Abstract
Aims
The COVID-19 pandemic presents an unprecedented burden on global healthcare systems, and existing infrastructures must adapt and evolve to meet the challenge. With health systems reliant on the health of their workforce, the importance of protection against disease transmission in healthcare workers (HCWs) is clear. This study collated responses from several countries, provided by clinicians familiar with practice in each location, to identify areas of best practice and policy so as to build consensus of those measures that might reduce the risk of transmission of COVID-19 to HCWs at work.
Methods
A cross-sectional descriptive survey was designed with ten open and closed questions and sent to a representative sample. The sample was selected on a convenience basis of 27 senior surgeons, members of an international surgical society, who were all frontline workers in the COVID-19 pandemic. This study was reported according to the Standards for Reporting Qualitative Research (SRQR) checklist.
Results
Responses were received by all 27 surgeons from 22 countries across six continents. A number of the study respondents reported COVID-19-related infection and mortality in HCWs in their countries. Differing areas of practice and policy were identified and organized into themes including the specification of units receiving COVID-19 patients, availability and usage of personal protective equipment (PPE), other measures to reduce staff exposure, and communicating with and supporting HCWs. Areas more specific to surgery also identified some variation in practice and policy in relation to visitors to the hospital, the outpatient department, and in the operating room for both non-urgent and emergency care.
Conclusion
COVID-19 presents a disproportionate risk to HCWs, potentially resulting in a diminished health system capacity, and consequently an impairment to population health. Implementation of these recommendations at an international level could provide a framework to reduce this burden.
Introduction
In early 2020, a novel coronavirus rapidly spread out of China to the rest of the world.1 The World Health Organization (WHO) declared coronavirus disease 2019 (COVID-19), secondary to severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2),1-3 a pandemic on 11 March 2020.4 Existing health infrastructures around the world were unprepared for this unprecedented burden, with many hospitals reporting shortages in frontline healthcare workers (HCWs), personal protective equipment (PPE), bed space, and ventilators in intensive care units (ICUs) relatively early in the pandemic.5
With health systems reliant on an adequate workforce, it is paramount to protect HCWs by minimizing their risk of contracting COVID-19 through work. There is a dual benefit to protecting HCWs from developing COVID-19: to minimize the number of HCWs that are unable to work (due to sickness, self-isolation, or quarantine), and to minimize transmission of the virus to the vulnerable patients for whom they care. HCWs may be exposed to many patients positive for COVID-19 who likely display more severe features, and consequently longer virus-shedding periods.6 This puts HCWs at greater risk than those infected through community transmission.
Performing surgical procedures (both elective and emergency) present a number of unique challenges during the COVID-19 pandemic. The disposable PPE equipment (hat, mask, gown, visor, and gloves) used during surgical procedures, reduces the supply available for workers in direct contact with infected patients.7 Operating rooms (ORs) have positive pressure air filtration systems that push high volumes of air out of the OR. When a patient or HCW with COVID-19 is in the OR, they have a greater chance of dispersing the virus.8 Many interventions in surgery generate aerosols, including the use of power tools.9,10 These aerosols have a potential to disperse a high viral load to HCWs.11 Additionally, some patients undergo non-urgent elective procedures requiring routine postoperative inpatient stays, putting them at risk of cross-contamination in a hospital with other patients carrying COVID-19.
This study aims to identify differences in practice and policy in surgery in the context of the COVID-19 pandemic to inform debate and policy development and contribute towards international consensus.
Methods
The study was conducted in accordance with the 2014 Standards for Reporting Qualitative Research (SRQR), endorsed by the EQUATOR network, to ensure transparency in reporting of qualitative research.12 A survey-based approach in a non-experimental design was used to describe the reality of the current policies and practices in relation to the COVID-19 pandemic. A cross-sectional descriptive survey was designed and remained open only on the dates between 23 March 2020 and 27 March 2020. The survey was developed to allow information to be collected on attitudes and behaviour. The questionnaire was in English and included ten questions (see Table I) that were self-completed. The questions were a combination of closed questions to allow comparisons and open questions to allow collection of qualitative data. Respondents were also asked to send a copy of their government or hospital policy. Administration of the questionnaire by the senior author and the subsequent responses were conducted via email. Peer relationships existed between the senior author and all questionnaire respondents and were not thought to influence responses. Due to the time sensitivity of this data to inform policy and readers globally, no specific research tool, pretesting, validity or reliability testing was practical. With figures changing daily, an iterative approach was incorporated and all respondents were asked on 5 April 2020, prior to manuscript submission, to provide updated morbidity and mortality data of HCWs, if available.
Table I.
The ten questions of the cross-sectional descriptive survey.
| Number | Question |
|---|---|
| 1 | How many medical staff were infected in your country? |
| 2 | How many of those were surgeons? |
| 3 | How many died? Of those that died, how many were surgeons? |
| 4 | What measures were taken by the hospital / government specifically to protect the medical staff? |
| 5 | Were routine outpatient clinics cancelled? |
| 6 | How did you manage the trauma patients - both in the emergency department and in clinics? |
| 7 | Were elective operations cancelled? If not, how were they managed? |
| 8 | What specific precautions were taken, if any, in the operating room? |
| 9 | What specific precautions were taken in the outpatient clinic/ward setting? |
| 10 | Were decisions made to manage more patients non-operatively/conservatively due to Covid-19? |
The representative sample for the survey was selected by convenience sampling from English-speaking senior clinicians familiar with practice in each location, practicing in major trauma or teaching hospitals with geographical proximity to the epicentre of each country. In South Korea two hospitals were identified, one from the ‘fulminant’ and another one from the ‘non-fulminant’ zone. In all, 27 actively involved in the care of frontline COVID-19 patients were selected to receive the survey from 22 countries on six continents. Participants were selected as they were likely to express opinions that were representative of a broader surgical professional population within the corresponding country. Where major differences in practices were identified between urban and rural settings within countries, one opinion was sought from each region. Consent to participate was assumed in a voluntary response to the survey.
Data analysis and synthesis
All responses were electronically collated into a database and grouped by country. Data were analyzed prospectively at multiple interims. No further sampling was performed when sampling saturation was thought to have been reached. To enhance trustworthiness and credibility, all responses were analyzed independently by two physician authors (ZBH, VK), with complementary expertise in epidemiology and surgery respectively. Comparisons were made for responses to closed questions. Written responses to open questions that included free text were analyzed by grouping quotations from respondents into themes. This allowed a number of themes to be developed, with multiple countries contributing to each theme.
Results
There were a total of 27 respondents from 22 countries on six continents (see Figure 1). Combined, the country of origin of the respondents represented 57.5% of the world’s population and over 6.6 million medically-qualified HCWs. Among countries sampled in this study at the time of data collection, there was substantial variation in the numbers of confirmed COVID-19 cases and COVID-19-related mortality figures. All 27 respondents worked in major trauma centres in large cities.
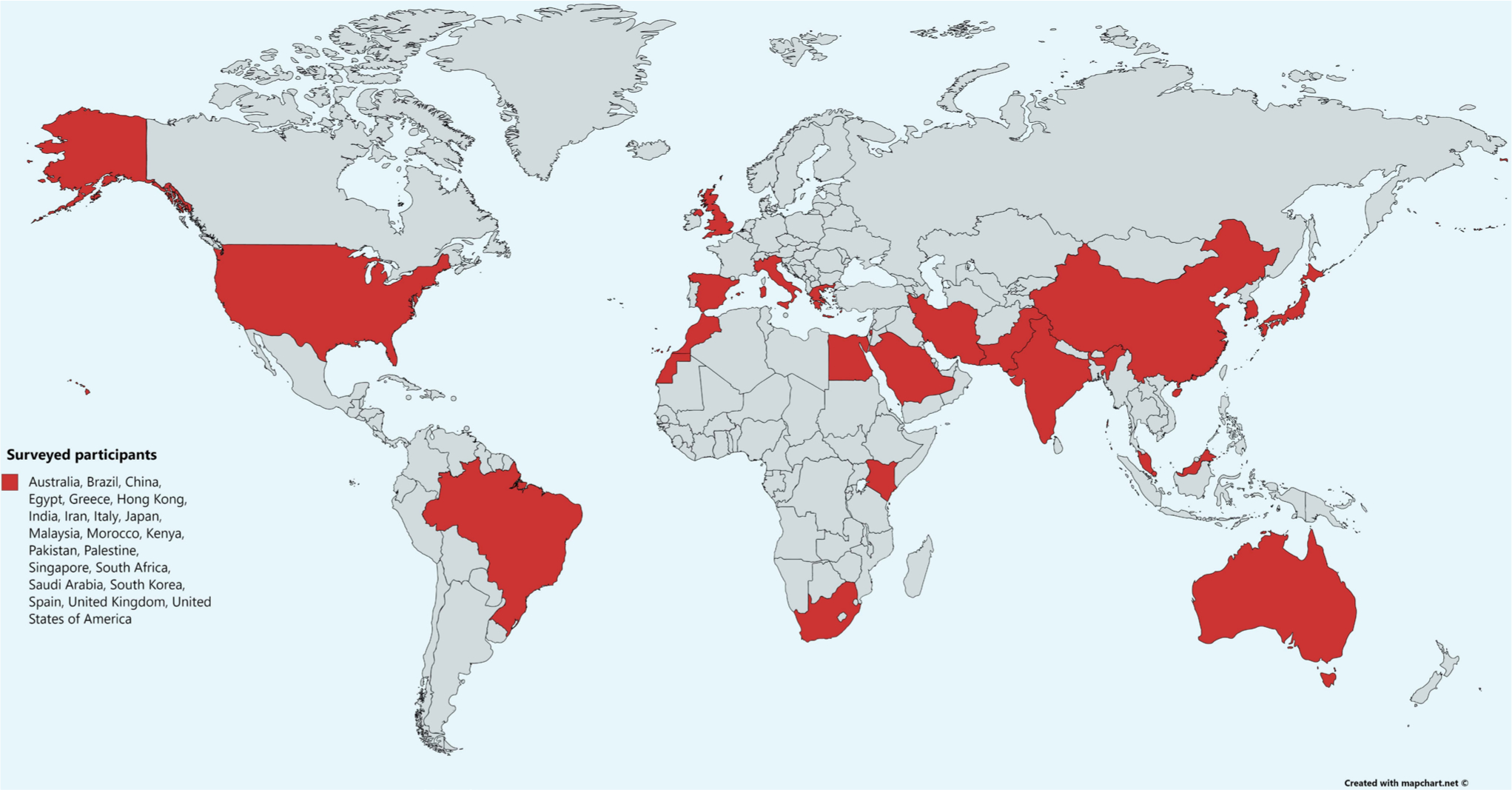
Fig. 1
World map indicating countries represented by survey respondents. Designed using an open source online tool, mapchart.net.
In this group, 16/22 (73%) countries reported confirmed cases of HCWs contracting COVID-19 infections in their countries (see Table II), however specific morbidity and mortality rates of HCWs varied vastly between countries. At the time of data collection, Spain had an estimated 19,400 infected HCWs, representing 14.4% of all cases in the country, at least 75 of these had died, 20 of whom were surgeons. Italy had 11,252 infected HCWs, 52 of whom had died, including one surgeon. China reported that 3019 HCWs were infected, 87.5% of whom were from Hubei province, and 61 HCWs died in total. In the USA, in Massachusetts alone, 924 cases in HCWs had been reported,13 with the total state cases of 5,752 at the same time point; therefore, HCWs represented around 16% of the infected population. Iran had reported 350 infected HCWs, of whom 96 had died. Malaysia, South Korea, and Japan and reported 138, 100, and 50 to 100 infected HCWs respectively. The UK had reported eight HCW deaths but the number infected was unknown. All other participant countries were not aware of the number or none had been reported.
Table II.
Country profiles of respondents, including population size, number of medically qualified HCWs, and whether they had confirmed COVID-19 infections in HCWs as of 5 April 2020.
| Country | Population* | Percentage world population (7,775,840,000) | Number of physicians | Respondents reporting COVID-19 infections in HCWs |
|---|---|---|---|---|
| Australia | 25,499,884 | 0.32793735 | 86,550 | Yes |
| Brazil | 212,559,417 | 2.73358784AQ: | 453,351 | Yes |
| China | 1,438,030,215 | 18.4935674 | 2,508,408 | Yes |
| Egypt | 102,334,404 | 1.31605594 | 77,083 | Unknown |
| Greece | 10,423,054 | 0.13404409 | 51,356 | Unknown |
| Hong Kong | 14,290 | |||
| India | 1,380,004,385 | 17.7473351 | 1,041,395 | Unknown |
| Iran | 83,992,949 | 1.08017846 | 90,470 | Yes |
| Italy | 60,461,826 | 0.77756006 | 242965 | Yes |
| Japan | 126,476,461 | 1.62653117 | 308,105 | Yes |
| Malaysia | 32,365,999 | 0.41623798 | 46,491 | Yes |
| Morocco | 36,910,560 | 0.47468261 | 25,992 | Yes |
| Kenya | 53,771,296 | 0.69151752 | 8,042 | No |
| Pakistan | 220,892,340 | 2.84075212 | 184,711 | Unknown |
| Palestine | 5,101,414 | 0.06560595 | 8,810 | No |
| Singapore | 5,850,342 | 0.07523743 | 12,967 | No |
| South Africa | 59,308,690 | 0.76273033 | 51,616 | Yes |
| Saudi Arabia | 34,813,871 | 0.44771846 | 77138 | Unknown |
| South Korea | 51,269,185 | 0.65933951 | 120,630 | Yes |
| Spain | 46,754,778 | 0.60128267 | 188,595 | Yes |
| UK | 67,886,011 | 0.87303765 | 185,692 | Yes |
| USA | 331,002,651 | 4.25680892 | 835,987 | Yes |
-
*
Source: https://www.worldometers.info/world-population/population-by-country/ ; †World Health Organization (WHO). Global Health Workforce Statistics. Retrieved 5 April 2020 (https://apps.who.int/gho/data/node.main.HWF.); ‡Figures not reported by WHO.
At the time of data collection, there were respondents from six different countries that were aware of COVID-19-related mortality in HCWs, but only five of these countries (Italy, Spain, Iran, UK, and China) had HCW mortality that was directly attributable to frontline work.
Specialist care and isolating COVID-19 patients
Respondents stated that there were policies in place for ‘isolating any confirmed or suspicious cases’ with a number of respondents stating that there were regional policies in place for ‘dedicating specific centres to deal with such cases’.
Personal protective equipment
In all, 12 out of 22 (55%) respondent countries commented on their experience of the distribution or use of PPE during the COVID-19 pandemic. Comments included the government advice, in particular as to the type of face mask. FFP2 (or the equivalent rating N95) masks were specifically mentioned as mandatory PPE for treating COVID-19 patients in 8/22 (36%), as only these masks have protection against aerosols. Other respondents described three levels of PPE: level 1 = ‘all the medical staff must wear a surgical mask in the hospital’; level 2 (for staff working in the emergency department) = ‘N95 mask and isolation gown is essential for protection’ ; and for level 3 (staff working with confirmed infected COVID-19 patients) ‘protection suits, N95 masks, goggle, shoes, sleeves, and work caps’ or ‘plastic masks or plastic films can also be used instead of goggles’. Some respondents were concerned about the availability of PPE in the workplace, reporting that PPE was ‘nothing other than giving us a mask’. Others stressed the need for education for HCWs in the use of PPE ‘HCWs providing care for any patient under investigation, need to have undergone training on the appropriate use of PPE’.
Limiting HCW exposure, staff testing, self-isolation, and support
One respondent noted a policy to reduce staff exposure by ‘rotating teams: one team working in hospital, one team in teaching/academic/teleconference’ activity. Other respondents reported that with the reduced activity, HCWs had reduced exposure as ‘2/3 staff [were sent] on extraordinary leave’.
The issue of testing of symptomatic staff was raised by a number of respondents with some stating that there was access to rapid polymerase chain reaction (PCR) testing: ‘PCR performed for medical staff if symptoms [were present]’ or that ‘detection kits [were] available’. Others stated that HCWs at risk or in contact with COVID-19 patients had daily occupational health assessments. Others stressed the importance of ‘aggressive contact tracing’.
Self-isolation for travelling doctors: some of the respondents specifically mentioned that ‘if a doctor comes from abroad, he/she is put in home quarantine for 14 days’ or ‘quarantine for all staff who have travelled out’.
Some respondents described shielding protocols in their countries for vulnerable staff with ‘HCWs involved in providing care to confirmed COVID-19 patients should not [have a]… high risk condition/immunocompromised illness, e.g. uncontrolled diabetes mellitus, chronic lung, liver or kidney disease, malignancy, HIV infection, and/or not on prolonged steroids or immunosuppressant treatment and non-pregnant’.
One respondent noted that there was a policy in place implementing a ‘psychological support team’ for staff tested or concerned about developing COVID-19 disease.
Communication to staff
Several respondents noted policy in the hospital to improve communication with staff such as ‘regular almost daily updates by SMS or email; on symptoms, cases per area and treatment protocols’ with others citing regular updates and guidelines by national associations.
Visitor and outpatient policies
In most countries, respondents reported that all visitors or those attending for outpatient appointments ‘have to answer a questionnaire and their temperatures are checked’, with high-risk patients not allowed entry to the hospital and ‘turned away to the specific centres dealing with COVID-19’.
Overall, 20 out of 22 (91%) respondent countries reported cancelling or reducing routine outpatient clinics. Some respondents stated that ‘appointments are prioritised by medical case note review and delayed where possible’. Others described a change in practice such that ‘all of our patients are screened by phone prior to coming to the clinic’ and that ‘routine outpatient appointments switched to virtual clinics’.
Where outpatients were seen, 8/22 (36%) respondents described that arrangements were in place to screen all clinic attendants by temperature assessment and/or specific questionnaire. Four of the respondents noted that all patients attending the outpatient clinic were required to wear masks and 10/22 stated that medical staff in outpatients were required to wear masks (in some cases an FFP2/N95 mask).
A number of respondents reported the measures in place for all outpatients and visitors to maintain social distancing (ranging from a minimum of 1 m, through 1.5 m, up to 2 m) and to use hand sanitizer or wash their hands.
Some respondents reported that all visitors to hospitals were prevented from entering until further notice.
Trauma and emergency care
While respondents reported that ‘trauma cases are down as people stay at home’ due to national ‘lockdowns’, others stated that ‘all cases are seen with full PPE precautions. High risk cases were also tested before trauma treatment. If positive, referred to specialist COVID-19 centres for trauma treatment’. Others used a risk-based approach with ‘trauma patients screened for travel history and temperature; if positive, treated in COVID-19 centres with full precautions’. With regional organization in response to COVID-19, some hospitals had ‘stopped receiving trauma’, some had modified practice such as ‘life and limb emergencies treated only’ or ‘more nonoperative management’. A number of other centres reported ‘no change to routine practice’.
Some respondents noted the importance of ‘minimizing [the] length of stay at hospital’ to reduce infection risk to patients and that this was aided by the fact that ‘elective lists used for trauma to minimize waiting time and to empty hospitals’.
Some respondents reported that ‘trauma clinics were set up away from the main hospital’ and emergency departments.
Care in the operating room
Some respondents reported that COVID-19 patients ‘will only be operated by the COVID-19 teams set up in each department in full PPE’ and that they have specially designated COVID-19 operating rooms with ‘negative pressure’. Others report policy that all COVID-19 patients should be operated ‘in laminar flow’ ventilated operating rooms.
A number of respondents reported that it was policy to ‘PCR pre-op to diagnose asymptomatic patients’ that are scheduled to go to the operating room.
Others stated that special precautions were taken in the operating room for patients with COVID-19. Of particular concern were issues around the anaesthetic. Several respondents outlined policy to avoid general anaesthesia. With, where possible, ‘all cases done under spinal anaesthesia’. Some stated that where intubation was needed ‘videoscope aided intubation’ should be used and that ‘glasses protection or face shield and N95 masks’ should be used ‘in intubation’.
General operating room etiquette was to be reinforced with respondents stating that ‘masks and gloves worn by all’ and that there be ‘minimal staff in theatre’. Additional PPE policy was in place according to a number of respondents that included the standard PPE for the operating room including eye protection and ‘surgeons wear FFP2 (mask)’ and ‘triple gloves’.
Discussion
The results from this study suggest HCWs could represent 14% to 16% of the infected population and are therefore at a disproportionate risk to the rest of the population. Globally, there is substantial variation in measures taken to protect HCWs, and some valuable lessons to learn.
The media has recently highlighted HCW concerns over contracting COVID-19 at work. Their concerns are valid as some countries nearing the peak of their infection, such as Spain, have reported that 13% to 14% of the country’s cases are in HCWs.14,15 Similar reports were documented in China. At the start of the outbreak in Wuhan, a hospital reported that 40/138 patients (29%) were HCWs.16 Another study in Wuhan reported the infection rate of orthopaedic surgeons was between 1.5% to 20.7%, and found that the peak onset of infection was eight days earlier than that of the public, suggesting nosocomial rather than community infection.17 High-exposure risks,18 inadequate protection measures,19 and health system unpreparedness appear to be important factors responsible for the increased risk in HCWs.20 The increased risk of infection to HCWs has also been documented in previous disease outbreaks.21,22
Although this study shows variation in measures taken to protect HCWs, it also demonstrates common themes. Before the COVID-19 pandemic, in response to previous outbreaks, Hong Kong had developed a robust infrastructure and policy to be implemented immediately should another outbreak occur.23,24 In response to the COVID-19 pandemic, other countries also rapidly instituted simple and evidence-based public health measures to minimize transmission to HCWs.1,25 The effects of these measures are seen in the answers from respondents in this study. A broad spectrum of practices and policies are reported in our results, with some respondents reporting that their countries (e.g. Hong Kong and Singapore) implemented and adhered to strict regulations early.26 Policies included risk stratification e.g. questioning and temperature recordings of all patients, visitors and HCWs entering the hospital. Time will tell whether these policies will be successful in protecting HCWs, but early impressions suggest they offer benefit. Some of the social isolation and lockdown policies implemented for COVID-19 resemble the traffic-control bundling protocols that were successfully developed during the SARS outbreak.27
Respondents in this study highlighted the importance of communication of COVID-19 guidelines and education for HCWs (e.g. in Hong Kong and Malaysia). Training schemes like these have also been used in China and South Korea to reduce transmission of the infection.1,17,28 Additionally, strategies have been implemented to protect the education and training of residents in the USA, while also reducing their exposure through rotating teams on 'active duty' or 'working remotely' with phase transitions every two weeks, which has been described in detail by Schwartz et al.29 Education can also be delivered through online streaming (e.g. Singapore).26
PPE has been in critically short supply globally.5,30 The respondents in this study have suggested ways to stratify risk to HCWs (through levels) to conserve the supply of PPE. Initial reports from China have also provided guidance.19 The US Centers for Disease Control and Prevention (CDC) and other professional bodies released guidance on context-dependent appropriate usage of PPE in response to COVID-19.31,32 With limited supplies, advice about re-using and repurposing equipment has also been provided.33 Additionally, methods for dealing with surges in demand from previous infectious disease outbreaks have previously been documented and have informed policy during the COVID-19 outbreak.34 Policies surrounding mask usage vary, with some countries introducing mass-masking (e.g. China), but due to a thin evidence-base, guidance in other countries have been slow.35
The respondents in our study report that several countries have adopted surveillance schemes of HCWs during the COVID-19 pandemic. Others have emphasized the importance of supporting psychological wellbeing of HCWs at a time of extreme stress. Advocacy to provide social and mental health support have been well documented in the literature.27,36,37 Wellbeing advice has included shorter working hours, regular rest periods, and rotating shifts for those working in high-risk areas.37
The respondents to our study reported that most countries affected by the pandemic stopped non-urgent outpatient work and surgery. Some reported that they were able to introduce telemedicine or ‘virtual’ consultations, which received reimbursement in the USA.38 In a new style of practicing medicine, helpful guidance has been issued on the appropriate use of video consultations.39-41 This transition potentially minimizes transmission risk to HCWs. The positive consequences of these practices for elective and non-urgent care have been well documented in Singapore.26
Defining non-urgent care has been controversial. The American College of Surgeons recently released a triaging framework to assist with decision-making, and the Elective Surgery Acuity Scale (ESAS) intended to be applied on a case-by-case basis.42 The Royal College of Surgeons have also advised that triage should avoid “blanket policies” but rather rely on a day-by-day, data-driven assessment of the changing risk–benefit analysis, taking into account expert clinical opinion and a site-specific granular understanding of the logistical issues at play.43 Additionally, the National Health Service in the UK released in-depth guidance for many specialties on approaches to urgent and non-urgent care.44 There has been variable uptake of this guidance.45
This study highlights novel practice in urgent care during the COVID-19 pandemic. Pre-operative testing of all patients undergoing urgent procedures is one such area. Some countries have adopted this on a universal basis (e.g. Hong Kong) or a selective basis for patients with exposure history or symptoms (e.g. USA). The COVID-19 causative virus, SARS-CoV-2, has been associated with aerosol transmission and nosocomial spread,11 and practical recommendations for critical care and anaesthesiology teams have been reported.46 In several settings in our study, protocols were followed to minimize the risk of transmission through aerosol-generating procedures. These included enhanced PPE, minimization of personnel in procedures, and using videoscope-aided intubation. Tracheal intubation, non-invasive ventilation, and manual ventilation before intubation have all been found to expose HCWs to a higher risk.9,46 Several professional bodies have released guidance on special PPE precautions during procedures with higher risk.32 Surgeons may also be at a substantial risk through the use of power tools,10 and other force-generating instruments generating tissue spray (e.g. in orthopaedic surgery).8 Helpful guidance in minimizing infection risk has been published by the European Centre for Disease Prevention and Control.47
The authors acknowledge the non-uniformity and selection bias limitations associated with non-random convenience sampling in surveys, while recognizing the generalizability and internal and external validity of the survey approach. The sample size is relatively low but does not include response bias as 100% of those surveyed responded. There is likely to be variability in the practices observed between different surgeons, hospitals, and regions with varying prevalence. However, the authors have selected countries to sample from to establish breadth in points of view.
Conclusion
Based on the responses in this study, collating examples of best and sometimes novel practice, the authors are able to make the following recommendations.
-
COVID-19 should be treated in specialized, resourced, and potentially dedicated centres. A regional approach should be taken to treating COVID-19. Designated centres should have an adequate complement of trained staff, recommended equipment and evidence-based policies for the treatment of COVID-19.
-
Standardized, high-quality, evidence-based PPE should be available to all staff. An example policy would be based upon three risk levels:
-
Level 1 (low risk, in the ED area where no suspected COVID-19 (e.g. unrelated injury and no COVID-19 symptoms) patients are managed): FFP1 surgical masks, eye protection, disposable apron, wrist length gloves.
-
Level 2 (medium risk, in the ED area where suspected COVID-19 (e.g. respiratory symptoms and/or fever) patients are treated and OR: as above, with changeable clothes (scrubs), impermeable gowns, visors, and FFP 2 (N95) masks.
-
Level 3 (high-risk, treating confirmed COVID-19 patients): as above but isolation suits over all clothes and sealed extraction hoods or helmets where available.
-
-
Protecting and supporting staff should be paramount. Example policies could include:
-
Rotating teams: minimize number of staff exposed at one time.
-
Extraordinary leave: staff who do not need to be at work should be at home.
-
Shielding: all at-risk staff with pre-existing conditions should self-isolate.
-
Testing: all staff with any symptoms should be rapidly tested and if positive they should self-isolate.
-
Support: psychological support should be available for all HCWs.
-
-
Communication: regular or even daily communication of the all relevant information and guidance by email and/or SMS should take place.
-
Screening: visitors, outpatients and preoperative patients should be screened for COVID-19, either by temperature and questionnaire assessment or where possible, laboratory testing.
-
Reduction in outpatient activity: instituting virtual or teleconferencing clinics in place of face-to-face clinics where possible.
-
Reduction in operating room activity: non-urgent operations should be postponed until after the pandemic.
-
Emergency OR policy should be consistent and robust. Examples of good policy may include:
-
Only real emergencies should attend the operating room at the peak of the pandemic.
-
Patients attending emergency OR should be screened.
-
The OR should have the minimal number of staff.
-
Level 2 PPE needed for all staff in the OR, level three if COVID-19-positive patient.
-
Avoid general anaesthesia in COVID-19 patients where possible.
-
COVID-19 presents a disproportionate risk to HCWs, potentially resulting in a diminished health system capacity, and consequently an impairment to population health. Implementation of these recommendations at an international level could provide a framework to reduce this burden.
References
1. Adhikari SP , Meng S , Wu YJ , et al. Epidemiology, causes, clinical manifestation and diagnosis, prevention and control of coronavirus disease (COVID-19) during the early outbreak period: a scoping review . Infect Dis Poverty . 2020 ; 9 ( 1 ): 29 . doi: https://doi.org/10.1186/s40249-020-00646-x PubMed Crossref Google Scholar
2. Coronaviridae Study Group of the International Committee on Taxonomy of V . The species Severe acute respiratory syndrome-related coronavirus: classifying 2019-nCoV and naming it SARS-CoV-2 . Nat Microbiol . 2020 ; 5 ( 4 ): 536 – 544 . doi: https://doi.org/10.1038/s41564-020-0695-z PubMed Crossref Google Scholar
3. Guo YR , Cao QD , Hong ZS , et al. The origin, transmission and clinical therapies on coronavirus disease 2019 (COVID-19) outbreak - an update on the status . Mil Med Res . 2020 ; 7 ( 1 ): 11 . doi: https://doi.org/10.1186/s40779-020-00240-0 PubMed Crossref Google Scholar
4. Organization WH . Rolling updates on coronavirus disease (COVID-19) . 2020 . https://www.who.int/emergencies/diseases/novel-coronavirus-2019/events-as-they-happen Google Scholar
5. Ranney ML , Griffeth V , Jha AK . Critical Supply Shortages - The Need for Ventilators and Personal Protective Equipment during the Covid-19 Pandemic . N Engl J Med . 2020 ; 382 ( 18 ): e41 . doi: https://doi.org/10.1056/NEJMp2006141 PubMed Crossref Google Scholar
6. Liu Y , Yan L-M , Wan L , et al. Viral dynamics in mild and severe cases of COVID-19 . Lancet Infect Dis . 2020 . doi: https://doi.org/10.1016/S1473-3099(20)30232-2 Crossref PubMed Google Scholar
7. Iacobucci G . Covid-19: all non-urgent elective surgery is suspended for at least three months in England . BMJ . 2020 ; 368 : m1106 . doi: https://doi.org/10.1136/bmj.m1106 PubMed Crossref Google Scholar
8. Raphael T . Why Surgeons Don't Want to Operate Right Now . 2020 . https://www.bloomberg.com/opinion/articles/2020-03-24/the-coronavirus-crisis-is-putting-surgeons-at-risk-too Google Scholar
9. Tran K , Cimon K , Severn M , Pessoa-Silva CL , Conly J . Aerosol generating procedures and risk of transmission of acute respiratory infections to healthcare workers: a systematic review . PLoS One . 2012 ; 7 ( 4 ): e35797 . doi: https://doi.org/10.1371/journal.pone.0035797 PubMed Crossref Google Scholar
10. Wenner L , Pauli U , Summermatter K , et al. Aerosol Generation During Bone-Sawing Procedures in Veterinary Autopsies . Vet Pathol . 2017 ; 54 ( 3 ): 425 – 436 . doi: https://doi.org/10.1177/0300985816688744 PubMed Crossref Google Scholar
11. van Doremalen N , Bushmaker T , Morris DH , et al. Aerosol and Surface Stability of SARS-CoV-2 as Compared with SARS-CoV-1 . N Engl J Med . 2020 ; 382 ( 16 ): 1564 – 1567 . doi: https://doi.org/10.1056/NEJMc2004973 PubMed Crossref Google Scholar
12. O'Brien BC , Harris IB , Beckman TJ , Reed DA , Cook DA . Standards for reporting qualitative research: a synthesis of recommendations . Acad Med . 2014 ; 89 ( 9 ): 1245 – 1251 . doi: https://doi.org/10.1097/ACM.0000000000000388 PubMed Crossref Google Scholar
13. Saccone M . More than 500 Massachusetts hospital workers test positive for COVID-19 . 2020 . https://www.boston25news.com/news/local/more-than-500-massachusetts-healthcare-workers-test-positive-covid-19/2B5BNFQTHJFXBGD7VNBBPFVDSU/ Google Scholar
14. Jones S . Spain: doctors struggle to cope as 514 die from coronavirus in a day . 2020 . https://www.theguardian.com/world/2020/mar/24/spain-doctors-lack-protection-coronavirus-covid-19 Google Scholar
15. NUGENT C . 'It's Like Being a War Medic.' A Madrid Doctor Speaks Out About Grave Shortages in Protective Gear . 2020 . https://time.com/5813848/spain-coronavirus-outbreak-doctor/ Google Scholar
16. Wang D , Hu B , Hu C , et al. Clinical Characteristics of 138 Hospitalized Patients With 2019 Novel Coronavirus-Infected Pneumonia in Wuhan, China . JAMA . 2020 : 1061 . doi: https://doi.org/10.1001/jama.2020.1585 PubMed Crossref Google Scholar
17. Guo X , Wang J , Hu D , et al. Survey of COVID-19 Disease Among Orthopaedic Surgeons in Wuhan, People’s Republic of China . The Journal of Bone and Joint Surgery . 2020 : 1 . doi: https://doi.org/10.2106/JBJS.20.00417 Google Scholar
18. Koh D . Occupational risks for COVID-19 infection . Occup Med (Lond) . 2020 ; 70 ( 1 ): 3 – 5 . doi: https://doi.org/10.1093/occmed/kqaa036 PubMed Crossref Google Scholar
19. Zhang Z , Liu S , Xiang M , et al. Protecting healthcare personnel from 2019-nCoV infection risks: lessons and suggestions . Front Med . 2020 . doi: https://doi.org/10.1007/s11684-020-0765-x PubMed Crossref Google Scholar
20. Bernstein L , Boburg S , Sacchetti M , Brown E . Covid-19 hits doctors, nurses and EMTs, threatening health system . 2020 . https://www.washingtonpost.com/health/covid-19-hits-doctors-nurses-emts-threatening-health-system/2020/03/17/f21147e8-67aa-11ea-b313-df458622c2cc_story.html Google Scholar
21. Suwantarat N , Apisarnthanarak A . Risks to healthcare workers with emerging diseases: lessons from MERS-CoV, Ebola, SARS, and avian flu . Curr Opin Infect Dis . 2015 ; 28 ( 4 ): 349 – 361 . doi: https://doi.org/10.1097/QCO.0000000000000183 PubMed Crossref Google Scholar
22. Shoman H , Karafillakis E , Rawaf S . The link between the West African Ebola outbreak and health systems in Guinea, Liberia and Sierra Leone: a systematic review . Global Health . 2017 ; 13 ( 1 ): 1 . doi: https://doi.org/10.1186/s12992-016-0224-2 PubMed Crossref Google Scholar
23. Apisarnthanarak A , Mundy LM , Tantawichien T , Leelarasamee A . Infection Prevention and Control in Asia: Current Evidence and Future Milestones . Clin Infect Dis . 2017 ; 64 ( suppl_2 ): S49 – S50 . doi: https://doi.org/10.1093/cid/cix071 PubMed Crossref Google Scholar
24. Wong ATY , Chen H , Liu SH , et al. From SARS to Avian Influenza Preparedness in Hong Kong . Clin Infect Dis . 2017 ; 64 ( suppl_2 ): S98 – S104 . doi: https://doi.org/10.1093/cid/cix123 PubMed Crossref Google Scholar
25. Wu X , Zhou H , Wu X , Huang W , Jia B . Strategies for qualified triage stations and fever clinics during the outbreak of COVID-2019 in the county hospitals of Western Chongqing . J Hosp Infect . 2020 . doi: https://doi.org/10.1016/j.jhin.2020.03.021 PubMed Crossref Google Scholar
26. Chang Liang Z , Wang W , Murphy D , Po Hui JH , Coronavirus N . And orthopaedic surgery: early experiences from Singapore . The Journal of bone and joint surgery American volume . 2020 . Google Scholar
27. Schwartz J , King CC , Yen MY . Protecting Health Care Workers during the COVID-19 Coronavirus Outbreak -Lessons from Taiwan's SARS response . Clin Infect Dis . 2020 . doi: https://doi.org/10.1093/cid/ciaa255 PubMed Google Scholar
28. Huh S . How to train the health personnel for protecting themselves from novel coronavirus (COVID-19) infection during their patient or suspected case care . J Educ Eval Health Prof . 2020 ; 17 : 10 . doi: https://doi.org/10.3352/jeehp.2020.17.10 PubMed Google Scholar
29. Schwartz AM , Wilson J , Boden SD , et al. Managing resident workforce and education during the COVID-19 pandemic: evolving strategies and lessons learned . The Journal of Bone & Joint Surgery . 2020 . Crossref PubMed Google Scholar
30. Rimmer A . Covid-19: GPs call for same personal protective equipment as hospital doctors . BMJ . 2020 ; 368 : m1055 . doi: https://doi.org/10.1136/bmj.m1055 PubMed Crossref Google Scholar
31. CfDCa P . Isolation Precautions . 2007 . https://www.cdc.gov/infectioncontrol/guidelines/isolation/ Crossref PubMed Google Scholar
32. CfDCa P . Interim Infection Prevention and Control Recommendations for Patients with Suspected or Confirmed Coronavirus Disease 2019 (COVID-19) in Healthcare Settings . 2020 . https://www.cdc.gov/coronavirus/2019-ncov/infection-control/control-recommendations.html#adhere Google Scholar
33. CfDCa P . Strategies for Optimizing the Supply of N95 Respirators . 2020 . https://www.cdc.gov/coronavirus/2019-ncov/hcp/respirators-strategy/index.html Google Scholar
34. Hick JL , Barbera JA , Kelen GD . Refining surge capacity: conventional, contingency, and crisis capacity . Disaster Med Public Health Prep . 2009 ; 3 ( 2 Suppl ): S59 – S67 . doi: https://doi.org/10.1097/DMP.0b013e31819f1ae2 PubMed Crossref Google Scholar
35. Leung CC , Lam TH , Cheng KK . Mass masking in the COVID-19 epidemic: people need guidance . Lancet . 2020 ; 395 ( 10228 ): 945 . doi: https://doi.org/10.1016/S0140-6736(20)30520-1 PubMed Crossref Google Scholar
36. Chen Q , Liang M , Li Y , et al. Mental health care for medical staff in China during the COVID-19 outbreak . Lancet Psychiatry . 2020 ; 7 ( 4 ): e15 – e16 . doi: https://doi.org/10.1016/S2215-0366(20)30078-X PubMed Crossref Google Scholar
37. Ho CS , Chee CY , Ho RC , CS H , RC H . Mental health strategies to combat the psychological impact of COVID-19 beyond paranoia and panic . Ann Acad Med Singapore . 2020 ; 49 ( 3 ): 1 – 3 . Google Scholar
38. AHIP . Statement by the AHIP Board of Directors: Taking Action to Address Coronavirus COVID-19 . 2020 . https://www.ahip.org/statement-by-the-ahip-board-of-directors-taking-action-to-address-coronavirus-covid-19/?utm_term=statement&utm_campaign=AHIP%20Board%20of%20Directors%20Releases%20Statement%20Addressing%20Coronavirus%20%2F%20Updates%20on%20Coronavirus%20Response%20%2F%20AHIP%20Releases%20Report%20of%20Impact%20to%20MA%20Advanced%20Notice%20%2F%20AHIP%20Podcast%20Builds%20Thought%20Leadership&utm_content=email&utm_source=Act-On+Software&utm_medium=email Google Scholar
39. Hollander JE , Carr BG . Virtually Perfect? Telemedicine for Covid-19 . N Engl J Med . 2020 ; 382 ( 18 ): 1679 – 1681 . doi: https://doi.org/10.1056/NEJMp2003539 PubMed Crossref Google Scholar
40. Greenhalgh T , Wherton J , Shaw S , Morrison C . Video consultations for covid-19 . BMJ . 2020 ; 368 : m998 . doi: https://doi.org/10.1136/bmj.m998 PubMed Google Scholar
41. Smith AC , Thomas E , Snoswell CL , et al. Telehealth for global emergencies: implications for coronavirus disease 2019 (COVID-19) . J Telemed Telecare . 2020 ; 1357633X : 20916567 . Crossref PubMed Google Scholar
42. ACo S . COVID-19: Guidance for Triage of Non-Emergent Surgical Procedures . 2020 . https://www.facs.org/covid-19/clinical-guidance/triage Google Scholar
43. RCoSo E . COVID-19: good practice for surgeons and surgical teams. 2020 . 2020 . https://www.rcseng.ac.uk/standards-and-research/standards-and-guidance/good-practice-guides/coronavirus/covid-19-good-practice-for-surgeons-and-surgical-teams/ (date last accessed accessed May 03 2020 ). Google Scholar
44. NEaNI C . Specialty guides for patient management . 2020 . https://www.england.nhs.uk/coronavirus/publication/specialty-guides/ Google Scholar
45. Farr C . Hospitals are still scheduling elective procedures during coronavirus crisis . and frontline medical workers fear they’re infecting patients . 2020 . https://www.cnbc.com/2020/03/20/hospitals-still-scheduling-elective-surgery-during-coronavirus-crisis.html Google Scholar
46. Wax RS , Christian MD . Practical recommendations for critical care and anesthesiology teams caring for novel coronavirus (2019-nCoV) patients . Can J Anaesth . 2020 ; 67 ( 5 ): 568 – 576 . doi: https://doi.org/10.1007/s12630-020-01591-x PubMed Crossref Google Scholar
47. Control ECfDPa . Infection prevention and control for COVID-19 in healthcare settings . 2020 . https://www.ecdc.europa.eu/sites/default/files/documents/COVID-19-infection-prevention-and-control-healthcare-settings-march-2020.pdf Google Scholar
Author contributions
Z. Hussain: Carried out literature search, Produced the figures, Designed the study, Carried out data collection, analysis, and interpretation, Wrote the paper.
P. Yau: Designed the study, Collected and interpreted the data, Wrote the manuscript.
H. Shoman: Carried out literature search, Created the figures, Designed the study, Collected, analyzed, and interpreted the data, Wrote the paper.
G. Thevendran: Designed the study, Collected and interpreted the data collection, Wrote the paper.
F. Randelli: Designed the study, Collected and interpreted the data, Wrote the paper.
M. Zhang: Designed the study, Collected and interpreted the data, Wrote the paper.
A. Norrish: Designed the study, Collected and interpreted the data, Wrote the paper.
V. Khanduja: Carried out the literature search, Created the figures, Designed the study, Collected, analyzed, and interpreted the data, Wrote the paper.
Funding statement
The project (20-054) was supported by a literature grant from the ON Foundation, Switzerland.
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
Acknowledgements
The authors would like to acknowledge the help of all their collaborators who gave up their time despite their busy schedule to participate in this survery. Patricia Fucs MD, Santa Casa Medical School and Hospitals, São Paulo, Brazil; Mike Held MD PhD, University of Cape Town, South Africa; Fabio Valerio Sciarretta MD, Clinica Nostra Signora della Mercede, Roma, Italy; Seow Hui Teo MBBS, MRCS, MS (Ortho), National Orthopaedic Centre of Excellence in Research and Learning (NOCERAL), University of Malaya, Kuala Lumpur, Malaysia; Kyung-Hoi Koo MD, Seoul National University Bundang Hospital, South Korea; Shin-Yoon Kim MD, PhD, Kyungpook National University Hospital, Daegu, South Korea; Thami Benzakour MD, Casablanca Morocco; Allan Mishra MD, Stanford University Medical Centre, Stanford, USA.; Fernando Rosa MD, Brazil; Hatem Galal Said MD, Assiut University Hospital, Egypt; Athanasios Papavasiliou BSc, MD, PhD, Interbalkan European Medical Center, Thessaloniki, Greece; Aala Ahmed MD, Annajah university, Palestine; Rohit Amritanand MS (Orth), MAMS, FACS, Christian Medical College, Vellore, Tamil Nadu, India; Umer Butt MD, MRCS, FRCS (T&O), AO hospital, Karachi, Pakistan; Oliver Marin-Peña MD, Hospital Universitario Infanta Leonor, Madrid, Spain; Afshin Taheriazam, Tehran Medical Sciences, Islamic Azad University, Tehran, Iran; Mohamed Sukeik MD (Hons), FRCSEd (Tr&Orth), PGA MD (Res), Dr Sulaiman Al Habib Hospital, Al Khobar, Kingdom of Saudi Arabia; Parminder Singh MBBS, MRCS, FRCS(Tr&Orth), MS, FRACS, Maroondah Hospital, Monash & Deakin University, Melbourne, Australia; Naoki Nakano MD, PhD, Kobe University Graduate School of Medicine, Kobe, Japan; Fred Otsyeno FCS (ECSA), SICOT Dip, MMED, MBChB, Kenyatta National Hospital, Nairobi, Kenya; Wei Chen MD, The Third Hospital of Hebei Medical University, Shijiazhuang, P. R. China.
Follow Z. B. Hussain @zaaminhussain
Follow H. Shoman @haitham_shoman
Follow V. Khanduja @CambridgeHipDoc
© 2020 Author(s) et al. This is an open-access article distributed under the terms of the Creative Commons Attributions licence (CC-BY-NC-ND), which permits unrestricted use, distribution, and reproduction in any medium, but not for commercial gain, provided the original author and source are credited.









