Abstract
We live in troubled times. Increased opposition reliance on explosive devices, the widespread use of individual and vehicular body armour, and the improved survival of combat casualties have created many complex musculoskeletal injuries in the wars in Iraq and Afghanistan. Explosive mechanisms of injury account for 75% of all musculoskeletal combat casualties. Throughout all the echelons of care medical staff practice consistent treatment strategies of damage control orthopaedics including tourniquets, antibiotics, external fixation, selective amputations and vacuum-assisted closure. Complications, particularly infection and heterotopic ossification, remain frequent, and re-operations are common. Meanwhile, non-combat musculoskeletal casualties are three times more frequent than those derived from combat and account for nearly 50% of all musculoskeletal casualties requiring evacuation from the combat zone.
Introduction
Musculoskeletal combat casualties during the wars in Iraq and Afghanistan differ from those of previous conflicts because of the development of opposition tactics, the nearly universal use of individual and vehicular body armour and the far-forward deployment of contemporary medical technologies and treatment algorithms.1-3 Enemies of US/Coalition Forces in Iraq and Afghanistan have employed unconventional tactics, including terrorism and insurgency, to offset the US/Coalition Forces’ modern and well-equipped combat forces. The enemy weapon of choice has been the improvised explosive device (IED), which is constructed from conventional or homemade explosive material and tactically employed in the form of buried artillery rounds, antipersonnel mines and car bombs. Consequently, over 75% of US combat casualties are caused by explosive injuries, representing the highest proportion in US military history.4 Explosive blasts produce devastating and often contaminated injuries to all body systems. All US soldiers use individual body armour, including protective vests and Kevlar helmets, which has minimised the impact of otherwise life-threatening injuries; this is evidenced by the decrease in lethality of a gunshot wound to 4.6%4 from 33% in the Second World War.5Additionally, the US introduced the Mine-Resistant Ambush-Protected Vehicle (MRAP) to counter the burgeoning IED threat. Significant advances in the approach to combat medical care include equipping all US soldiers with tourniquets. These have significantly decreased pre-hospital death rates in service members as a result of extremity exsanguination, from the 9% seen during the Vietnam War to 2%, with minor associated morbidity.6,7 Additionally, the US military developed and implemented the Joint Theatre Trauma System and Joint Theatre Trauma Registry to permit a systematic approach to battlefield care analysis that may decrease mortality and improve outcomes after combat injury. These endeavours have produced 27 evidence-based clinical practice guidelines, which include the damage-control resuscitation guideline. This has decreased the mortality rates of combat casualties requiring a massive transfusion (> 10 units red blood cells/24 hours) from 32% to 21%.8
Modern body armour and up-armoured vehicles have greatly increased the protection of critical central body systems, while leaving the extremities relatively exposed to primary (shockwave), secondary (projectile) and tertiary (burns) blast-related effects that result in a large number of complex musculoskeletal injuries with heavy bacterial contamination and multiple concurrent injuries (Fig. 1). The importance of appropriate treatment of combat-related musculoskeletal injuries cannot be overstated, as 84% of all medical discharges from the military have at least one orthopaedically related disqualifying condition.9

Fig. 1
Figure 1a – pre-operative clinical photograph of a mangled distal lower extremity. Figure 1b – anteroposterior radiograph of a different mangled limb. Both demonstrate the severe contamination, with osseous and soft-tissue injuries, that are associated with blasts from improvised explosive devices. Both limbs required immediate transtibial amputation during the first debridement and irrigation procedure.
Musculoskeletal combat casualties and in-theatre treatment
As of 2 April 2012, there have been 47 483 US service members wounded in action and 4986 combat deaths in the Iraq and Afghanistan Wars.10 Early studies on these conflicts reported that between 49% and 54% of all soldiers injured sustained a musculoskeletal injury to an extremity.4,11 A prospective, longitudinal cohort study of 4122 deployed soldiers reported musculoskeletal combat injury rates per 1000 soldier combat years as follows: soft-tissue/neurovascular injury, 32.8; closed fracture, 6.4; open fracture, 5.0; major amputation, 2.1; and minor amputation, 0.6. Most notable was that 44% to 82% of all combat fractures were open3,11 and that explosive injuries frequently had significant associated soft-tissue defects that required multiple debridements before amputation or definitive flap coverage.12
There are five echelons of care for combat casualties, with each echelon progressively further from the battlefield but possessing increasingly advanced medical capabilities (Fig 2).13 The initial management of all combat casualties includes the use of Advanced Trauma Life Support protocols supplemented with clinical practice guidelines for resuscitation and the management of specific injuries. Minor injuries can be treated at more forward, lower echelons of care and the service member may remain in theatre until returned to duty; more extensive injuries are evacuated to higher echelons of care. The principles of damage-control orthopaedics, including controlling haemorrhage, preventing infection and preserving function are practised throughout the evacuation chain.14,15 Antibiotics16,17and tetanus prophylaxis, when necessary, are given. Field tourniquets, particularly for proximal/junctional injuries, should generally be removed in the controlled environment of the operating theatre where direct vascular control is most feasible. Musculoskeletal combat wounds are thoroughly debrided and irrigated and are universally managed in an open manner with either negative pressure wound therapy using vacuum-assisted closure (VAC; KCI Inc., San Antonio,Texas)18 or conventional absorbent dressings. Additionally, wound VACs reduce the need for painful dressing changes during the evacuation process and have been demonstrated to operate safely at altitude during aeromedical evacuation.18 External fixators and splints are used to provisionally stabilise fractures.19,20 The external fixation of pelvic and long-bone fractures reduces blood loss, allows for ongoing resuscitation and provides access to wounds while maintaining fracture stability (Fig 3).14 Lower echelons of care perform any essential immediate amputations, but every effort is made to initially preserve limbs when they are perfused or revascularised, often using temporary vascular shunts.21,22 When performed, traumatic amputations are completed in an open, length-preserving fashion, as maximum retention of viable tissue provides surgeons at the higher echelons of care with more options for coverage and length preservation. Extremity fasciotomies for compartment syndrome are performed in approximately 30% of limb casualties, often prophylactically before medical evacuation.23 Blast-injured tissues and wounds evolve slowly, and continued evidence of necrosis and residual contamination becomes evident for days, or even weeks, after injury. All wounds are re-inspected, with significant injuries often undergoing a formal irrigation and debridement at 24 to 72 hour intervals, as each combat casualty progresses through the echelons of care. The majority of musculoskeletal casualties are evacuated to a Level IV facility within 48 hours of injury.18

Fig. 2
Diagram of the Joint Echelons of Care in the Military Health System. BN = battalion, COMMZ = communications zone, CONUS = continental United States, OCONUS = outside continental United States, USMC = United States Marine Corps. (Reproduced with permission fromOwens BD, Belmont PJ Jr, eds. Combat Orthopaedic Surgery: Lessons Learned in Iraq and Afghanistan. SLACK Inc, 2001; Thorofare: New Jersey.)

Fig. 3
Clinical photograph of an active-duty service member who sustained bilateral limb-threatening tibial fractures after a blast injury. The fractures were provisionally stabilised with external fixators. The segmental bone loss in his right tibia, after thorough irrigation and debridement, had antibiotic beads placed within the defect. The left lower extremity was treated with vacuum-assisted closure and a “Jacob’s Ladder” large vessel loop configuration applied to the skin margins by skin staples in order to initially treat the associated soft-tissue loss.
Definitive treatment of complex musculoskeletal combat injuries
Once the patient arrives at a Level IV or V facility, definitive treatment measures progress as rapidly as wounds permit. Although the orthopaedic surgeon’s role in this process is important, a large rehabilitation team consisting of trauma and plastic/ reconstructive surgeons, pain specialists, rehabilitation physicians, physical and occupational therapists, psychiatrists, prosthetists/ orthotists, and social workers is critical to the success of rehabilitation. The importance of patient dedication to, and family support during, the rehabilitation period cannot be overstated.
Although early flap coverage of open fractures has been shown to be beneficial in civilian trauma settings, in a combat environment most flap coverage is delayed because of a combination of slowly evolving wounds, multiple injuries and systemic polytrauma, and the time constraints of the evacuation process itself.12 Wounds are closed when the patient is physiologically stable and the gross tissue appearance is consistently healthy, although in due course more objective means of assessing the suitability of a wound for closure may be feasible.24,25 Dermal replacement scaffolds have proved beneficial in covering small areas of exposed tendon and bone instead of formal flap coverage26, and have been used more liberally in recent years in order to increase the robustness of delayed split-thickness skin grafts, particularly over distal residual limbs. Contrary to some reports in the civilian literature, rotational flap coverage within the zone of injury is still performed when tissue conditions permit, with good results when compared with free-tissue transfer.27
Many fractures are still treated with intramedullary or internal fixation, particularly type I or II injuries, or those for which definitive external fixation is impractical or impossible. However, concerns about high infection rates have limited the use of intramedullary nails for type IIIB and IIIC injuries.28 A high union rate and relatively low complication rate were noted in one study of open combat-related tibial fractures that had been treated with ring external fixation and a standard treatment algorithm.29 Nonetheless, injury treatment and fracture fixation must be individualised to the patient given the wide variety of injuries to the bone, articular surfaces, and neurovascular systems, as well as the volume of soft-tissue and muscle loss.
The majority of combat-related amputations are immediate traumatic or early amputations for unsalvageable distal extremities. For these patients, the ultimate amputation level is often determined by the extent of the initial bone and, more importantly, soft-tissue loss, provided that an open, length-preserving procedure has been performed in the combat theatre. After serial irrigation and debridement, residual limbs are closed at the most distal practicable amputation level, while avoiding excessively long or short levels. This is based on the ability to obtain robust soft-tissue coverage, often using atypical skin flaps, while salvaging as much bone length and joint surface as possible. Extensive surgical intervention is indicated in order to salvage a functional knee or elbow joint, and local and free-tissue transfers have been employed with good effect toward this end when soft tissues were insufficient to maintain a transradial or transtibial level. Distal amputations should not be routinely revised through the site of more proximal fractures. Despite a high infection rate, all fractures eventually healed and salvage of the amputation level was successful in all patients in a recent series of associated amputations with proximal fractures.30 Appropriate traction neurectomies of all named nerves are critical to avoid painful neuromas. Stable anchorage of the distal soft tissues through a combination of deep myodesis and superficial myoplasty is essential in order to improve residual limb control, secure padding, and prevent symptoms such as soft-tissue snapping, instability or redundancy. Split-thickness skin grafts, although avoided when possible, are often placed over distal residual limbs to salvage length after synthetic neodermis incorporation, provided that the underlying soft tissues are robust and viable.
Approximately 15% of amputations are performed more than 12 weeks after injury in a delayed, elective fashion31,32, usually as a result of persistent pain or limited function after an apparently successful limb salvage. Amputation can occasionally be required because of late complications such as recurrent infection and/or nonunion.33 As with the published civilian literature, nerve function on initial examination is neither a reliable predictor of ultimate function nor a good criterion for early amputation in the absence of direct, visualised nerve disruption.34 Enthusiasm for the modified Ertl tibiofibular synostosis technique of transtibial amputation has waned because of the persistent absence of a detectable functional benefit (unpublished data). Recently, casualties have demonstrated a higher reoperation and complication rate with this procedure as compared with traditional transtibial amputation.35 Prosthetic advances, including more pliable sockets and improved suspension mechanisms, recreational specialty limbs and terminal devices, and microprocessor and powered knees and ankles, have substantially increased the functional outcomes likely for wounded warriors with limb loss.36 Approximately 15% to 20% of patients with severe injuries to the lower extremity, whether ultimately treated with limb salvage or amputation, will return to duty either with or without a military specialty (vocational) change.31,37 A number of patients with either an amputation or successful limb salvage have redeployed to the combat theatre in active roles after rehabilitation.
Complications
Complications after the definitive management of combat-related injuries to the extremity are frequent and remain a constant shadow over the rehabilitation process. Two, in particular, warrant mention. Infections can be devastating and frequent, developing in approximately 15% to 40% of injuries, depending on the specific patient population and injuries studied.16,28,30,35 Despite the attention given to Acinetobacter baumanni infections early in the conflicts, the majority of early infections actually result from other gram-negative organisms, and the majority of late infections are created by gram-positive organisms. Unfortunately, multi-drug-resistant organisms are common. The treatment of infections involves aggressive serial debridement, culture- and sensitivity-specific antibiotics, frequent use of antibiotic-impregnated polymethylmethacrylate beads or spacers, and temporary implant removal, when feasible. Most infections can be successfully eradicated in this fashion, with recalcitrant infections often involving necrotic bone, compromised soft-tissue envelopes, and/or retained implants. Loss of some residual limb length after the treatment of deep infection of a residual limb is common, but loss of a functional joint level is fortunately exceedingly rare.
Heterotopic ossification (HO), the mature formation of lamellar bone in non-osseous tissue, occurs in approximately 63% of all major injuries to an extremity, including both salvaged limbs and amputations.38,39 The development of HO can cause pain and limit joint movement through soft-tissue tethering or direct impingement. This can lead to arthrofibrosis, entrap critical neurovascular structures (Fig. 4), and cause persistent symptoms and/or recurrent skin breakdown. Primary prophylaxis with either local radiotherapy or non-steroidal anti-inflammatory drugs is generally either not feasible or medically contraindicated after blast-related multi-system trauma. The only treatment for persistently symptomatic HO remains surgical excision, which can be difficult, bloody, and fraught with wound complications. While many patients with HO remain asymptomatic or respond to conservative measures, more than 25% eventually require surgical excision. Research into combat-related HO is thus a topic of substantial research focus with regard to physiological causes, potential early diagnostic methods, and prevention.40-42
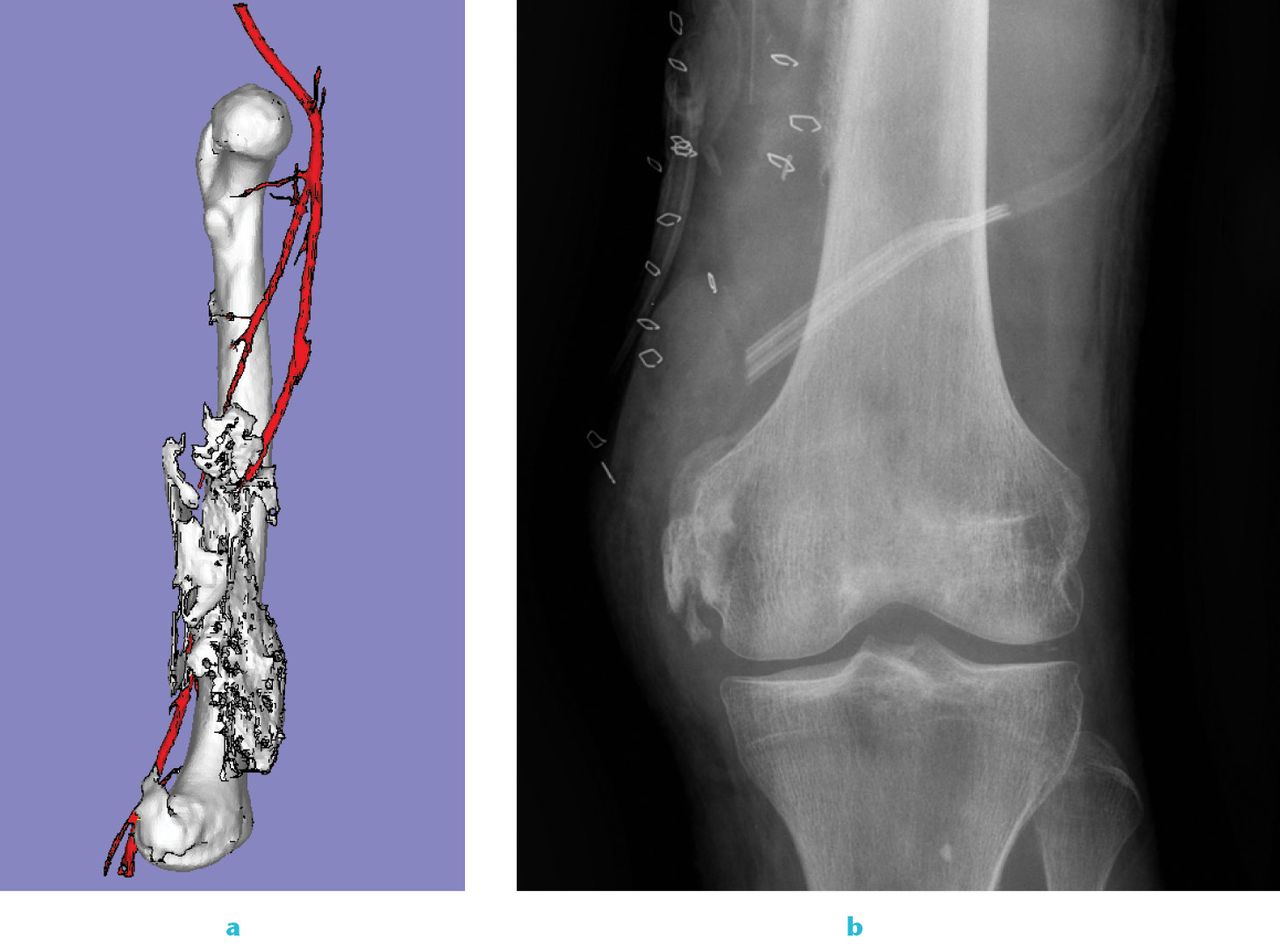
Fig. 4
Figure 4a – three-dimensional CT scan reconstruction of a patient with severe heterotopic ossification (HO) incarcerating his superficial femoral vessels and severely limiting the range of movement of his knee because of quadriceps and adductor involvement, resulting in secondary arthrofibrosis. The patient was neurovascularly intact distally in this otherwise sound limb, and underwent successful excision of the HO and lysis of knee adhesions without injury to the entrapped vessels. Figure 4b – post-operative anteroposterior radiograph of this patient’s distal femur and knee.
Musculoskeletal noncombat and non-emergency injuries
Two longitudinal cohort studies of a US Army Brigade Combat Team reported a 347% increase in noncombat compared with combat musculoskeletal casualties.3,43These investigations found that noncombat injuries accounted for 48% of all musculoskeletal casualties that were medically evacuated to an echelon IV/V facility.3,43 Additionally, many service members sustained non-emergency musculoskeletal injuries which were treated conservatively in theatre and ultimately required surgery after their combat tour.43,44 The incidence rates of anterior cruciate ligament disruption and first-time shoulder dislocation, as noncombat injuries, are nearly five times greater than those seen in a civilian population. This is indicative of the daily rigours of the combat environment.43 Further examination of these Brigade Combat Team service members who completed a combat deployment revealed that 19% had an orthopaedic consultation on their return and 4% required an orthopaedic surgical procedure; more than 50% of these involved the knee or shoulder.44
The large number of musculoskeletal noncombat45 and non-emergency injuries has increased the importance of providing treatment at the appropriate echelon of care in order to minimise troop loss. Therefore, the US Army established the Telemedicine Orthopaedic Consultation Programme in order to assist remotely deployed medical providers with expert orthopaedic advice.46 In an early analysis of the programme, surgical intervention or medical evacuation was only recommended in 25% and 16% of the consultations, respectively, whereas virtually all service members requiring orthopaedic advice would previously have been evacuated to higher echelons of care.46
Conclusion
The initial management of all open musculoskeletal combat wounds includes patient stabilisation and urgent debridement and irrigation of wounds, followed by provisional stabilisation of fractures. Wounds should initially be treated with a VAC or left open and generally require serial procedures to permit safe and durable closure or coverage. The definitive treatment of severe injuries most often occurs at high-volume, higher echelon facilities with greater technical resources, after both the combat casualty and combat wounds have stabilised. Despite high complication rates, remarkable functional outcomes are possible in many instances with surgeon diligence, patient dedication, and the involvement of a multidisciplinary rehabilitation team of experts.
1 Covey DC . From the frontlines to the home front: the crucial role of military orthopaedic surgeons. J Bone Joint Surg [Am]2009;91-A:998–1006. Google Scholar
2 Belmont PJ Jr, Goodman GP. The combat environment and epidemiology of musculoskeletal combat casualties. In: Owens BD, Belmont PJ Jr, eds. Combat Orthopaedic Surgery: Lessons Learned in Iraq and Afghanistan. Thorofare, NJ: SLACK Incorporated; 2011:13-22. Google Scholar
3 Belmont PJ Jr , ThomasD, GoodmanGP, et al.Combat musculoskeletal wounds in a US Army Brigade Combat team during Operation Iraqi Freedom. J Trauma2011;71:E1–E7.CrossrefPubMed Google Scholar
4 Belmont PJ Jr , GoodmanGP, ZacchilliM, et al.Incidence and epidemiology of combat injuries sustained during “the surge” portion of Operation Iraqi Freedom by a U.S. Army brigade combat team. J Trauma2010;68:204–210. Google Scholar
5 Bellamy RF, Zajtchuk R. Assessing the effectiveness of conventional weapons. In: Zajtchuk R, ed. Textbook of Military Medicine, Part I: Warfare, Weaponry, and the Casualty, Vol. 5, Conventional Warfare: Ballistic, Blast, and Burn Injuries. Washington, DC: Office of the Surgeon General, Department of the Army, United States of America; 1991:53-82. Google Scholar
6 Kragh JF Jr , LittrelML, JonesJA, et al.Battle casualty survival with emergency tourniquet use to stop limb bleeding. J Emerg Med2011;41:590–597.CrossrefPubMed Google Scholar
7 Kragh JF Jr , WaltersTJ, BaerDG, et al.Survival with emergency tourniquet use to stop bleeding in major limb trauma. Ann Surg2009;249:1–7.CrossrefPubMed Google Scholar
8 Eastridge BJ , CostanzoG, JenkinsD, et al.Impact of joint theater trauma system initiatives on battlefield injury outcomes. Am J Surg2009;198:852–857.CrossrefPubMed Google Scholar
9 Cross JD, Ficke JR, Hsu JR, Masini BD, Wenke JC. Battlefield orthopaedic injuries cause the majority of long-term disabilities. J Am Acad Orthop Surg 2011;199(Suppl 1):S1-S7. Google Scholar
10 No authors listed. Directorate for Information Operations and Reports. Department of Defense. http://siadapp.dmdc.osd.mil/ (date last accessed 16 August 2012.). Google Scholar
11 Owens BD , Kragh JF Jr, MacaitisJ, SvobodaSJ, WenkeJC. Characterization of extremity wounds in Operation Iraqi Freedom and Operation Enduring Freedom. J Orthop Trauma2007;21:254–257.CrossrefPubMed Google Scholar
12 Tintle SM , GwinnDE, AndersenRC, KumarAR. Soft tissue coverage of combat wounds. J Surg Ortho Adv2010;19:29–34.PubMed Google Scholar
13 Hetz SP . Introduction to military medicine: a brief overview. Surg Clin N Am2006;86:675–688.CrossrefPubMed Google Scholar
14 Andersen RC , UrsuaVA, ValosenJM, et al.Damage control orthopaedics: an in-theater perspective. Surg Ortho Adv2010;19:13–17.PubMed Google Scholar
15 Bagg MR , CoveyDC, Powell ET 4th. Levels of medical care in the global war on terrorism. J Am Acad Orthop Surg2006;14:S7–S9.CrossrefPubMed Google Scholar
16 Murray CK, Obremskey WT, Hsu JR, et al. Prevention of infections associated with combat-related extremity injuries. J Trauma 2011;71(2 Suppl 2):S235-257. Google Scholar
17 Tribble DR , LloydB, WeintrobA, et al.Antimicrobial prescribing practices following publication of guidelines for the prevention of infections associated with combat-related injuries. J Trauma2011;71:S299–S306.CrossrefPubMed Google Scholar
18 Fang R , DorlacWC, FlahertySF, et al.Feasibility of negative pressure wound therapy during intercontinental aeromedical evacuation of combat casualties. J Trauma2010;69:S140–S145.CrossrefPubMed Google Scholar
19 Camuso MR . Far-forward fracture stabilization: external fixation versus splinting. J Am Acad Orthop Surg2006;14:S118–S123.CrossrefPubMed Google Scholar
20 Possley DR , BurnsTC, StinnerDJ, et al.Temporary external fixation is safe in a combat environment. J Trauma2010;69:S135–S139.CrossrefPubMed Google Scholar
21 Borut LT , AcostaCJ, TadlockLC, et al.The use of temporary vascular shunts in military extremity wounds: a preliminary outcome analysis with 2-year follow-up. J Trauma2010;69:174–178.CrossrefPubMed Google Scholar
22 Gifford SM , AidinianG, ClouseWD, et al.Effect of temporary shunting on extremity vascular injury: an outcome analysis from the Global War on Terror vascular initiative. J Vasc Surg2009;50:549–555. Google Scholar
23 Kragh JF Jr , WadeCE, BaerDG, et al.Fasciotomy rates in Operations Enduring Freedom and Iraqi Freedom: association with injury severity and tourniquet use. J Orthop Trauma2011;25:134–139.CrossrefPubMed Google Scholar
24 Hawksworth JS , StojadinovicA, GageFA, et al.Inflammatory biomarkers in combat wound healing. Ann Surg2009;250:1002–1007.CrossrefPubMed Google Scholar
25 Forsberg JA , ElsterEA, AndersenRC, et al.Correlation of procalcitonin and cytokine expression with dehiscence in wartime extremity wounds. J Bone Joint Surg [Am]2008;90-A:580–588. Google Scholar
26 Helgeson MD , PotterBK, EvansKN, ShawenSB. Bioartificial dermal substitute: a preliminary report on its use for the management of complex combat-related soft tissue wounds. J Orthop Trauma2007;21:394–399.CrossrefPubMed Google Scholar
27 Burns TC , StinnerDJ, PossleyDR, et al.Does the zone of injury in combat related type III open tibia fractures preclude the use of local soft tissue coverage?J Orthop Trauma2010;24:697–703.CrossrefPubMed Google Scholar
28 Lacap AP, Frisch HM. Intramedullary nailing following external fixation in tibial shaft fractures sustained in Operations Enduring and Iraqi Freedom. Poster presented at the Annual Meeting of the Orthopaedic Trauma Association; 2007 Oct 17-20; Boston, MA. Google Scholar
29 Keeling JJ , GwinnDE, TintleSM, AndersenRC, McGuiganFX. Short-term outcomes of severe open wartime tibial fractures treated with ring external fixation. J Bone Joint Surg [Am]2008;90-A:2643–2651.CrossrefPubMed Google Scholar
30 Gordon WT , O’BrienFP, StraussJE, AndersenRC, PotterBK. Outcomes associated with the internal fixation of long-bone fractures proximal to ipsilateral traumatic amputations. J Bone Joint Surg [Am]2010;92-A:2312–2318. Google Scholar
31 Cross JD , StinnerDJ, BurnsTC, et al.Return to duty after type III open tibia fracture. J Orthop Trauma2012;26:43–47.CrossrefPubMed Google Scholar
32 Stinner DJ , BurnsTC, KirkKL, et al.Prevalence of late amputations during the current conflicts in Afghanistan and Iraq. Mil Med2010;175:1027–1029.CrossrefPubMed Google Scholar
33 Helgeson MD , PotterBK, BurnsTC, HaydaRA, GajewskiDA. Risk factors for and results of late delayed amputation following combat-related extremity injuries. Orthopedics2010;33:669. Google Scholar
34 Beltran MJ, Burns TC, Eckel TT, et al. Fate of combat nerve injury. J Orthop Trauma 2012;(Epub ahead of print). Google Scholar
35 Tintle SM , KeelingJJ, ForsbergJA, et al.Operative complications of combat-related transtibial amputations: a comparison of the classic Burgess and modified Ertl tibiofibular synostosis techniques. J Bone Joint Surg [Am]2011;93-A:1016–1021. Google Scholar
36 Harvey ZT , PotterBK, VanderseaJ, WolfE. Prosthetic advances. J Surg Orthop Adv2012;21:58–64.PubMed Google Scholar
37 Stinner DJ , BurnsTC, KirkKL, FickeJR. Return to duty rate of amputee soldiers in the current conflicts in Afghanistan and Iraq. J Trauma2010;68:1476–1479.CrossrefPubMed Google Scholar
38 Potter BK , BurnsTC, LacapAP, GranvilleRR, GajewskiDA. Heterotopic ossification following traumatic and combat-related amputations: prevalence, risk factors, and preliminary results of excision. J Bone Joint Surg [Am]2007;89-A:476–486. Google Scholar
39 Forsberg JA , PepekJM, WagnerS, et al.Heterotopic ossification in high-energy wartime extremity injuries: prevalence and risk factors. J Bone Joint Surg [Am]2009;91-A:1084–1091.CrossrefPubMed Google Scholar
40 Potter BK , ForsbergJA, DavisTA, et al.Heterotopic ossification following combat-related trauma. J Bone Joint Surg [Am]2010;92-A Suppl 2;74-89.:.CrossrefPubMed Google Scholar
41 Davis TA , O’BrienFP, AnamK, et al.Heterotopic ossification formation in complex orthopedic combat wounds: quantification and characterization of osteogenic precursor cell activity in traumatized muscle. J Bone Joint Surg [Am]2011;93-A:1122–1131. Google Scholar
42 Alfieri KA , ForsbergJA, PotterBK. Blast injuries and heterotopic ossification. Bone Joint Res2012;1:174–179.CrossrefPubMed Google Scholar
43 Belmont PJ Jr , GoodmanGP, WatermanB, et al.Disease and nonbattle injuries sustained by a U.S. Army Brigade Combat Team during Operation Iraqi Freedom. Mil Med2010;175:469–476.CrossrefPubMed Google Scholar
44 Goodman GP , SchoenfeldAJ, OwensBD, et al.Non-emergent orthopaedic injuries sustained by soldiers in Operation Iraqi Freedom. J Bone Joint Surg [Am]2012;94-A:728–735.CrossrefPubMed Google Scholar
45 Hauret KG, Taylor BJ, Clemmons NS, Block SR, Jones BH. Frequency and causes of nonbattle injuries air evacuated from Operations Iraqi Freedom and Enduring Freedom, U.S. Army, 2001-2006. Am J Prev Med 2010:38(1 Suppl):S94-107. Google Scholar
46 Blank E , LappanC, Belmont PJ Jr, et al.Early analysis of the United States Army’s Telemedicine Orthopaedic Consultation Program. J Surg Ortho Adv2011;20:50–55. Google Scholar









