Abstract
Aims
An evidence-based radiographic Decision Aid for meniscal-bearing unicompartmental knee arthroplasty (UKA) has been developed and this study investigates its performance at an independent centre.
Patients and Methods
Pre-operative radiographs, including stress views, from a consecutive cohort of 550 knees undergoing arthroplasty (UKA or total knee arthroplasty; TKA) by a single-surgeon were assessed. Suitability for UKA was determined using the Decision Aid, with the assessor blinded to treatment received, and compared with actual treatment received, which was determined by an experienced UKA surgeon based on history, examination, radiographic assessment including stress radiographs, and intra-operative assessment in line with the recommended indications as described in the literature.
Results
The sensitivity and specificity of the Decision Aid was 92% and 88%, respectively. Excluding knees where a clear pre-operative plan was made to perform TKA, i.e. patient request, the sensitivity was 93% and specificity 96%. The false-positive rate was low (2.4%) with all affected patients readily identifiable during joint inspection at surgery.
In patients meeting Decision Aid criteria and receiving UKA, the five-year survival was 99% (95% confidence intervals (CI) 97 to 100). The false negatives (3.5%), who received UKA but did not meet the criteria, had significantly worse functional outcomes (flexion p < 0.001, American Knee Society Score - Functional p < 0.001, University of California Los Angeles score p = 0.04), and lower implant survival of 93.1% (95% CI 77.6 to 100).
Conclusion
The radiographic Decision Aid safely and reliably identifies appropriate patients for meniscal-bearing UKA and achieves good results in this population. The widespread use of the Decision Aid should improve the results of UKA.
Cite this article: Bone Joint J 2016;98-B(10 Suppl B):3–10.
Unicompartmental knee arthroplasty (UKA) provides significant benefits to patients, healthcare providers and healthcare payers.1-3 Compared with total knee arthroplasty (TKA), patients undergoing UKA recover faster, achieve better functional outcomes, have a lower morbidity and mortality and report higher patient satisfaction.1,2,4,5 Furthermore, UKA has been reported to be more cost effective than TKA in both the short- and long-term.3,6,7 One concern with UKA however is the more variable long-term implant survival, with UKA having a higher overall revision rate than TKA.1 This higher incidence of revision is multi-factorial, although it is known to be related to patient selection, surgical caseload, as well as a lower threshold for revision than with TKA.8
Despite meniscal-bearing UKA being appropriate in up to half the patients receiving treatment with knee arthroplasty, UKA is used in only 8% with large variation in usage between surgeons.9 One proposed reason for this variation is the lack of recognition of indications for UKA. The primary indication for meniscal-bearing UKA is anteromedial osteoarthritis (AMOA), with spontaneous osteonecrosis of the knee (SONK) representing another important indication.10 Patient factors including age, weight and level of activity; radiographic factors including chondrocalcinosis and lateral osteophytes; and operative factors including the presence of a chondral ulcer on the medial side of the lateral femoral condyle, have been demonstrated not to compromise outcomes and are not considered to be contra-indications.11-13 Therefore, identification of AMOA is crucial in determining suitability for meniscal-bearing UKA.
Patients are considered to have AMOA, and are therefore deemed suitable for meniscal-bearing UKA, if they meet each of the following criteria: bone-on-bone osteoarthritis (OA) in the medial compartment, retained full thickness cartilage in the lateral compartment, a functionally normal medial collateral ligament (MCL), and a functionally normal anterior cruciate ligament (ACL). In addition, they should have a patellofemoral joint (PFJ) that does not have severe damage laterally with bone loss, grooving and subluxation.13-15 These criteria are assessed radiographically and are confirmed at operation. Additionally, practical considerations, such as the ability to flex the knee to 110° under anaesthetic to prepare the femoral condyle, need to be taken into account.
The criteria for AMOA are assessed using standing anteroposterior, valgus stress (in 20º flexion), true lateral and skyline radiographs. In the majority of patients, bone-on-bone arthritis in the medial compartment is demonstrated on the standing anteroposterior radiograph. However, in a proportion of knees, typically those with smaller anteromedial lesions, additional radiographs, such as a varus stress (in 20º flexion), or a standing flexed (at 20º, otherwise known as a Rosenberg or Schuss view)16 radiograph is required. A valgus stress radiograph is required to demonstrate both that there is full thickness cartilage in the lateral compartment, and that the medial compartment opens fully, indicating that the MCL is functionally normal and not shortened. Stress radiographs should be performed with the knee in 20° flexion to relax the posterior capsule, and with the x-ray beam aligned parallel to the joint surface (which is best achieved by using a firm 6 inch triangular bolster behind the knee and tilting the x-ray tube 10º).17 The functional status of the ACL is best determined from a true lateral radiograph, taken with the knee slightly flexed and the femoral condyles overlapping, as clinical evaluation of the ACL in the setting of OA can be misleading.18,19 Where the ACL is functionally abnormal, or absent, the tibial erosion extends to the back of the tibial plateau and may be accompanied by posterior femoral subluxation. If the tibial erosion cannot be seen, or does not extend to the back of the tibia, there is a 95% chance that the ACL is functionally normal.20 The PFJ should be assessed via a skyline radiograph with the knee in 30° flexion. Only in the presence of lateral bone loss with grooving and subluxation is there a contra-indication to meniscal-bearing UKA.21
The concept of a radiographic, atlas based, patient selection tool for UKA was first suggested by Oosthuizen et al22 and stimulated by this, we have developed a radiographic Decision Aid, using the five evidence-based criteria outlined above, to improve patient selection for medial meniscal-bearing UKA. This study covers the development of the Decision Aid and investigates its sensitivity and specificity in predicting suitability for meniscal-bearing UKA in a consecutive cohort of patients undergoing knee arthroplasty (UKA or TKA) under the care of an independent surgeon (KRB) who was not involved in the development of the Decision Aid. The mid-term functional outcomes and implant survival in those knees where the Decision Aid advised meniscal-bearing UKA, and who underwent UKA were also investigated.
Materials and Methods
Development of the Decision Aid
An atlas-based radiographic Decision Aid, based on the five criteria that are required to be met to perform medial meniscal-bearing UKA for AMOA has been developed. The Decision Aid is divided into five sections, each assessing one of the five criteria, with radiographic view and exemplar radiographs provided that demonstrate when the criteria are met, as well as exemplar radiographs that demonstrate when the criteria are not met. Example radiographs of knees meeting the criteria to perform UKA were taken from a previously reported series23 of meniscal-bearing UKA, in which the long-term functional outcomes and implant survival are known. Examples of knees not meeting the criteria are taken from a series of patients undergoing TKA during the same time period. Illustrative radiographs for each criterion were selected by consensus by the Decision Aid development team (TWH, HGP, DWM). Each criterion is assessed by way of a binary, yes-no, polar question with all criteria required to be met to perform meniscal-bearing UKA for an indication of AMOA.
Validation of the Decision Aid in an independent population
Between 01 January 2008 and 31 December 2008, 550 consecutive primary TKA or primary medial meniscal-bearing UKA were performed by an experienced UKA surgeon (KRB) at an independent centre not involved with the development of the Decision Aid. All patients signed an institutional review board approved general research consent allowing for retrospective review. The benchmark with which the Decision Aid was compared was actual treatment received, which was determined by an experienced UKA surgeon (KRB) based on history, examination, radiographic assessment including stress radiographs, and intra-operative assessment in line with the recommended indications as described by Goodfellow et al.14
Suitability for meniscal-bearing UKA was determined by assessing pre-operative radiographs using the radiographic Decision Aid with the assessor (TWH) blinded to the treatment received. A total of 12% of radiographs (n = 227 of 1962 radiographs) were re-assessed at three months by the primary assessor and also by an independent assessor (AC).
Patients were followed-up independently using a standard protocol. Functional outcomes were assessed using the American Knee Society Objective Score (AKSS-O), Functional Score (AKSS-F),24 Lower Extremity Activity Scale (LEAS)25 and the University of California, Los Angeles (UCLA) activity score.26 Where patients had died, information about the status of their knee, and the presence of any further operation was obtained via primary and secondary care records as well as via patient’s relatives where appropriate.
Performance of the Decision Aid was assessed by calculating the sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV) and accuracy at identifying suitability for UKA. Performance was calculated based on radiographic assessment alone, and radiographic assessment combined with results of pre-operative findings from patient history, examination, prior clinical investigations and surgeon assessment. Patient history factors assessed included patient preference for implant type (i.e. successful contralateral arthroplasty) and history of inflammatory arthritis (UKA contraindicated). Patient examination factors included expected flexion < 110° which is required to prepare the femur at the time of operation. Prior clinical investigations included the results of a direct assessment of the joint at arthroscopy, as well as MRI demonstrating SONK. Other findings from MRI, including the status of the tibiofemoral joint and ACL, were not taken into account as these have not been demonstrated to affect patient outcomes and should not be used for patient selection.27 Surgeon assessment included cases where the patient may have been suitable for UKA however a pre-operative decision was made by the surgeon to proceed with TKA.
Statistical analysis
To assess for differences in functional outcome between subgroups, non-parametric tests (Mann-Whitney U) were performed. A life-table analysis was performed to assess survival using implant-related re-operations, which included any re-operations in which components were changed, of which the bearing was replaced for dislocation, and any re-operations in which new components were inserted as the end point. Confidence intervals (CI) were calculated using the method described by Peto et al.28 A p-value < 0.05 was considered to be statistically significant.
Results
Of the 540 knees (356 patients) in which radiographs were available, 239 (44%) underwent medial meniscal-bearing Oxford Phase 3 UKA (Zimmer Biomet, Warsaw, Indiana) and 301 (56%) underwent TKA. Complete sets of radiographs were not available in 83 knees (29 UKA, 54 TKA) which included two cases of SONK, leaving 457 knees for assessment against Decision Aid criteria (Fig. 1, Table I).
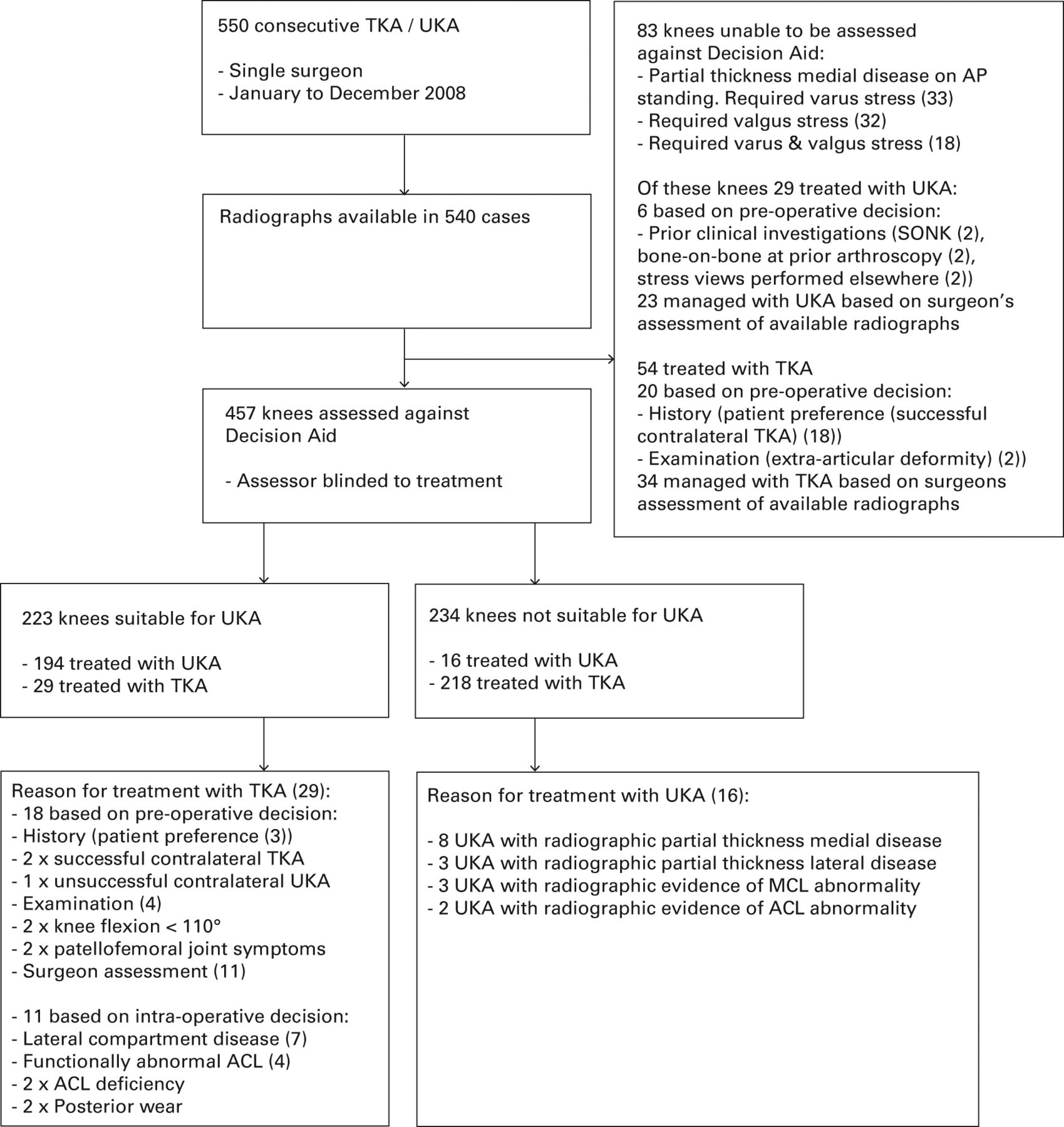
Fig. 1
Flowchart of study patients (UKA, unicompartmental knee arthroplasty; TKA, total knee arthroplasty; AP, anteroposterior; SONK, spontaneous osteonecrosis of the knee; MCL, medial collateral ligament; ACL, anterior cruciate ligament).
Table I
Demographic details on knees undergoing surgery
| UKA mean (sd) (n = 239) | TKA mean (sd) (n = 301) | p-value | |
|---|---|---|---|
| Time from surgery (yrs) | 6.7 (0.4) | 6.7 (0.5) | 0.23 |
| Follow-up (yrs) | 3.9 (1.8) | 2.8 (2.4) | < 0.001 |
| Age (yrs) | 63.2 (10.3) | 65.8 (10.2) | 0.01 |
| % male | 41.0 | 40.2 | 0.85* |
| Body mass index | 31.9 (7.3) | 33.3 (7.6) | 0.02 |
-
* chi-squared test UKA, unicompartmental knee arthroplasty; TKA, total knee arthroplasty; sd, standard deviation
Based on the radiographic Decision Aid 49% (223) of knees were deemed suitable for medial meniscal-bearing UKA and 51% (234) were not suitable. There was excellent intra- (Cohen’s kappa 0.90) and inter-observer (Cohen’s kappa 0.85) agreement.
Of those 234 knees identified as not suitable for UKA, 40% (93 knees) did not meet one radiographic criteria, 38% (88 knees) did not meet two criteria, 22% (52 knees) did not meet three criteria and < 1% (one knee) did not meet four criteria. Of those knees that did not meet radiographic criteria, 46% (108 knees) had preserved medial compartment cartilage, 45% (105 knees) had posterior bone loss on their true lateral radiograph indicating ACL insufficiency, 67% (157 knees) had evidence of lateral compartment disease, 11% (25 knees) had evidence of MCL shortening and 16% (37 knees) evidence of bone loss with grooving to the lateral PFJ.
The functional outcomes of knees treated with UKA are outlined in Table II. In the 194 knees meeting Decision Aid criteria for UKA, who received UKA, there were four implant related re-operations (four patients) at a mean of 3.8 years (0.9 to 6.4). There was one case of instability (0.9 years), one case of lateral compartment progression of arthritis (6.1 years), one case of femoral loosening associated with ACL deficiency (6.4 years) and one case due to an unknown cause with the revision operation performed elsewhere (2.0 years). The five-year survival in this cohort was 98.9% (95% CI 96.6 to 100) (Table III).
Table II
Functional outcomes in those undergoing unicompartmental knee arthroplasty (UKA) (Mann-Whitney U test)
| Decision Aid appropriate for UKA mean (sd) | Decision Aid not appropriate for UKA mean (sd) | p-value | |
|---|---|---|---|
| Flexion | |||
| Pre-operative | 115.8 (8.8) | 109.2 (11.9) | < 0.001 |
| Post-operative | 117.8 (7.8) | 112.0 (11.4) | < 0.001 |
| Change | 2.1 (10.6) | 2.7 (12.7) | 0.65 |
| Knee Society Objective Score | |||
| Pre-operative | 38.6 (13.9) | 40.4 (18.9) | 0.69 |
| Post-operative (most recent) | 87.7 (16.2) | 90.2 (13.6) | 0.63 |
| Change | 49.1 (21.4) | 49.1 (22.7) | 0.98 |
| Knee Society Functional Score | |||
| Pre-operative | 57.5 (15.5) | 51.7 (18.9) | 0.001 |
| Post-operative (most recent) | 72.9 (22.7) | 64.2 (25.1) | < 0.001 |
| Change | 15.3 (22.9) | 12.2 (24.9) | 0.12 |
| Lower Extremity Activity Score | |||
| Pre-operative | 9.5 (2.8) | 9.1 (2.9) | 0.09 |
| Post-operative (most recent) | 9.9 (2.9) | 9.7 (3.0) | 0.44 |
| Change | -8.1 (3.8) | -7.7 (3.7) | 0.32 |
| University of California, Los Angeles Score | |||
| Post-operative (most recent) | 6.2 (2.5) | 5.3 (1.9) | 0.04 |
-
sd, standard deviation
Table III
Life table analysis with 95% confidence intervals (CI) when Decision Aid was appropriate for unicompartmental knee arthroplasty (UKA) and UKA was performed
| Follow-up (yrs) | Number at start | Revised | Withdrawn | At risk | Annual failure | Survival | 95% CI | 95% CI |
|---|---|---|---|---|---|---|---|---|
| 0 to 1 | 194 | 0 | 7 | 190.5 | 0.000 | 100 | 100 | 100 |
| 1 to 2 | 187 | 1 | 7 | 183.5 | 0.005 | 99.5 | 98.4 | 100 |
| 2 to 3 | 179 | 1 | 25 | 166.5 | 0.006 | 98.9 | 97.2 | 100 |
| 3 to 4 | 153 | 0 | 57 | 124.5 | 0.000 | 98.9 | 97.0 | 100 |
| 4 to 5 | 96 | 0 | 19 | 86.5 | 0.000 | 98.9 | 96.6 | 100 |
In 29 knees, the Decision Aid indicated suitability for meniscal-bearing UKA, however, TKA was performed (18 pre-operative decision, 11 intra-operative decision) (Fig. 1). Knees that were identified by the Decision Aid as suitable for UKA but underwent TKA had significantly worse post-operative flexion (110°, standard deviation (sd) 11° versus 118°, sd 8°; p < 0.001) and Knee Society Functional Scores (63.2, sd 20 vs 72.9, sd 23; p = 0.04) compared with knees managed with UKA who were identified as suitable. No other differences in functional scores were seen between these groups and no difference in functional outcome was detected between those knees identified as suitable for UKA that underwent TKA, and those identified as not suitable for UKA who were treated with TKA (Table IV).
Table IV
Functional outcomes in those undergoing total knee arthroplasty (TKA) (Mann-Whitney U test)
| Decision Aid not appropriate for UKA received TKA mean (sd) | Decision Aid appropriate for UKA received TKA mean (sd) | p-value | |
|---|---|---|---|
| Flexion | |||
| Pre-operative | 109.2 (11.9) | 110.9 (11.8) | 0.49 |
| Post-operative | 112.0 (11.4) | 110.2 (10.8) | 0.43 |
| Change | 2.7 (12.7) | -1.1 (15.4) | 0.18 |
| Knee Society Objective Score | |||
| Pre-operative | 10.4 (18.9) | 34.7 (10.9) | 0.17 |
| Post-operative (most recent) | 90.2 (13.6) | 90.9 (12.9) | 0.91 |
| Change | 49.1 (22.7) | 55.7 (17.4) | 0.17 |
| Knee Society Functional Score | |||
| Pre-operative | 51.7 (18.9) | 56.0 (15.9) | 0.24 |
| Post-operative (most recent) | 64.2 (25.4) | 63.2 (20.4) | 0.89 |
| Change | 12.2 (24.9) | 4.8 (16.5) | 0.45 |
| Lower Extremity Activity Score | |||
| Pre-operative | 9.1 (2.9) | 9.0 (2.4) | 0.80 |
| Post-operative (most recent) | 9.7 (3.0) | 9.9 (1.9) | 0.49 |
| Change | -7.7 (3.7) | -6.9 (2.9) | 0.40 |
| University of California, Los Angeles Score | |||
| Post-operative (most recent) | 5.3 (1.9) | 5.6 (1.1) | 0.57 |
-
UKA, unicompartmental knee arthroplasty
There were no cases of failure in this group at a mean follow-up of 3.2 years (0 to 7) or in those knees (218 knees) not meeting Decision Aid criteria for UKA who were treated with TKA at a mean follow-up of 2.9 years (0 to 7).
In the 16 knees that did not meet Decision Aid criteria for meniscal-bearing UKA but received UKA, (Fig. 1) at a mean follow-up of 4.3 years (1 to 6) significantly lower flexion, AKSS-F and UCLA scores were obtained compared with those knees identified as suitable for UKA and were treated with UKA (Table II). However, they also had lower pre-operative functional scores, and no difference in improvement from baseline was observed. In this group there was one case of failure, progression of arthritis in the lateral compartment, at 2.3 years. The five-year survival (93.1%; 95% CI 77.6 to 100) in knees not suitable for UKA that underwent UKA was lower than those identified as suitable for UKA treated with UKA, however due to small numbers it was not possible to assess the significance of this difference.
The performance of the Decision Aid is outlined in Table V. A sensitivity analysis, performed to assess the role of skyline and stress radiographs in the evaluation for meniscal-bearing UKA, demonstrated a decrease in accuracy of 1% and 5%, respectively if these radiographs were not performed (Table VI).
Table V
Performance of the Decision Aid in predicting suitability for unicompartmental knee arthroplasty (UKA)
| Sensitivity (%) | Specificity (%) | Positive predictive value (%) | Negative predictive value (%) | Accuracy (%) | |
|---|---|---|---|---|---|
| Radiology alone | 92 | 88 | 87 | 93 | 90 |
| Radiology plus history | 92 | 89 | 88 | 93 | 91 |
| Radiology plus examination | 92 | 90 | 89 | 93 | 91 |
| Radiology plus surgeon assessment | 92 | 93 | 92 | 93 | 93 |
| Radiology plus results of prior investigations | 93 | 88 | 87 | 93 | 90 |
| Radiology plus all of above | 93 | 96 | 95 | 94 | 94 |
-
History: patient preference for implant type (i.e., successful contralateral replacement) Examination: clinical finding influencing implant selection (i.e., predicted flexion < 110° under anaesthetic, required to perform UKA) Surgeon assessment: pre-operative decision made by the surgeon to proceed with total knee arthroplasty based on patient assessment Prior investigations: prior arthroscopy demonstrating indication or MRI demonstrating spontaneous osteonecrosis of the knee
Table VI
Sensitivity analysis – skyline and stress radiographs
| Sensitivity (%) | Specificity (%) | Positive predictive value (%) | Negative predictive value (%) | Accuracy (%) | |
|---|---|---|---|---|---|
| All radiographic and clinical findings | 93 | 96 | 95 | 94 | 94 |
| Radiographic and clinical findings - no skyline radiograph | 93 | 94 | 93 | 94 | 93 |
| Radiographic and clinical findings - no stress radiograph | 88 | 90 | 90 | 89 | 89 |
Discussion
This study, which was undertaken in a cohort of patients operated on by a surgeon who was not involved with the development of the Decision Aid (KRB), found the sensitivity and specificity of the radiographic Decision Aid at predicting suitability for meniscal-bearing UKA to be 92% and 88%, respectively. When the radiographic findings were combined with pre-operative factors that influence implant selection (i.e. patient request for TKA or flexion so limited that is was impossible to implant a UKA), the sensitivity and specificity increased to 93% and 96%, respectively. In those patients who met Decision Aid criteria for UKA and in whom UKA was performed excellent survival, 99% at five years (95% CI 96.6 to 100), and functional outcomes were achieved. Taken together this suggests that the Decision Aid is a useful tool for identifying appropriate patients for UKA in those who meet the criteria for joint arthroplasty.
The main concern about the Decision Aid is that there were a few false positives (2.4%) where the Decision Aid suggested a UKA should be done yet the surgeon did not perform a UKA. As a UKA was not undertaken, we cannot know what the outcome would have been had one been implanted, and therefore, have to assume that it might not have been good. Importantly, in all of these false positives the contraindication to UKA, such as a ruptured ACL, was readily identifiable during routine examination of the joint at the time of surgery. As inspection of the knee at the time of surgery is part of the surgical routine, with this stated to be necessary on the Decision Aid, we believe that it is safe to recommend the Decision Aid as the primary assessment for patient suitability for UKA. The only proviso being that the patient must be asked for consent for the possibility of a TKA, with TKA instrumentation being available should this be required.
In 3.5% of cases (16 knees) the Decision Aid did not support the use of a UKA, yet one was implanted. In these false negatives, although the clinical outcomes were satisfactory, the patients had significantly worse functional outcomes (flexion p < 0.001, AKSS-F p < 0.001, UCLA p = 0.04), and a lower implant survival 93.1% (95% CI 77.6 to 100) compared with those who had a UKA that was supported by the Decision Aid. This would suggest that the Decision Aid does identify the optimal patients for UKA, and that surgeons should be cautions when extending the indications beyond those recommended by the Decision Aid. The most common reason why the Decision Aid did not support a UKA that was implanted was that there was only partial thickness cartilage loss in the medial compartment and not bone-on-bone, as this subgroup of patients has previously been shown to have unpredictable results in independent studies.29,30
Sensitivity analysis, investigating the role of skyline and stress radiographs, highlighted the importance of performing stress radiographs when identifying suitability for meniscal-bearing UKA. In this series, if stress radiographs were not performed, the accuracy of the Decision Aid would be reduced by 5% (Table VI). In the absence of stress radiographs, 10% of knees would be inappropriately identified as suitable for meniscal-bearing UKA (PPV) as lateral compartment disease, demonstrated on valgus stress, would be missed. In addition, 11% of knees would be inappropriately identified as not suitable for meniscal-bearing UKA (NPV) due to medial bone-on-bone arthritis, demonstrated on varus stress, not being seen on standing anteroposterior radiographs. This highlights the importance of performing stress radiographs in the assessment of suitability for UKA, particularly as during visual intra-operative examination, it is often impossible to assess the cartilage thickness in the lateral compartment.
The sensitivity analysis demonstrated that not performing skyline radiographs only resulted in a 1% reduction in the accuracy of the Decision Aid. This finding, combined with the fact that bone loss and grooving in the lateral part of the PFJ is readily identified at the time of operation, suggests that skyline radiographs could be omitted as they do not significantly influence patient selection. Furthermore, in the past skyline radiographs were not recommended. The reason why skyline radiographs, and to certain extent stress radiographs, have been included in the Decision Aid is different. The majority of surgeons currently restrict usage of UKA to cases where the lateral compartment and PFJ are virtually pristine, in order to avoid disease progression. This is incorrect, as providing the valgus stress radiograph shows full thickness cartilage laterally, and there is not severe arthritis in the lateral part of the PFJ seen on the skyline radiograph, this study demonstrates that excellent outcomes can be achieved. Indeed full thickness ulceration is commonly seen on the medial side of the lateral femoral condyle, as well as in the PFJ, and these factors have previously been demonstrated not to compromise outcomes.12,15,21 If surgeons use the Decision Aid then they can complete an evidence-based document to determine whether a UKA is indicated. Furthermore, they can keep the document in the patient’s record; thus, if their decision to perform a UKA is ever questioned, they will have evidence to show that it was correct.
The recommended indications for meniscal-bearing UKA are satisfied in about half of knees needing knee arthroplasty. In this study, which excluded lateral UKA, it was used and was supported by the Decision Aid in 42% of cases and very good results were achieved. There are also multiple published or presented series from surgeons who use UKA for about half of their knee arthroplasties in which the Oxford Phase 3 UKA has achieved a ten-year survival of around 95%.23,31-33 Analysis of data from the National Joint Registry of England and Wales demonstrates that surgeons undertaking the Oxford UKA in less than 20% of knee arthroplasties, and in particular less than 10%, have a high revision rate, partly because the number is small, and partly because they are using the wrong indications.1 At 20% and above the revision rate is acceptable, however, best results are achieved when surgeons undertake the Oxford UKA in about half of knee arthroplasties. Under these optimal circumstances the rate of re-operation of UKA is similar to that of TKA.1 The use of the Decision Aid would ensure that surgeons use the recommended indications, and therefore achieve optimal results. Under these circumstances the patients will have all the advantages of UKA, including a faster recovery, lower morbidity and mortality compared with TKA, without the higher re-operation rate.
Importantly, this radiological Decision Aid can be implemented at all hospitals as it does not require specialist equipment or imaging modalities and enables surgeons to develop a patient management plan during a single clinic appointment. As it is simple it could not only be used by surgeons, but also referring physicians. Alternative techniques such as MRI have been proposed to assess suitability for UKA, however, they add additional time and cost, and the clinical relevance of these findings with respect to patient selection is yet to be clarified. Furthermore, Hurst et al27 have demonstrated no difference in clinical outcomes following UKA in knees with MRI contra-indications to UKA compared with those without questioning the clinical relevance of MRI findings.
There are certain limitations to this study. This study retrospectively analyses the mid-term outcome of patients treated by a single experienced UKA surgeon with longer-term data yet to be available. In the absence of a benchmark for patient selection for UKA a single experienced UKA surgeon series was chosen such that use of UKA was high and that UKA was being used in all appropriate cases in line with the current evidence. However, it is acknowledged that there may be variation even amongst experienced UKA surgeons in terms of their patient selection, and that the results seen in this high volume user series may not be generally applicable. Additionally, the association between high use of UKA and improved outcomes in patients undergoing this procedure has not been established to be causative. Whilst there is uncertainty as to whether increasing use will result in improved outcomes, optimising patient selection by ensuring that patients meet the indications of Goodfellow et al14 would be expected to improve outcomes as the long-term results seen in published series that have adhered to these recommendations, have reported similarly good outcomes to those seen in this series.31,33,34 Further work is required to establish the effect of introducing the radiological Decision Aid into general use to assess the true impact of this decision tool.
The radiological Decision Aid has a high sensitivity and specificity for predicting suitability for meniscal-bearing UKA and demonstrates that meniscal-bearing UKA can be used in around half of knees with excellent implant survival and functional outcomes. The Decision Aid is safe as, providing surgeons examine the knee at surgery, no patient should have an inappropriate UKA. The use of the radiological Decision Aid should optimise patient selection, which will minimise the revision rate of UKA and will allow more patients to benefit from UKA.
Take home message: The use of the radiological Decision Aid optimises patient selection for meniscal-bearing UKA which in turn should minimise the revision rate and improve results allowing more patients to benefit from this procedure.
1 Liddle AD , JudgeA, PanditH, MurrayDW. Adverse outcomes after total and unicompartmental knee replacement in 101,330 matched patients: a study of data from the National Joint Registry for England and Wales. Lancet2014;384:1437–1445.CrossrefPubMed Google Scholar
2 Liddle AD , PanditH, JudgeA, MurrayDW. Patient-reported outcomes after total and unicompartmental knee arthroplasty: a study of 14 076 matched patients from the National Joint Registry for England and Wales. Bone Joint J2015;97-B:793–801. Google Scholar
3 Willis-Owen CA , BrustK, AlsopH, MiraldoM, CobbJP. Unicondylar knee arthroplasty in the UK National Health Service: an analysis of candidacy, outcome and cost efficacy. Knee2009;16:473–478.CrossrefPubMed Google Scholar
4 Price AJ , WebbJ, TopfH, et al.Rapid recovery after oxford unicompartmental arthroplasty through a short incision. J Arthroplasty2001;16:970–976.CrossrefPubMed Google Scholar
5 Price AJ , ReesJL, BeardDJ, et al.Sagittal plane kinematics of a mobile-bearing unicompartmental knee arthroplasty at 10 years: a comparative in vivo fluoroscopic analysis. J Arthroplasty2004;19:590–597.CrossrefPubMed Google Scholar
6 Slover J , EspehaugB, HavelinLI, et al.Cost-effectiveness of unicompartmental and total knee arthroplasty in elderly low-demand patients. A Markov decision analysis. J Bone Joint Surg [Am]2006;88-A:2348–2355.CrossrefPubMed Google Scholar
7 Rougraff BT , HeckDA, GibsonAE. A comparison of tricompartmental and unicompartmental arthroplasty for the treatment of gonarthrosis. Clin Orthop Relat Res1991;273:157–164.PubMed Google Scholar
8 Baker PN , PetheramT, AveryPJ, GreggPJ, DeehanDJ. Revision for unexplained pain following unicompartmental and total knee replacement. J Bone Joint Surg [Am]2012;94-A:126.CrossrefPubMed Google Scholar
9 The NJR Editorial Board. 11th Annual Report 2014. National Joint Registry for England, Wales and Northern Ireland. http://www.njrcentre.org.uk/njrcentre/Reports,PublicationsandMinutes/Annualreports/tabid/86/Default.aspx (date last accessed 11 July 2016). Google Scholar
10 Pandit H , JenkinsC, BarkerK, DoddCA, MurrayDW. The Oxford medial unicompartmental knee replacement using a minimally-invasive approach. J Bone Joint Surg [Br]2006;88-B:54–60.CrossrefPubMed Google Scholar
11 Pandit H , JenkinsC, GillHS, et al.Unnecessary contraindications for mobile-bearing unicompartmental knee replacement. J Bone Joint Surg [Br]2011;93-B:622–628.CrossrefPubMed Google Scholar
12 Kendrick BJ , RoutR, BottomleyNJ, et al.The implications of damage to the lateral femoral condyle on medial unicompartmental knee replacement. J Bone Joint Surg [Br]2010;92-B:374–379.CrossrefPubMed Google Scholar
13 Berend KR , BerendME, DaluryDF, et al.Consensus Statement on Indications and Contraindications for Medial Unicompartmental Knee Arthroplasty. J Surg Orthop Adv2015;24:252–256.PubMed Google Scholar
14 Goodfellow JW , KershawCJ, BensonMK, O'ConnorJJ. The Oxford Knee for unicompartmental osteoarthritis. The first 103 cases. J Bone Joint Surg [Br]1988;70-B:692–701.CrossrefPubMed Google Scholar
15 Beard DJ , PanditH, OstlereS, et al.Pre-operative clinical and radiological assessment of the patellofemoral joint in unicompartmental knee replacement and its influence on outcome. J Bone Joint Surg [Br]2007;89-B:1602–1607.CrossrefPubMed Google Scholar
16 Davies AP , CalderDA, MarshallT, GlasgowMM. Plain radiography in the degenerate knee: a case for change. J Bone Joint Surg [Br]1999;81-B:632–635. Google Scholar
17 Gibson PH , GoodfellowJW. Stress radiography in degenerative arthritis of the knee. J Bone Joint Surg [Br]1986;68-B:608–609.CrossrefPubMed Google Scholar
18 Johnson AJ , HowellSM, CostaCR, MontMA. The ACL in the arthritic knee: how often is it present and can preoperative tests predict its presence?Clin Orthop Relat Res2013;471:181–188.CrossrefPubMed Google Scholar
19 Dodd M , TrompeterA, HarrisonT, PalmerS. The pivot shift test is of limited clinical relevance in the arthritic anterior cruciate ligament-deficient knee. J Knee Surg2010;23:131–135.CrossrefPubMed Google Scholar
20 Keyes GW , CarrAJ, MillerRK, GoodfellowJW. The radiographic classification of medial gonarthrosis. Correlation with operation methods in 200 knees. Acta Orthop Scand1992;63:497–501.CrossrefPubMed Google Scholar
21 Beard DJ , PanditH, GillHS, et al.The influence of the presence and severity of pre-existing patellofemoral degenerative changes on the outcome of the Oxford medial unicompartmental knee replacement. J Bone Joint Surg [Br]2007;89-B:1597–1601.CrossrefPubMed Google Scholar
22 Oosthuizen CR , BurgerS, VermaakDP, GoldschmidtP, SpangenbergR. The X-Ray Knee instability and Degenerative Score (X-KIDS) to determine the preference for a partial or a total knee arthroplasty (PKA/TKA). SA Orthopaedic Journal2015;14:61–69. Google Scholar
23 Pandit H , HamiltonTW, JenkinsC, et al.The clinical outcome of minimally invasive Phase 3 Oxford unicompartmental knee arthroplasty: a 15-year follow-up of 1000 UKAs. Bone Joint J2015;97-B:1493–1500.CrossrefPubMed Google Scholar
24 Insall JN , DorrLD, ScottRD, ScottWN. Rationale of the Knee Society clinical rating system. Clin Orthop Relat Res1989;248:13–14.PubMed Google Scholar
25 Saleh KJ , MulhallKJ, BershadskyB, et al.Development and validation of a lower-extremity activity scale. Use for patients treated with revision total knee arthroplasty. J Bone Joint Surg [Am]2005;87-A:1985–1994.CrossrefPubMed Google Scholar
26 Zahiri CA , SchmalzriedTP, SzuszczewiczES, AmstutzHC. Assessing activity in joint replacement patients. J Arthroplasty1998;13:890–895.CrossrefPubMed Google Scholar
27 Hurst JM , BerendKR, MorrisMJ, LombardiAV Jr. Abnormal preoperative MRI does not correlate with failure of UKA. J Arthroplasty2013;28:184–186. Google Scholar
28 Peto R , PikeMC, ArmitageP, et al.Design and analysis of randomized clinical trials requiring prolonged observation of each patient. II. analysis and examples. Br J Cancer1977;35:1–39.CrossrefPubMed Google Scholar
29 Pandit H , GulatiA, JenkinsC, et al.Unicompartmental knee replacement for patients with partial thickness cartilage loss in the affected compartment. Knee2011;18:168–171.CrossrefPubMed Google Scholar
30 Maier MW , KuhsF, StreitMR, et al.Unicompartmental knee arthroplasty in patients with full versus partial thickness cartilage loss (PTCL): equal in clinical outcome but with higher reoperation rate for patients with PTCL. Arch Orthop Trauma Surg2015;135:1169–1175.CrossrefPubMed Google Scholar
31 Yoshida K , TadaM, YoshidaH, et al.Oxford phase 3 unicompartmental knee arthroplasty in Japan--clinical results in greater than one thousand cases over ten years. J Arthroplasty2013;28:168–171.CrossrefPubMed Google Scholar
32 Lim HC , BaeJH, SongSH, KimSJ. Oxford phase 3 unicompartmental knee replacement in Korean patients. J Bone Joint Surg [Br]2012;94-B:1071–1076.CrossrefPubMed Google Scholar
33 Faour-Martin O , Valverde-GarciaJA, Martin-FerreroMA, et al.Oxford phase 3 unicondylar knee arthroplasty through a minimally invasive approach: long-term results. Int Orthop2013;37:833–838.CrossrefPubMed Google Scholar
34 Lim HC , BaeJH, SongSH, KimSJ. Oxford phase 3 unicompartmental knee replacement in Korean patients. J Bone Joint Surg [Br]2012;94-B:1071–1076.CrossrefPubMed Google Scholar
Author contributions:
T. W. Hamilton: Developed the radiological decision aid and study protocol, Collected primary data, Performed data analysis and interpretation, Wrote the manuscript.
H. G. Pandit: Developed the radiological decision aid and study protocol, Performed data analysis and interpretation, Wrote the manuscript.
A. V. Lombardi: Collected primary data, Critically appraised the manuscript.
J. B. Adams: Collected primary data, Critically appraised the manuscript.
C. R. Oosthuizen: Developed the initial concept of a radiological decision aid, Critically appraised the manuscript.
A. Clavé: Performed data analysis and interpretation, Critically appraised the manuscript.
C. A. F. Dodd: Developed study protocol, Critically appraised the manuscript.
K. R. Berend: Collected primary data, Critically appraised the manuscript.
D. W. Murray: Developed the radiological decision aid an study protocol, Performed data analysis and interpretation, Wrote the manuscript.
This is an open-access article distributed under the terms of the Creative Commons Attributions licence (CC-BY-NC), which permits unrestricted use, distribution, and reproduction in any medium, but not for commercial gain, provided the original author and source are credited.
T. W. Hamilton has been supported by the NIHR Biomedical Research Centre, based at Oxford University Hospitals Trust, Oxford. The views expressed are those of the author(s) and not necessarily those of the NHS, the NIHR or the Department of Health. Financial support has been received from Zimmer Biomet.
A. V. Lombardi reports grants and personal fees from Zimmer Biomet, grants and personal fees from Pacira Pharmaceuticals, grants and personal fees from Orthosensor, grants and other from SPR Therapeutics, personal fees from Innomed, outside the submitted work.
C. A. F. Dodd reports grants and personal fees from Zimmer Biomet during the conduct of the study.
J. B. Adams and K.R. Berend report grants from Zimmer Biomet, grants from Pacira Pharmaceuticals, grants from Orthosensor, grants from SPR Therapeutics, outside the submitted work.
D. W. Murray and H. G. Pandit report grants and personal fees from Zimmer Biomet during the conduct of the study; in addition, D. W. Murray, H. G. Pandit and T. W. Hamilton have a Patent Pending Application Number 1507059.2, and a patent Copyright, both held by Isis Innovation Ltd. (Technology Transfer Office, University of Oxford). Decision Aid for medial unicompartmental knee replacement licensed to Zimmer Biomet, who manufacture both unicompartmental and total knee replacements.
The author or one or more of the authors have received or will receive benefits for personal or professional use from a commercial party related directly or indirectly to the subject of this article. In addition, benefits have been or will be directed to a research fund, foundation, educational institution, or other non- profit organisation with which one or more of the authors are associated.
This article was primary edited by G. Scott.
Supplementary material. An Appendix, the radiological Decision Aid, is available alongside the online version of this article at www.boneandjoint.org.uk









