Abstract
Aims
Femoroacetabular impingement (FAI) describes abnormal bony contact of the proximal femur against the acetabulum. The term was first coined in 1999; however what is often overlooked is that descriptions of the morphology have existed in the literature for centuries. The aim of this paper is to delineate its origins and provide further clarity on FAI to shape future research.
Methods
A non-systematic search on PubMed was performed using keywords such as “impingement” or “tilt deformity” to find early anatomical descriptions of FAI. Relevant references from these primary studies were then followed up.
Results
Although FAI has existed for almost 5,000 years, the anatomical study by Henle in 1855 was the first to describe it in the literature. The relevance of the deformity was not appreciated at the time but this triggered the development of further anatomical studies. Parallel to this, Poland performed the first surgical correction of FAI in 1898 and subsequently, descriptions of similar procedures followed. In 1965, Murray outlined radiological evidence of idiopathic cam-type deformities and highlighted its significance. This led to a renewed focus on FAI and eventually, Ganz et al released their seminal paper that has become the foundation of our current understanding of FAI. Since then, there has been an exponential rise in published literature but finding a consensus, especially in the diagnosis of FAI, has proven to be difficult.
Conclusion
Current research on FAI heavily focuses on new data, but old evidence does exist and studying it could be equally as important in clarifying the aetiology and classification of FAI.
Cite this article: Bone Joint Res 2020;9(9):572–577.
Article summary
-
To elucidate the origins of femoroacetabular impingement (FAI) and uncover early literature on the topic.
-
To describe the most important published works on FAI and how these have altered with time.
-
When challenging old data on FAI, it is important to appreciate the historical context surrounding it.
Key messages
-
This is the first study, to our knowledge, to give a comprehensive review of historic literature regarding FAI.
-
We found that although evidence of FAI has existed in the literature for centuries, our understanding of it has been heavily influenced by Ganz’s review in the early 2000.
-
When challenging old data on FAI, it is important to appreciate the historical context surrounding them.
Strengths and limitations
-
We used a wide range of historical studies from the mid-19th century onwards.
-
As many of the studies were not available on online databases and were only available as hard copy, we had to references search to find older papers.
-
Although our process was rigorous, it is possible that there is missing literature on the topic.
Introduction
Femoroacetabular impingement (FAI) describes the abnormal intracapsular impact of the proximal femur against the acetabulum during ranges of motion due to morphological changes in one or both of these structures. This, over time, leads to the failure of the labrum, the labrochondral junction, and/or the adjacent cartilage and is thought to be a common cause of early osteoarthritis (OA) in a non-dysplastic hip.1
There are two distinct types of FAI: cam-type and pincer-type.2 Although the impingement can take place all around the articular circumference, the predominant localization is anterolateral.
Cam-type impingement is caused by a decreased femoral head-neck offset, often due to an osseous prominence and can be further subdivided into idiopathic (primary) and secondary. Secondary cam-type impingement has been well studied and involves pathological processes that alter the femoral head-neck morphology such as Perthes’ disease3 and femoral neck fractures.4 Unlike secondary impingement, the aetiology of idiopathic impingement is unclear although it is understood it involves extension of the femoral head epiphysis due to a growth abnormality of the cartilage or bone.5
Pincer-type impingement arises from increased acetabular coverage with a normal contour of the femoral head and can be split into non-focal and focal.6 Non-focal over-coverage describes the deformity in which the acetabular fossa is deepened and includes protrusio acetabuli. Focal over-coverage, on the other hand, affects only a part of the acetabulum and can occur anteriorly or posteriorly.
The term ‘femoroacetabular impingement’ was coined by Myers et al7 in 1999 and research into this condition grew exponentially after the review by Ganz et al1 suggested FAI may be the underlying cause of idiopathic OA. The concept of hip impingement, however, is not a novel one and descriptions of the deformity surrounding it have existed in the literature for more than a century. In this review, we delve into the history of FAI to better understand its origins and explore how past research contributed to our current understanding of this morphological abnormality.
Search strategy and criteria
A non-systematic search of PubMed was performed to find anatomical descriptions of FAI. Various keywords such as “impingement”, “tilt deformity”, “pistol grip”, and “slipped capital femoral epiphysis” were initially used to discover papers and reviews, mainly from the late 20th century. Referenced papers from these primary studies were then duly followed up, including those not available on PubMed. Further keywords such as “cervical fossa”, “reaction area”, or “acetabular protrusion” were also identified and used to find earlier papers from the 19th to early 20th centuries.
3,000 BC to 19th century: gathering information from human cadavers
Due to the lack of investigations in the early to mid-19th century, discoveries in human morphology, including that of the femoroacetabular joint, depended on anatomical studies on human cadavers. Crucially, some of these studies showed morphological variants in the acetabulum and/or proximal femur. At the time of discovery, the implications of these variants were not appreciated but now they serve as important historical evidence.
The first discovery of such a variant was in 1824 by a German pathologist, Adolph William Otto.8 On closer inspection of an anatomical specimen of a female pelvis in the Natural History Museum of Breslau (Poland), he noted a “very deep insertion of both femoral heads in the acetabula”; this was what we currently term as global pincer-type impingement, ‘protrusio acetabuli’.
Abnormal version of the acetabulum, on the other hand, was first brought into context with OA of the hip joint by Preiser in 1907.9 Today this is understood as focal anterior over-coverage in a retroverted acetabulum.
Along with pincer-type impingement, early pathoanatomical studies discovered two major variations of the femoral neck anteriorly corresponded to the morphological changes seen in cam-type impingement.10 The first was an extension of the articular surface of the femoral head upon the neck. Although Poirier11 is often credited for the discovery of this landmark, a subtle version was present in an illustration by Henle in 1855 (Figure 1).12 It is thought to correspond to the classical osseous bump of cam-type deformity.13
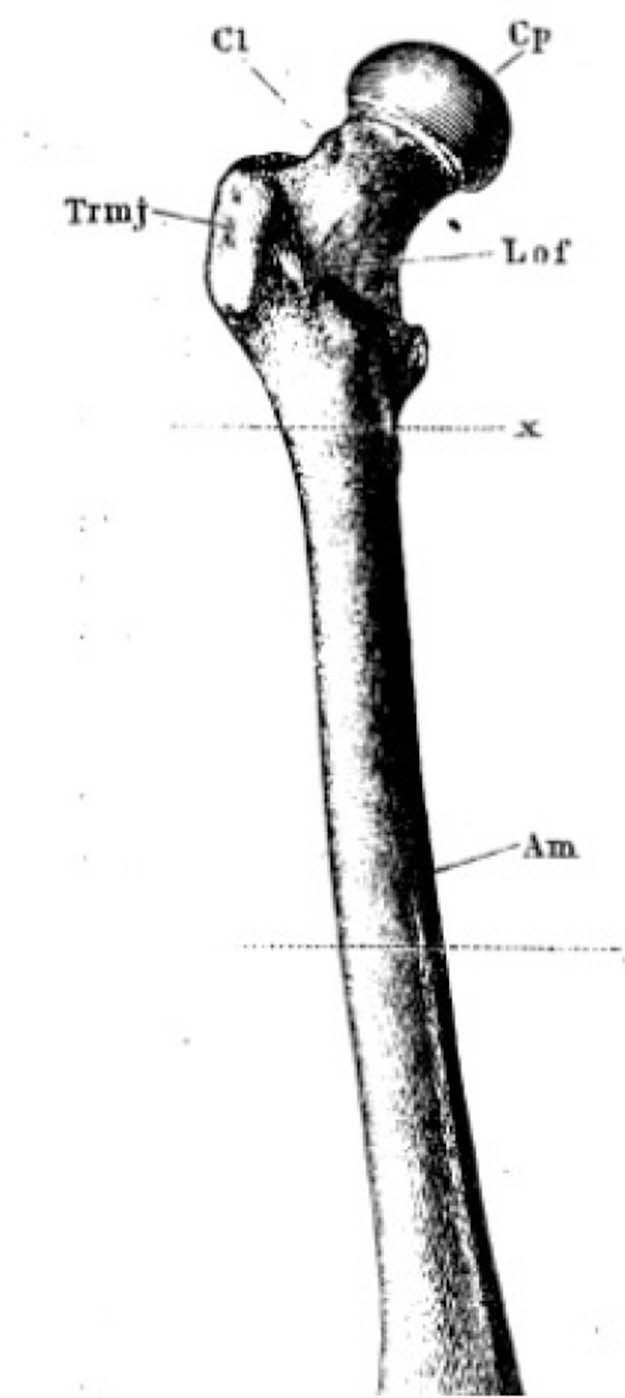
Fig. 1
Henle’s depiction of the femur. Surface markings on the anterosuperior surface of the femoral neck can be seen.
The other noted deformity was a depressed area below Poirier’s facet resulting from a ‘surface reaction’, known as the ‘cervical fossa’ discovered by Allen in 1882.14 This is thought to correspond to fibrocystic changes arising from repetitive bony contact between the femoral head-neck and acetabulum.15
Anatomical studies also had a significant role in delineating the first incidents of FAI, which was present even before the 19th century. Rather remarkably, morphological abnormalities that bore resemblance to Poirier’s facet were recently discovered in a 5,000-year-old skeleton.16 This study also used computerized methods to reconstruct and analyze the specimen’s hip revealing a cam-type deformity.
FAI is therefore not a new disease but simply a new method of conceptualizing a pre-existing condition despite suggestions that inclusive-type deformities are a product of our current lifestyle.17
Early surgical procedures in the early 20th century
The link between these morphological changes and impingement, however, were deduced long after these descriptions.15 The clinical sequelae of hip impingement was in fact first described in 1898 by a British surgeon, John Poland.18 In his extensive review, he mentions a case of traumatic epiphyseal separation (now known as slipped capital femoral epiphysis (SCFE))19 in a 12-year-old boy with reduced range of motion (ROM). It was theorized that the underlying cause was an impingement and he was treated by partial ostectomy of the femoral neck. This corrected the deformity, and he regained full movement of the hip.
This procedure was further elaborated by Mikulicz in 1903, who noticed a loss of the concavity of the femoral neck in patients with SCFE and carried out a ‘bumpectomy’ to relieve the impingement (Figure 2).20 Whitman conducted a similar operation in 1909 on a 15-year-old girl who presented with a limp and stiffness of the right hip due to a “sharp angular anterior border of the neck”.21 Again, through removing the projection, the child made a remarkable recovery and had nearly full ROM. Several reports confirmed these were not isolated cases,22,23 although postoperative outcomes were variable and in one case led to ‘almost complete ankylosis of the hip’.24 On the whole, however, these procedures were successful and Herndon et al25 even showed evidence of long-term benefit.
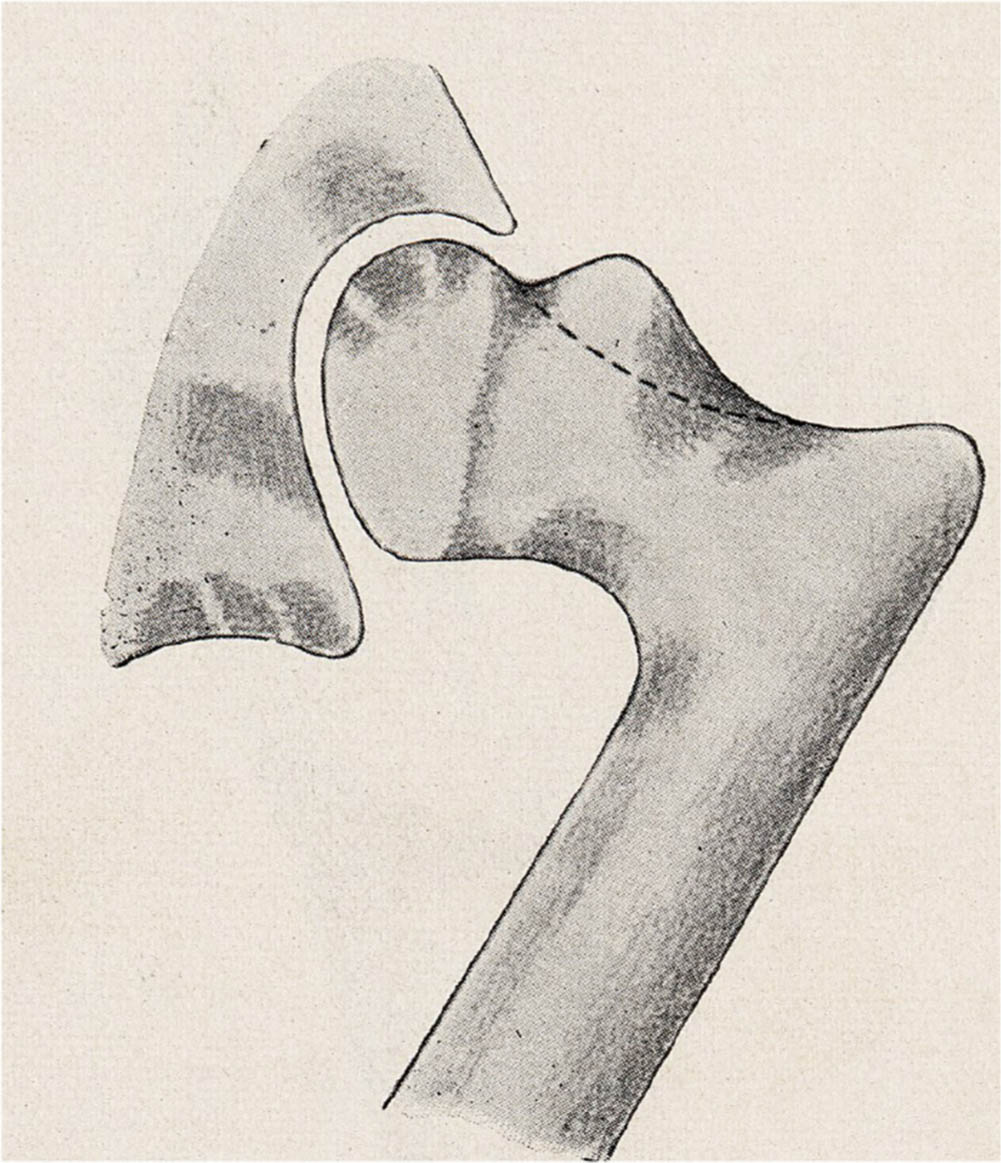
Fig. 2
Diagram illustrating the ‘bump’ causing the impingement. The dotted line outlines the border for bumpectomy.
Smith-Petersen26 in 1936 also recognized the potential of surgical intervention in patients with impingement but crucially extrapolated this theory to treat a lady with hip pain from protrusio acetabuli, a pincer-type deformity. Further, Smith-Petersen outlined his surgical approach, which involved accessing the femoral head anteriorly, allowing impingement to be assessed intraoperatively.
Rise of radiological findings in the 20th century
Non-focal pincer-type deformities, and more specifically protrusio acetabuli, were the first type of FAI to be noted radiologically in 1911.27 Over the next couple of decades, over 50 radiological examples of protrusio acetabuli were described but as there were no common criteria, only straightforward cases could be diagnosed. To rectify this, Köhler described protrusion as the point the floor of the hip-socket touches or crosses the border of the ilioischial line.28 In 1962, protrusio acetabuli was clarified as the point the femoral head overlaps this line to distinguish it from coxa profunda, which was defined as the point the acetabular floor was medial to the line but the femoral head was lateral to it.29
Radiological methods to assess coverage of the acetabulum were also described as early as 1939 by Wiberg,30 who constructed two lines passing through the centre of the femoral head: one travelling along the longitudinal axis and the other passing tangentially through the superolateral edge of the acetabular roof. The angle between the two lines is known as the lateral centre-edge angle (CEA). The study, however, mainly focused on under-coverage of the acetabulum and the threshold of over-coverage (44°) was only determined in 1999.31
Radiological evidence of cam-type impingement was found indirectly while researching the underlying aetiology of idiopathic OA. Elmslie32 in 1933 described in his review that “pre-existing deformity” often preceded characteristic radiological findings of OA.
In 1965, Murray noted OA was linked to “slight” anatomical variations.33 In particular, he found 39.5% of patients with idiopathic OA had a “tilt deformity”, described as a “medial angulation of the femoral head to the femoral neck”. Using a combination of radiological views, Stulberg et al34 in 1975 found further anomalies in the contours of the femoral head and neck. There was evidence of flattening of the neck, displacement of the head so it was off-centre, ‘hooking’ at the head-neck junction, and a bump on the anterolateral surface of the neck. Together the deformity was labelled ‘pistol-grip’.
Claims that the deformities might be a consequence of OA instead of the cause were rebuked by Harris,35 who analyzed radiographs of patients with pistol grip deformities before and after their osteoarthritic changes and noted 90% of patients had their deformity before. It is now widely recognized that these deformities not only lead to OA but are also indicators of cam-type deformities.
Another related radiological finding is the small oval radiolucent area located on the superior quadrant of the femoral neck known as the ‘herniation pit’. Pitt et al36 in 1982 found these pits corresponded to the cervical fossae and more recent reports show these are more prevalent in patients with FAI.15
Spotting focal pincer-type impingement on a regular radiograph can be difficult; therefore, it was only discovered in 1987 when Tönnis37 used a CT scan on a patient with hip pain and found evidence of acetabular retroversion. Reynolds et al38 in 1999 then published a paper detailing two features visible on an anteroposterior radiograph that indicated acetabular retroversion: the crossover sign and an absent posterior wall (Figure 3).
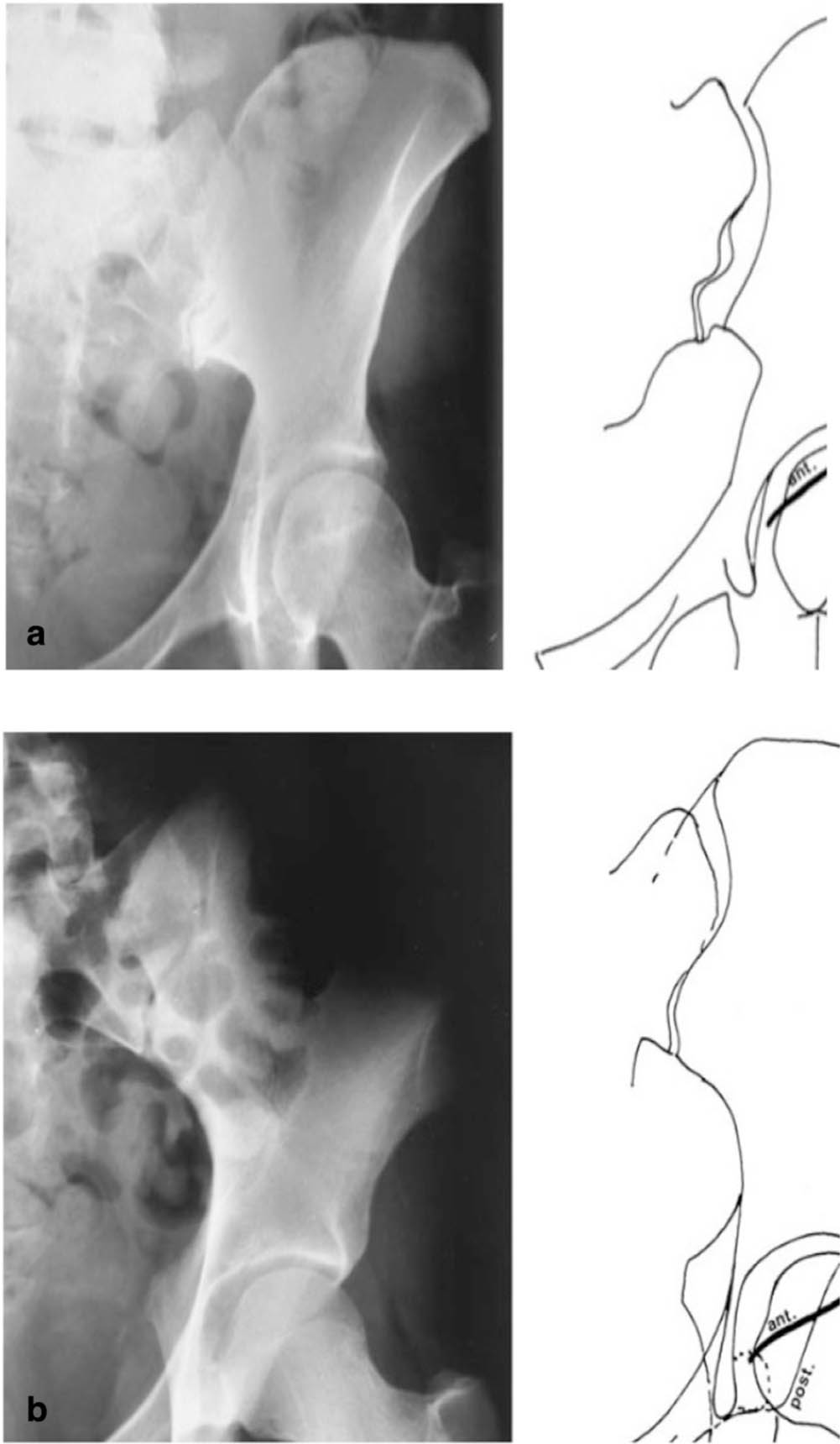
Fig. 3
a) In a normal acetabulum, the line outlining the edge of the anterior rim always lies medial to the line outlining the posterior rim and the line of the edge of the posterior wall descends laterally or through the centre of the femoral head. b) In a retroverted acetabulum, there is an overlap of the two lines (‘crossover sign’) and the line outlining the posterior rim descends medially (‘absent posterior wall’).
A sudden rise in interest of femoroacetabular impingement during the turn of the 21st century
Almost a century after Poland’s description, impingements caused by other secondary cam-type deformities were described. In 1991, Ganz et al4 reported cases following femoral head fractures and in 1993, Snow et al3 described cases following childhood Perthes’ disease.
Then in 1999 Myers et al7 used the term ‘femoroacetabular impingement’ for the first time in the literature. In their study, they outlined cases of impingement caused as a complication to periacetabular osteotomy. It is noteworthy that this study used surgical dislocation;7 this gave an unrestricted view of the femoroacetabular joint, which was key to understanding primary cam-type deformities.
Parallel to these surgical discoveries, our understanding of the radiology behind FAI was being refined. Markers such as ‘pistol grip’ and ‘tilt’ deformities neglect many cases of FAI, especially those resulting from subclinical slipped epiphysis.39 They are also qualitative and so the degree of deformity cannot be ascertained. This led to development of more precise and sensitive tools for diagnosing FAI: α angle and head-neck offset.
The α angle quantifies the loss of concavity at the femoral head-neck junction and was first described by Nötzli et al40 in 2002. Using oblique angle magnetic resonance images, they drew a best-fit circle around the femoral head and two straight lines from the centre of the head. One line passes through the centre of the neck, the other passes through the anterior point at which the distance from the centre of the head to the edge of the bone exceeds the radius of the head. The angle between these two lines is defined as the α angle and a cut-off value (42°) was used to diagnose cam-type deformity.41
The femoral head-neck junction may, however, not feature an obvious focal deformity and the α angle fails to account for this. Another radiological measure – the head-neck offset – is therefore necessary. This was described by Eijer et al42 in 2001 and is calculated by drawing three parallel lines. The first is drawn through the centre of the femoral neck. The second and third are drawn parallel to the first line, with the former being drawn at a tangent to the concave neck and the latter being drawn at a tangent to the convex head. The offset is then measured as the distance between the second and third line. To standardize the measure across all hips, a ratio of the anterior to posterior head-neck offset is used with a cut-off value now generally accepted as < 0.17.43
Research surrounding FAI was rising but as a concept was not fully developed until the review by Ganz et al1 in 2003. They organized seemingly disparate past findings while adding their own experience from surgical dislocation to describe FAI in its entirety from its mechanism to its treatment.
Beyond 2003: deconstructing established theories
After 2003, research into FAI rose exponentially and over 2,000 studies have been published on it since 1999. Along with new discoveries, there has been greater scrutiny on previously accepted theories, especially radiological features.
Although the α angle is regarded as the most commonly used radiological marker to determine cam-type impingement,44 there are still controversial elements associated with it. The major point of discussion involves the threshold at which impingement should be diagnosed and this currently varies from 42° to 83°.44,45 Discrepancies can be explained by differences in the methodology of calculating the threshold and the imaging methods used. Further, nearly all calculations rely on asymptomatic hips as reference;40,46 however, 25% of the asymptomatic young male population has evidence of FAI.47 Agricola et al48 in 2014 tried to obviate this problem by combining asymptomatic and early osteoarthritic populations. They noticed a bimodal distribution in the populations separately and when combined, demonstrating a split in the distribution of α angles with and without cam-deformity.48 They then took the threshold at which these two distributions could be best distinguished, which was determined as 60°. There are, however, further problems to the alpha-angle beyond the threshold including its specificity to impingement and variability between clinicians.45 As a result, the α angle is no longer used in isolation to diagnose cam-type FAI.
Issues surrounding radiological diagnoses are not limited to cam-type deformities. Acetabular retroversion, for example, is notoriously difficult to diagnose on an anteroposterior radiograph and even on a well-positioned radiograph, the crossover sign is thought to overestimate acetabular retroversion.49 Since 2003, a more specific radiological sign - ischial spine projection - has been identified as an improvement on the crossover sign.50 Further, the link between coxa profunda and pincer-type impingement has been questioned.51
In conclusion, although believed to be a novel concept, evidence of FAI has existed in the literature for at least a couple of centuries in a variety of different contexts. The seemingly disparate models were summarized succinctly by Ganz et al1 in 2003 and became the foundation of our current understanding of FAI. As more research has been published, however, the less clear FAI has become and there are now disagreements on how FAI should be diagnosed or even what FAI really is. In the midst of this, it is difficult to determine what the true gold standard recommendations should be.
With such an exponential increase in published literature, confusion such as this is inevitable and it is following a similar pattern to previous pathologies such as shoulder impingement.45 Therefore, appreciating the origin of our knowledge, not just in terms of its diagnosis as we have outlined in this review but also in its treatment, becomes all the more important. In doing so, the direction of future research may perhaps become a little clearer.
References
1. Ganz R , Parvizi J , Beck M , et al. Femoroacetabular impingement: a cause for osteoarthritis of the hip . Clin Orthop Relat Res . 2003 ( 417 ): 112 – 120 . Crossref PubMed Google Scholar
2. Mamisch TC , Kim YJ , Richolt JA , Millis MB , Kordelle J . Femoral morphology due to impingement influences the range of motion in slipped capital femoral epiphysis . Clin Orthop Relat Res . 2009 ; 467 ( 3 ): 692 – 698 . Crossref PubMed Google Scholar
3. Snow SW , Keret D , Scarangella S , Bowen JR . Anterior impingement of the femoral head: a late phenomenon of Legg-Calvé-Perthes’ disease . J Pediatr Orthop . 1993 ; 13 ( 3 ): 286 – 289 . Google Scholar
4. Ganz R , Bamert P , Hausner P , Isler B , Vrevc F . [Cervico-acetabular impingement after femoral neck fracture] . Unfallchirurg . 1991 ; 94 ( 4 ): 172 – 175 . (Article in German) PubMed Google Scholar
5. Siebenrock KA , Wahab KHA , Werlen S , et al. Abnormal extension of the femoral head epiphysis as a cause of cam impingement . Clin Orthop Relat Res . 2004 ( 418 ): 54 – 60 . Crossref PubMed Google Scholar
6. Tannast M , Siebenrock KA , Anderson SE . Femoroacetabular impingement: radiographic diagnosis-what the radiologist should know . AJR Am J Roentgenol . 2007 ; 188 ( 6 ): 1540 – 1552 . Google Scholar
7. Myers SR , Eijer H , Ganz R . Anterior femoroacetabular impingement after periacetabular osteotomy . Clin Orthop Relat Res . 1999 ( 363 ): 93 – 99 . PubMed Google Scholar
8. Otto AW . Seltene Beobachtungen Zur Anatomie, Physiologie und Pathologie gehörig . 2nd , 1824 : 19 – 20 . Google Scholar
9. Preiser G . [Arthritis of the hip and its relation with abnormal version of the acetabulum] . Zeitschr Chirurg . 1907 ; 89 : 541 . (Article in French) Google Scholar
10. Villotte S . [Some remarks about femoroacetabular impingement and osseous non-metric variations of the proximal femur] . Bull Mém Soc Anthropol Paris . 2009 : 95 – 98 . Google Scholar
11. Poirier P . Traité d’anatomie humaine . Ostéologie . 1911 : 515 . Google Scholar
12. Henle J . Handbuch Der systematischen Anatomie des Menschen . Braunschweig : Knochenlehre , 1855 : 254 . Google Scholar
13. Mellado JM , Radi N . Cam-type deformities: Concepts, criteria, and multidetector CT features . Radiologia . 2015 ; 57 ( 3 ): 213 – 224 . Crossref PubMed Google Scholar
14. Allen H . A system of human anatomy including its medical and surgical relations, section II: bones and joints . Philadelphia : Henry C. Lea’s Sons , 1882 : 189 – 193 . Google Scholar
15. Leunig M , Beck M , Kalhor M , et al. Fibrocystic changes at anterosuperior femoral neck: prevalence in hips with femoroacetabular impingement . Radiology . 2005 ; 236 ( 1 ): 237 – 246 . Crossref PubMed Google Scholar
16. Zurmühle CA , Milella M , Steppacher SD , et al. ArtiFacts: Femoroacetabular Impingement-A New Pathology? Clin Orthop Relat Res . 2017 ; 475 ( 4 ): 973 – 980 . Crossref PubMed Google Scholar
17. Siebenrock KA , Ferner F , Noble PC , et al. The cam-type deformity of the proximal femur arises in childhood in response to vigorous sporting activity . Clin Orthop Relat Res . 2011 ; 469 ( 11 ): 3229 – 3240 . Crossref PubMed Google Scholar
18. Brand RA . 50 years ago in CORR: slipping of the upper femoral epiphysis. Beckett Howorth MD. CORR 1957;10:148-173 . Clin Orthop Relat Res . 2009 ; 467 : 859 – 860 . Crossref PubMed Google Scholar
19. Poland J . Traumatic Separation of the Epiphyses . London : Smith Elder & Company , 1898 : 628 – 630 . Google Scholar
20. Vulpius O , Stoffel A . Orthopädische Operationslehre . Stuttgart : Ferdinand Enke Verlag , 1913 . Google Scholar
21. Whitman R . Further Observations on Injuries of the Neck of the Femur in Early Life . Med Rec . 1909 : 1 – 8 . Google Scholar
22. HEYMAN CH , HERNDON CH , STRONG JM . Slipped femoral epiphysis with severe displacement; a conservative operative treatment . J Bone Joint Surg Am . 1957 ; 39-A : 293 – 303 . PubMed Google Scholar
23. HOWORTH B . Slipping of the upper femoral epiphysis . Clin Orthop . 1957 ; 10 : 148 – 173 . PubMed Google Scholar
24. Key JA . The classic: epiphyseal Coxa vara or displacement of the capital epiphysis of the femur in adolescence . Clin Orthop Relat Res . 2013 ; 471 ( 7 ): 2087 – 2117 . Crossref PubMed Google Scholar
25. HERNDON CH , HEYMAN CH , BELL DM . Treatment of slipped capital femoral epiphysis by Epiphyseodesis and Osteoplasty of the femoral neck . J Bone Joint Surg Am . 1963 ; 45-A ( 5 ): 999 – 1012 . PubMed Google Scholar
26. Smith-Petersen MN . The classic: treatment of malum coxae senilis, old slipped upper femoral epiphysis, intrapelvic protrusion of the acetabulum, and Coxa plana by means of acetabuloplasty. 1936 . Clin Orthop Relat Res . 2009 ; 467 ( 3 ): 608 – 615 . Crossref PubMed Google Scholar
27. Schertlin . Ueber einen fall von intrapelviner Vorwolbung und centraler Wanderung Der Huftpfann . Beitr. z. klin . 1911 ; 71 : 406 . Google Scholar
28. Kohler A . Roentgenology: the borderlands of the normal and early pathological in the Skiagram . London : Bailliere, Tindall, and Cox , 1935 . Google Scholar
29. RUELLE M , DUBOIS JL . [The protrusive malformation and its arthrosic complication. I. Radiological and clinical symptoms. Etiopathogenesis] . Rev Rhum Mal Osteoartic . 1962 ; 29 : 476 – 489 . (Article in French) PubMed Google Scholar
30. Wiberg G . Studies on dysplastic Acetabula and congenital subluxation of the hip joint with special references to the complication of osteoarthritis . Acta Chirurgica Scandinavica . 1939 ; 83 . Google Scholar
31. Tönnis D , Heinecke A . Acetabular and femoral anteversion: relationship with osteoarthritis of the hip . J Bone Joint Surg Am . 1999 ; 81-A : 1747 – 1770 . Crossref PubMed Google Scholar
32. Elmslie RC . Remarks on aetiological factors in osteo-arthritis of the hip-joint . BMJ . 1933 ; 1 ( 3757 ): 1 – 46 . Crossref PubMed Google Scholar
33. Murray RO . The aetiology of primary osteoarthritis of the hip . Br J Radiol . 1965 ; 38 ( 455 ): 810 – 824 . Crossref PubMed Google Scholar
34. Stulberg SD . Unrecognised childhood disease: a major cause of idiopathic osteoarthritis of the hip . In : Cordell LD , Harris WH , Ramsey PL , MacEwen GD , eds . The Hip: Proceedings of the Third Open Scientific Meeting of the Hip Society . St Louis, Missouri : CV Mosby , 1975 : 212 – 228 . Google Scholar
35. Harris WH . Etiology of osteoarthritis of the hip . Clin Orthop Relat Res . 1986 ( 213 ): 20 – 33 . PubMed Google Scholar
36. Pitt MJ , Graham AR , Shipman JH , Birkby W . Herniation pit of the femoral neck . American Journal of Roentgenology . 1982 ; 138 ( 6 ): 1115 – 1121 . PubMed Google Scholar
37. Tönnis D . Congenital Dysplasia and Dislocation of the Hip in Children and Adults . Heidelberg : Springer-Verlag Berlin Heidelberg , 1987 . Google Scholar
38. Reynolds D , Lucas J , Klaue K . Retroversion of the acetabulum. A cause of hip pain . J Bone Joint Surg Br . 1999 ; 81-B : 281 – 288 . Crossref PubMed Google Scholar
39. Goodman DA , Feighan JE , Smith AD , et al. Subclinical slipped capital femoral epiphysis. Relationship to osteoarthrosis of the hip . J Bone Joint Surg Am . 1997 ; 79-A ( 10 ): 1489 – 1497 . PubMed Google Scholar
40. Nötzli HP , Wyss TF , Stoecklin CH , et al. The contour of the femoral head-neck junction as a predictor for the risk of anterior impingement . J Bone Joint Surg Br . 2002 ; 84-B ( 4 ): 556 – 560 . Crossref PubMed Google Scholar
41. Clohisy JC , Carlisle JC , Beaulé PE , et al. A systematic approach to the plain radiographic evaluation of the young adult hip . J Bone Joint Surg Am . 2008 ; 90-A ( Suppl 4 ): 47 – 66 . Crossref PubMed Google Scholar
42. Eijer H , Leunig M , Mahomed MN , Ganz R . Cross-Table lateral radiographs for screening of anterior femoral head-neck offset in patients with Femoro-Acetabular impingement . HIP International . 2001 ; 11 ( 1 ): 37 – 41 . Google Scholar
43. Peelle MW , Della Rocca GJ , Maloney WJ , Curry MC , Clohisy JC . Acetabular and femoral radiographic abnormalities associated with labral tears . Clin Orthop Relat Res . 2005 ; 441 : 327 – 333 . Crossref PubMed Google Scholar
44. Nepple JJ et al. Diagnostic imaging of femoroacetabular impingement . J Am Acad Orthop Surg . 2013 ; 21 ( Suppl 1 ): S20 – 26 . Crossref PubMed Google Scholar
45. Reiman MP , Thorborg K . Femoroacetabular impingement surgery: are we moving too fast and too far beyond the evidence? Br J Sports Med . 2015 ; 49 ( 12 ): 782 – 784 . Crossref PubMed Google Scholar
46. Meyer DC , Beck M , Ellis T , Ganz R , Leunig M . Comparison of six radiographic projections to assess femoral head/neck asphericity . Clin Orthop Relat Res . 2006 ; 445 : 181 – 185 . Crossref PubMed Google Scholar
47. Reichenbach S , Jüni P , Werlen S , et al. Prevalence of cam-type deformity on hip magnetic resonance imaging in young males: a cross-sectional study . Arthritis Care Res . 2010 ; 62 ( 9 ): 1319 – 1327 . Crossref PubMed Google Scholar
48. Agricola R , Waarsing JH , Thomas GE , et al. Cam impingement: defining the presence of a CAM deformity by the alpha angle: data from the check cohort and Chingford cohort . Osteoarthritis Cartilage . 2014 ; 22 ( 2 ): 218 – 225 . Crossref PubMed Google Scholar
49. Zaltz I , Kelly BT , Hetsroni I , Bedi A . The crossover sign overestimates acetabular Retroversion . Clin Orthop Relat Res . 2013 ; 471 ( 8 ): 2463 – 2470 . Crossref PubMed Google Scholar
50. Kalberer F , Sierra RJ , Madan SS , Ganz R , Leunig M . Ischial spine projection into the pelvis: a new sign for acetabular retroversion . Clin Orthop Relat Res . 2008 ; 466 : 677 – 683 . Google Scholar
51. Nepple JJ , Lehmann CL , Ross JR , Schoenecker PL , Clohisy JC . Coxa profunda is not a useful radiographic parameter for diagnosing pincer-type femoroacetabular impingement . J Bone Joint Surg Am . 2013 ; 95-A ( 5 ): 417 – 423 . Google Scholar
Author contributions
K. Matsumoto: Carried out the primary research, Wrote the manuscript.
R. Ganz: Provided the historical perspective, Edited the manuscript.
V. Khanduja: Conceptualized and supervised the study, Provided the initial papers on history, Liaised with the original author for historical detail, Edited and assumed overall responsibility for the manuscript.
Funding statement
The author or one or more of the authors have received or will receive benefits for personal or professional use from a commercial party related directly or indirectly to the subject of this article.
ICMJE COI statement
R. Ganz reports personal payment of stock from Examedical S.p.A. Italy, unrelated to this article.
V. Khanduja reports personal payments for lectures including service on speakers bureaus, from Smith & Nephew and Arthrex, unrelated to this article. V. Khanduja also reports an associate editor position on The Bone & Joint Journal.
Follow V. Khanduja @CambridgeHipDoc
© 2020 Author(s) et al. This is an open-access article distributed under the terms of the Creative Commons Attribution Non-Commercial No Derivatives (CC BY-NC-ND 4.0) licence, which permits the copying and redistribution of the work only, and provided the original author and source are credited. See https://creativecommons.org/licenses/by-nc-nd/4.0/.









