Abstract
Objectives
The purpose of this study was to compare the joint space width between one-leg and both-legs standing radiographs in order to diagnose a primary osteoarthritis of the knee.
Methods
Digital radiographs of 100 medial osteoarthritic knees in 50 patients were performed. The patients had undergone one-leg standing anteroposterior (AP) views by standing on the affected leg while a both-legs standing AP view was undertaken while standing on both legs. The severity of the osteoarthritis was evaluated using the joint space width and Kellgren-Lawrence (KL) radiographic classification. The t-test was used for statistical analysis.
Results
The mean medial joint space width found in the one-leg and in the both-legs standing view were measured at 1.8 mm and 2.4 mm, respectively (p < 0.001, 95% CI 0.5 to 0.7). 33%, 47.4% and 23.1% of the knees diagnosed with a KL grade of I, II and III in the both-legs standing views were changed to KL grade II, III and IV in the one-leg standing views, respectively. No changes for KL IV osteoarthritis diagnoses have been found between both- and one-leg standing views.
Conclusions
One-leg standing radiographs better represent joint space width than both-legs standing radiographs. 32% of both-legs standing radiographs have changed the KL grading to a more severe grade than that in the one-leg standing radiographs.
Cite this article: P. Pinsornsak, K. Naratrikun, S. Kanitnate, T. Sangkomkamhang. The one-leg standing radiograph: An improved technique to evaluate the severity of knee osteoarthritis. Bone Joint Res 2016;5:436–441. DOI: 10.1302/2046-3758.59.BJR-2016-0049.R1.
Article focus
-
The study compared the severity of osteoarthritis (OA) in knees when using one-leg and both-legs standing radiographs.
Key messages
-
One-leg standing radiographs better represented joint space width in an OA knee than both-legs standing radiograph.
-
Approximately one third of the both-legs standing radiographs changed their Kellgren-Lawrence classification to a more severe grade than had been judged from the one-leg standing radiographs.
-
We recommend using a one-leg standing radiograph to assess the severity of OA in the knee.
Strengths and limitations
-
Strength: Assessment by one-leg standing radiograph is a simple technique for assessing the severity of OA knee.
-
Limitations: This technique was not applied to all patients. In particular, it was not applied to those who could not bear weight.
-
Our technique can examine only the distal femoral articulation due to the full extension of the knee joint in the standing position. The posterior femoral condyle articulation cannot be assessed with this technique. The flexion weight-bearing knee radiograph will better represent posterior erosion in these cases.
Introduction
Osteoarthritis (OA) is a common cause of knee pain in the elderly which is diagnosed by clinical signs, symptoms, and radiographs.1 Both-legs standing radiographs of the knee are one of the standard measurement tools used in assessing the severity of disease. The Kellgren-Lawrence (KL) classification is a popular method for grading the severity of OA of the knee from plain radiographs in four classifications.2 Grade I is a doubtful narrowing of the joint space and possible osteophytic lipping; grade II is a possible narrowing of the joint space with the definite presence of osteophytes; grade III shows moderate multiple osteophytes, definite narrowing of the joint space, some sclerosis, and possible deformity of bone ends; and grade IV is the presence of large osteophytes, marked narrowing of the joint space, severe sclerosis, and a definite deformity of the bone ends.
Treatment options for knee OA depend on the severity of the disease, which is usually determined by the clinical presentation and radiographs. Chronic knee pain with severe joint space narrowing (KL II to IV) in a both-legs standing radiograph of the knee is usually treated with surgery. However, in patients with knee pain and mild to moderate joint space narrowing (KL I to II), it is usually treated with conservative methods.
For evaluation of the joint space, weight-bearing knee radiographs have shown better results compared with supine radiographs.3 The standard, anteroposterior (AP), weight-bearing knee radiographs are usually performed by standing on both legs. We found a number of patients with severe symptomatic knee OA who would require knee surgery. However, the joint space width was measured as KL grade I to II in both legs on standing radiographs. Re-evaluation with the use of one leg standing radiographs found that the KL grading had changed to grade III-IV (Fig.1). Also, complete cartilage loss had been confirmed during the surgery. Joint space width may be larger in both legs on standing due to avoidance of weight-bearing on the painful arthritic knee or by shared weight-bearing between both legs.

Fig.
Radiographs showing the patient performing (a) both-legs and (b) one-leg standing anteroposterior view of the left knee.
Inaccurate assessment of the joint space affects clinical decision making. Joint space evaluation is also important for determining the treatment for unicompartmental knee arthroplasty. Varus/valgus stress radiographs are well known as a way of evaluating the real cartilage thickness, but there is the disadvantage of radiation exposure to the technician and the fact that it is technically demanding to reproduce a reliable radiograph.4 Flexed knee weight-bearing is another popular technique for evaluating a narrowing joint space, as it is more accurate than both-legs standing radiographs, which correlates with the arthroscopic findings of posterior femoral condyle erosion in these cases.5,6 Several degrees of the knee flexion (15° to 45°) have shown decreased joint space narrowing of the OA knee.7-12 However, standing with the knee flexed in order to get an accurate evaluation is more technically demanding and is a difficult position for the patient to maintain.7
The purpose of this current study was to compare the severity of joint space narrowing and KL grading between one-leg and both-leg standing radiographs in the evaluation of primary medial compartmental OA of the knee.
Materials and Methods
In the period between July and November 2013, 50 patients (100 knees) who had been suffering with symptomatic bilateral knee pain, and had been diagnosed with primary medial compartmental knee OA by the American College of Rheumatology clinical criteria, were included in the study.1 All of the patients had medial knee pain with at least three of the following six clinical criteria: 50 years of age or older, had shown stiffness lasting less than 30 minutes, had exhibited crepitus, bony tenderness, bony enlargement and no palpable warmth of the synovium. We excluded three patients with inflammatory arthritis (two with gouty arthritis, and one with rheumatoid arthritis), one patient with a previous history of knee injury resulting in arthroscopic surgery, one patient with valgus osteoarthritis and two patients who were unable to bear weight on one leg.
This study was approved by the Ethics Committee, Institutional Review Board of Thammasat University (Registry #MTU-EC-OT-6-045/55) and all participants provided written informed consent.
Digital radiographs of both knees were taken for all patients. The both-legs standing AP radiographs were performed by standing in full extension and with equal weight-bearing on both legs (Fig. 2). In the one-leg standing anteroposterior radiograph, the patient was instructed to stand on the affected leg while elevating the contralateral leg and holding on to the support pole in order to avoid falling (Fig. 2). The patella was positioned facing the x-ray beam,which was set at a 10° caudal tilt parallel to the joint line with its focus at the centre of each knee. The distance from the x-ray source to the knee, from the knee to cassette, as well as the exposure, were controlled by the technician in all radiographs. All radiographic magnification was calibrated with the metal coin that had been attached to the medial portion of the knee.
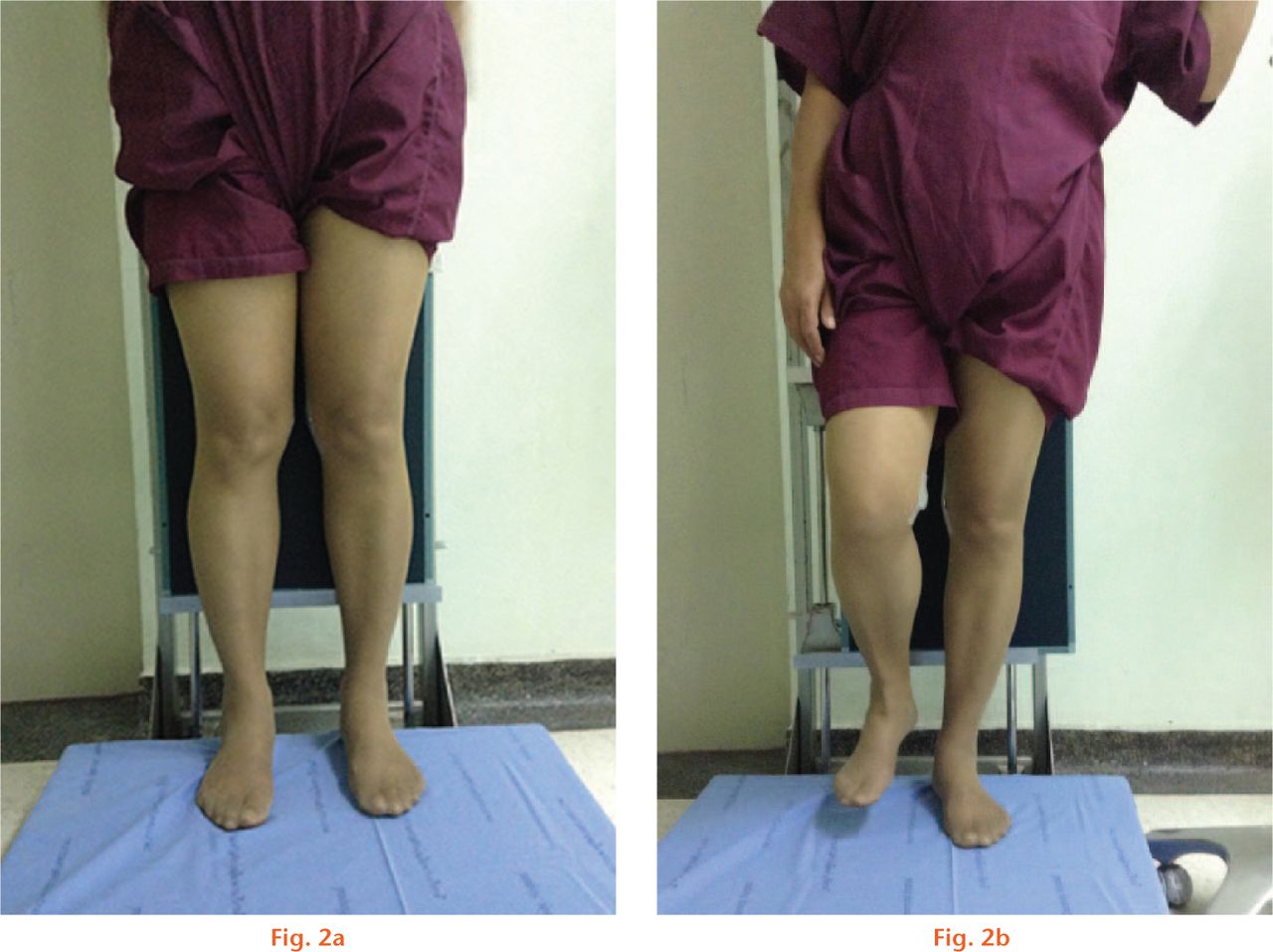
Fig.
Photographs showing the method of performing (a) both-legs and (b) one-leg standing views of the knee.
The severity of OA knee was evaluated using the KL classification. The medial/lateral joint space width, which was recorded perpendicular to the joint line at the narrowest point of each compartment (Fig. 3), was measured in all radiographs. The tibiofemoral angle was measured from the angle between the anatomical axis of the femur and tibia (Fig. 4). Measurements were performed on the digital screen by the measurement tool in the Picture Archiving and Communication System (PACS), Synapse programme (FUJIFILM Medical Systems Inc., Hanover Park, Illinois). The reliability of the measurements (Cronbach’s alpha coefficient) was assessed by two independent orthopaedic surgeons (NK and KS), with two measurements taken a month apart. The observers were blinded to all clinical information and type of radiograph.
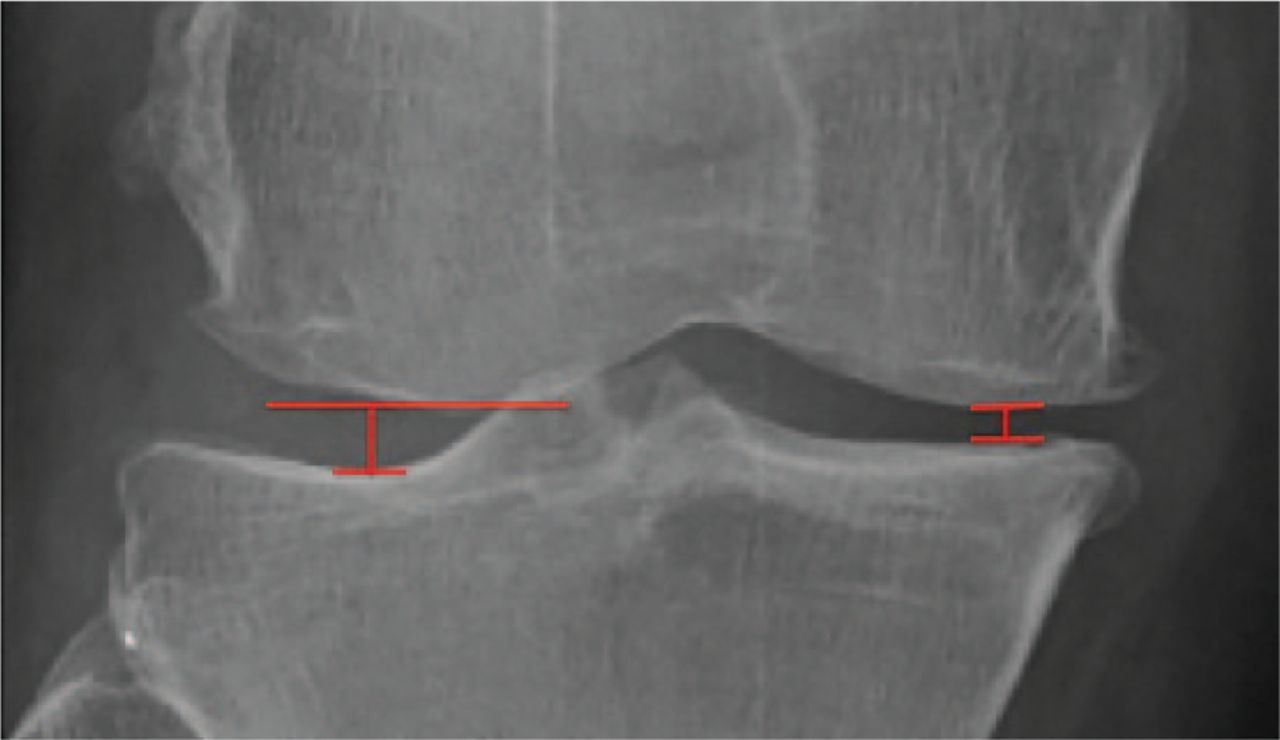
Fig. 3
Radiograph showing the measurement of joint space width of the medial and lateral joint spaces of the knee. We measured at the narrowest point of each joint space.

Fig. 4
Radiograph showing the measurement of the tibiofemoral angle.
From the ten patients in our pilot study which were included to determine the difference of medial joint space width between the two groups, with a 5% level of significance and at 80% power, the mean medial joint space widths in the both-leg and the one-leg standing films were 2.37 mm and 1.81 mm, respectively, which had produced a sample size of 100 knees per group. The chi-squared test and paired t-test were used for the parametric data, and the Mann-Whitney U test for non-parametric data; all statistical analyses were performed using SPSS software version 13 (SPSS Inc, Chicago, Illinois).
Results
Of the 50 patients, 44 (88%) were female, and six (12%) were male. The mean age was 61.12 years (standard deviation (sd) 7.67). The mean body mass index (BMI) was 26.03 kg/m2 (sd 3.96). With the standard both-legs standing view, we found 15% at KL grade I, 38% at KL grade II, 39% at KL grade III, and 8% at KL grade IV. The mean tibiofemoral angle was measured at 3.1° (sd 2.5°) varus in the both-legs and 3.47° (sd 3.2°) in the one-leg standing radiographs (p-value = 0.013, 95% confidence interval 0.08 to 0.66).
The reproducibility of the joint space evaluation was good. For both-legs standing radiographs, the inter-observer and intra-observer kappa values (K) were 0.58 and 0.64. For one-leg standing radiographs, kappa values were 0.57 and 0.65, respectively. The mean medial joint space width decreased from 2.4 mm in the both-legs standing radiographs to 1.8 mm in the one-leg standing radiographs. The mean lateral joint space width increased from 4.3 mm in the both-legs standing radiographs to 4.8 mm in the one-leg standing radiographs (Table I). Based on the KL grading in both-legs standing radiographs, the one-leg standing radiograph showed a significant decrease in the medial joint space width in KL I to III (Table II). Comparing the KL grading of both-legs with the one-leg standing radiographic view, 33.3% (five of 15) of the knees which had been classified as KL I in the both-legs standing radiographs were changed to KL II in the one-leg standing radiographs. In all, 47% (18 of 38) of KL II in the both-legs standing radiographs were changed to KL III, and 23.1% (9 of 39) with KL III in the both-legs standing radiographs were changed to KL IV, but there were no changes in KL IV grades from the both-legs to the one-leg standing radiographic view (Table III). There were no patients who moved up two KL grades (i.e. grade I to III or II to IV) based on one-leg standing radiographs.
Table I.
Mean and differences in joint space width between both-legs and one-leg standing radiographs
| Side | Mean (mm) |
Differences both-leg/one-leg (standard deviation) | 95% confidence interval | p-value (paired t-test) | |
|---|---|---|---|---|---|
| Both-legs | One-leg | ||||
| Medial | 2.4 | 1.8 | 0.6 (0.5) | 0.5 to 0.7 | < 0.001 |
| Lateral | 4.3 | 4.8 | 0.5 (0.7) | 0.4 to 0.6 | < 0.001 |
Table II.
Mean and differences in medial joint space width (MJSW) between both-legs and one leg standing radiographs and Kellgren-Lawrence (KL) classification based on both-legs standing radiographs
| KL classification based on both-legs | % of knees | Mean MJSW |
Differences both-leg/one-leg (standard deviation) | 95% confidence interval | p-value (paired t-test) | |
|---|---|---|---|---|---|---|
| Both-legs | One-leg | |||||
| I | 15 | 3.9 | 3.3 | 0.6 (0.8) | 0.1 to 1.0 | 0.009 |
| II | 38 | 2.8 | 2.2 | 0.6 (0.5) | 0.5 to 0.8 | < 0.001 |
| III | 39 | 1.9 | 1.3 | 0.6 (0.5) | 0.4 to 0.7 | < 0.001 |
| IV | 8 | 0 | 0 | 0 | – | – |
Table III.
The Kellgren-Lawrence (KL) classification according to the both- legs and one leg standing view
| KL classification based on both-legs standing (knees) | KL classification based on one-leg standing (knees) n (%) |
|||
|---|---|---|---|---|
| I | II | III | IV | |
| I | 10 (66.7) | 5 (33.3) | ||
| II | 20 (52.6) | 18 (47.4) | ||
| III | 30 (76.9) | 9 (23.1) | ||
| IV | 8 (100) | |||
Discussion
Misdiagnosis of mild to moderate OA (rather than severe OA) based on the joint space visualised in both-legs standing radiographs impedes patient care due to delayed surgical intervention. The present study shows a technique for assessing the severity of knee OA which better represents joint space narrowing, is easy to apply, and is cost effective compared with more sophisticated investigation (i.e. MRI).
This study has several limitations. First, the one-leg standing radiograph is not applicable to all patients. Elderly patients with severe knee pain and who are unable to stand on one leg are not candidates for this investigation. However, intra-articular injections of a local anaesthetic (4 mL of 1% lidocaine) for pain relief prior to taking the images can be arranged for some of these patients. For the patients who could not bear weight due to other reasons, standing radiographs would not be the diagnostic tool of choice. However, MRI6 could be used. Secondly, our technique can examine only the distal femoral articulation due to the full extension of the joint required in the standing position. Posterior femoral condyle articulation cannot be assessed with this technique. The flexion weight-bearing knee radiograph5,8 will better represent posterior erosion in these cases. Thirdly, for the patient demonstrating large osteophytic rim formation, the weight-bearing radiograph will not represent cartilage erosion due to the contact between the osteophytes. Lastly, even the standing radiographs of patients who exhibit decreased joint space may not represent the actual severity of knee pain in OA, and clinical correlation will still need to be considered to plan treatment.
The measurement of radiographic joint space width is reliable and represents cartilage erosion in the patient with knee OA.13,14 In this study, we have found increased KL grading in one-leg compared with both-legs standing radiographs in the mild to moderate (KL I to III), but not in the severe osteoarthritic knee (KL IV). This supports our hypothesis that standing on both legs does not put the patient’s full weight on the affected knee and results in errors in the evaluation of the cartilage. Moreover, a narrower joint space width in one-leg standing may possibly be a result of the slight flexion of the knee. Buckland-Wright et al15 reported a 7° to 10° flexed knee weight-bearing radiograph better represented narrowing joint space than both knee extension and Lyon Schuss views. One-leg standing radiographs better represent the real joint space in mild to moderate knee OA with good inter- and intra-observer reliability. Unfortunately, standing with full knee extension is only representative of the distal articulating surface. Rosenburg et al8 proposed a 45° posteroanterior knee flexion weight-bearing technique and found better accuracy than the full extension weight-bearing anteroposterior view in evaluation of joint space narrowing. A 30° posteroanterior knee flexion weight-bearing view (standing tunnel view) reported a better representation of joint space narrowing compared with a conventional knee full extension, weight-bearing radiograph.6,10 The study compares three radiographic views for the evaluation of medial compartment OA (both-legs and one-leg standing in full extension AP, and 30° knee flexion in the PA view) and has found the lowest joint space width in the 30° knee flexion PA view (2.8 mm, sd 1.8), followed by the one-leg standing in full extension AP (3.2 mm, sd 1.5), and then with both leg standing in full extension AP (3.5 mm, sd 1.5). There were no differences in non-osteoarthritic knees.16 However, we prefer one-leg standing radiographs over the knee flexion weight-bearing technique, as standing in knee flexion is more difficult to control the angle and maintain flexion for OA patients.
MRI is the best diagnostic tool for direct visualisation of the cartilage, bone, meniscus and ligaments, but has limited availability, is time-consuming, uncomfortable for the patient and expensive.6 Due to these limitations, the role of MRI is usually reserved for research or in cases in which the diagnosis is unclear.
In conclusion, approximately 32% of both-legs standing radiographs have changed the KL grading to a more severe grade than that of the one-leg standing radiographs. We recommend the use of the one-leg rather than both-legs standing radiographs for evaluating cartilage thickness of knee OA in patients who are able to tolerate this procedure. The knee flexion radiograph is recommended as an additional tool in the assessment of symptomatic OA, where full extension weight-bearing radiographs fail to show joint space narrowing.
Funding Statement
None declared.
Acknowledgement: We thank C. Amatyakul for help with the statistical analysis.
ICMJE conflict of interest
None declared.
References
1 Altman R , AschE, BlochD, et al.. Development of criteria for the classification and reporting of osteoarthritis. Classification of osteoarthritis of the knee. Arthritis Rheum1986;29:1039-1049.CrossrefPubMed Google Scholar
2 Kellgren JH , LawrenceJS. Radiological assessment of osteo-arthrosis. Ann Rheum Dis1957;16:494-502.CrossrefPubMed Google Scholar
3 Leach RE , GreggT, SiberFJ. Weight-bearing radiography in osteoarthritis of the knee. Radiology1970;97:265-268.CrossrefPubMed Google Scholar
4 Eriksson K , Sadr-AzodiO, SinghC, OstiL, BartlettJ. Stress radiography for osteoarthritis of the knee: a new technique. Knee Surg Sports Traumatol Arthrosc2010;18:1356-1359.CrossrefPubMed Google Scholar
5 Davies AP , CalderDA, MarshallT, GlasgowMM. Plain radiography in the degenerate knee. A case for change. J Bone Joint Surg [Br]1999;81-B:632-635.CrossrefPubMed Google Scholar
6 Guermazi A , RoemerFW, BursteinD, HayashiD. Why radiography should no longer be considered a surrogate outcome measure for longitudinal assessment of cartilage in knee osteoarthritis. Arthritis Res Ther2011;13:247.CrossrefPubMed Google Scholar
7 Yamanaka N , TakahashiT, IchikawaN, YamamotoH. Posterior-anterior weight-bearing radiograph in 15 degree knee flexion in medial osteoarthritis. Skeletal Radiol2003;32:28-34.CrossrefPubMed Google Scholar
8 Rosenberg TD , PaulosLE, ParkerRD, CowardDB, ScottSM. The forty-five-degree posteroanterior flexion weight-bearing radiograph of the knee. J Bone Joint Surg [Am]1988;70-A:1479-1483.PubMed Google Scholar
9 Messieh SS , FowlerPJ, MunroT. Anteroposterior radiographs of the osteoarthritic knee. J Bone Joint Surg [Br]1990;72-B:639-640.CrossrefPubMed Google Scholar
10 Vignon E , PipernoM, Le GraverandMP, et al.. Measurement of radiographic joint space width in the tibiofemoral compartment of the osteoarthritic knee: comparison of standing anteroposterior and Lyon schuss views. Arthritis Rheum2003;48:378-384.CrossrefPubMed Google Scholar
11 Mason RB , HorneJG. The posteroanterior 45 degrees flexion weight-bearing radiograph of the knee. J Arthroplasty1995;10:790-792.CrossrefPubMed Google Scholar
12 Niinimäki T , OjalaR, NiinimäkiJ, LeppilahtiJ. The standing fixed flexion view detects narrowing of the joint space better than the standing extended view in patients with moderate osteoarthritis of the knee. Acta Orthop2010;81:344-346.CrossrefPubMed Google Scholar
13 Ravaud P , GiraudeauB, AuleleyGR, et al.. Radiographic assessment of knee osteoarthritis: reproducibility and sensitivity to change. J Rheumatol1996;23:1756-1764.PubMed Google Scholar
14 Reichmann WM , MaillefertJF, HunterDJ, et al.. Responsiveness to change and reliability of measurement of radiographic joint space width in osteoarthritis of the knee: a systematic review. Osteoarthritis Cartilage2011;19:550-556.CrossrefPubMed Google Scholar
15 Buckland-Wright JC , WolfeF, WardRJ, FlowersN, HayneC. Substantial superiority of semiflexed (MTP) views in knee osteoarthritis: a comparative radiographic study, without fluoroscopy, of standing extended, semiflexed (MTP), and schuss views. J Rheumatol1999;26:2664-2674.PubMed Google Scholar
16 Piperno M , Hellio Le GraverandMP, ConrozierT, et al.. Quantitative evaluation of joint space width in femorotibial osteoarthritis: comparison of three radiographic views. Osteoarthritis Cartilage1998;6:252-259.CrossrefPubMed Google Scholar









