Abstract
Objectives
Nylon sutures and skin staples are used commonly in total knee arthroplasty (TKA) surgical wound closure. However, there is no study that compares the wound healing efficacy and patient satisfaction scores of both techniques in the same knee.
Methods
We randomised 70 patients who underwent primary TKA into two groups. In one group of 34 patients, the skin at the upper half of the wound was closed with skin staples and the lower half of the wound was closed with simple interrupted nylon sutures. In the other group of 36 patients, the skin at the upper half of the wound was closed with nylon stitches and the lower half of the wound was closed with skin staples. We recorded the wound closure time, pain score at the time of stitch removal, wound complication rate, patient satisfaction score, and the Hollander wound evaluation score at the post-operative periods of five days, 14 days, six weeks, three months, and six months. Each half wound was analysed separately.
Results
The mean patient body mass index was 26.8 kg/m2 (standard deviation 6.3). A total of 70 nylon stitched wounds and 70 skin stapled wounds were analysed. There were no significant differences in wound complication rates, patient satisfaction score, and the Hollander wound evaluation score between both types of wounds (p > 0.05). The wound closure time for skin stapled wounds was significantly lower than the nylon stitched wounds (p < 0.001). However, the skin stapled wounds had a significantly higher pain score at the time of stitch removal (p < 0.001).
Conclusion
Skin staples and nylon stitches had comparable results with respect to wound healing and patient satisfaction in TKA wound closure in non-obese patients. The benefit of skin staples over nylon stitches was a decrease in operative time, but was more painful upon removal.
Cite this article: V. Yuenyongviwat. A randomised controlled trial comparing skin closure in total knee arthroplasty in the same knee: nylon sutures versus skin staples. Bone Joint Res 2016;5:185–190. DOI: 10.1302/2046-3758.55.2000629.
Article focus
-
We aimed to compare the efficacy and safety of nylon sutures and skin staples for total knee arthroplasty wound closure.
Key messages
-
There were no differences in the wound complication rate, patient satisfaction, and cosmesis between skin staples and nylon stitches.
-
The benefit of skin staples over nylon stitches was a decrease in operative time.
-
Skin staples are more painful upon removal compared with nylon stitches.
Strengths and limitations
-
Strength: This study is a prospective randomised controlled trial which evaluated both techniques in the same knee in order to balance the healing potential, rehabilitation protocol, wound care, and patient compliance confounders.
-
Limitation: We could not blind the patients from the different methods of closure in the patient’s knee.
Introduction
Successful surgical wound healing is one factor that increases post-operative patient function and satisfaction. Wound complications can affect patient recovery, increase the cost of treatment, and prolong the hospital stay.1-3 Total knee arthroplasty (TKA) requires early rehabilitation to improve range of movement (ROM) but might increase stress on the surgical wound.4-7 Therefore, the skin closure technique is an important factor to avoid wound complications.8,9 The principles of a proper skin closure technique include a tension-free and watertight closure without skin-edge inversion.10 The surgical wound should heal rapidly and be cosmetically acceptable without wound infection and dehiscence.9
There are many types of materials and methods for skin closure, but nylon sutures and skin staples are the two techniques used most commonly in orthopaedic surgery.11 Theoretically, a stapled wound has no ‘cross-hatched’ scarring because the tissue is able to expand under the ‘open rectangle’ formation of the staple compared with a simple interrupted suture, which applies tension at the healing skin edge.12,13 Many studies which compared the efficacy and complications of wound closure techniques between skin staples and various types of sutures have shown controversial results. A report showed an increased risk of wound infection in closure by staples compared with sutures.11 On the other hand, some studies reported no difference in the rate of wound complications between sutures and staples.14,15 However, some also found a lower rate of complications from staple closure compared with suture closure.9
Although many studies compared the efficacy and safety of suture with skin staples for orthopedic wound closure, the number of studies that compared nylon sutures to skin staples in TKA is limited. In particular, there is no study that compares both of these techniques in the same knee in order to balance the healing potential, rehabilitation protocol, wound care, and patient compliance confounders which may affect the rate of wound healing and wound complications. Therefore, this study aims to compare the efficacy and safety of nylon sutures and skin staples in the same knee.
Patients and Methods
This prospective randomised controlled trial was conducted between June 2013 and April 2014. A total of 75 patients scheduled for primary TKA were invited into this study. The patients were aged between 50 to 80 years and had a full understanding of the questions in this study. The exclusion criteria were patients who had previous knee surgery, history of cancer in the process of cancer treatment, and history of nickel allergy. Two patients were excluded from the study because of previous knee surgery and three patients declined to participate in the study. Finally, 70 patients were enrolled in the study and provided written informed consent. This study was approved by the local Ethics Committee and Institutional Review Board. The procedures in this study were in accordance with the Declaration of Helsinki on ethical principles for medical research involving human subjects.16
Patients were randomised into two groups by blocks of four using a computer generated random number.17 Opaque sealed envelopes were used for allocation concealment. The random allocation was done in the operative room after subcutaneous stitches were finished. In the first group of 34 patients, the skin on the upper half of the wound was closed with skin staples and the lower half of the wound was closed with simple nylon stitches. In the second group of 36 patients, the skin on the upper half of the wound was closed with nylon stitches and the lower half of the wound was closed with skin staples. The patients were randomised into different suture positions to decrease confounding factors from different soft-tissue conditions between the upper and lower parts of the TKA wound.
All patients underwent TKA with the same surgical techniques and instruments. Cemented posterior stabilised total knee prostheses (NexGen Legacy posterior-stabilised (LPS-flex), Zimmer, Warsaw, Indiana) were used in every patient. Cefazolin was injected 30 minutes prior to starting the operation for prophylaxis against surgical infection. Clindamycin was used for patients with a penicillin or cephalosporin allergy. A single dose of tranexamic acid was injected before inflating a tourniquet. The operations were performed under inflated pneumatic tourniquet throughout the operation. A suction drain was placed in the joint before the joint capsule was closed. For capsule closure figure-of-eight stitches by No. 1 polyglactin 910 (Coated Vicryl Plus, Ethicon Inc., Somerville, New Jersey) were used. For subcutaneous approximation suture 3-0 polyglactin 910 (Coated Vicryl Plus, Ethicon Inc.) with buried knots was used. After subcutaneous suturing, the wound length was measured with a sterile ruler. The skin was then closed with skin staples (Proximate Plus MD 35 W, Ethicon Endo-surgery LLC, Guaynabo, Peurto Rico) for half of the length of the wound and 4-0 nylon (Ethilon, Ethicon Inc.) simple interrupted stitches for the second half of the wound (Fig. 1). Skin closure was undertaken in the 45° knee flexion position. The stitches were placed 10 mm apart.
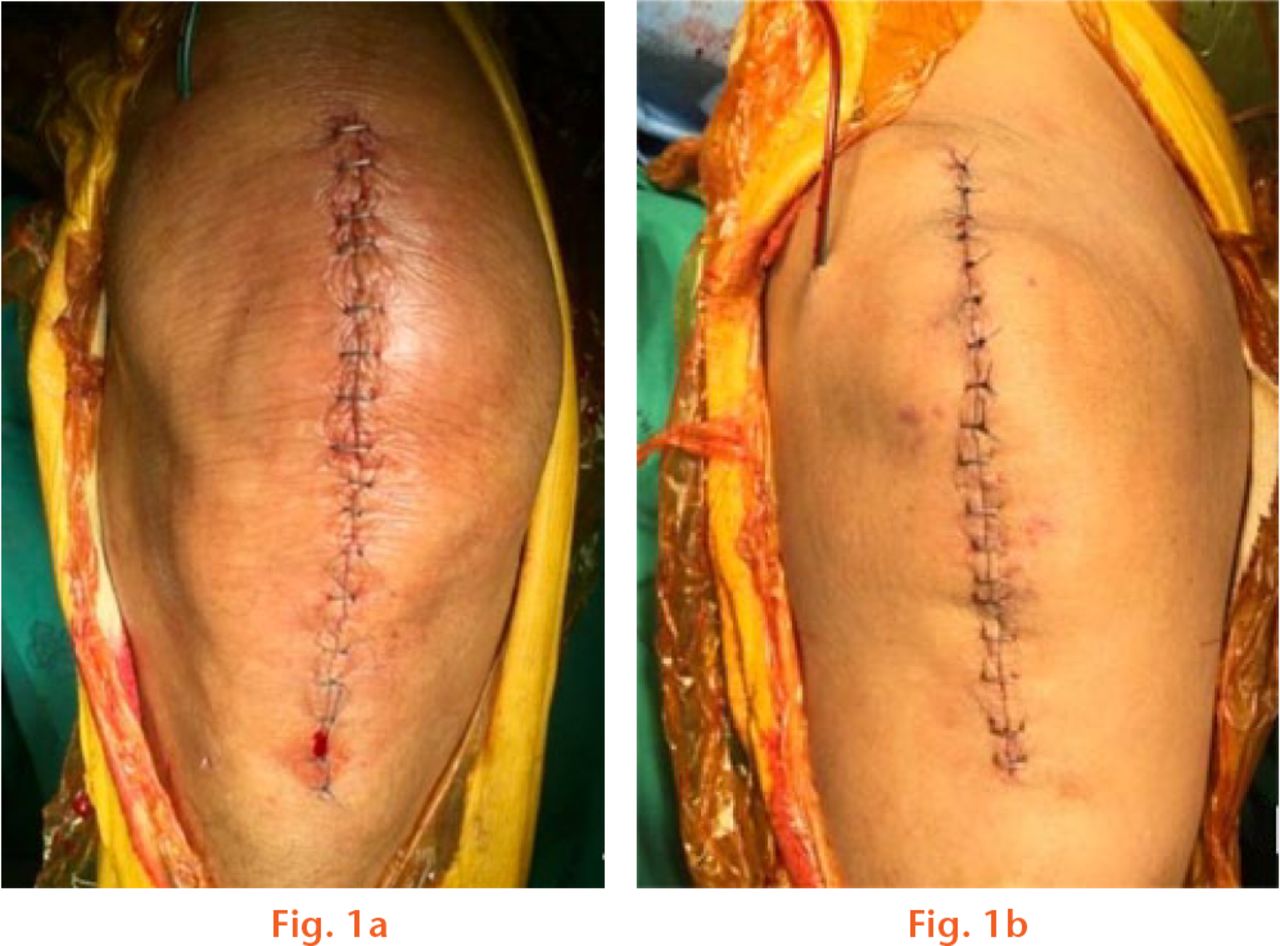
Fig.
Photographs showing how half of the wound was closed with staples and other half with nylon sutures; a) staple/suture group, b) suture/staple group.
Early ROM exercise and ambulation with a supportive device was started at post-operative day 1. Wound care was performed with a Betadine swab (Betadine, Ids Manufacturing Co., Ltd, Pathum Thani, Thailand) and covered with sterile gauze daily. Aspirin was used as the thromboembolic prophylaxis. The suction drain was removed at 48 hours after the operation. The patients were followed up at day 5, day 14 and six weeks, three months, and six months after surgery. The stitches were removed on post-operative day 14.
The level of pain was recorded by a verbal numeric rating scale (VNRS) from 0 (no pain) to 10 (worst imaginable pain) immediately after the stitches were removed. Wound complications such as stitch abscess, wound dehiscence, prolonged discharge, and the resuture rate were recorded. In the study design, if a wound developed a generalised infection, we would consider that both the proximal and distal ends of the wound had developed the complication.
The degree of patient satisfaction with the wound appearance was also evaluated by a VNRS where 10 indicated ‘Most satisfied’ and 0 represented ‘Least satisfied’. The Hollander wound evaluation score was used for wound cosmetic evaluation. The assessor evaluated the wounds on a 0 or 1 point scale in each category for the presence or absence of a step-off, contour irregularities, margin separation, edge inversion, excessive distortion, and overall appearance.18
Wound complications and patient satisfaction were recorded on day 5, day 14, six weeks, three months, and six months after surgery. The Hollander wound evaluation scores were recorded at day 14, six weeks, three months, and six months after surgery. Pain upon removal of the stitches and the degree of patient satisfaction were recorded by a trained member of staff who was blinded to treatment allocation. However, wound complications and the Hollander wound evaluation scores were recorded by another member of staff who was not blinded to treatment allocation, as direct wound observation was required for every follow-up visit.
Statistical analysis
The analyses were performed with R version 3.1.0 software (R Foundation for statistical computing, Vienna, Austria). The Kolmogorov-Smirnov test was used to determine normal distribution. Patient demographic data such as age, weight, height, body mass index (BMI), incision length, total operative time, and total drainage were compared with the Student’s t-test. Fisher’s exact test was used to compare gender, operative side, American Society of Anesthesiologists (ASA)19 classification, and wound complication rates. The differences between the skin stapled wounds and nylon stitched wounds with regard to the VNRS for patient satisfaction, Hollander wound evaluation score, VNRS for pain upon stitch removal, and stitching time were evaluated by the Wilcoxon signed-rank test. The Kruscal-Wallis test was used for subgroup analyses of the VNRS for patient satisfaction and the Hollander wound evaluation scores.
Based on previous research,8 a statistical power analysis was performed for sample size estimation. To detect a 20% difference in wound complication rate with a significance level set to 0.05 and a power set to 0.9, 55 samples per group were required.
Demographics and description of study population
The patient demographic data of both groups are shown in Table I. There were no significant differences in terms of age, gender, side of operation, weight, height, BMI, ASA classification, incision length, and operative time.
Table I.
Demographic data
| Characteristic | Group 1, n = 34 (staple/suture) | Group 2, n = 36 (suture/staple) | p-value |
|---|---|---|---|
| Age (yrs) | 67 (sd 8.3)* | 70.2 (sd 9.1)* | 0.13 |
| Gender (male:female) | 4:30 | 9:27 | 0.22 |
| Side (right:left) | 16:18 | 18:18 | 0.82 |
| Weight (kg) | 61.6 (sd 8.2)* | 63.4 (sd 11)* | 0.41 |
| Height (cm) | 155.4 (sd 6.3)* | 152.4 (sd 8.8)* | 0.11 |
| Body mass index (kg/m2) | 25.6 (sd 3.6)* | 27.4 (sd 4.1)* | 0.06 |
| American Society of Anesthesiologists classification (I:II) | 8:26 | 11:25 | 0.60 |
| Incision length (mm) | 125.7 (sd 9.5)* | 126.4 (sd 9)* | 0.52 |
| Operative time (min) | 104.2 (sd 16.7)* | 103.1 (sd 23.6)* | 0.36 |
| Total drainage (ml) | 448 (sd 207)* | 539 (sd 255)* | 0.11 |
-
*
Values are expressed as mean and standard deviation (sd)
Accounting for all patients
All of the 70 enrolled patients (34 patients in Group 1 and 36 patients in Group 2) completed the study; therefore, 70 nylon stitched wounds and 70 skin stapled wounds were analysed (Fig. 2).
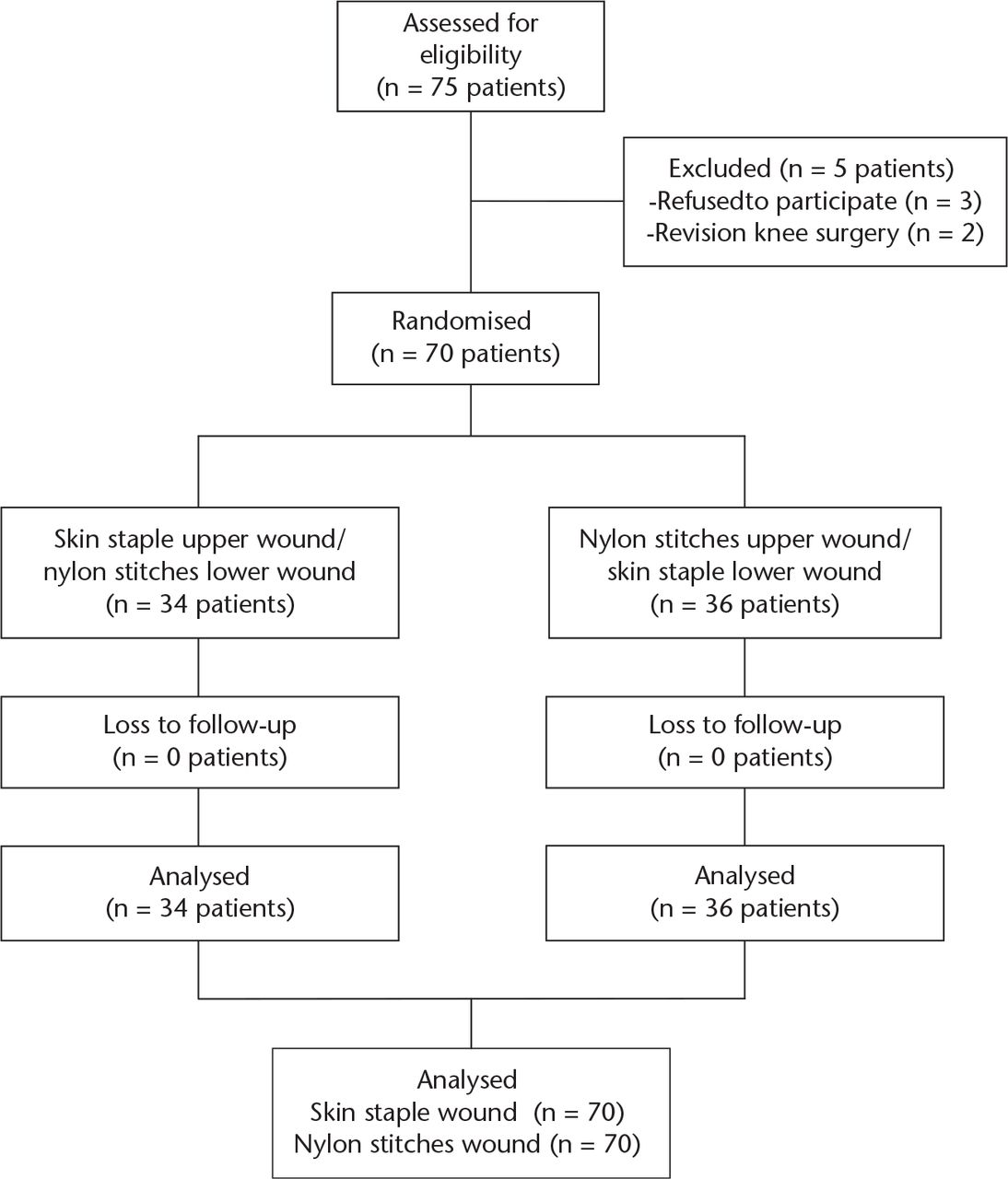
Fig. 2
Flow study diagram.
Results
There were no differences in the wound complication rates such as prolonged discharge, stitch abscess, wound dehiscence, or re-suture rate between the skin stapled wounds and nylon stitched wounds at day 5, day 14, six weeks, three months, and six months post–operation (Table II). Prolonged discharge was the main complication which was found mostly on day 5 post-operatively and was found in only one case at day 14 post-operatively. However, none of these cases required debridement or re-suturing.
Table II.
Post-operative wound complications
| Post-operative date | Staple (n = 70 ) | Suture (n = 70 ) | p-value |
|---|---|---|---|
| Day 5 | |||
| Prolonged discharge | 4 | 2 | 0.42 |
| Stitch abscess | 0 | 0 | |
| Wound dehiscence | 0 | 0 | |
| Re-suture | 0 | 0 | |
| Day 14 | |||
| Prolonged discharge | 1 | 0 | 0.49 |
| Stitch abscess | 0 | 0 | |
| Wound dehiscence | 0 | 0 | |
| Re-suture | 0 | 0 | |
| 6 wks, 3 mths, 6 mths | |||
| Prolonged discharge | 0 | 0 | |
| Stitch abscess | 0 | 0 | |
| Wound dehiscence | 0 | 0 | |
| Re-suture | 0 | 0 |
The median patient satisfaction score of the wound appearance in skin stapled wound and nylon stitched wound was not significantly different between the groups at day 5, day 14, six weeks, three months, and six months post-operatively (p = 0.72, 0.16, 0.13, 0.7, and 0.13, respectively) (Table III). The median Hollander wound evaluation score also did not differ between skin staple wounds and nylon stitched wounds at two weeks, six weeks, three months and six months post-operatively (p = 0.41, 0.78, 0.64, and 0.81, respectively) (Table IV). The skin stapled wounds had a significantly higher VNRS pain score at the time of stitch removal (median 5; 1 to 10) compared with removal of the nylon stitches (median 3; 0 to 8) (p < 0.001). The median wound closure time for skin stapled wounds was significantly lower than the nylon stitched wounds (skin staple 18 seconds; 8 to 37) versus nylon stitches 208.5 seconds; 126 to 325) (p < 0.001).
Table III.
Median (range) patient satisfaction scores of the wound appearance
| Group | Post-operative date |
||||
|---|---|---|---|---|---|
| Day 5 | Day 14 | 6 wks | 3 mths | 6 mths | |
| Staple | 7 (3 to 9) | 7 (2 to 10) | 9 (5 to 10) | 9 (5 to 10) | 9 (5 to 10) |
| Suture | 7 (4 to 10) | 7 (3 to 10) | 8 (5 to 10) | 8 (4 to 10) | 9 (5 to 10) |
| p-value | 0.72 | 0.16 | 0.13 | 0.07 | 0.13 |
Table IV.
Median (range) Hollander wound evaluation scores
| Group | Post-operative date |
|||
|---|---|---|---|---|
| Day 14 | 6 wks | 3 mths | 6 mths | |
| Staple | 5 (4 to 6) | 5 (5 to 6) | 5 (5 to 6) | 5 (5 to 6) |
| Suture | 5 (4 to 6) | 5 (5to 6) | 5 (5 to 6) | 5 (5 to 6) |
| p-value | 0.41 | 0.78 | 0.64 | 0.81 |
Subgroup analyses were done to compare between nylon stitches in the upper half of the wound, nylon stitches in the lower half of the wound, staples in the upper half of the wound and staples in the lower half of the wound. The results found no statistical significance between the groups in terms of wound complications and the Hollander scores (Tables V and VI). However, patient satisfaction scores at post-operative three months and six months were found to be statistically significantly different between the groups. The lower half of both skin stapled and nylon stitched wounds had a higher patient satisfaction score compared with the upper half of the wound (Table VII).
Table V.
Subgroup. Wound complication of prolonged discharge
| Group | Post-operative date (n, %) |
|
|---|---|---|
| Day 5 | Day 14 | |
| Upper wound | ||
| Nylon | 0 | 0 |
| Staple | 2 (5.9) | 1 (2.8) |
| Lower wound | ||
| Nylon | 2 (5.9) | 0 |
| Staple | 2 (5.6) | 0 |
| p-value | 0.53 | 0.40 |
Table VI.
Subgroup. Median (range) Hollander wound evaluation scores.
| Group | Post-operative date |
|||
|---|---|---|---|---|
| Day 14 | 6 wks | 3 mths | 6 mths | |
| Upper wound | ||||
| Staple | 5 (4 to 6) | 5 (5 to 6) | 5 (5 to 6) | 5 (5 to 6) |
| Suture | 5 (4 to 6) | 5 (5 to 6) | 5 (5 to 6) | 5 (5 to 6) |
| Lower wound | ||||
| Nylon | 5 (4 to 6) | 5 (5 to 6) | 5 (5 to 6) | 5 (5 to 6) |
| Staple | 5 (4 to 6) | 5 (5 to 6) | 5 (5 to 6) | 5 (5 to 6) |
| p-value | 0.94 | 0.25 | 0.15 | 0.14 |
Table VII.
Subgroup. Median (range) patient satisfaction scores of wound appearance
| Group | Post-operative date |
||||
|---|---|---|---|---|---|
| Day 5 | Day 14 | 6 wks | 3 mths | 6 mths | |
| Upper wound | |||||
| Nylon | 6.5 (5 to 8) | 7 (3 to 10) | 8 (5 to 10) | 8 (4 to 10) | 8 (5 to 10) |
| Staple | 7 (5 to 9) | 7 (3 to 10) | 8 (5 to 10) | 8 (5 to 10) | 9 (5 to 10) |
| Lower wound | |||||
| Nylon | 7 (4 to 10) | 7 (3 to 10) | 9 (5 to 10) | 10 (6 to 10) | 10 (6 to 10) |
| Staple | 7 (3 to 9) | 8 (2 to 10) | 9 (5 to 10) | 10 (5 to 10) | 9 (7 to 10) |
| p-value | 0.11 | 0.15 | 0.02 | 0.001* | 0.013* |
-
*
Kruskal-Wallis test - statistically significant differences between the four groups of data
Discussion
There is controversy related to the wound closure technique of the two most common methods i.e. skin staple and nylon suture, in terms of efficacy, rate of complication, and cosmetic outcomes.20 Previous studies were not conducted in the same patient, in which case the wound healing rate might be different from person to person depending on the patient’s activity, wound care, and baseline soft tissue quality. Therefore, the authors of this study evaluated the efficacy of skin staples and nylon sutures in the same knee of the same patient.
This study has a number of limitations. First, we could not blind the patient from the different methods of closure of the patient’s knee because it might increase the difficulty in patient care procedures. Furthermore, the patients could see the wound when the dressings were changed, and after they were discharged from hospital. Secondly, the assessor for wound complications and the Hollander evaluation score was also not blinded from the wound closure method because direct observation for the evaluation of the wound was needed. However, a different assessor was blinded from the wound closure method while recording the VNRS for the patient’s satisfaction and pain score upon stitch removal. Finally, this study was likely underpowered due to the lower than expected complication rate. However, the results of this study will be beneficial in planning a future study that is sufficiently powered to confirm our findings.
The wound complication rate in TKA was not different between the two types of wound closure in this study. Similarly, in a randomised study, Hlubek et al14 found late discharge in 25.6% of fifth post-operative day stapled wounds and late discharge in 30.3% of sutured wounds, and treatment for late discharge was required in 6.1% and 7.7% of sutured wounds and stapled wounds, respectively (no statistical difference). However, in another randomised study by Stockley and Elson,21 skin stapled wounds had a higher rate of wound complications (13.3% marked erythema, 3.3% superficial wound infection) compared with nylon stitched wounds (no outcomes).
There have been no recent studies that compared the results of patient satisfaction of the wound appearance and cosmesis scores between skin staples and nylon stitches. However, there was one randomised controlled trial study that reported no differences in patient satisfaction and the cosmesis score of skin staples compared with 2-octylcyanoacrylate and monocryl subcutaneous suture in TKA patients.8 This study found that skin staples had comparable results with nylon sutures in terms of patient satisfaction and the cosmesis score.
The overall mean BMI in our study was relatively low (26.8 kg/m2, standard deviation 6.3) compared with previous studies which reported a range from 28 kg/m2 to 33.7 kg/m2.9,14 This result was possibly one cause of the lower rate of wound complications compared with previous studies. Therefore, the results from this study should be applied to non-obese patients.
Pain upon staple removal compared with nylon stitches in TKA patients has been previously reported by others. Stockley and Elson21 reported more pain upon removal of skin staples than nylon stitches. Another study also found a higher pain score for staple removal compared with suture removal.22
In conclusion, this study found no differences in the wound complication rate, patient satisfaction of wound appearance, and cosmesis score in TKA wound closure between skin staples and nylon stitches in non-obese patients. The benefit of skin staples over nylon stitches was a decrease in operative time. However, skin staples are more painful upon removal compared with nylon stitches. Based on this, we believe that surgeons can consider either type of skin closure technique which depends on surgeon preferences.
Funding
The authors wish to thank N. Mueangkaew and S. Chuayjuljit for data collection and G. Shingledecker for his assistance in proofreading the English of this study.
This study was funded by the Faculty of Medicine, Prince of Songkla University, Songkhla, Thailand.
ICMJE conflict of interest
None declared.
References
1 Vince KG , AbdeenA. Wound problems in total knee arthroplasty. Clin Orthop Relat Res2006;452:88-90.CrossrefPubMed Google Scholar
2 Livesey C , WyldeV, DescampsS, et al.. Skin closure after total hip replacement: a randomised controlled trial of skin adhesive versus surgical staples. J Bone Joint Surg [Br]2009;91-B:725-729.CrossrefPubMed Google Scholar
3 Kirkland KB , BriggsJP, TrivetteSL, WilkinsonWE, SextonDJ. The impact of surgical-site infections in the 1990s: attributable mortality, excess length of hospitalisation, and extra costs. Infect Control Hosp Epidemiol1999;20:725-730. Google Scholar
4 Moffet H , ColletJP, ShapiroSH, et al.. Effectiveness of intensive rehabilitation on functional ability and quality of life after first total knee arthroplasty: A single-blind randomised controlled trial. Arch Phys Med Rehabil2004;85:546-556. Google Scholar
5 Isaac D , FalodeT, LiuP, et al.. Accelerated rehabilitation after total knee replacement. Knee2005;12:346-350.CrossrefPubMed Google Scholar
6 Bade MJ , Stevens-LapsleyJE. Early high-intensity rehabilitation following total knee arthroplasty improves outcomes. J Orthop Sports Phys Ther2011;41:932-941.CrossrefPubMed Google Scholar
7 Iyengar KP , NadkarniJB, IvanovicN, MahaleA. Targeted early rehabilitation at home after total hip and knee joint replacement: does it work?Disabil Rehabil2007;29:495-502.CrossrefPubMed Google Scholar
8 Khan RJ , FickD, YaoF, et al.. A comparison of three methods of wound closure following arthroplasty: a prospective, randomised, controlled trial. J Bone Joint Surg [Br]2006;88-B:238-242.CrossrefPubMed Google Scholar
9 Patel RM , CayoM, PatelA, AlbarilloM, PuriL. Wound complications in joint arthroplasty: comparing traditional and modern methods of skin closure. Orthopedics2012;35:e641-e646.CrossrefPubMed Google Scholar
10 Shetty AA , KumarVS, Morgan-HoughC, et al.. Comparing wound complication rates following closure of hip wounds with metallic skin staples or subcuticular vicryl suture: a prospective randomised trial. J Orthop Surg (Hong Kong)2004;12:191-193.CrossrefPubMed Google Scholar
11 Smith TO , SextonD, MannC, DonellS. Sutures versus staples for skin closure in orthopaedic surgery: meta-analysis. BMJ2010;340:c1199.CrossrefPubMed Google Scholar
12 Edlich RF , BeckerDG, ThackerJG, RodeheaverGT. Scientific basis for selecting staple and tape skin closures. Clin Plast Surg1990;17:571-578.PubMed Google Scholar
13 Graham DA , JefferyJA, BainD, DaviesP, BentleyG. Staple vs. subcuticular vicryl skin closure in knee replacement surgery: a spectrophotographic assessment of wound characteristics. Knee2000;7:239-243.CrossrefPubMed Google Scholar
14 Hlubek R , WalderP, KánˇaJ, SalounováD. Metal staples versus conventional suture for wound closure in total knee arthroplasty. Acta Chir Orthop Traumatol Cech2014;81:233-237.(In Czech) Google Scholar
15 Shantz JA , VernonJ, LeiterJ, MorshedS, StrangesG. Sutures versus staples for wound closure in orthopaedic surgery: a randomised controlled trial. BMC Musculoskelet Disord2012;13:89. Google Scholar
16 No authors listed. World Medical Association Declaration of Helsinki. http://jama.jamanetwork.com/article.aspx?articleid=1760318 (date last accessed 28 April 2016).PubMed Google Scholar
17 No authors listed. Research Randomizer. http://www.randomizer.org/ (date last accessed 28 April 2016). Google Scholar
18 Hollander JE , SingerAJ, ValentineS, HenryMC. Wound registry: development and validation. Ann Emerg Med1995;25:675-685.CrossrefPubMed Google Scholar
19 Saklad M . Grading of patients for surgical procedures. Anesthiol1941;2:281-284. Google Scholar
20 Newman JT , MorganSJ, ResendeGV, et al.. Modality of wound closure after total knee replacement: are staples as safe as sutures? A retrospective study of 181 patients. Patient Saf Surg2011;5:26.CrossrefPubMed Google Scholar
21 Stockley I , ElsonRA. Skin closure using staples and nylon sutures: a comparison of results. Ann R Coll Surg Engl1987;69:76-78.PubMed Google Scholar
22 Slade Shantz JA , VernonJ, MorshedS, LeiterJ, StrangesG. Sutures versus staples for wound closure in orthopaedic surgery: a pilot randomised controlled trial. Patient Saf Surg2013;7:6. Google Scholar









