Abstract
Objectives
Throughout the 20th Century, it has been postulated that the knee moves on the basis of a four-bar link mechanism composed of the cruciate ligaments, the femur and the tibia. As a consequence, the femur has been thought to roll back with flexion, and total knee arthroplasty (TKA) prostheses have been designed on this basis. Recent work, however, has proposed that at a position of between 0° and 120° the medial femoral condyle does not move anteroposteriorly whereas the lateral femoral condyle tends, but is not obliged, to roll back – a combination of movements which equates to tibial internal/ femoral external rotation with flexion. The aim of this paper was to assess if the articular geometry of the GMK Sphere TKA could recreate the natural knee movements in situ/in vivo.
Methods
The pattern of knee movement was studied in 15 patients (six male: nine female; one male with bilateral TKAs) with 16 GMK Sphere implants, at a mean age of 66 years (53 to 76) with a mean BMI of 30 kg/m2 (20 to 35). The motions of all 16 knees were observed using pulsed fluoroscopy during a number of weight-bearing and non-weight-bearing static and dynamic activities.
Results
During maximally flexed kneeling and lunging activities, the mean tibial internal rotation was 8° (standard deviation (sd) 6). At a mean 112° flexion (sd 16) during lunging, the medial and lateral condyles were a mean of 2 mm (sd 3) and 8 mm (sd 4) posterior to a transverse line passing through the centre of the medial tibial concavity. With a mean flexion of 117° (sd 14) during kneeling, the medial and lateral condyles were a mean of 1 mm (sd 4) anterior and 6 mm (sd 4) posterior to the same line. During dynamic stair and pivoting activities, there was a mean anteroposterior translation of 0 mm to 2 mm of the medial femoral condyle. Backward lateral condylar translation occurred and was linearly related to tibial rotation.
Conclusion
The GMK Sphere TKA in our study group shows movements similar in pattern, although reduced in magnitude, to those in recent reports relating to normal knees during several activities. Specifically, little or no translation of the medial femoral condyle was observed during flexion, but there was posterior roll-back of the lateral femoral condyle, equating to tibiofemoral rotation. We conclude that the GMK Sphere is anteroposteriorly stable medially and permits rotation about the medial compartment.
Cite this article: Professor G. Scott. Can a total knee arthroplasty be both rotationally unconstrained and anteroposteriorly stabilised?: A pulsed fluoroscopic investigation. Bone Joint Res 2016;5:80–86. DOI: 10.1302/2046-3758.53.2000621.
Article focus
-
An in vivo kinematic evaluation of 16 knees replaced using the GMK Sphere total knee arthroplasty.
-
Static and dynamic activities were observed using pulsed fluoroscopy.
-
The kinematics were found to replicate with reduced magnitude the reported kinematics of the normal knee.
Key messages
-
A knee prosthesis which is medially stable due to a spherical medial compartment in the presence of a flat lateral tibial articulation will permit isolated lateral femoral rollback.
Strengths and limitations
-
The well-established method of fluoroscopic evaluation was directed by the originator of the technique.
-
The study was restricted to only 16 knees, but at various durations of follow-up.
-
Ethically, it was only possible to examine the knees on one occasion.
Introduction
In 1904, Zuppinger,1 on the basis of the first experimental study of the knee using radiographs, proposed that both the medial and lateral femoral condyles rolled back across the tibia as the knee flexed. He believed that this occurred under the influence of the cruciate ligaments which were thought to act with the femur and tibia to form a four-bar linkage mechanism. Although this hypothesis was rejected by the leading contemporary anatomists, Fick2 in 1911 and Strasser3 in 1917, over time the four-bar linkage mechanism became generally accepted, being popularised especially by the work of Kapandji.4 As the theory prevailed as the orthodox view of knee movement throughout much of the 20th century, it has heavily influenced the design of knee arthroplasty prostheses.
The first investigators to to question Zuppinger’s hypothesis1 were Brantigan and Voshell.5 In 1941, they observed that as the cadaver knee flexed, the menisci did not move equally but instead the medial meniscus moved little, if at all, whereas the lateral meniscus moved posteriorly. Investigations in Prague by Freeman and Pinskerova6 in which they used anatomical dissection and MRI to study cadaver knees with intact cruciate ligaments confirmed Brantigan and Voshell’s work.5 These conclusions were supported with radiostereometric analysis/CT and 3D digitisation.7 The results of this latter study were independently confirmed by Williams and Logan8 and Johal et al9 who also extended the findings to include the living and the weight-bearing knee. The first total knee arthroplasty (TKA) to be produced with a medially spherical design was the Medial Rotation Knee (MRK, initially Finsbury Orthopaedics, subsequently MatOrtho, Leatherhead, United Kingdom) but it retained a conventional lateral compartment with a roller-in-a-trough geometry. More recently, a less laterally constrained design, also with a medially spherical compartment, the Saiph (MatOrtho), has become available. However, the tibial insert retains some lateral concavity. Kinematic results of the Saiph have recently been reported.10 A further development has been the introduction of another medially spherical TKA with no lateral constraint but instead, like the natural knee, a lateral compartment which is flat anteroposteriorly. This implant is the GMK Sphere (Medacta International AG, Castel San Pietro, Switzerland). Our objective was to assess if the articular geometry of the GMK Sphere TKA could reproduce the pattern of movement first reported in modern times in Prague.11
Patients and Methods
The prosthesis
The GMK Sphere TKA (Fig. 1) has been developed with design features intended to replicate the knee kinematics reported by Freeman and Pinskerova.6 The femoral surface is spherical on the medial side, generally up to 100° (being dependent on the specific size of femoral component), after which the radius closes slightly. The tibial polyethylene insert is also spherical, matching the larger femoral radius. On the lateral side, the femoral surface is again spherical with the same radius as the medial side. In contrast, the lateral tibial surface is flat anteroposteriorly (AP). Mediolaterally, the central section of the lateral tibial articular surface is also flat but medially it curves upwards to conform to the femur while the edge is provided with a 2 mm elevated lip. The prosthesis is implanted after the resection of both cruciate ligaments for surgical convenience and to avoid any possibility of conflict between the theoretical action of the ligaments and the motion which would be guided by the prosthesis itself. With regard to the latter, the intention is to provide a prosthesis which is AP stable from 0° to 120° but which could rotate around a medial longitudinal axis because the lateral femoral condyle is free to roll back across the tibia. Flexion occurs about an axis that passes through the centres of the two spheres (Fig. 1). Thus, the prosthesis would theoretically provide the knee motion suggested as ‘normal’ by Freeman and Pinskerova.6
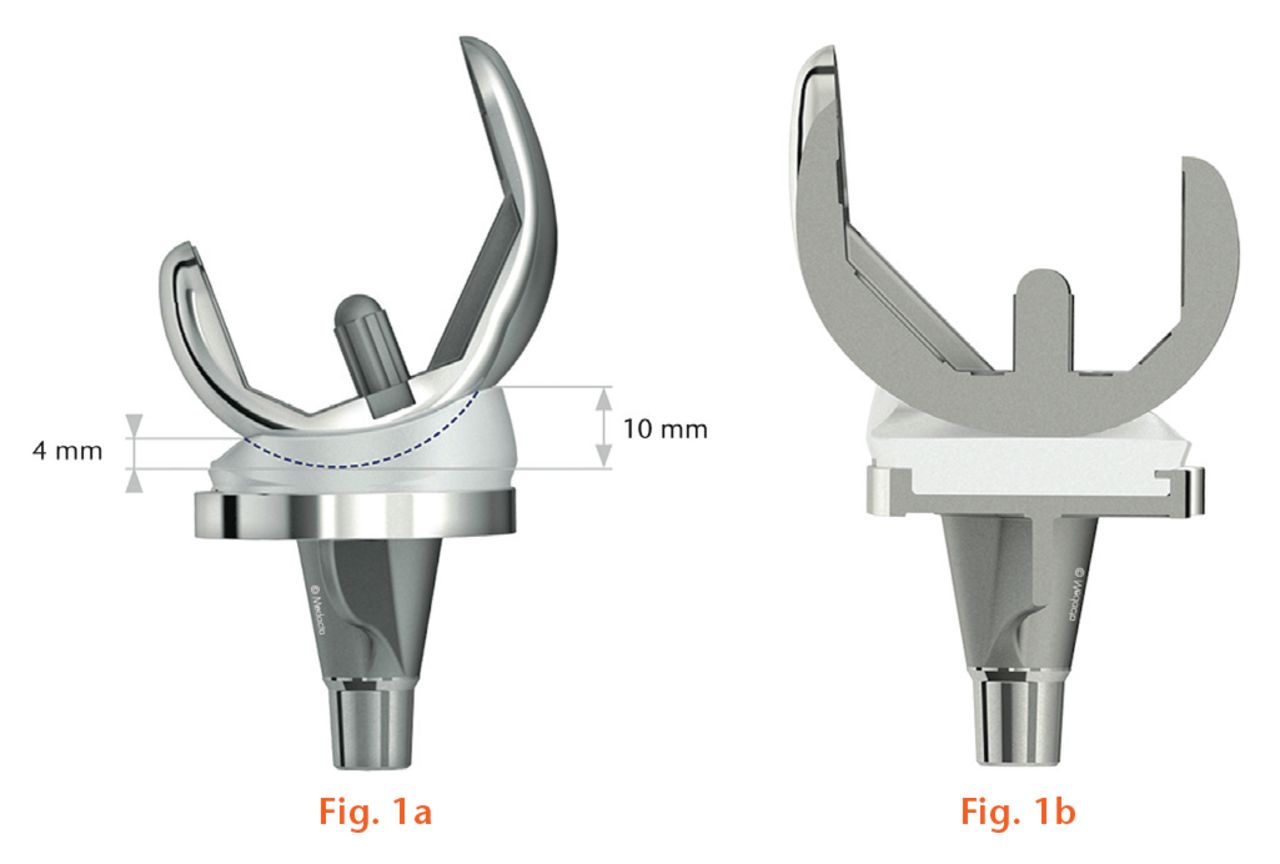
Fig.
The GMK Sphere prosthesis incorporates a spherical medial tibiofemoral articulation (left) to provide anteroposterior stability and a flat lateral tibial surface to permit longitudinal rotation (right).
The patients
Following approval from the Institutional Review Board and the Ethics Committee, patients with the GMK Sphere TKA who were more than six months post-operative, and who were willing to be studied, were recruited from three United Kingdom centres (SWLEOC, RNOH, RLH). Inclusion criteria were patients aged between 50 and 85 years at the time of surgery who had obtained (1) a functional result sufficient to enable them to perform safely the activities of the study with mean post-operative Knee Society Scores12 of 86 points (80 to 90) for the knee and 89 (80 to 100) for function, as well as a mean post-operative Oxford Knee Score13,14 of 40 points (34 to 48) and (2), an unloaded range of movement from an extended position of 0° to 5° to flexion > 90°. Informed written consent was obtained.
A total of 16 knees in 15 patients fulfilled our inclusion criteria. These comprised six men (one with bilateral TKAs) and nine women, with a mean age of 66 years (53 to 76). Their mean BMI was 30 kg/m2 (20 to 35). The 16 knees were operated upon by GS, JS or REF.
Radiological methods
The kinematic investigation was conducted by SAB and AE – the latter assisted in the reading of images. The imaging was conducted at the South West London Elective Orthopaedic Centre using a pulsed fluoroscopy system (Precision RXi Digital System, GE Healthcare, Chalfont St Giles, United Kingdom) to capture images and record them digitally in DICOM format. For all activities, the fluoroscopic unit was positioned to obtain a sagittal projection of the knee being studied. Images for dynamic activities were processed at 15 frames per second, while only single images were used for static deep flexion lunging and kneeling activities. The x-ray beam parameters were 60 to 70 kVp accelerating voltage, 13 ms pulse duration, and 15 frames per second. All images were anonymised before analysis was performed.
The patients’ knee movements were recorded during several static postures and dynamic activities. The static postures were maximum flexion kneeling and lunging.15-19 Dynamic activities were stepping up and down on a 22 cm step without swing-through of the contralateral limb, and pivoting about a fixed foot placement with the weight-bearing knee near extension.9,17,18 The pivoting activity required the patient to plant their foot with the toes pointed outward, and then pivot from a position of femoral internal rotation to femoral external rotation in one smooth fully weight-bearing action.
Digitised images were corrected for optical distortion using bilinear interpolation.20 The Canny edge detector was used to detect implant boundaries.21 The optical geometry of the fluoroscopy system (principal distance, principal point) was determined from images of a calibration target.20 The implant surface model was projected onto the geometrically corrected image, and its three-dimensional pose was iteratively adjusted to match its silhouette with the silhouette of the patients’ implant components and bones. An initial manual registration was subsequently numerically refined using non-linear least-squares minimisation of an edge-based cost function. The results of this shape-matching process have standard errors of approximately 0.5° to 1.0° for rotations and 0.5 mm to 1.0 mm for translations in the sagittal plane.20
Joint kinematics were determined from the three-dimensional pose of each implant using Cardan angles.22 Lateral radiographs of each knee were used to determine the sagittal alignment of the implant components with respect to the mechanical axis of the limb, and these offsets were added to the fluoroscopically measured flexion angles between implant components to provide the anatomical flexion angles. AP translations of the femoral condyles were measured with respect to a medial/lateral line passing through the deepest point of the tibial medial articulation and parallel to the anterior edge of the posterior notch of the tibial baseplate. AP femoral condylar translations were determined from the lowest point on each condyle relative to the transverse plane of the tibial baseplate, which is equivalent to projecting the centre of the spherical condyles onto the same plane for flexion up to about 100°, depending upon the femoral implant size. This system of kinematic analysis in TKA has been widely applied for over 20 years and used to study two other medially spherical designs10,17 and also other non-medially spherical designs.23
Statistical analysis
Descriptive statistics were compiled to permit comparison of measured knee motions with previous reports.6,9,16-19 Comparisons of pre- and post-operative clinical scores, and knee kinematics between lunging and kneeling activities were performed using paired t-tests with significance set at a p-value < 0.05. Linear correlation was used to examine the relationship between longitudinal rotation of the knee and AP translation of the lateral femoral condyle. All statistical tests were performed using Excel (Microsoft, Redmond, Washington).
Results
The mean post-operative interval at the time of the investigation was 10.25 months (6 to 19). On the day of fluoroscopic assessment, the mean range of movement from maximum active extension to maximum supine flexion (i.e. when the knee was unloaded) was 108° (sd 8).
Static activities
The static mean maximum knee flexion obtained during lunging was 112° (sd 16) and 117° (sd 14) for kneeling (p = 0.320, Table I), in the course of which the medial condyle typically remained within a few millimetres of the centre of the concavity of the tibial insert while the lateral condyle translated posteriorly to a degree directly related to tibial internal rotation (Table I, Fig. 2). The medial and lateral condylar AP positions were 2 mm to 3 mm more posterior for lunging than for kneeling (Table I, Fig. 2). A mean 8° tibial internal rotation was observed in maximum flexion in both lunging and kneeling activities (Table I). However, the correlation for lateral condylar posterior translation as a function of maximum flexion during kneeling was only R2 = 0.15.
Table I.
Tibiofemoral kinematics during maximum flexion lunging and kneeling postures with results presented as means with standard deviations (sd), (t-tests for all comparisons).
| Lunge | Kneel | p-value | |
|---|---|---|---|
| Flexion (°) | 112; sd 16 | 117; sd 14 | 0.320 |
| Valgus (°) | -1; sd 2 | -2; sd 2 | 0.163 |
| Tibial internal rotation (°) | 8; sd 6 | 8; sd 6 | 0.930 |
| Medial condyle AP (mm) | -2; sd 3 | 1; sd 4 | < 0.001 |
| Lateral condyle AP (mm) | -8; sd 4 | -6; sd 4 | 0.002 |
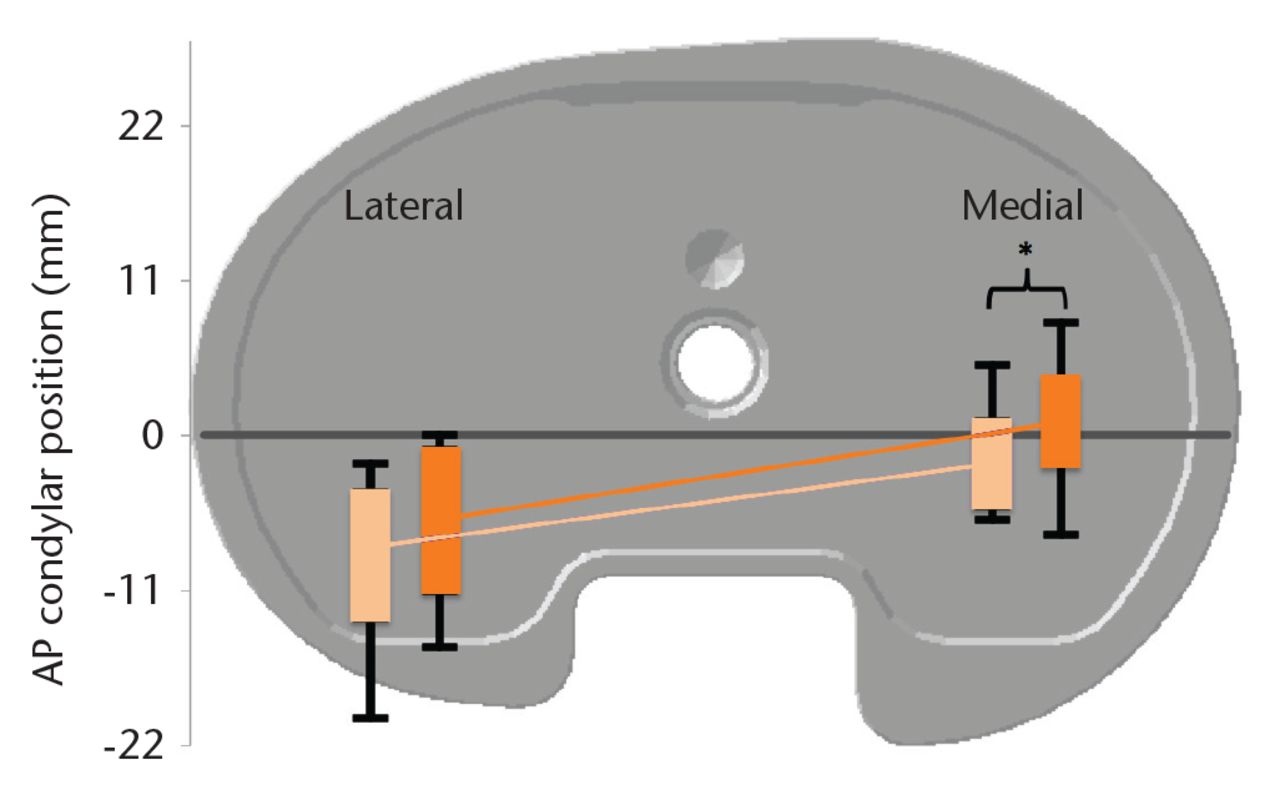
Fig. 2
The femoral condyles show an externally rotated orientation in maximum flexion during lunging (light orange) and kneeling (dark orange) activities. Mean condylar position is indicated by the light and dark orange lines, the colour-filled rectangles show the one standard deviation, and the black bars indicate the extreme range for all knees in the cohort. All translations were normalised to a medium-sized tibial baseplate and referenced to a medial/lateral line (grey) passing through the deepest point of the tibial insert concavity and parallel to the posterior baseplate notch. Normalised medial condylar position was more posterior during lunging than during kneeling activities (t-test, p = 0.04). (AP, anteroposterior).
Dynamic activities
During the step-up/down activity, the femoral medial condylar position generally remained within 1 mm of the centre in the tibial concavity, while the lateral condyle translated posteriorly 5 mm in a direct linear relationship to the amount of tibial internal rotation (R2 = 0.98, Fig. 3). The mean trend for tibial rotation was 5° tibial internal rotation with 60° increasing flexion but there was wide variation between knees (Fig. 4a). There was a small individual variation in medial condylar translation, with all knees showing medial condylar positions within 3 mm of the centre of the tibial concavity during the stepping motion (Fig. 4b). Lateral femoral condylar translations showed wide individual variation coupled with the tibial rotations (Fig 4c).
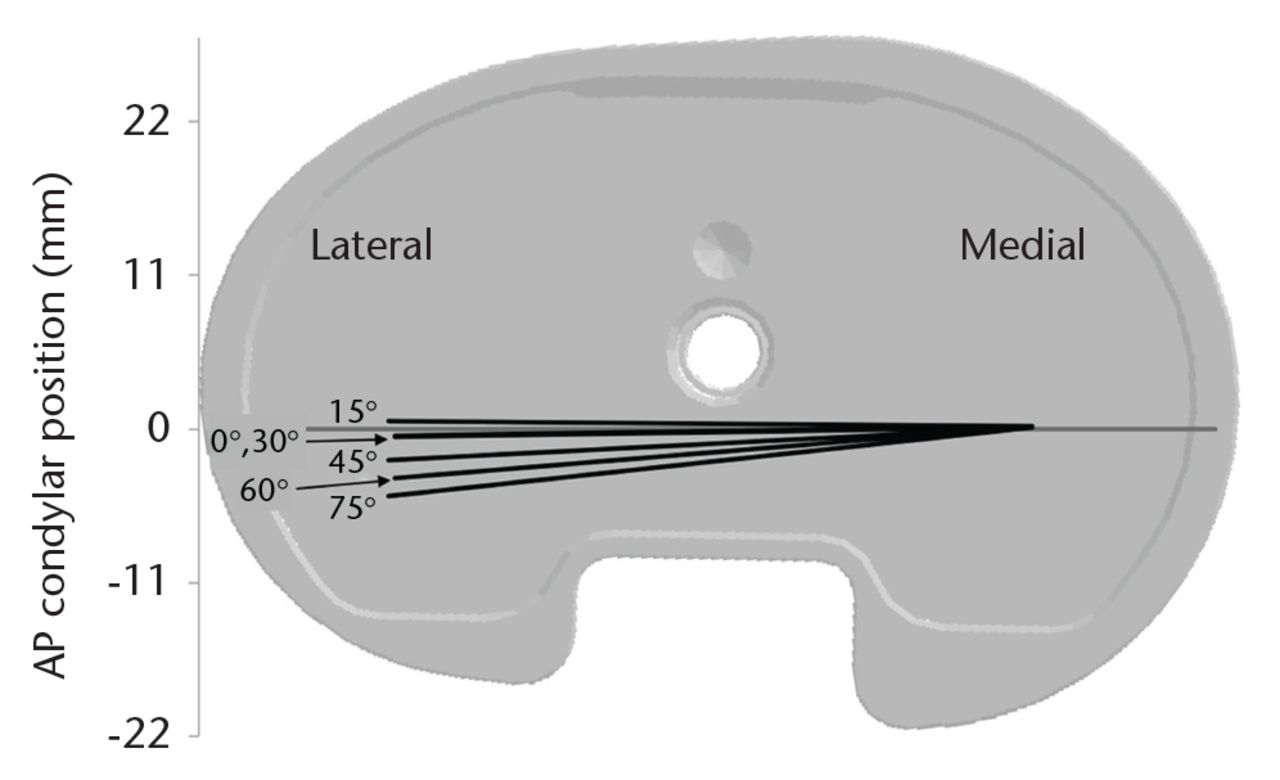
Fig. 3
The femoral condyles rotate about a fixed medial centre during the step-up/down activity. Generally, knees rotated from 1° to 6° tibial internal rotation as the femur flexed from 0° to 75° flexion. The figure shows the mean position and rotation of the femoral condyles with respect to a medium-size tibial baseplate during the step-up/down activity. (AP, anteroposterior)
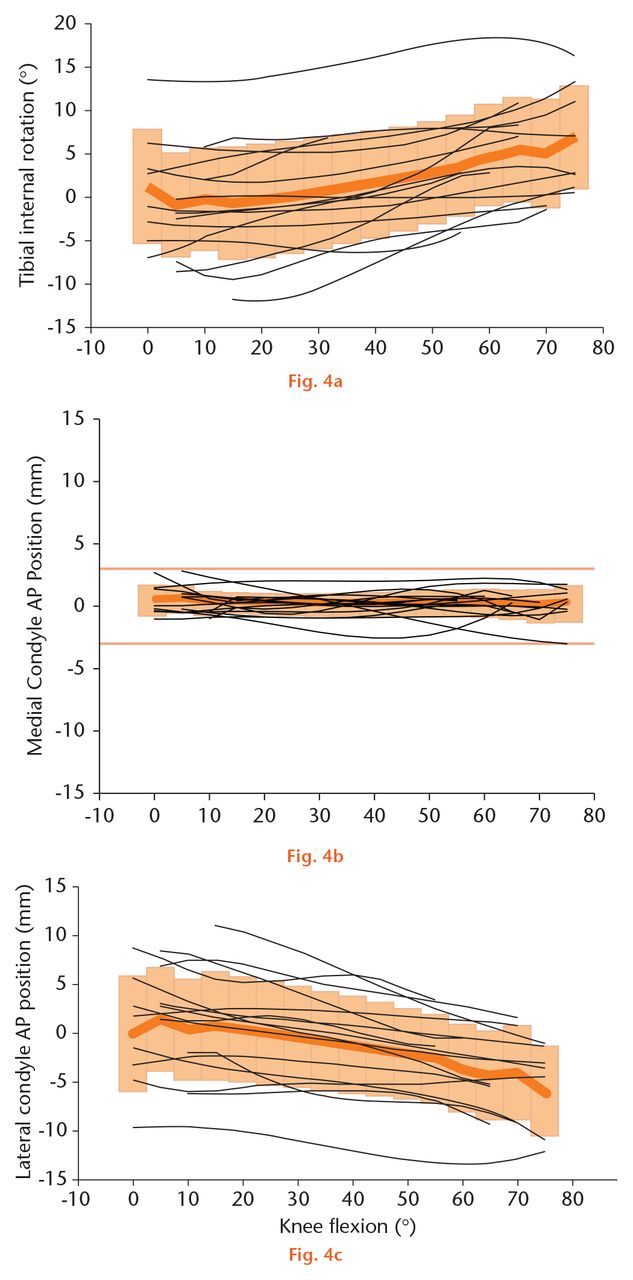
Fig.
Knee kinematics during the step-up activity were characterised by little medial condylar translation with highly individual lateral condylar translation and tibial rotation. (a) Tibial internal rotation generally increased with flexion but this was highly individual. (b) There was very little medial condylar translation. (c) There was a mean 5 mm posterior translation of the lateral condyle but again it was highly individual. The thick orange line represents the mean for the group, and the shaded orange area represents one standard deviation. The thin black lines represent the individual data for each knee. (AP, anteroposterior)
During pivoting activity, a mean 11° (3 to 20) tibial rotation was observed (Fig. 5). The patients performed the pivoting activity at a mean 1° knee flexion (-13 to +14). Only a weak linear initial relationship was found between knee flexion and the amount of tibial rotation (R2 = 0.13). The medial condyle remained within 2 mm of the centre of the tibial insert concavity, while the lateral condyle translated in a direct linear relationship to the amount of tibial longitudinal rotation (R2 = 0.98, Fig. 6).
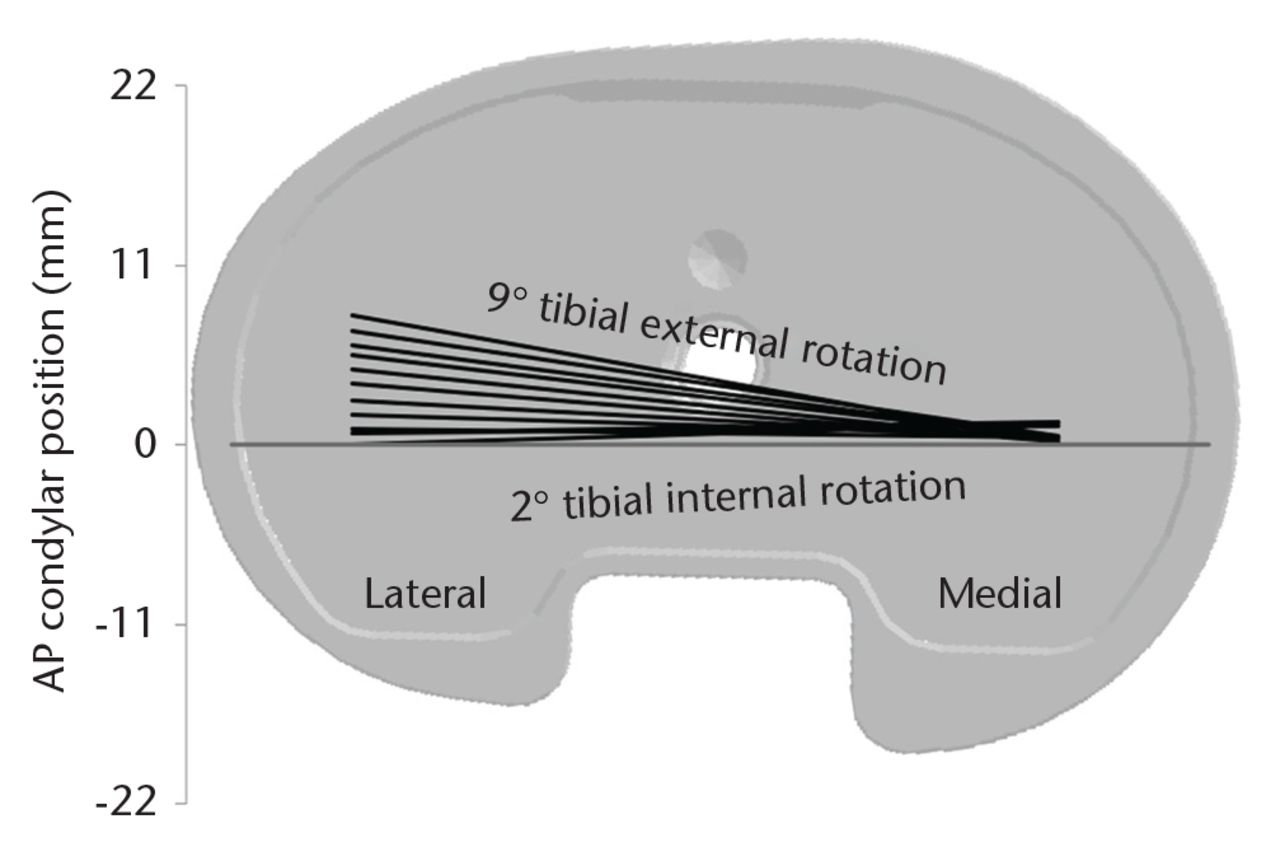
Fig. 5
Femoral translations during pivoting activity show predominantly lateral condylar movement about a stationary medial condyle. This diagram superimposes mean locations of the lowest condylar points onto a medium-size baseplate (AP, anteroposterior).
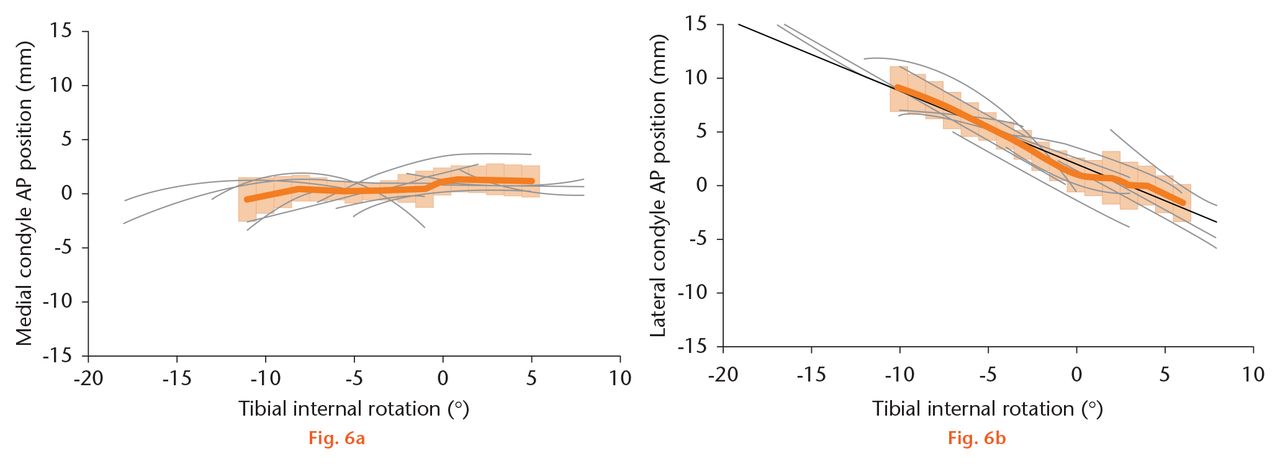
Fig.
During pivoting activity, there was little medial condylar translation (a) and lateral condylar translation (b) was linearly related to tibial rotation (R2 = 0.98). The thick orange line shows the group mean, the shaded orange area represents one standard deviation, and the thin grey lines are data for individual knees. Positive values in each graph represent an anterior translation with negative values showing a posterior position (AP, anteroposterior).
Discussion
The GMK Sphere prosthesis seeks to replicate in replaced knees the kinematics of healthy knees as reported by Freeman and Pinskerova.6 This design incorporates a spherical medial tibiofemoral articulation to provide joint stability over the 0° to 100° flexion arc, and a sagittally flat lateral and coronally partially conforming tibial articulation to permit longitudinal rotation. A total of 16 knees in 15 patients with this prosthesis were studied using fluoroscopy during a variety of active and passive tasks to determine the degree to which their knee motions reproduced those observed in natural knees. In general, there was little translation observed at the medial tibiofemoral articulation, and lateral tibiofemoral translation was closely related to the longitudinal rotation. Over a range of activities, therefore, the prosthesis was observed to move in a manner consistent with the pattern first observed by Iwaki et al in Prague.11
Lunging and kneeling activities were captured as static snapshots of the implanted knee when in semi weight-bearing maximum flexion, not as continuous motion from extension to flexion. Compared with the mean knee pose near extension, where the rotations and translations were close to 0° and 0 mm, the lunging activity in implanted knees showed a mean of 8° tibial internal rotation, 2 mm medial posterior translation and 8 mm posterior translation of the lateral condyle. Similarly, the kneeling activity showed a mean 8° tibial internal rotation, 1 mm anterior medial condylar translation and 6 mm posterior translation laterally. Moro-oka et al24 observed similar activities in healthy knees and found a mean of 11° tibial internal rotation at 114° flexion. Iwaki et al11 found a mean of 8.5° absolute tibial rotation at 115° flexion, but a total of 17° tibial internal rotation, 2 mm posterior medial and 16 mm posterior lateral condylar translations from 5° to 115° flexion. These comparisons suggest that movements in the implanted knees follow similar patterns to the normal knee but show less total tibial rotation in deeply flexed postures than in healthy intact knees.
The extent of the longitudinal rotation observed in the implanted knees resembles that reported with other arthroplasty designs studied in a similar manner,25-27 but in the GMK Sphere rotation occurs around a medial axis. The medial femoral translations, although small in magnitude, demonstrate the balance between the forces acting on the joint and the increase in relative medial tibiofemoral AP laxity at higher flexion angles, caused by the reduced posterior femoral radius. This may allow the medial femoral condyle to rise with respect to the concave tibial surface and in turn allow the femur to move in the AP direction.
During stair activity, implanted knees underwent a mean of 6° tibial internal rotation, 0.3 mm posterior translation medially and 5.9 mm posterior femoral translation laterally from 0° to 75° flexion. For the same range of flexion with cadaver specimens, Iwaki et al11 reported a mean 8.6° tibial internal rotation, 1.3 mm medial condylar posterior translation, and 8.3 mm lateral condylar posterior translation (these numbers were obtained by digitising Fig. 6a from Iwaki et al6 and fitting fourth order polynomials to the data which, in all cases, resulted in R2 > 0.97 data models). The dynamics of in vivo stair climbing and passive knee movements in cadavers are certainly different, but it appears that knee kinematics in patients with GMK Sphere implants and in the specimens reported by Iwaki et al11 share similar directions and magnitudes of tibiofemoral motion over this arc of flexion.
The pivoting activity was performed to gain a sense of the longitudinal rotation laxity with the knee near extension, which is relevant to the terminal stance phase of walking and to achieving activities of daily living. Blankevoort et al28 reported that the intact knee has ‘tibial rotatory laxity’ of approximately 15° in full extension. The implanted knees showed a mean range of tibial longitudinal rotation of 11° at 1° flexion during the pivoting activity. This rotation, as shown in Figure 5, resulted from AP movement of the lateral compartment. There was little measurable AP movement of the medial condyle during the pivoting activity, except when the tibia was forced to rotate internally and a small medial anterior femoral translation was observed in several knees.
In the patients in our study there was considerable individual variation in the extent of the tibial internal rotation with each activity. This may account for the low correlations found between the maximum flexion angle and the amount of tibial internal rotation and lateral condylar translation. In fluoroscopic studies of natural knees, the same pattern of tibial internal rotation with flexion has been found, with similar variability between subjects.24,29 In addition, these movements have been demonstrated in natural knees with medial compartment osteoarthritis where the magnitude of the tibial internal rotation is reduced but the same pattern and variation in extent of rotation has been reported.30
Two femoral movements observed in the natural knee were absent in the replaced joints. First, between 30° and 0° flexion in the natural knee, the medial tibiofemoral contact area moves forwards (but the condyle does not) and the flexion facet lifts upwards away from the tibia posteriorly.31 As the medial tibiofemoral articulation in the replaced knees is a sphere-in-sphere joint (but the natural knee is not) from 0°to 100° flexion, movement of the contact area cannot occur in the same manner. Second, beyond 120° flexion the medial femoral condyle moves progressively backwards with flexion32 and moves proximally by rolling up onto the posterior medial meniscal horn while lifting away from the tibia anteriorly.30,32 In seven replaced knees of the current study, more than 120° flexion was observed and these knees showed mean medial femoral condyle translations of 1 mm posteriorly for lunging and 2 mm anteriorly for kneeling. Posterior and proximal medial condyle translations in lunging and kneeling were absent in the replaced knees that flexed beyond 120°. This absence might be due to the prosthetic femoral condyle being more nearly spherical (with the intention of reducing wear) than found in the natural knee, or possibly because periarticular scarring limited flexion so that the replaced joints did not flex sufficiently to enter the deep flexion arc. Whatever the cause, these findings appear to confirm a prediction made by Pinskerova et al31 in 2004:
“… while it may be possible to design a total knee replacement implant which could replicate the movement of the condyles or the contact areas, to replicate both, i.e., to produce normality, is probably impossible”.
We acknowledge that there are limitations in the current study. Firstly, a relatively small number of patients was studied, all of whom had good clinical and functional outcomes. Therefore, the results may not be applicable to all patients receiving this prosthesis. Nevertheless, the GMK Sphere appears to be a highly stable articulation, similar to previously published medially spherical designs,10,18 and so key findings should be consistent across most patients. Secondly, relatively few activities were observed. However, these activities have been assessed in previous studies18,24,33-37 and, therefore, offer a basis to compare the kinematics of the GMK Sphere with those of other designs. We also accept that each patient has been examined only once. While repeated examination might have been desirable to see if any temporal changes emerged, such action is precluded by the requirement to restrict the patient’s exposure to ionising radiation. Nevertheless, our patients ranged from six to 19 months following surgery at the time of their examination. A final shortcoming is the use of single-plane imaging. While biplanar fluoroscopy is more accurate, single-plane is demonstrably adequate for quantifying tibial rotations and AP translations of the condyles, and has the advantage of providing a relatively larger field of view and the potential for lower exposure to radiation.37
We conclude that the GMK Sphere prosthesis functions in vivo in a manner similar to the natural knee as reported from Freeman and Pinskerova,6 and thus it behaves consistently with the goals of the design. The observed motions were similar in pattern, and frequently in magnitude, to those previously reported in normal knees.6 None of the knees demonstrated paradoxical forward sliding of the femur during deep flexion or pivoting activities. The GMK Sphere appeared to tolerate the individual variability between patients in the motions examined without loss of the overall objectives of the design which may be a clinical advantage. The provision of stable and consistent knee kinematics is the first requirement for long-term clinical success. Further studies will determine outcomes with respect to implant survival and patient function.
Funding Statement
Medacta International provided funding for the conduct of this study.
Professor Banks reports funding received from DJO Surgical, Lima, Exactech and Stryker/MAKO Surgical, none of which is related to this article.
Professor Field reports funding received from Medacta, ORUK, Smith & Nephew, Corin and JRI, none of which is related to this article.
L. Kanouse, K. Steiner and E. Isaac made important contributions in generating study data. Additionally, we would like to acknowledge the efforts of J. Buly, J. Curtis, J. Hisole, C. Pearce, J. Stammers, A. Hartfield and J. Gray for their efforts in carrying out this study. All authors read and approved the final manuscript.
ICMJE conflict of interest
None declared.
References
1. Zuppinger H . Die aktive Flexion im unbelasteten Kniegelenk. Zuricher Habil Schr, Wisebaden: Bergmann, 1904:703-763.[[bibmisc]] Google Scholar
2. Fick R . Mechanik des kniegelenkes. In: von BardelebenK. Hanbuch der Anatomie des Menschenhrsg hrsg. Band 2, 1, Vol. 3: Jena: Gustv Fischer, 1911:521.[[bibmisc]] Google Scholar
3. Strasser H . Lebrbuch del Muskel- und Gelenkmechanik. III Band: Die untere Extemitárt. Berlin: Springer-Verlag, 1917.[[bibmisc]] Google Scholar
4. Kapandji IA . The mechanical role of the cruciate ligaments. In: The physiology of the joints. Vol 2. 2nd ed.Paris: Maloine SA, 1970:120.[[bibmisc]] Google Scholar
5. Brantigan OC , VoshellAF. The mechanics of the ligaments and menisci of the knee joint. J Bone Joint Surg [Am]1941;23-A:44-66. Google Scholar
6. Freeman MA , PinskerovaV. The movement of the normal tibio-femoral joint. J Biomech2005;38:197-208.CrossrefPubMed Google Scholar
7. McPherson A , KärrholmJ, PinskerovaV, SosnaA, MartelliS. Imaging knee position using MRI, RSA/CT and 3D digitisation. J Biomech2005;38:263-268.CrossrefPubMed Google Scholar
8. Williams A , LoganM. Understanding tibio-femoral motion. Knee2004;11:81-88.CrossrefPubMed Google Scholar
9. Johal P , WilliamsA, WraggP, HuntD, GedroycW. Tibio-femoral movement in the living knee. A study of weight bearing and non-weight bearing knee kinematics using ‘interventional’ MRI. J Biomech2005;38:269-276. Google Scholar
10. Shimmin A , Martinez-MartosS, OwensJ, IorgulescuAD, BanksS. Fluoroscopic motion study confirming the stability of a medial pivot design total knee arthroplasty. Knee2015;22:522-526.CrossrefPubMed Google Scholar
11. Iwaki H , PinskerovaV, FreemanMAR. Tibiofemoral movement 1: the shapes and relative movements of the femur and tibia in the unloaded cadaver knee. J Bone Joint Surg [Br]2000;82-B:1189-1195.CrossrefPubMed Google Scholar
12. Insall JN , DorrLD, ScottRD, ScottWN. Rationale of the Knee Society clinical rating system. Clin Orthop Relat Res1989;248:13-14.PubMed Google Scholar
13. Dawson J , FitzpatrickR, MurrayD, CarrA. Questionnaire on the perceptions of patients about total knee replacement. J Bone Joint Surg [Br]1998;80-B:63-69.CrossrefPubMed Google Scholar
14. Murray DW , FitzpatrickR, RogersK, et al.. The use of the Oxford hip and knee scores. J Bone Joint Surg [Br]2007;89-B:1010-1014. Google Scholar
15. Ries MD . Effect of ACL sacrifice, retention, or substitution on kinematics after TKA. Orthopedics2007;30:74-76.PubMed Google Scholar
16. Moro-oka TA , MuenchingerM, CancianiJP, BanksSA. Comparing in vivo kinematics of anterior cruciate-retaining and posterior cruciate-retaining total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc2007;15:93-99.CrossrefPubMed Google Scholar
17. Moonot P , MuS, RailtonGT, FieldRE, BanksSA. Tibiofemoral kinematic analysis of knee flexion for a medial pivot knee. Knee Surg Sports Traumatol Arthrosc2009;17:927-934.CrossrefPubMed Google Scholar
18. Moonot P , ShangM, RailtonGT, FieldRE, BanksSA. In vivo weight-bearing kinematics with medial rotation knee arthroplasty. Knee2010;17:33-37.CrossrefPubMed Google Scholar
19. Banks S , BellemansJ, NozakiH, et al.. Knee motions during maximum flexion in fixed and mobile-bearing arthroplasties. Clin Orthop Relat Res2003;410:131-138.CrossrefPubMed Google Scholar
20. Banks SA , HodgeWA. Accurate measurement of three-dimensional knee replacement kinematics using single-plane fluoroscopy. IEEE Trans Biomed Eng1996;43:638-649.CrossrefPubMed Google Scholar
21. Canny J . A computational approach to edge detection. IEEE Trans Pattern Anal Mach Intell1986;8:679-698.PubMed Google Scholar
22. Tupling SJ , PierrynowskiMR. Use of cardan angles to locate rigid bodies in three-dimensional space. Med Biol Eng Comput1987;25:527-532.CrossrefPubMed Google Scholar
23. Stiehl JB , KomistekRD, DennisDA, PaxsonRD, HoffWA. Fluoroscopic analysis of kinematics after posterior-cruciate-retaining knee arthroplasty. J Bone Joint Surg [Br]1995;77-B:884-889.PubMed Google Scholar
24. Moro-oka TA , HamaiS, MiuraH, et al.. Dynamic activity dependence of in vivo normal knee kinematics. J Orthop Res2008;26:428-434.CrossrefPubMed Google Scholar
25. Banks SA , HodgeWA. Implant design affects knee arthroplasty kinematics during stair-stepping. Clin Orthop Relat Res2004;426:187-193.CrossrefPubMed Google Scholar
26. Okamoto N , BreslauerL, HedleyAK, MizutaH, BanksSA. In vivo knee kinematics in patients with bilateral total knee arthroplasty of 2 designs. J Arthroplasty2011;26:914-918.CrossrefPubMed Google Scholar
27. Watanabe T , IshizukiM, MunetaT, BanksSA. Matched comparison of kinematics in knees with mild and severe varus deformity using fixed- and mobile-bearing total knee arthroplasty. Clin Biomech (Bristol, Avon)2012;27:924-928.CrossrefPubMed Google Scholar
28. Blankevoort L , HuiskesR, de LangeA. The envelope of passive knee joint motion. J Biomech1988;21:705-720.CrossrefPubMed Google Scholar
29. Hamai S , Moro-okaTA, DunbarNJ, et al.. In vivo healthy knee kinematics during dynamic full flexion. Biomed Res Int2013;2013:717546.CrossrefPubMed Google Scholar
30. Hamai S , Moro-okaTA, MiuraH, et al.. Knee kinematics in medial osteoarthritis during in vivo weight-bearing activities. J Orthop Res2009;27:1555-1561.CrossrefPubMed Google Scholar
31. Pinskerova V , JohalP, NakagawaS, et al.. Does the femur roll-back with flexion?J Bone Joint Surg [Br]2004;86-B:925-931.CrossrefPubMed Google Scholar
32. Pinskerova V , SamuelsonKM, StammersJ, et al.. The knee in full flexion: an anatomical study. J Bone Joint Surg [Br]2009;91-B:830-834.CrossrefPubMed Google Scholar
33. Fantozzi S , CataniF, EnsiniA, et al.. Femoral Rollback of Cruciate-Retaining and Posterior-Stabilized Total Knee Replacements: In Vivo Fluoroscopic Analysis during Activities of Daily Living. J Orthop Res2006;24:2222-2229.CrossrefPubMed Google Scholar
34. Dennis DA , MahfouzMR, KomistekRD, HoffW. In vivo determination of normal and anterior cruciate ligament-deficient knee kinematics. J Biomech2005;38:241-253.CrossrefPubMed Google Scholar
35. Kanisawa I , BanksAZ, BanksSA, MoriyaH, TsuchiyaA. Weight-bearing knee kinematics in subjects with two types of anterior cruciate ligament reconstructions. Knee Surg Sports Traumatol Arthrosc2003;11:16-22.CrossrefPubMed Google Scholar
36. Banks SA , HodgeWA. 2003 Hap Paul Award Paper of the International Society for Technology in Arthroplasty. Design and activity dependence of kinematics in fixed and mobile-bearing knee arthroplasties. J Arthroplasty2004;19:809-816.CrossrefPubMed Google Scholar
37. Acker S , LiR, MurrayH, et al.. Accuracy of single-plane fluoroscopy in determining relative position and orientation of total knee replacement components. J Biomech2011;44:784-787.CrossrefPubMed Google Scholar









