Abstract
The COVID-19 pandemic creates unique challenges in the practice of spinal surgery. We aim to show how the use of a high-definition 3D digital exoscope can help streamline workflows, and protect both patients and healthcare staff.
The Coronavirus Disease 2019 (COVID-19) pandemic has caused significant disruption to daily lives and practices worldwide. Singapore reported its first case on 23 January 2020, and substantial measures have since been implemented nationwide1 to both protect its citizens and to limit the spread of the disease. Similarly, our spinal surgical practice has been adapted to safeguard healthcare staff and patients during this period.
Our institution has implemented guidelines on risk stratification of patients requiring surgery and the type of personal protective equipment (PPE) required by the operating theatre team.1 An N95 mask and eye protection (goggles or eye shield) are required in at-risk cases to protect against aerosol contamination and infection. The use of thick goggles or eye shields creates an additional barrier to microscope or surgical loupes use, and compromises on clarity and surgical safety (Figure 1).2,3 Operating time may be prolonged and extended usage of PPE is known to cause discomfort and headaches.4 In this situation, patients may have to have their surgery delayed until they have recovered or have passed their quarantine period. However, in patients requiring emergency surgery, this may not always be possible. We may end up having to compromise patient care by either delaying the surgery, opting for a compatible but less than ideal surgical modality, or risk exposing the surgical team to potential infection.

Fig. 1
Difficulties of using protective goggles with a traditional microscope.
High-definition (HD) 3D exoscope systems have been utilized in spinal surgeries with comparable results.5,6 We have found that the use of an exoscope to be far more beneficial compared to a traditional microscope in this instance. The model we have utilized is the Modus V (Synaptive Medical, Toronto, Canada). This allows for stereoscopic 3D images to be viewed on a HD monitor via the use of 3D glasses. The protective goggles can be easily combined with the lens from the 3D glasses (Figure 2). By removing the need for visualization through an eyepiece while maintaining an optimal 3D visual field, it is compatible with the use of mandated protective eye wear.

Fig. 2
Original 3D glasses with lens removed (left). Protective goggles with 3D lens attached (right).
Making the switch from the traditional microscope to the exoscope system may necessitate some adjustments in the operating theatre layout. The monitors must be angled appropriately such that both surgeons can easily visualize individual screens, and the working height of the scope set such that instruments may easily pass below, yet does not obstruct the surgeon’s line of sight7 (Figure 3). With the change to a head-up orientation, transitioning from a traditional microscope to the 3D exoscope system does incur a slight learning curve in terms of hand-eye coordination for the surgeon. In our case, we had the advantage of having carried out 13 cases utilizing the 2D function also available on the same exoscope system, thus minimising the adjustment process. There is, however, a likely increase in operating time in the initial stages due to unfamiliarity with the device.6 Similarly, the initial set-up time required in the first few cases utilizing the exoscope resulted in an estimated additional 15 to 20 minutes to allow for optimising the theatre layout, as well as allowing theatre staff to familiarise with the mechanics of the device. However, once teething issues have resolved, we have found the overall set up time required for the exoscope to be comparable to that of a traditional microscope.

Fig. 3
Layout of operating theatre with exoscope set up.
We have utilized this system in 8 spinal surgeries (Table I), and found that setting the scope height at 450 mm to 600 mm with a zoom of 50% to 70% and lighting at 30% to be most ideal in our set up. The advantage of this feature is that the whole surgical team is able to clearly see the surgical site while maintaining a larger distance from each other (Figure 4). The improved ergonomic set up, as a result of more comfortable viewing angles, further reduces surgeon fatigue, which can be exacerbated by prolonged wearing of PPE. Using a digital microscope with automated tracking, autofocus functions, and voice controls also helps reduce the level and frequency of physical contact required with the microscope, further ensuring the integrity of the sterile field.

Fig. 4
Operating room with exoscope and monitor during a procedure.
Table I.
Spine surgeries carried out using the Synaptive Modus V exoscope.
| Case | Age | Sex | Diagnosis | Procedure |
|---|---|---|---|---|
| 1 | 44 | M | L4/L5 stenosis with herniated disc | L4/L5 microdiscectomy |
| 2 | 38 | F | L5/S1 prolapsed intervertebral disc | L5/S1 microdiscectomy |
| 3 | 57 | M | T11/12 circumferential stenosis | T11-L2 decompression + fusion |
| 4 | 48 | M | L5/S1 herniated disc | L5/S1 decompression |
| 5 | 70 | M | T8/T9 thoracic stenosis | T8-T10 decompression and instrumented fusion |
| 6 | 20 | M | L1 burst fracture with cord compression | T12-L3 posterior decompression and instrumented fusion |
| 7 | 81 | F | C7/T1 intradural meningioma | C7-T1 laminectomy+ excision of tumour |
| 8 | 29 | M | T3 chance fracture, T4 burst fracture, and T5 wedge fracture, with cord compression | T2-6 decompression and instrumented stabilisation |
-
*
Synaptive Medical, Toronto, Canada.
As a measure of clinical efficacy, we compared the eight cases carried out using the 3D exoscope (Table I) against matched cases performed with the traditional microscope before the declaration of the pandemic. Complication rates with either system are similarly low, with no complications noted in any of the eight exoscope cases. There was one incidence of a postoperative wound infection in one of the earlier cases prior to the pandemic. In terms of length of stay, we did not note any difference between the two systems with regards to number of days in hospital due to surgical issues. Having been familiarised with the 2D function of the exoscope system, operating times when using the 3D modality was also comparable to similar cases carried out with the traditional microscope.
However, despite its benefits, one considerable reason that the 3D exoscope system may be slow on the uptake in healthcare institutions around the world is the cost. Particularly when healthcare systems are under considerable strain with additional stresses from the COVID-19 pandemic, a recommended retail price of SGD $900,000 to $1,000,000 (GBP £521,000 to £580,000) may be prohibitive.
3D exoscopes have been shown to be at least an equivalent or superior alternative to traditional microscopes in terms of surgical field visualization (Figure 5), ease of handling, and training purposes in microscope-assisted surgery.5,6 There is as yet no definitive end in sight to the COVID-19 pandemic, and these safety measures and PPE guidelines mandated will likely continue to be in place for the foreseeable future. Adopting the use of exoscopes in spinal surgery during and after the COVID-19 pandemic may play a role in helping to streamline the workflow by reducing the barriers for surgical procedures to be carried out in a smooth and timely manner. Importantly, this improves patient care, and at the same time reduces the risk of infection exposure to the surgical team.
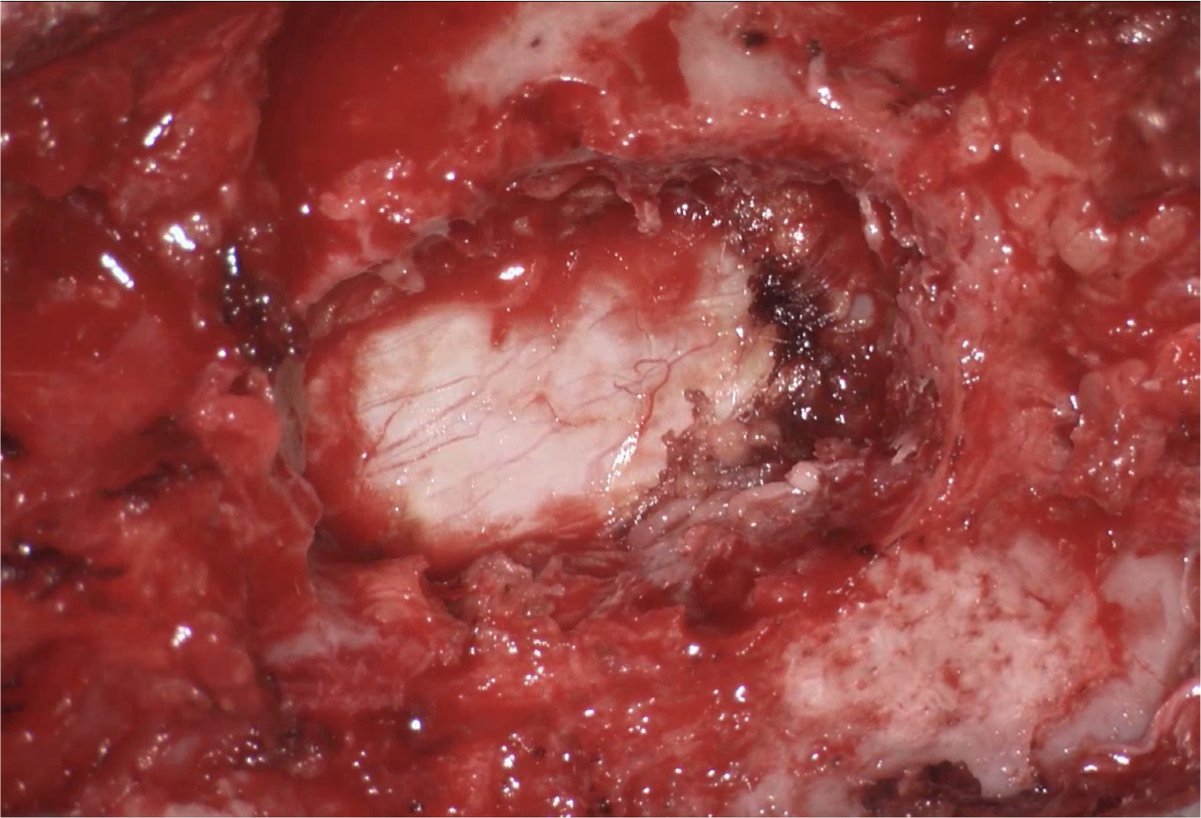
Fig. 5
Intraoperative visualization with exoscope.
References
1. BJN T , HLT T , Loo WL DS . Impact of the coronavirus disease 2019 pandemic on spinal surgery in Singapore . Singapore Med J . 2020 : 1 – 7 . Google Scholar
2. Amin-Hanjani S , Bambakidis NC , Barker FG , et al. Editorial. COVID-19 and neurosurgical practice: an interim report . J Neurosurg . 2020 : 1 – 2 . Crossref PubMed Google Scholar
3. Hwee J , Chiew J , Sechachalam S . The impact of coronavirus disease 2019 (COVID-19) on the practice of hand surgery in Singapore . J Hand Surg Am . 2020 ; 45 ( 6 ): 536 – 541 . Crossref PubMed Google Scholar
4. JJY O , Bharatendu C , Goh Y , et al. Headaches associated with personal protective equipment – a cross-sectional study among frontline healthcare workers during COVID-19 . Headache . 2020 . Google Scholar
5. Barbagallo GMV Certo F . Three-Dimensional, high-definition Exoscopic anterior cervical discectomy and fusion: a valid alternative to Microscope-Assisted surgery . World Neurosurg . 2019 ; 130 : e244 – e250 . Crossref PubMed Google Scholar
6. Kwan K , Schneider JR , Du V , et al. Lessons learned using a high-definition 3-dimensional exoscope for spinal surgery . Oper Neurosurg . 2019 ; 16 ( 5 ): 619 – 625 . Crossref PubMed Google Scholar
7. Ariffin MHM , Ibrahim K , Baharudin A , Tamil AM . Early experience, setup, learning curve, benefits, and complications associated with Exoscope and three-dimensional 4K hybrid digital Visualizations in minimally invasive spine surgery . Asian Spine J . 2020 ; 14 ( 1 ): 59 – 65 . Crossref PubMed Google Scholar
Author contributions
T. H. L. Teo: Wrote the manuscript, Produced the figures.
B. J-N. Tan: Wrote the article, Produced the figures.
W. L. Loo: Supervised the study, Produced the figures.
A. K. S. Yeo: Supervised the study.
S. K. Dinesh: Supervised the study, Editing the manuscript, Produced the figures.
Funding statement
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
© 2020 Author(s) et al. This is an open-access article distributed under the terms of the Creative Commons Attributions licence (CC-BY-NC-ND), which permits unrestricted use, distribution, and reproduction in any medium, but not for commercial gain, provided the original author and source are credited.









