Abstract
Aims
Our rural orthopaedic service has undergone service restructure during the COVID-19 pandemic in order to sustain hip fracture care. All adult trauma care has been centralised to the Royal Shrewsbury Hospital for assessment and medical input, before transferring those requiring operative intervention to the Robert Jones and Agnes Hunt Orthopaedic Hospital. We aim to review the impact of COVID-19 on hip fracture workload and service changes upon management of hip fractures.
Methods
We reviewed our prospectively maintained trust database and National Hip Fracture Database records for the months of March and April between the years 2016 and 2020. Our assessment included fracture pattern (intrascapular vs extracapsular hip fracture), treatment intervention, length of stay and mortality.
Results
We treated 288 patients during March and April between 2016 and 2020, with a breakdown of 55, 58, 53, 68, and 54 from 2016 to 2020 respectively. Fracture pattern distribution in the pre-COVID-19 years of 2016 to 2019 was 58% intracapsular and 42% extracapsular. In 2020 (COVID-19 period) the fracture patterns were 65% intracapsular and 35% extracapsular. Our mean length of stay was 13.1 days (SD 8.2) between 2016 to 2019, and 5.0 days (6.3) days in 2020 (p < 0.001). Between 2016 and 2019 we had three deaths in hip fracture patients, and one death in 2020. Hemiarthroplasty and dynamic hip screw fixation have been the mainstay of operative intervention across the five years and this has continued in the COVID-19 period. We have experienced a rise in conservatively managed patients; ten in 2020 compared to 14 over the previous four years.
Conclusion
There has not been a reduction in the number of hip fractures during COVID-19 period compared to the same time period over previous years. In our experience, there has been an increase in conservative treatment and decreased length of stay during the COVID -19 period.
Cite this article: Bone Joint Open 2020;1-8:500–507.
Introduction
The COVID-19 pandemic has placed immense pressure upon the National Health Service (NHS) as well as the general public. National Health Service England (NHSE) guidance in this COVID-19 period (1 March 2020 to 30 April 2020) suggests that there may be a role for nonoperative management of some fragility fractures; however, hip fractures will continue to be one of the most common operations and social isolation policy is unlikely to prevent this injury.1 The proposed benefits of nonoperative care for fragility fractures include reduction of inpatient stay and associated risk of exposure to COVID-19, as well as resource allocation to manage the pandemic.1 Within England, Wales, and Northern Ireland, 175 trauma units have provided care to 66,313 hip fractures patients in 2018.2 The National Hip Fracture Database (NHFD) was established in 2007 as the result of a collaboration between the British Orthopaedic Association (BOA) and the British Geriatrics Society. This has led to a reduction in mortality with 6.1% of patients dying within 30 days of hip fracture in 2018.2 Hip fractures remain a surgical priority during COVID-19 as reiterated by both the BOA and Royal College of Surgeons coronavirus guidelines.3,4
In order to sustain hip fracture services, initial management was centralised through the Royal Shrewsbury Hospital (RSH) for preoperative orthopaedic assessment and medical optimisation. Medically stable patients were then transferred to Robert Jones and Agnes Hunt Orthopaedic Hospital (RJAH) for operative intervention. We aim to review the impact of COVID-19 on workload and the related service changes on the management of hip fractures attending our orthopaedic service within rural Shropshire.
Methods
We collected data from a prospectively maintained database, reviewing all hip fracture patients who attended the hospital during 1 March and 30 April between 2016 and 2020. Data parameters included: baseline demographics of age and sex, fracture type, treatment intervention, length of inpatient stay, and mortality. We also cross-checked the data with hospital clinical electronic records and the National Hip Fracture Database. The hip fracture pattern was categorized as intracapsular or extracapsular. Treatment was classified as: conservative (nonoperative), dynamic hip screw (DHS), hemiarthroplasty, total hip arthroplasty (THA), cannulated screw fixation or intramedullary nailing. For the purposes of discussion and comparison we have categorized the months of March and April 2020 as the COVID-19 period, in keeping with the changes to healthcare services during these months.
In order to address the logistical challenges of the pandemic, all adult trauma, including hip fractures, from the region were diverted to the RSH for emergency care, medical optimization, and definitive orthopaedic surgical assessment. Orthopaedic surgical services were redirected to the regional specialist centre, RJAH. Medical admission in RSH was used as proxy for orthogeriatric review prior to surgical management for unstable patients, as there are care benefits including reduced mortality with this co-management model.5 Transfer was facilitated 24 hours a day to allow prompt access to a trauma multidisciplinary team for a definitive treatment plan and timely operative intervention. Care has remained consistent with pre-COVID-19 pandemic, where hip fracture patients are managed as per National Hip Fracture Guidelines,6 with the input of both trauma orthopaedic surgeons and orthogeriatric physician care. All patients received baseline preoperative investigations of the relevant pelvic and hip radiographs, plain chest radiographs, electrocardiogram, COVID-19 swabs and bloods tests. Patients were then transferred to RJAH once assessed as medically stable and suitable for operative intervention.
RJAH has adapted to deliver care for trauma patients during COVID-19 pandemic including the cessation of elective operating, similar to other orthopaedic centres in order to help resource management and continued emergency care.7–10 The clinical environments were categorized as green (low-risk for COVID-19) and a blue (high-risk COVID-19) areas, similar to the proposed pathways described by the BOA for recommencement of non-urgent care.11 Patients received a risk assessment for COVID-19 exposure in RSH, based on a simple risk of exposure questionnaire such that high risk or positive patients who remained medically stable were managed in a separate blue ward within RJAH. The RSH orthogeriatric consultants were also redeployed to RJAH in order to care for the patients who were transferred.
Descriptive statistics were used to present means, SD, and ranges. Chi-squared tests ere used for categorical data and independent-samples t-test for continuous data, with significance set at p < 0.05. Statistical analysis of results was conducted using RStudio Team 2020 (Boston, Massachusetts, USA), and tables and figures produced on Excel (Microsoft, Redmond, Washington, USA).
Results
We treated 288 patients in the months of March and April during the years of 2016 to 2020 (Figure 1). Of these patients, 181 were female and 107 were male, with a mean age of 82.6 (40 to 98). We found that over the five years there were a greater proportion of intracapsular (58%, n = 173) compared to extracapsular hip fractures (42%, n = 115) at our trust (Table I). Between 2016 and 2019 mean length of stay was 13.1 days (SD 8.2). During the COVID-19 period the mean length of stay was 5.0 (SD 6.3). There was one COVID-19 related death due to respiratory infection (COVID-19 positive) who was palliated under the care of physicians. In the four years prior to COVID-19 there were three mortalities in hip fracture patients as a result of: hepatic failure secondary to alcohol excess and variceal bleed; end stage renal failure on background of previous renal hydronephrosis; and infective exacerbation of chronic obstructive pulmonary disease. Patients unsuitable for surgical intervention were treated conservatively. This decision was made following physician assessment in RSH and discussion with the RJAH trauma orthogeriatric team. There were ten patients managed conservatively during COVID-19 due to unstable medical conditions and patient choice (Table II).
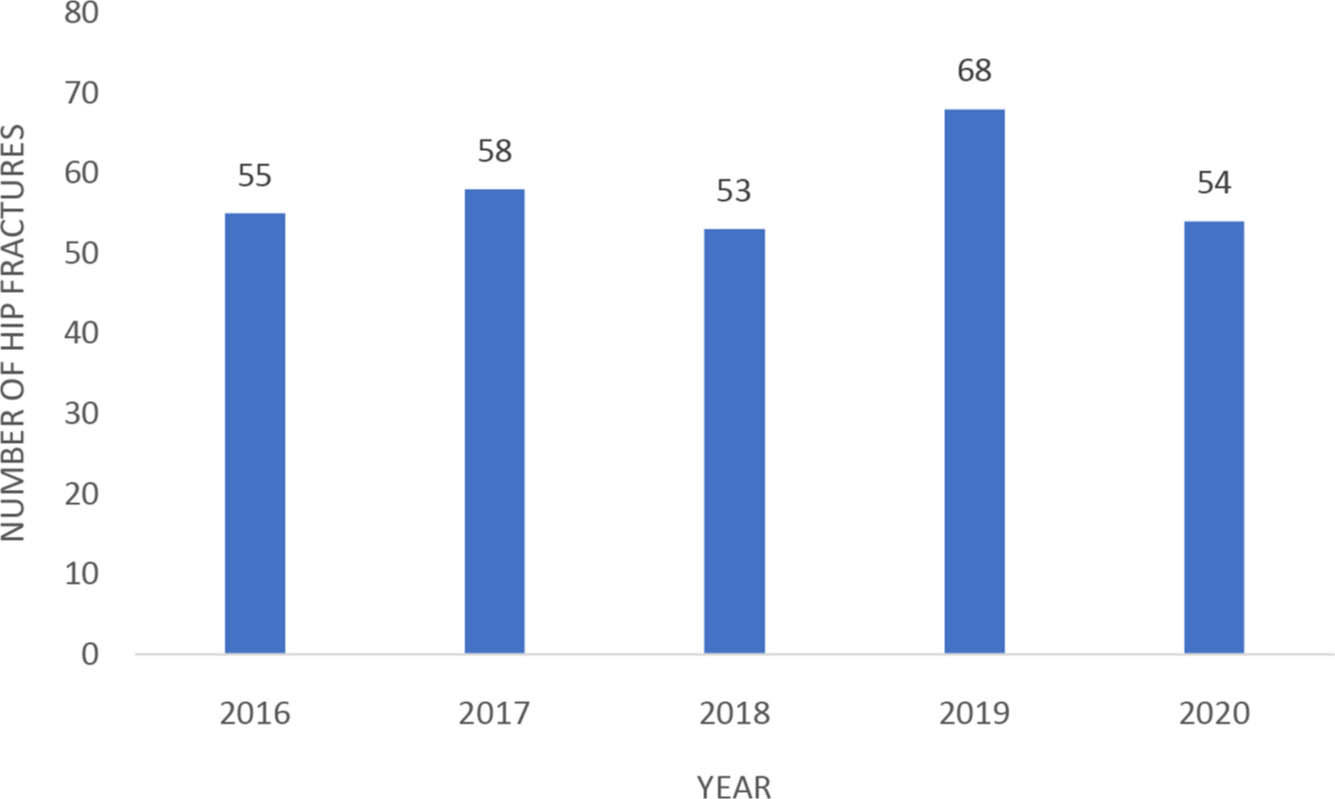
Fig. 1
Hip fracture incidence, (March and April 2016 to 2020).
Table I.
Hip fracture patient demographics and fracture patterns between 2016 and 2020.
| Patient demographics | 2016 to 2020 | Pre-COVID-19 (2016 to 2019) | COVID-19 (2020) | p-value* |
|---|---|---|---|---|
| Fractures, n | 288 | 234 | 54 | |
| Sex, M:F | 107:181 | 89:145 | 18:36 | 0.519† |
| Mean age, yrs (SD; range) | 82.6 (10.0; 40 to 98) | 82.4 (10.4; 40 to 98) | 84.5 (8.3; 62 to 98) | 0.194‡ |
| Fracture pattern, n | 0.337† | |||
| Intracapsular | 173 | 135 | 35 | |
| Extracapsular | 115 | 99 | 19 |
-
*
Between pre-COVID-19 (2016 to 2019) and COVID-19 (2020)
-
†
Chi-squared test.
-
‡
Independent-samples t-test.
Table II.
Conservatively managed hip fractures during the COVID-19 pandemic.
| Patient number | Considerations and conditions guiding decision making |
| 1 | Acute coronary syndrome requiring ongoing cardiology care |
| 2 | End stage heart failure as assessed by cardiology |
| 3 | Undisplaced intertrochanteric fracture, history of coronary bypass, metallic valve arthroplasty, pacemaker, upper and lower limb axonal neuropathy |
| 4 | Advanced dementia, baseline mobility bed to chair with assistance, lasting power of attorney advised patient preference for conservative treatment |
| 5 | Unstable thoracic aortic aneurysm as assessed by cardiology |
| 6 | Recent subarachnoid and subdural haemorrhage under palliative care |
| 7 | Undisplaced intracapsular hip fracture, history of severe heart failure and multiple pulmonary embolus |
| 8 | Undisplaced intracapsular hip fracture, baseline mobility bed to chair with assistance, patient choice against operative intervention |
| 9 | Respiratory infection, COVID-19 positive and subsequently died |
| 10 | Undisplaced intracapsular hip fracture, patient choice against operative intervention |
Hemiarthroplasty and DHS have taken precedence in the management of hip fractures within our trust, especially in the pre-COVID-19 years (Figure 2). This has continued during the COVID-19 period, although there has been an evident rise in the number of patients who have been managed conservatively and limited undertaking of intramedullary fixation (Figure 3).
Across the range of operative interventions for hip fractures, we have not found a statistically significant change to management (Table III). There was limited undertaking of intramedullary nailing or cannulated screws during COVID-19, although these are few throughout our five-year experience compared to hemiarthroplasty and DHS.
Table III.
Hip fracture management and outcome between 2016 and 2020.
| Management | 2016 to 2020 | Pre-COVID-19 (2016 to 2019) | COVID-19 (2020) | p-value* |
| Nonoperative treatment, n | 24 | 14 | 10 | 0.018†‡ |
| Operative treatment, n | 264 | 220 | 44 | 0.522‡ |
| Type of operation, n | ||||
| Dynamic hip screw | 101 | 84 | 17 | 0.668‡ |
| Hemiarthroplasty | 132 | 109 | 23 | 0.744‡ |
| Total hip arthroplasty | 11 | 9 | 2 | 0.962‡ |
| Cannulated screws | 2 | 1 | 1 | 0.261‡ |
| Intramedullary nailing | 18 | 17 | 1 | 0.157‡ |
| Mean length of stay, days (SD) | 11.6 (8.5) | 13.1 (8.2) | 5.0 (6.3) | < 0.001†§ |
| Mortality, n | 4 | 3 | 1 |
-
*
Between pre-COVID-19 (2016 to 2019) and COVID-19 (2020)
-
†
Statistically significant.
-
‡
Chi-squared test.
-
§
Independent-samples t-test.
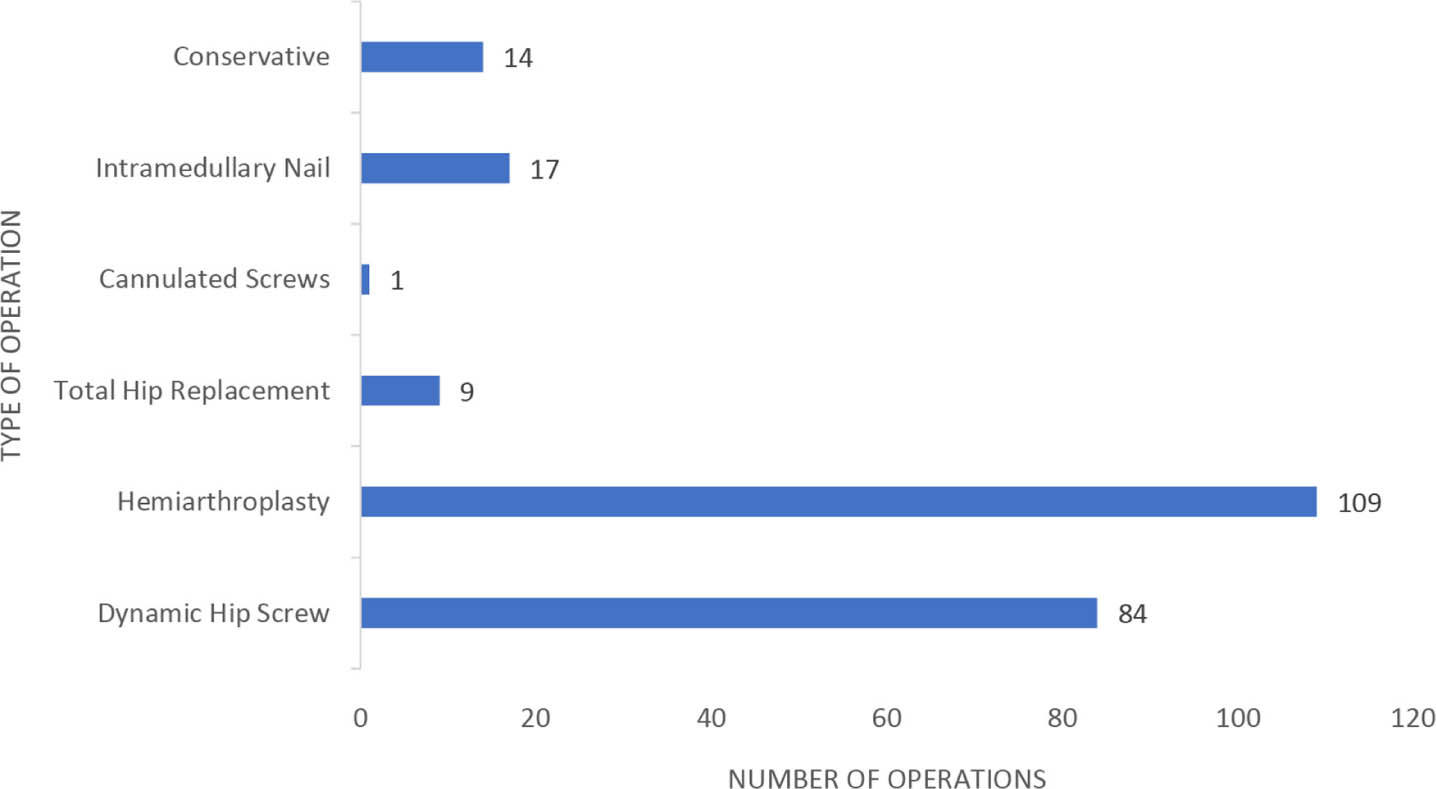
Fig. 2
Pre-COVID-19 hip fracture treatment (March and April, 2016 to 2019)
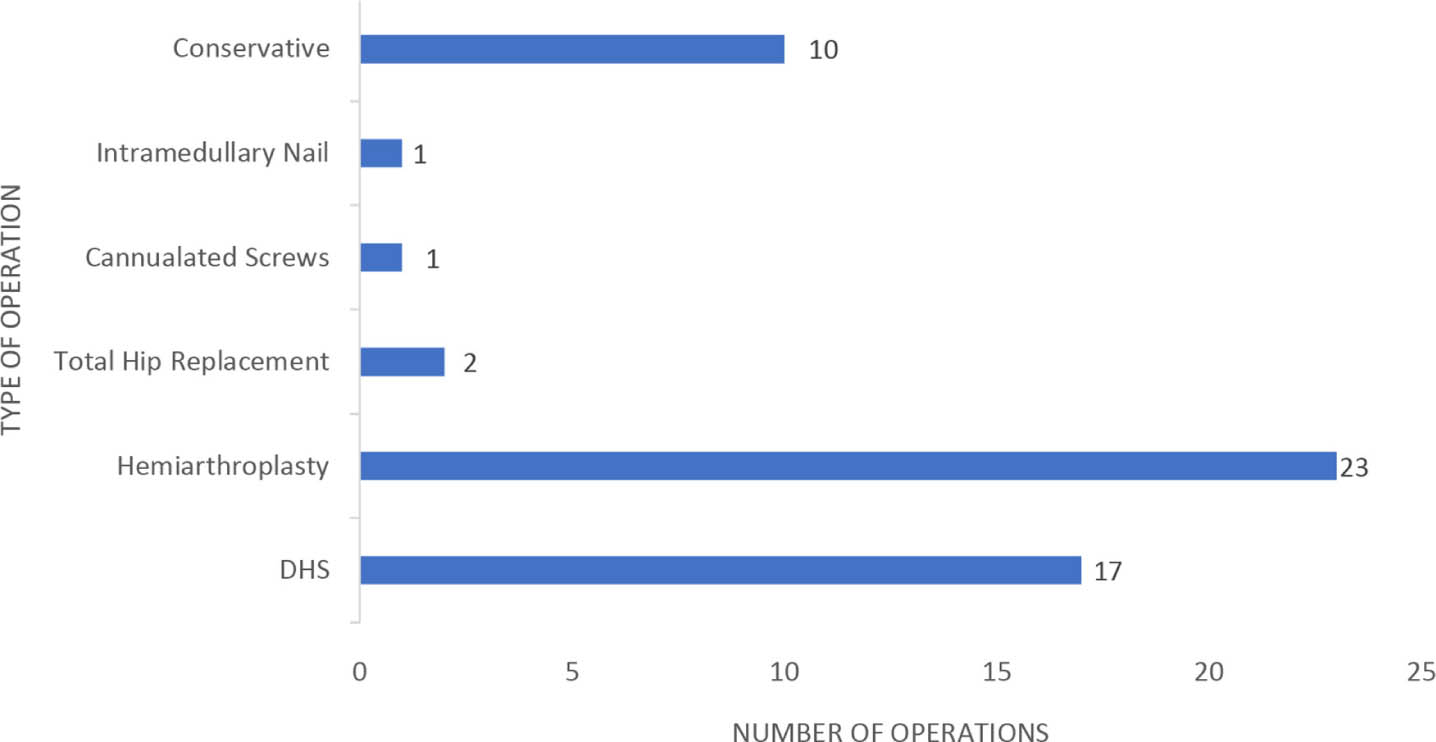
Fig. 3
COVID-19 period hip fracture treatment (March and April, 2020).
Discussion
The COVID-19 global pandemic caused by the severe acute respiratory syndrome coronavirus2 (SARS-CoV-2) has taken an immense toll on the NHS. With over 44,000 deaths COVID-19 deaths, the United Kingdom has been one of the worst affected nations in the world.12 The impact has necessitated large scale redesign of healthcare services, with new COVID-19 period guidelines across specialities.13 In our region the trauma and orthopaedic surgery services have needed to adapt with the combined efforts of the RSH and RJAH. Elective operating has been stopped in keeping with national guidance for prioritisation.4
In our experience, the number of patients attending with hip fractures has not decreased during COVID-19 despite government-introduced shielding and social distancing.14 Indeed, the challenges of timely access to regular carers, community support from friends and family may have proven detrimental to patients suffering hip fractures. We cannot infer causation, although the challenges to both assessment and the provision of care during COVID-19 are highlighted by the CarersUK reports.15,16
We did not find a statistical significance difference between the ages of the two patient groups, however the age range during COVID-19 has been higher with the youngest patient being 62 years compared to 40 years in the pre-COVID period (Table I). Lockdown and travel restrictions may affect young patients more as they sustain hip fractures following high energy trauma such as road traffic accidents, whereas the older population more commonly experience low-energy mechanism such as fall and fragility fractures.17–19 United Kingdom 2011 National Census data also shows that Shropshire has a higher than average population over the age of 65, and so travel lockdown measures are unlikely to alter this population's activity.20
BOA guidance has supported the selection of hemiarthroplasty in place of THA so as to prevent delay and deliver timely surgery for hip fracture during COVID-19.3 In our pre-COVID-19 experience, hemiarthroplasty was the most common procedure followed by DHS which is consistent with NHFD 2019 report.2 The accepted practice as per the National Institute for Health and Care Excellence (NICE) is to provide either hemiarthroplasty or THA for intracapsular fractures as per eligibility criteria.6 Pre-COVID-19, the NHFD 2019 report shows 33.4% of eligible displaced intracapsular fractures were treated with THR nationally.21 Pre-COVID-19, RJAH has delivered elective care and as such we cannot compare it to the current trauma hip fracture management in this hospital. Within our experience and with the presence of readily available specialist orthopaedic workforce at RJAH, we have not seen derogation from THA to hemiarthroplasty during COVID-19, as two cases were performed in this time (Table III). At present we do not have a comparative literature to show if other units are undertaking hemiarthroplasties during COVID-19 for those who may have otherwise qualified for a THA pre-COVID-19.
There has been a statistically significant three-fold increase in conservative treatment during the COVID-19 period compared to pre-COVID-19 in our hospital (Table III). A Cochrane systematic review that included five studies and 428 patients demonstrated that surgical management of undisplaced intracapsular fractures and undisplaced extracapsular hip fractures have better outcomes in terms of reduced length of stay and retaining patient independence, however there was limited evidence to inform practice.22 A meta-analysis of 1,189 patients also found that there were only a few small studies comparing nonoperative and operative management of hip fractures, and nonoperatively treated hip fractures had a significantly higher 30-day and one-year mortaility.23 We found one inpatient mortality in our COVID-19 period group, who was managed conservatively as a result of severe respiratory infection.
This increase in conservative management may be due to a worsening of chronic medical comorbidities, which included a number of patients who presented with unstable cardiac pathology that required intensive medical input (Table II). These patients are also the population at risk from COVID-19 and were advised to shield. Literature also corroborates the finding of comorbidity deterioration within the context of natural disasters. The University of Oxford Centre for Evidence-Based Medicine have summarized the issues of suboptimal management of chronic conditions during national emergencies, where elderly patients are particularly at an increased risk of morbidity and mortality.24-27 This is a particularly vulnerable group whose health is less amenable to tolerate significant adjustments to regular monitoring.
In addition, the strain on medical specialities in managing with organisational restructuring and redeployment of workforce may have also led to challenges in optimisation of potential operative candidates during the COVID-19 period It is also clear that physicians have faced increased stress and sleep disturbance during the COVID-19 pandemic.28,29 We reiterate that these are possibilities, not criticisms of the efforts of medical and care workforces during the pandemic.
Length of stay has decreased significantly in the COVID-19 period when compared to pre-COVID-19. This considerable decrease is partly as a result of efforts to expedite discharge in order to minimize patient exposure to COVID-19 within hospitals, and thereby increase capacity for hospital beds. RJAH established an enhanced arrangement with social services to facilitate more efficient discharge into the community during the COVID-19 pandemic, an example of the wider health and social care response to COVID-19. The Chancellor of the Exchequer announced plans for an enhanced NHS discharge process in March and supported this with a £2.9 billion fund.30 This push for hospital capacity was also directed by government and NHS initiative through Strategic Coordination Groups, with the aim to "create and maintain acute bed capacity through faster rates of appropriate discharge from NHS beds for the foreseeable future".31
The considerable changes to organisational pathways and an ever-evolving practice during the COVID-19 period, along with regular amendments to public care policy, mean that this is a snapshot of care during the current pandemic. Further studies may explore the role of chronic comorbidities in the management of hip fracture patients during COVID-19 and whether we should expect a more unwell population in future, which may further drive nonoperative care or necessitate more intensive pre and postoperative optimisation.
The COVID-19 pandemic has forced significant changes to healthcare practice, affecting all specialities. Hip fracture care remains an orthopaedic priority and, in our experience, we have restructured services to an orthopaedic specialist hospital to continue delivering care for these patients. Effective multidisciplinary collaboration with medical and orthogeriatric specialities is required in the management of hip fractures and we recognise the increased strain on these allied specialities from the direct management of COVID-19 patients.
There has not been a clear reduction in number of hip fractures during COVID-19 lockdown period compared to same time period over previous years. In our experience, there has been a significant increase in conservative management of hip fractures, with patients being more medically unstable at presentation with deterioration of chronic health conditions. This population were observing measures of social restrictions and shielding during COVID-19 period. We have also seen a significant decrease in length of stay compared to pre-COVID-19.
References
1. Baldwick C , Clinical guide for the perioperative care of people with fragility fractures during the Coronavirus pandemic . NHS [Internet] 2020 [cited 10 Jun 2020] . Version BOA1, published for BOA members 24/3/2020 . 2020 . Google Scholar
2. No authors listed . National Hip Fracture Database Annual Report. Natl. Hip Fract. Database . https://www.nhfd.co.uk/20/hipfractureR.nsf/docs/2019Report (date last accessed 2 June 2020). Google Scholar
3. British Orthopaedic Association . Management of patients with urgent orthopaedic conditions and trauma during the coronavirus pandemic. March:1–6 . 2020 . Google Scholar
4. No authors listed . Clinical guide to surgical prioritisation during the coronavirus pandemic . Royal Colleges of Surgeons . 2020 . https://www.rcseng.ac.uk/coronavirus/surgical-prioritisation-guidance/ (date last accessed 12 August 2020). Google Scholar
5. Grigoryan KV , Javedan H , Rudolph JL . Orthogeriatric care models and outcomes in hip fracture patients: a systematic review and meta-analysis . J Orthop Trauma . 2014 ; 28 ( 3 ): e49 . Crossref PubMed Google Scholar
6. National Institute for Health and Care Excellence . Overview Hip fracture in adults Quality Standard [QS16] . Nice . 2017 . Google Scholar
7. Oussedik S , Zagra L , Shin GY , D'Apolito R , Haddad FS . Reinstating elective orthopaedic surgery in the age of COVID-19 . Bone Joint J . 2020 ; 102-B ( 7 ): 807 – 810 Crossref PubMed Google Scholar
8. Jenkins P . The Early Effect of COVID-19 on Trauma and Elective Orthopaedic Surgery . British orthopaedic association . 2020 . https://www.boa.ac.uk/policy-engagement/journal-of-trauma-orthopaedics/journal-of-trauma-orthopaedics-and-coronavirus/the-early-effect-of-covid-19-on-trauma-and-elect.html (date last accessed 29 June 2020). Google Scholar
9. Mathai NJ , Venkatesan AS , Key T , Wilson C , Mohanty K . COVID-19 and orthopaedic surgery: evolving strategies and early experience . Bone & Joint Open . 2020 ; 1 ( 5 ): 160 – 166 . Crossref PubMed Google Scholar
10. Hadfield JN , Gray AC . The evolving COVID-19 effect on hip fracture patients . Injury . 2020 ; 51 ( 7 ): 1411 – 1412 . Crossref PubMed Google Scholar
11. British Orthopaedic Association . Re-starting non-urgent trauma and orthopaedic care : Full guidance. 2020;(May):1–13 . Google Scholar
12. No authors listed . Number of coronavirus (COVID-19) cases and risk in the UK. Dep. Heal. Soc. Care Public Heal. Engl . https://www.gov.uk/guidance/coronavirus-covid-19-information-for-the-public (date last accessed 10 June 2020). Google Scholar
13. No authors listed . Coronavirus Specialty guides for patient management . NHS England . 2020 . https://www.england.nhs.uk/coronavirus/publication/specialty-guides/ (date last accessed 4 July 2020). Google Scholar
14. Holmes F . COVID-19 Timeline . British Foreign Policy Group . 2020 . https://bfpg.co.uk/2020/04/covid-19-timeline/ (date last accessed 5 July 2020). Crossref PubMed Google Scholar
14. No author listed . Caring behind closed doors: forgotten families in the coronavirus outbreak . Carers UK . 2020 . https://www.carersuk.org/for-professionals/policy/policy-library/caring-behind-closed-doors-report (date last accessed 12 August 2020). Google Scholar
15. No authors listed . Coronavirus act 2020 — what it means for carers – detailed briefing on the health and care provisions on the act . Carers UK . 2020 . https://www.carersuk.org/news-and-campaigns/campaigns/coronavirus-act-emergency-measures (date last accessed 12 August 2020). Google Scholar
17. Robinson CM , Court-Brown CM , McQueen MM , Christie J . Hip fractures in adults younger than 50 years of age. epidemiology and results . Clin Orthop Relat Res . 1995 ; 312 : 238 – 246 . PubMed Google Scholar
18. Melton LJ . Hip fractures: a worldwide problem today and tomorrow . Bone . 1993 ; 14 ( SUPPL. 1 ): 1 – 8 . Crossref PubMed Google Scholar
19. Kannus P , Parkkari J , Sievänen H , et al. Epidemiology of hip fractures . Bone . 1996 ; 18 ( 1 ): S57 – S63 . Crossref PubMed Google Scholar
20. No authors listed . Population . Shropshire Council . https://www.shropshire.gov.uk/information-intelligence-and-insight/facts-and-figures/population/ (date last accessed 15 July 2020). Crossref PubMed Google Scholar
21. No authors listed . NHFD Dashboard report for All NHFD 2019. Natl. Hip Fract. Database . 2019 . https://www.nhfd.co.uk/20/NHFDcharts.nsf/fmDashboard?readform (date last accessed 2 July 2020). Google Scholar
22. Handoll HHG , Parker MJ . Conservative versus operative treatment for hip fractures in adults . Cochrane Database Syst Rev . 2008 ( 3 ): CD000337 . Crossref PubMed Google Scholar
23. van de Ree CLP , De Jongh MAC , Peeters CMM , de RCLPvan , De JMAC , et al. Hip fractures in elderly people: surgery or no surgery? A systematic review and meta-analysis . Geriatr Orthop Surg Rehabil . 2017 ; 8 ( 3 ): 173 – 180 . Google Scholar
24. Evans J . Mapping the vulnerability of older persons to disasters . Int J Older People Nurs . 2010 ; 5 ( 1 ): 63 – 70 . Crossref PubMed Google Scholar
25. Dempsey TM , Lapinsky SC , Melnychuk E , et al. Special populations: disaster care considerations in chronically ill, pregnant, and morbidly obese patients . Crit Care Clin . 2019 ; 35 ( 4 ): 677 – 695 . Crossref PubMed Google Scholar
26. Allweiss P . Diabetes and disasters: recent studies and resources for preparedness . Curr Diab Rep . 2019 ; 19 ( 11 ): 131 . Crossref PubMed Google Scholar
27. Hartmann-Boyce J , Mahtani KR . Supporting people with long-term conditions (LTCs) during national emergencies . CEBM . 2020 . https://www.cebm.net/covid-19/supporting-people-with-long-term-conditions-ltcs-during-national-emergencies/ (date last accessed 5 July 2020). Google Scholar
28. Galbraith N , Boyda D , Mcfeeters D , Hassan T . The mental health of doctors during the COVID-19 pandemic . BJPsych Bulletin . 2020 ; 289 : 1 – 4 . [cited 5 Jul 2020]. Crossref PubMed Google Scholar
29. Abdulah DM , Musa DH . Insomnia and stress of physicians during COVID-19 outbreak . Sleep Med X Elsevier BV . 2020 ; 100017 . Crossref PubMed Google Scholar
30. No authors listed . £2.9 billion funding to strengthen care for the vulnerable . GOV.UK . 2020 . https://www.gov.uk/government/news/2-9-billion-funding-to-strengthen-care-for-the-vulnerable (date last accessed 7 July 2020). Google Scholar
31. Willett K , Winn M , Roughton R , Skinner A . Chief executives of councils NHS England and NHS improvement regional directors COVID-19 hospital discharge service requirements . 2020 . https://www.england.nhs.uk/coronavirus/wp-content/uploads/sites/52/2020/03/hmg-letter-hospital-discharge-guidance-v3.pdf (date last accessed 12 August 2020). Google Scholar
Author contributions
M. S. Cheruvu: Designed the study, Collected the data, Performed the statistical anlysis, Wrote the manuscript.
D. S. Bhachu: Collected the data, Write the manuscript.
J. Mulrain: Collected the data, Wrote the paper.
S. Resool: Collected the data, Wrote the manuscript.
P. Cool: Designed the study, Performed the statistical analysis, Revised the manuscript.
D. J. Ford: Designed the study, Wrote and revised the manuscript.
R. A. Singh: Designed the study, Wrote and revised the manuscript.
Funding statement
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
Follow M. S. Cheruvu @SCheruvu01
Follow D. S. Bhachu @MrDSBhachu
© 2020 Author(s) et al. This is an open-access article distributed under the terms of the Creative Commons Attributions licence (CC-BY-NC-ND), which permits unrestricted use, distribution, and reproduction in any medium, but not for commercial gain, provided the original author and source are credited.









