Abstract
In the UK we have many surgeon inventors – surgeons who innovate and create new ways of doing things, who invent operations, who design new instruments to facilitate surgery or design new implants for using in patients. However truly successful surgeon inventors are a rare breed and they need to develop additional knowledge and skills during their career in order to push forward their devices and innovations. This article reviews my own experiences as a surgeon inventor and the highs and lows over the whole of my surgical career.
1975: The Portex Toenail Treatment kit (Fig. 1)

Fig. 1
Portex Toenail Treatment Kit (Portex 1979).
My first invention was developed in 1975 while working in the Accident and Emergency (A& E) Department at Newcastle General Hospital. The A& E Department was run by a unique consultant – David Milne, who was trained as a General Surgeon and self-trained also as an Orthopaedic Surgeon. David, who has recently died, was responsible for stimulating a whole generation of young surgeons into entering surgery and inspiring innovation. Within the A& E Department we carried out minor operations and I learned how to carry out amongst others wedge resections, nail avulsions and surgical nail-bed ablation operations. Phenol ablation was just coming in at that time. My colleague registrar, Terry Andrew and I felt that this kind of surgery was excessively destructive and, my mother, a General Practitioner in Dundee, had told me how she had successfully treated ingrowing toenails in the past by inserting cotton wool along the edge of the toenail. I therefore designed “The Portex Toenail Treatment Kit” which involved designing an introducer for a plastic “gutter” which was inserted along the lateral edge of the toenail under local anaesthetic. The gutter was retained for about two months while the ingrowing toenail healed. We published our paper on the effectiveness of this treatment in the British Medical Journal (BMJ) in 19791 and Portex started marketing the Portex Toenail Treatment Kit in that year. It was a struggle to persuade Portex to take this on, but because the kit was developed from a minor modification of one of their intravenous cannula sets the cost implications were relatively small and the regulatory processes in 1979 were far simpler than they are today. Unfortunately the Portex Toenail Treatment Kit was a commercial disaster. Very few were sold, despite having a supportive paper published in the BMJ and I learned later that the reason was that the device did not have a credible “Product Champion”. I was a mere surgical registrar and when I did present a lecture on ingrowing toenails it was ignored by the Consultant body at that time.
1989: The Interax Knee (Fig. 2)

Fig. 2
Interax Total Knee Replacement (Howmedica 1989).
I was appointed Professor of Orthopaedic & Accident Surgery in 1986, replacing Professor William Waugh, an international expert on knee surgery and knee replacement. I was approached by Dr Aki Hoshino, a young Japanese registrar who wished to come to Nottingham to conduct some joint research. Under my supervision he conducted a project focussing on the “Impact-absorbing properties of the human knee” funded with a research grant from Howmedica and we published our results in the Journal of Bone and Joint Surgery [Br] in 1987.2 At that time Howmedica International decided to develop a new design of knee replacement and as a consequence of Aki's research, I was invited by Eddie Slater, Martin Wilkins, Peter Lawes, Alan Ashby and Brendan McGrath from Howmedica to join a group of ten surgeons – the “International Knee Development Group” to work on the design of a new uncemented knee replacement which would utilise a new mesh surface covered with hydroxyapatite coating and designed to promote osseo-integration. The group members were:- Aki Hoshino (Japan), Lindsay Laird (Australia), Maurilio Marcacci (Italy), Marc Martens (Belgium), Luis Munuera (Spain), Carl Wirth (Germany), Daniel Molé (France), Veijo Vahvanen (Finland), Denny Desjardins (Canada) and myself. The first meeting of the International Knee Development Group was held in the Waldorf Hotel, London on 11th and 12th September 1989 and we had regular annual meetings for the next 10 years. The Interax Knee was created and I was the first surgeon in the world to insert an Interax uncemented knee in Nottingham on 15th February 1991. We held our First International Symposium to launch the Interax Knee a year later at the London Hilton on Park Lane on 6th & 7th February 1992 (Fig. 3). The other major innovation we developed was individual medial and lateral meniscal bearings and, later a one-piece composite mobile meniscus called the ISA (Integrated Secure Asymmetric) tibial bearing, which has become very successful indeed. Our Intellectual Property was recognised with a formal royalty agreement between Howmedica and the University of Nottingham (which received 10% of the total group of surgeon's royalties) and I received from the University a sliding scale of the University Royalties up to 50% with the University retaining the balance. The ten team members were effectively “Product Champions”, attending international meetings to talk about the Interax Knee and ensuring that it had a high profile. Although this was hard work, it was enjoyable, and at that time partners were occasionally invited to join the research group – the rules have all changed since.

Fig. 3
Angus Wallace and Martin Wilkins at theFirst International Symposium to launch the Interax Knee a year the London Hilton on Park Lane on 6th & 7th February 1992.
Although the original single meniscal bearings included design features that improved knee range of movement they were subsequently shown in our clinical trials to be associated with excessive wear, and modifications were required. In the meantime Howmedica was taken over by Stryker, and Stryker decided to rationalise their knee arthroplasty products. As a consequence an announcement was made at our annual Interax Collaborators Group meeting on 3-4 March 2000 in London that the Interax Knee was to be merged with the Stryker Kinemax knee system. As a consequence of this announcement Luis Munuera and I met formally with Andre Cardenoso and Declan Slemon, representing Stryker at the Hilton Airport Hotel, Charles de Gaulle airport on Tuesday 21 March 2000. We reported after the meeting in a letter to our colleagues:-
“Gentlemen, the situation is this. With the Stryker acquisition of Howmedica, Stryker have decided to rationalise their knee replacement marketing strategy world-wide. They have too many different knee systems and this is harming their marketing opportunities.
“The logical change for Europe is to merge the Kinemax and Interax knee systems over the next 3 to 5 years. The most important part of that merger is to put the ISA (Integrated Secure Asymmetric) meniscus onto the Kinemax knee. However they have a problem with that merger in relation to their collaborating surgeons. The Kinemax Active Collaborating Surgeons are all appointed on Consultancy Agreements and do not hold royalties (except for one of the originators). This is quite different from the Interax Collaborating Surgeons who do not hold Consultancy Agreements but instead have Royalty Agreements. Stryker have a policy of NOT offering Royalty Agreements to Surgeons apart from exceptional situations. Stryker will NOT be offering the Interax Collaborating Surgeons any future Royalty Agreements but will honour all previously agreed Royalty Agreements.
“The Way Forward
Andre Cardenoso and Declan Slemon plan to meet with each of you during the next 3 weeks to discuss with you your personal Consultancy Agreement for the next 2 years. As part of that Consultancy Agreement they wish to build in a stronger “surgeons commitment” to the contract because they perceive, from some of our group, a less than optimal commitment to the needs of the company. Both Angus and Luis understand and sympathise with that view. Andre and Declan also recognise that during the last year the commitment from Howmedica/Stryker has been less than ideal, but that is now past.”
Unfortunately the Stryker solution to the problem of our royalties was that they transferred the successful ISA (Integrated Secure Asymmetric) tibial bearing onto the Kinemax knee, re-branded it and no subsequent royalties were paid to the Interax surgeons after 2002. This did not go down well with the Interax surgeons.
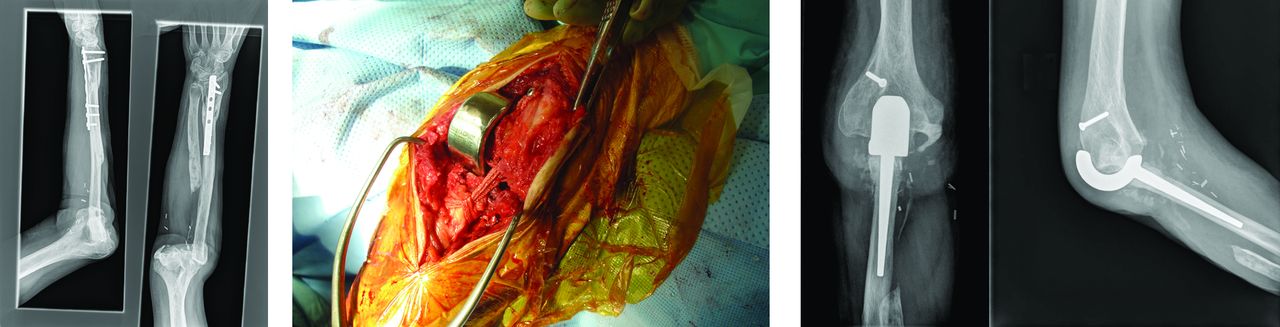
1989: The Nottingham Shoulder (Fig. 4)

Fig. 4
Nottingham Shoulder Replacement (Biomet 1993).
On a ward round at Harlow Wood Orthopaedic Hospital in 1989 I suggested to Simon Roberts and Heather Swallow, two of my SHOs, that they should carry out a research project on looking at the shape of the humeral head as I was having significant difficulty carrying out internal fixation of humeral neck fractures with Kirschner (K-) wires and often missed the head with the end of the wires. I thought it was possible that the humeral head did not sit squarely on the top of the humeral shaft. Simon and Heather set up a research project and took a number of humerii from the Anatomy department at the University of Nottingham to a company in Sheffield and carried out detailed measurements of the shape of the humeral head and the relationship of the humeral head to the upper humeral shaft. Both Simon and Heather were developing their careers and I encouraged them to present their research at a number of research meetings in 1990 – The British Association of Clinical Anatomists,3 the British Elbow & Shoulder Society4 and the European Society for Surgery of the Shoulder and Elbow in Milan.5 Heather Swallow presented our findings in Milan and a young shoulder surgeon spoke to her after her presentation. He was crestfallen as he had embarked on a similar project in France and we had presented our results ahead of his own. His studies however were more detailed and were later published in 1997.6 Unfortunately, by presenting our research findings publicly in 1990 I made a serious error. We had made the novel observation, not previously reported, that the humeral head was not placed in line with the humeral shaft, but was offset posteriorly. We therefore recommended that, in future, shoulder prosthesis should be designed with the humeral head offset posteriorly (achieved by indexing the head on the stem) which has now been adopted by all shoulder arthroplasty designers. If we had patented this design, before presenting our results publicly, we would have been able to patent the design and benefit financially from this development, but because we went public in advance we could not patent the new designs. Our research was published in the Journal of Bone and Joint Surgery [Br] in 1991.7
In 1989 I approached Biomet, a joint replacement company, to seek support for developing a shoulder replacement with a posteriorly offset humeral head. David Dines, a shoulder surgeon based at the Hospital for Special Surgery in New York, had developed the Biomodular shoulder arthroplasty system, and he very kindly agreed to us using his stem design (modified with a shiny distal stem) for the Nottingham Shoulder replacement system. On 10th May 1991 I inserted the first ever offset humeral head (as a prototype) in one of my Nottingham patients and on 29th October 1993 we launched the Nottingham Shoulder Arthroplasty system with its new polished distal stem. The unique features of the Nottingham Shoulder Arthroplasty system were the offset head, the shiny distal stem and the metal backed glenoid component designed for good osseo-integration. The early glenoid baseplates which had a sintered metal surface were found to have a high loosening rate – resulting in a high revision rate. In 1997 the metal glenoid baseplate had a hydroxyapatite surface applied to it and the loosening rate is now very low indeed. In 2004, with Lars Neumann, my colleague, we developed the Nottingham Inter-Locking Stem (ILS) prosthesis for complicated fractures that extend down the humeral shaft (Fig. 5). However by 2005 we noted that glenoid disassembly (the plastic bearing coming off the metal baseplate) was a problem and reported this to Biomet. By 2007 we had identified a group of 10 patients with this problem and again we advised Biomet about this. Unfortunately, despite Lars Neumann and myself suggesting an alternative capture mechanism, Biomet took no action. In 2009 the metal backed glenoid component was withdrawn by Biomet and the Medicines and Healthcare Products Regulatory Agency (MHRA) have been informed about the outcome – it is really important to involve the regulatory body (in this case the MHRA) when problems like this arise. In 2010 I reported the outcomes from the Nottingham glenoid components8 and the patients are currently all being reviewed as part of an ongoing PhD research project. I received no royalties from Biomet for the Nottingham Arthroplasty but we had a “gentleman's agreement” that they would fund my Nottingham Shoulder and Elbow Fellow from August 1993 onwards.
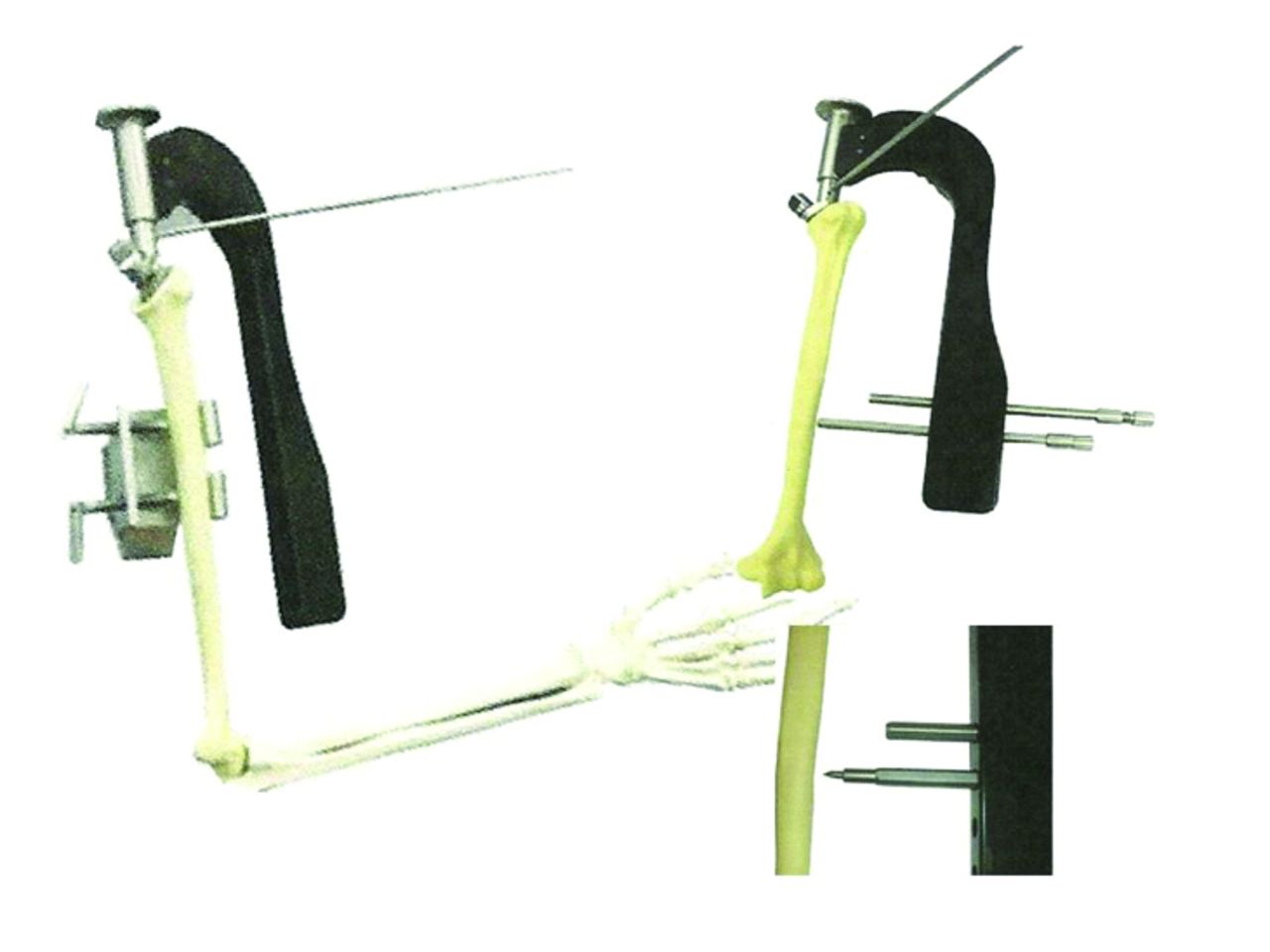
Fig. 5
Nottingham Inter-Locking Stem (ILS) prosthesis (Biomet 2004).
2005: Innovation in Shoulder Replacement Surgery with Wright Medical (2005) (Fig. 6)

Fig. 6
Cremascoli NGRi Shoulder Prosthesis (Wright Medical 2005).
Our experience with Biomet and the Nottingham Shoulder replacement had been very good for the first 10 years (1992-2002). Biomet had also been very generous in providing funding for the Nottingham Shoulder & Elbow Fellow from 1993 onwards but a combination of their failure to respond to requests for help in modifying the glenoid baseplate and their poor on-site support of the Nottingham Shoulder replacement in our Nottingham hospitals created strains. In 2000 I had started using the Delta III Reverse shoulder design for rotator cuff deficient patients and by 2005 I realised that this design, based on a concept developed by Paul Grammont in Dijon, France 25 years previously, was providing improvements in the results I was getting in my shoulder replacement patients with large and massive rotator cuff tears that I could never have achieved with a conventional anatomical design of shoulder replacement. In 2005 I approached Biomet to explore the development of a new design of shoulder replacement that would allow both an anatomic design and an inverse or reverse design to be inserted using the same basic components – a humeral stem and neck and a glenoid base-plate. This has subsequently been described as a platform shoulder system. Biomet were not interested as they had been working with the Hospital for Special Surgery in New York on a new Comprehensive® Total Shoulder System. Professor Garth Johnson, a bioengineer in Newcastle upon Tyne, who I had collaborated with previously had been working on shoulder biomechanics for the previosu 15 years and this project resulted in Garth and myself linking up once again to develop our new shoulder design. First we had to find a company to work with and after approaching a number of companies, Wright Medical, another US company indicated that they would like to work with us. This was also linked to a development in Italy with a company called Cremascoli who had developed a unique reverse, mobile bearing shoulder design called the NGRi Shoulder. Garth and I were invited to a meeting on Thursday 28th April 2005 at Le Meridien Etoile Hotel in Paris (Fig. 7).

Fig. 7
The NGRi Italian Surgeons
The Wright Medical Meeting on 28th April 2005
-
Welcome & IntroductionsGary Lancaster
-
BackgroundProf. Angus Wallace
-
Research: Past, Present & Future Prof. Garth Johnson
-
NGR-i Product ConceptAngelo De Lollis (Cremascolli)
-
The Italian ExperienceDr Livio Nogarin, Roberto Rotini & Enzo Vinci
-
Clinical Study ProposalDr Catherine Van Der Straeten (Belgium)
-
Summary & Next MeetingGary Lancaster
-
Dinner l'Orenoc RestaurantAll
We were successful in setting up a design partnership with Wright Medical and I subsequently visited Italy to see two of the 20 patients who had been treated with an NGRi shoulder replacement. These patients had outstanding results with near normal ranges of shoulder movement. However, we were concerned about two things – the stability and the wear properties of this new prosthesis and the lack of any Ethical approval for the insertion of this new design into ten Italian patients. Both Garth and I felt that we could improve the design and we felt the range of movement demonstrated by the first ten patients justified further developments. We worked with Wright Medical for two years and then, out of the blue, we were told that their US Board of Directors had made a policy decision to pull out of the shoulder arthroplasty field because they believed they were unlikely to make profits from shoulder replacements in the future.
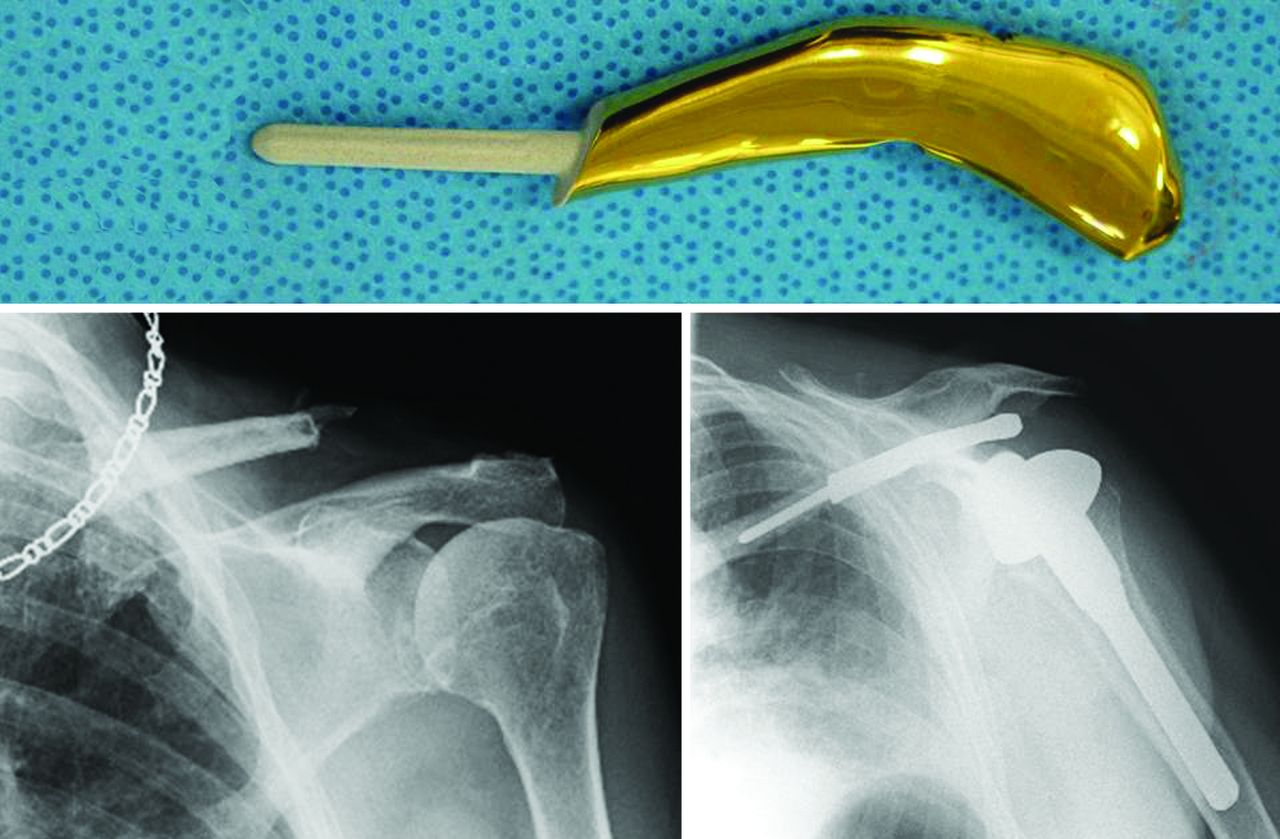
2007: VAIOS Shoulder (Fig 8)

Fig. 8
Vaios Anatomic and Inverse Shoulder Prosthesis (JRI Orthopaedics 2010).
For the second time we had to find another company to work with. I approached Brian Jones, CEO at JRI Ltd. Garth Johnson and I met with Brian, his Technical Director, Keith Jackson, and Research Director Minoo East at their Wimpole Street office on Friday 21st July 2006, and presented our research to date and the plans we had for developing a new shoulder replacement system. On Monday 24th July, Brain contacted me to confirm that JRI would support us. What an exciting day that was. Unfortunately, JRI did not have the research funding to support the development of the new shoulder and ultimately it was Government support through the Knowledge Transfer Partnership scheme which saved the day. JRI was about to change from being just a hip arthroplasty company to becoming a company with a number of different interests and subsequently Keith Jackson, who was very supportive of our project, was promoted from Technical Director to Managing Director of JRI Orthopaedics. He set up a design team to work with us on the a new shoulder arthroplasty system which incorporated both an Anatomical and an Inverse on Reverse design in 2006. Garth Johnson obtained KTP (Knowledge Transfer Partnership) funding and Ian Flatters, a bright post-graduate engineering student, was appointed to the project. Both Garth and I have now worked collaboratively with JRI Orthopaedics for over 8 years and together we have developed the Vaios Shoulder Replacement system, which is a 4th generation shoulder replacement system, now described as a “platform” system. In fact we produced the first system in the world that allowed the same components – humeral stem and neck and glenoid baseplate to be used both as an anatomic and as an inverse (or reverse) design. For me it has been great to work with JRI Orthopaedics, a UK company because I had always believed in supporting “UK PLC”. The Vaios shoulder has been judged the “Best New Mechanical Product of the Year” at the British Engineering Excellence Awards competition in October 2010 (Fig 9). I do have a Consultancy agreement with JRI Orthopaedics. My shoulder surgery team (myself and my Shoulder Fellows) have now inserted 280 Vaios shoulder replacements since April 2010 and we feel that both the previous problems with glenoid disassembly for anatomic glenoid components and instability for Inverse shoulder replacements have been resolved by this new Vaios artificial shoulder design. However, we need 5-year results to demonstrate that our prosthesis is a significant improvement on others. We have now reached three years and our results are very satisfactory to date. Finally in line with good clinical practice we have a mechanism in place that means I receive no Vaios Royalties related to the implants that I implant into my own patients.

Fig. 9
The Vaios Shoulder Arthroplasty was judged to be the “Best new Mechanical Product of the Year” at the British Engineering Excellence Awards competition in October 2010.
1995: The Nottingham Surgilig (now called LockDown) (Fig . 10)
In 1995 I approached Surgicraft to help develop a device for treating Acromio-Clavicular Joint (ACJ) injuries. I had previously tried using a Dacron vascular graft loop placed around the coracoid and the clavicle to stabilise the ACJ but that had eroded through the clavicle. Surgicraft funded a research project in my University department and we jointly designed a new implant that we called the “Nottingham Surgilig”. This was made of polyester (originally patented by ICI as “Terylene” when they invented it). Polyester had previously been used to make the Leeds-Keio ACL replacement that did not have good long-term results, tending to break after months and years. We were therefore very cautious with the introduction of the Nottingham Surgilig and only used it on 11 patients between 1995 and 2000. Lars Neumann, my Consultant colleague, helped with this development. These cases were either chronic ACJ dislocation patients with more than 6 months of symptoms, or previous failed surgical cases. Hisham Butt and I reported these early results in Orthopaedic Product News in 2005.9 The first cohort of patients did very well indeed and we started using the Surgilig for more cases from 2000 onwards. This culminated in a paper published by In-Ho Jeon, one of my Research Fellows, in 2007.10 The Nottingham Surgilig became steadily more popular and in 2006 I was approached by Surgicraft who offered me a Royalty Agreement for the Surgilig for the first time. However, that Royalty agreement came with a Consultancy commitment i.e. they wanted my help in publicising the results of the Surgilig and to help them with further development of the device and its uses. The Royalty and Consultancy agreement was completed by the University of Nottingham in 2007. The success of this implant has been highlighted in further published papers.11-14
Surgicraft were eager to break into the US market and submitted the Surgilig for Food & Drug Administration (FDA) clearance in 2009. This took some considerable time but in February 2011 FDA clearance was given on condition that the Surgilig was re-named because the FDA were unhappy about calling a device an artificial ligament and the name LockDown was selected by Surgicraft, without my involvement. If you Google “Lockdown”, you will realise why! The Nottingham Surgilig, now called “LockDown”, has had over 5000 sales in Europe and it has now become very popular in North America.
As part of my Consultancy agreement with Surgicraft, we have developed further uses for the Surgilig – for stabilising the Sterno-Clavicular Joint (Fig. 11), for stabilising the collateral ligaments at the elbow and for stabilising the collateral ligaments and inferior tibio-fibular ligaments in the ankle. The reason why the Surgilig has become so successful is that although it is non-biological, it has a facility for soft-tissue ingrowth and the body develops a fibrous tissue sheath around it once implanted, which provides a secondary biological “ligament” to support the Surgilig. Further work on analysing these findings is underway. Again I am proud to be supporting “UK PLC” in this way and the success of the Surgilig internationally is now benefitting the UK

Fig. 11
Nottingham Surgilig (now called LockDown) for stabilising the Sterno-Clavicular Joint (previously Surgicraft now Mandaco 569 Ltd 2010)
Negotiations relating to Intellectual Property (IP), Royalties and Consultancies
When I invented the Portex Ingrowing Toenail treatment kit I had no idea about IP and royalties, I was just grateful to Portex for commercialising my idea. However, my involvement as a team member of the Interax Knee replacement team opened my eyes. There are very few “new” inventions. If you review the published literature you will likely find that someone, somewhere has thought about your “new” idea and may even have tried to patent it. There is also much more to developing a new product than just being inventive. There is a whole process that needs to be developed:-
Idea > Invention > Pilot studies > Proof of Concept > Registration or provisional approval of product > Further pilot studies > Clinical studies > Preliminary marketing > Approval in other countries (i.e. FDA approval) > further Research and Development > further Marketing > working through distributors and their mark-up for their costs etc.
As an inventor it is difficult to understand the complexity of getting a new orthopaedic implant onto the market. Many inventors think “I have invented this new device; therefore I expect to get 50% royalties“. Nothing could be further from the truth. Your idea is only a tiny part of the full process. In my experience, if you are an inventor you will need to negotiate your royalties but they will be in the region of 8% (for a multi-surgeon group) to 1% for an individual surgeon with a relatively non-innovative design. Because I work for the University of Nottingham, they own my IP and therefore any negotiations have to go through the University. In the same way, if you are an NHS employee the NHS owns your IP and you will have to work with them in negotiating royalties. You may be surprised by my reflections on this but this is the way the whole system works. The University of Nottingham has helped me negotiate all my Royalty and Consultancy agreements. They retain over 50% of the payments for use by the University or my academic department and I am paid up to 50% by the University. The University lays down the following rules (Table I).
Table 1: Revenue Sharing Policy at the University of Nottingham
| In the event of commercialisation of IP, as an incentive to inventors and at its discretion, The University may elect to share revenue in the following proportions: |
|---|
| The first £25,000 of the aggregate net revenue will be apportioned as follows: |
|
|
|
| Thereafter the aggregate net revenue will be apportioned: |
|
|
|
In addition, for the Consultancy agreements the University has charged me 17.5% of the total cost for managing the Consultancy agreements that I hold.
Although commercial companies will agree to reimburse IP through royalties, most now also wish the inventor to provide on-going support and often wish them to act as a “Product Champion”. This is arranged through a “Consultancy agreement”, which usually includes a time commitment and a reimbursement rate for time devoted to the company. Doctors are generally not very good at working out their value.
How much should you charge for IP, a Consultancy Agreement and a commitment to be a Product Champion?
A new Consultant in the UK for instance starts with an annual salary of £74,504. He/she has 6 weeks annual leave, 10 days study leave and additional public holiday and NHS leave of 9 days per year. Therefore he/she works 43 weeks per year. The calculated hourly rate of work should be £74,504/43 weeks/40 hours/week. This means that the hourly rate of pay should start at £44 per hour but will be significantly higher to take into account the inventor's special expertise. The advice I have received from my University is that, as a general rule of thumb, no fee should ever be lower than twice the contracted consultant's pro rata salary.
For the Surgeon Inventor there are two considerations:
-
The fee for the work. Here the fee should recognise the status of the surgeon and the value of their advice and support as well as the time involved. In general, a consultant surgeon should charge at least £1500 per day. A high-standing surgeon with an international recognition should be able to double such a fee. In cases where the work is substantial and will require many days, then a lower rate can be used to recognise the size and longevity of the contract.
-
The fee for recognition of the invention. In cases where the consultancy fee is the only means by which the surgeon's inventive contribution is recognised, then the fee should include a component that relates to the inventive contribution. Here, we need to consider the value of the invention to the client, which would be a reflection of the expected profits over a reasonable period. It may also be necessary to recognise the contribution by the employing institutions of the inventor. Where no royalties are being paid to the institution there could be a negotiation relating to a proportion of the consultancy fee being passed to the employing institution. At the University of Nottingham the Technology Transfer Office and the University's consultancy business can work together with the inventor and the client to get a fit that works well for all the parties.
Many universities and NHS Trusts now have technology transfer offices and policies as well as external work policies and consultancy businesses, which work in concert to support the inventing academics.
Consultancy Fees and the Big Five Orthopaedic Implant Companies (Fig. 12)
Fig. 12
The US Department of Justice disciplinary procedures against Stryker Orthopaedics, Zimmer, Smith & Nephew, DePuy, and Biomet (2005)
In March 2005, the U.S. Department of Justice (DoJ) issued a subpoena requesting documents from Stryker Orthopaedics, Zimmer, Smith & Nephew, DePuy, and Biomet. These documents, which included consulting contracts, professional service agreements, and remuneration agreements between the company and surgeons or medical school graduates, were to be reviewed because of concerns that these companies had paid kickbacks to those willing to promote their joint replacement products, which would have been a violation of federal law. These cases were fully investigated and all five companies were found guilty of improper behavior – in particular paying Consultancy Fees inappropriately to encourage surgeons to use joint replacements rather than those surgeons being paid Consultancy Fees for genuine services rendered. As a consequence all five companies were subsequently monitored by the DoJ to ensure that they complied with the rules laid down by the US government. UK-based companies have not experienced such problems and appear to have always legitimately appointed Consultants appropriately. It is important for UK surgeons to understand the background to the current attitude of US companies to appointing Orthopaedic Consultants and to ensure that they work with these companies in a financially correct manner.
Conclusions from my Innovation and Invention Experiences
I am very proud of being an orthopaedic inventor (Table II). I also believe that many of our up and coming Registrars will be more inventive than I have been – the British, particularly the Scots, have always been innovative. I recommend you should always take advice from your colleagues and employers, in confidence, and if you receive support, you should take your idea forwards but always protect your ideas appropriately with confidentiality agreements which your employers will give you guidance on. Do not be greedy, IP is important but there is much more to developing a new product than just your Intellectual Property. I now work for UK PLC as well as working for my University and that has made me a very happy inventor and innovator.
Table II: Professor Wallace's Inventions and some of his Innovations
| Product | Role |
|---|---|
| The Portex Ingrowing Toenail Kit (1975) – Figure 1 | Inventor |
| Nottingham Rotator Cuff Hood (1987) – Figure 13 | Inventor |
| The Interax Total Knee Arthroplasty (1989) – Figure 3 | Co-Developer & Consultancy |
| Nottingham Total Shoulder Replacement (1989) – Figure 5 | Inventor |
| The Nottingham Surgilig (1995) – Figures 10, 11 | Co-inventor & Consultancy |
| Nottingham Augmentation Device (2001) – Figure 14 | Co-inventor |
| World First Claviculoplasty (2003) – Figure 15 | Inventor |
| Nottingham InterLocking Stem (ILS) system (2004) – Figure 6 | Co-inventor |
| Opus Arthroscopic Shoulder Equipment (2004) | Product Champion & Consultancy |
| Vaios Shoulder Arthroplasty System (2007) – Figure 9 | Co-Inventor |
| ClaviBrace (2010) – Figure 16 | Product Champion |
| Wallace Acromion Double Hook plate (2011) – Figure 17 | Inventor |
| Shepherd's Crook Elbow replacement (2012) – Figure 18 | Inventor |
| Nottingham ComfiBrace for Hip Fractures (2012) – Figure 19 | Co-Inventor |
| Harvard Tru-Grip Surgical Screwdriver (2012) – Figure 20 | Co-Developer & Consultancy |
| Hemi-Claviculoplasty (2013) – Figure 21 | Inventor |
With regard to the financial benefits, yes my wife Jackie and I have benefitted; however, the University and the taxman have both taken their share and we philosophically accept that. What I have learnt is that the Research & Development costs of commercialising a new device are considerable and should never be underestimated when you take a new device to the market.
Acknowledgments
I am very grateful to Mr Ben Ollivere for his encouragement to write this article, Dr Bruce Venning, Commercial Manager, Technology Transfer, BEIS, University of Nottingham, Ms Jenni Cain-Fowkes BA(Hons), LLB(Hons), Contracts Officer for the Faculty of Engineering, University of Nottingham, Professor Julian Ellis OBE, Ellis Developments Ltd, Nottingham and Professor Garth Johnson, Professor Emeritus, University of Newcastle upon Tyne for their support, comments and advice.
1 Andrew T , WallaceWA. Nail bed ablation--excise or cauterise? A controlled study. Br Med J1979;1:1539.CrossrefPubMed Google Scholar
2 Hoshino A , WallaceWA. Impact-absorbing properties of the human knee. J Bone Joint Surg [Br]1987;69-B:807–811.CrossrefPubMed Google Scholar
3 Roberts S, Foley J, Swallow HM, Wallace WA. The geometry of the humeral head and its implications for prosthesis design. British Association of Clinical Anatomists - Annual Congress;London 1990. Google Scholar
4 Swallow HM, Roberts S, Foley J, Wallace WA. The shape of the humeral head and its implications for prosthesis design. British Elbow and Shoulder Society - Annual Congress;London 1990. Google Scholar
5 Roberts S, Swallow HM, Foley J, Wallace WA. The shape of the humeral head and potential improvements in the design of the shoulder prosthesis. Third European Congress on Shoulder and Elbow Surgery;Milan 1990. Google Scholar
6 Boileau P , WalchG. The thee-dimensional geometry of the proximal humerus: implication for surgical technique and prosthetic design. J Bone Joint Surg [Br]1997;79-B:857–865. Google Scholar
7 Roberts SN , FoleyAP, SwallowHM, WallaceWA, CoughlanDP. The geometry of the humeral head and the design of prostheses. J Bone Joint Surg [Br]1991;73-B:647–650.CrossrefPubMed Google Scholar
8 Wallace WA. Results of uncemented metal-back glenoid implants: the UK experience. In: Walch G, Boileau P, Molé D, Favard L, Lévigne C, Sirveaux F, eds. Shoulder Concepts 2010 – The Glenoid. Montpellier-Paris: Sauramps Medical, 2010:145-147. Google Scholar
9 Butt HZ, Wallace WA. Nottingham Surgilig: a novel device for the surgical treatment of acromioclavicular dislocation. Orthopaedic Product News 2005:44-46. Google Scholar
10 Jeon I- H , DewnanyG, HartleyR, NeumannL, WallaceWA. Chronic acromioclavicular separation: the medium term results of coracoclavicular ligament reconstruction using braided polyester prosthetic ligament. Injury2007;38:1247–1253.CrossrefPubMed Google Scholar
11 Hodgson P , PullenH, JenkinsO, et al.Methods of coraco-clavicular reconstruction: a comparison of the modified Weaver-Dunn and Surgilig surgical techniques. Injury Extra2007;38:4–5. Google Scholar
12 Bhattacharya R , GoodchildL, RanganA. Acromioclavicular joint reconstruction using the Nottingham Surgilig: a preliminary report. Acta Orthop Belg2008;74:167–172.PubMed Google Scholar
13 Wood T , RosellP, ClasperJ. Preliminary results of the 'Surgilig™, synthetic ligament in the management of chronic ACJ disruption. J R Army Med Corps2009;155:191–193. Google Scholar
14 Carlos AJ , RichardsAM, CorbettSA. Stabilization of acromio-clavicular joint dislocation using the 'Surgilig' technique. Shoulder and Elbow2011;3:166–170. Google Scholar