
23. Brooker AF , Bowerman JW , Robinson RA , Riley LH . Ectopic ossification following total hip replacement. incidence and a method of classification . J Bone Joint Surg Am . 1973 ; 55-A ( 8 ): 1629 – 1632 . PubMed Google Scholar
24. Robinson PM , MacInnes SJ , Stanley D , Ali AA . Heterotopic ossification following total elbow arthroplasty: a comparison of the incidence following elective and trauma surgery . Bone Joint J . 2018 ; 100-B ( 6 ): 767 – 771 . Crossref PubMed Google Scholar
25. Longo UG , Franceschi F , Loppini M , Maffulli N , Denaro V . Rating systems for evaluation of the elbow . Br Med Bull . 2008 ; 87 : 131 – 161 . Crossref PubMed Google Scholar
26. Smith MV , Calfee RP , Baumgarten KM , Brophy RH , Wright RW . Upper extremity-specific measures of disability and outcomes in orthopaedic surgery . J Bone Joint Surg Am . 2012 ; 94-A ( 3 ): 277 – 285 . Crossref PubMed Google Scholar
27. Morrey BF , Adams RA . Semiconstrained arthroplasty for the treatment of rheumatoid arthritis of the elbow . J Bone Joint Surg Am . 1992 ; 74-A ( 4 ): 479 – 490 . PubMed Google Scholar
28. Evans JP , Smith CD , Fine NF , et al. Clinical rating systems in elbow research-a systematic review exploring trends and distributions of use . J Shoulder Elbow Surg . 2018 ; 27 ( 4 ): e98 – e106 . Crossref PubMed Google Scholar
29. Sun Z , Liu W , Wang W , Fan C . Development and validation of a new elbow-specific scoring system for patients with elbow stiffness: the Shanghai elbow dysfunction score . J Shoulder Elbow Surg . 2019 ; 28 ( 2 ): 296 – 303 . Crossref PubMed Google Scholar
30. de Boer YA , Hazes JM , Winia PC , Brand R , Rozing PM . Comparative responsiveness of four elbow scoring instruments in patients with rheumatoid arthritis . J Rheumatol . 2001 ; 28 ( 12 ): 2616 – 2623 . PubMed Google Scholar
31. Garland DE . A clinical perspective on common forms of acquired heterotopic ossification . Clin Orthop Relat Res . 1991 ; 263 : 13 – 29 . PubMed Google Scholar
32. Chen S , Yu S-yang , Yan H , et al. The time point in surgical excision of heterotopic ossification of post-traumatic stiff elbow: recommendation for early excision followed by early exercise . J Shoulder Elbow Surg . 2015 ; 24 ( 8 ): 1165 – 1171 . Crossref PubMed Google Scholar
33. Sun Z , Cui H , Liang J , Li J , Wang X , Fan C . Determining the effective timing of an open arthrolysis for post-traumatic elbow stiffness: a retrospective cohort study . BMC Musculoskelet Disord . 2019 ; 20 ( 1 ): 122 . Crossref PubMed Google Scholar
34. Aldridge JM , Atkins TA , Gunneson EE , Urbaniak JR . Anterior release of the elbow for extension loss . J Bone Joint Surg Am . 2004 ; 86-A ( 9 ): 1955 – 1960 . Crossref PubMed Google Scholar
35. Bryan RS , Morrey BF . Extensive posterior exposure of the elbow. A triceps-sparing approach . Clin Orthop Relat Res . 1982 ; 166 : 188 – 192 . PubMed Google Scholar
36. Kasparyan NG , Hotchkiss RN . Dynamic skeletal fixation in the upper extremity . Hand Clin . 1997 ; 13 ( 4 ): 643 – 663 . PubMed Google Scholar
37. Bachman DR , Fitzsimmons JS , O'Driscoll SW . Safety of arthroscopic versus open or combined heterotopic ossification removal around the elbow . Arthroscopy . 2020 ; 36 ( 2 ): 422 – 430 . Crossref PubMed Google Scholar
38. Wang W , Zhan Y-lin , Yu S-yang , Zheng X-you , Liu S , Fan C-yi . Open arthrolysis with pie-crusting release of the triceps tendon for treating post-traumatic contracture of the elbow . J Shoulder Elbow Surg . 2016 ; 25 ( 5 ): 816 – 822 . Crossref PubMed Google Scholar
39. Vasileiadis GI , Ramazanian T , Kamaci S , et al. Loss of pronation-supination in patients with heterotopic ossification around the elbow . J Shoulder Elbow Surg . 2019 ; 28 ( 7 ): 1406 – 1410 . Crossref PubMed Google Scholar
40. Yu S-yang , Yan H-de , Ruan H-jiang , Wang W , Fan C-yi . Comparative study of radial head resection and prosthetic replacement in surgical release of stiff elbows . Int Orthop . 2015 ; 39 ( 1 ): 73 – 79 . Crossref PubMed Google Scholar
41. Guglielmetti CLB , Gracitelli MEC , Assunção JH , et al. Randomized trial for the treatment of post-traumatic elbow stiffness: surgical release vs. rehabilitation . J Shoulder Elbow Surg . 2020 ; 29 ( 8 ): 1522 – 1529 . Crossref PubMed Google Scholar
42. Freibott CE , Bäcker HC , Shoap SC , Tedesco LJ , Galle SE , Rosenwasser MP . Treatment methods for post-traumatic elbow stiffness caused by heterotopic ossification . J Shoulder Elbow Surg . 2020 ; 29 ( 7 ): 1380 – 1386 . Crossref PubMed Google Scholar
43. Zhang B , Zhang W , Xu J , Ding J . Effect of topical tranexamic acid on post-traumatic elbow stiffness in patients treated with open arthrolysis: a prospective comparative study . J Shoulder Elbow Surg . 2020 ; 29 ( 7 ): 1375 – 1379 . Crossref PubMed Google Scholar
44. Schemitsch C , Seeto B , Rubinger L , Vicente M , Schemitsch E , McKee M . Functional outcome following elbow release and hardware removal after bicolumnar fixation of distal humeral fractures . Injury . 2020 ; 51 ( 7 ): 1592 – 1596 . Crossref PubMed Google Scholar
45. Giannicola G , Spinello P , Villani C , Cinotti G . Post-Traumatic proximal radioulnar Synostosis: results of surgical treatment and review of the literature . J Shoulder Elbow Surg . 2020 ; 29 ( 2 ): 329 – 339 . Crossref PubMed Google Scholar
46. Kwak J-M , Sun Y , Kholinne E , Koh K-H , Jeon I-H . Surgical outcomes for post-traumatic stiffness after elbow fracture: comparison between open and arthroscopic procedures for intra- and extra-articular elbow fractures . J Shoulder Elbow Surg . 2019 ; 28 ( 10 ): 1998 – 2006 . Crossref PubMed Google Scholar
47. Sun Z , Cui H , Ruan J , Li J , Wang W , Fan C . What range of motion and functional results can be expected after open Arthrolysis with hinged external fixation for severe posttraumatic elbow stiffness? Clin Orthop Relat Res . 2019 ; 477 ( 10 ): 2319 – 2328 . Crossref PubMed Google Scholar
48. Brewley EE , Gorman RA , Christmas KN , Simon P , Chapel RJ , Mighell MA . Use of a modified Outerbridge-Kashiwagi procedure for the treatment of posttraumatic elbow sequelae . J Shoulder Elbow Surg . 2019 ; 28 ( 7 ): 1387 – 1394 . Crossref PubMed Google Scholar
49. Haglin JM , Kugelman DN , Christiano A , Konda SR , Paksima N , Egol KA . Open surgical elbow contracture release after trauma: results and recommendations . J Shoulder Elbow Surg . 2018 ; 27 ( 3 ): 418 – 426 . Crossref PubMed Google Scholar
50. Edwards SG , Rhodes DA , Jordan TW , Sietsema DL . The olecranon Osteotomy-Facilitated elbow release (OFER) . J Bone Joint Surg Am . 2017 ; 99-A ( 21 ): 1859 – 1865 . Crossref PubMed Google Scholar
51. Gundes H , Selek Özgür , Gok U , Gumuslu B , Buluc L . The relation between elbow range of motion and patient satisfaction after open release of stiff elbow . Acta Orthop Traumatol Turc . 2017 ; 51 ( 4 ): 303 – 307 . Crossref PubMed Google Scholar
52. Kruse KK , Papatheodorou LK , Weiser RW , Sotereanos DG . Release of the stiff elbow with mini-open technique . J Shoulder Elbow Surg . 2016 ; 25 ( 3 ): 355 – 361 . Crossref PubMed Google Scholar
53. Pettersen PM , Eriksson J , Bratberg H , et al. Increased rom and high patient satisfaction after open arthrolysis: a follow-up-study of 43 patients with posttraumatic stiff elbows . BMC Musculoskelet Disord . 2016 ; 17 : 74 . Crossref PubMed Google Scholar
54. Cai J , Zhou Y , Chen S , et al. Ulnar neuritis after open elbow arthrolysis combined with ulnar nerve subcutaneous transposition for post-traumatic elbow stiffness: outcome and risk factors . J Shoulder Elbow Surg . 2016 ; 25 ( 6 ): 1027 – 1033 . Crossref PubMed Google Scholar
55. Brouwer KM , Lindenhovius ALC , de Witte PB , Jupiter JB , Ring D . Resection of heterotopic ossification of the elbow: a comparison of Ankylosis and partial restriction . J Hand Surg Am . 2010 ; 35-A ( 7 ): 1115 – 1119 . Crossref PubMed Google Scholar
56. Chen S , Liu J , Cai J , et al. Results and outcome predictors after open release of complete Ankylosis of the elbow caused by heterotopic ossification . Int Orthop . 2017 ; 41 ( 8 ): 1627 – 1632 . Crossref PubMed Google Scholar
57. Higgs ZCJ , Danks BA , Sibinski M , Rymaszewski LA . Outcomes of open arthrolysis of the elbow without post-operative passive stretching . J Bone Joint Surg Br . 2012 ; 94 ( 3 ): 348 – 352 . Crossref PubMed Google Scholar
58. Lindenhovius ALC , Doornberg JN , Ring D , Jupiter JB . Health status after open elbow contracture release . J Bone Joint Surg Am . 2010 ; 92-A ( 12 ): 2187 – 2195 . Crossref PubMed Google Scholar
59. Chen NC , Liu A . The role of prophylactic ulnar nerve release during elbow contracture release . J Hand Surg Am . 2014 ; 39-A ( 9 ): 1837 – 1839 . Crossref PubMed Google Scholar
60. Shuai C , Hede Y , Shen L , Yuanming O , Hongjiang R , Cunyi F . Is routine ulnar nerve transposition necessary in open release of stiff elbows? our experience and a literature review . Int Orthop . 2014 ; 38 ( 11 ): 2289 – 2294 . Crossref PubMed Google Scholar
61. Ring D , Hotchkiss RN , Guss D , Jupiter JB . Hinged elbow external fixation for severe elbow contracture . J Bone Joint Surg Am . 2005 ; 87-A ( 6 ): 1293 – 1296 . Crossref PubMed Google Scholar
62. Kulkarni GS , Kulkarni VS , Shyam AK , Kulkarni RM , Kulkarni MG , Nayak P . Management of severe extra-articular contracture of the elbow by open arthrolysis and a monolateral hinged external fixator . J Bone Joint Surg Br . 2010 ; 92-B ( 1 ): 92 – 97 . Crossref PubMed Google Scholar
63. Zhou Y , Cai J-Y , Chen S , Liu S , Wang W , Fan C-Y . Application of distal radius-positioned hinged external fixator in complete open release for severe elbow stiffness . J Shoulder Elbow Surg . 2017 ; 26 ( 2 ): e44 – e51 . Crossref PubMed Google Scholar
64. Fusaro I , Orsini S , Sforza T , Rotini R , Benedetti MG . The use of braces in the rehabilitation treatment of the post-traumatic elbow . Joints . 2014 ; 2 : 81 – 86 . Crossref PubMed Google Scholar
65. Veltman ES , Doornberg JN , Eygendaal D , van den Bekerom MPJ . Static progressive versus dynamic splinting for posttraumatic elbow stiffness: a systematic review of 232 patients . Arch Orthop Trauma Surg . 2015 ; 135 ( 5 ): 613 – 617 . Crossref PubMed Google Scholar
66. Marinelli A , Bettelli G , Guerra E , Nigrisoli M , Rotini R . Mobilization brace in post-traumatic elbow stiffness . Musculoskelet Surg . 2010 ; 94 Suppl 1 ( Suppl 1 ): 37 – 45 . Crossref PubMed Google Scholar
67. O'Driscoll SW , Giori NJ . Continuous passive motion (CPM): theory and principles of clinical application . J Rehabil Res Dev . 2000 ; 37 ( 2 ): 179 – 188 . PubMed Google Scholar
68. Lindenhovius ALC , van de Luijtgaarden K , Ring D , Jupiter J . Open elbow contracture release: postoperative management with and without continuous passive motion . J Hand Surg Am . 2009 ; 34-A ( 5 ): 858 – 865 . Crossref PubMed Google Scholar
69. Keener JD , Galatz LM . Arthroscopic management of the stiff elbow . American Academy of Orthopaedic Surgeon . 2011 ; 19 ( 5 ): 265 – 274 . Crossref PubMed Google Scholar
70. Joice M , Vasileiadis GI , Amanatullah DF . Non-Steroidal anti-inflammatory drugs for heterotopic ossification prophylaxis after total hip arthroplasty: a systematic review and meta-analysis . Bone Joint J . 2018 ; 100-B ( 7 ): 915 – 922 . Crossref PubMed Google Scholar
71. Sun Y , Cai J , Li F , Liu S , Ruan H , Fan C . The efficacy of celecoxib in preventing heterotopic ossification recurrence after open arthrolysis for post-traumatic elbow stiffness in adults . J Shoulder Elbow Surg . 2015 ; 24 ( 11 ): 1735 – 1740 . Crossref PubMed Google Scholar
72. Balboni TA , Gobezie R , Mamon HJ . Heterotopic ossification: pathophysiology, clinical features, and the role of radiotherapy for prophylaxis . Int J Radiat Oncol Biol Phys . 2006 ; 65 ( 5 ): 1289 – 1299 . Crossref PubMed Google Scholar
73. Ploumis A , Belbasis L , Ntzani E , Tsekeris P , Xenakis T . Radiotherapy for prevention of heterotopic ossification of the elbow: a systematic review of the literature . J Shoulder Elbow Surg . 2013 ; 22 ( 11 ): 1580 – 1588 . Crossref PubMed Google Scholar
74. Carver DC , Kuehn SB , Weinlein JC . Role of systemic and local antibiotics in the treatment of open fractures . Orthop Clin North Am . 2017 ; 48 ( 2 ): 137 – 153 . Crossref PubMed Google Scholar
75. Yan H , He J , Chen S , Yu S , Fan C . Intrawound application of vancomycin reduces wound infection after open release of post-traumatic stiff elbows: a retrospective comparative study . J Shoulder Elbow Surg . 2014 ; 23 ( 5 ): 686 – 692 . Crossref PubMed Google Scholar
Author contributions
Z. Sun: Conceptualized the study, Conducted the investigation, Administered the project, Collected the data, Wrote, reviewed, and edited the manuscript.
W. Liu: Conducted the investigation, Administered the project, Collected the data, Wrote, reviewed, and edited the manuscript.
J. Li: Conceptualized the study, Collected the data, Wrote, reviewed, and edited the manuscript.
C. Fan: Conceptualized the study, Acquired the funding, Administered the project, Supervised the study, Reviewed and edited the manuscript.
Z. Sun, W. Liu and J. Li contributed equally to this work.
Funding statement
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.This study was supported by Key Project of National Natural Science Foundation of China (81830076); United Project of Municipal Hospitals Emerging Frontier Technology of Shanghai Hospital Development Center (SHDC12018130); Project of Health Industry Special of Shanghai Pudong New Area Health and Family Planning Commission (PW2018B-01); Project of Key Discipline Group of Shanghai Pudong New Area Health and Family Planning Commission (PWZxq2017-03).
ICMJE COI statement
The authors, their immediate families, and any research foundation with which they are affiliated have not received any financial payments or other benefits from any commercial entity related to the subject of this article.
Acknowledgements
The authors would like to thank the personnel from the Elbow Dysfunction Treatment Team, led by Prof. Cunyi Fan, for participating in the discussion of this project.
© 2020 Author(s) et al. This is an open-access article distributed under the terms of the Creative Commons Attributions licence (CC-BY-NC-ND), which permits unrestricted use, distribution, and reproduction in any medium, but not for commercial gain, provided the original author and source are credited.









