Abstract
This pilot study reports the clinical outcomes of a combination of partial subscapularis tendon transfer and small-head hemiarthroplasty in patients with rotatator cuff arthropathy. A total of 30 patients (30 shoulders; eight men and 22 women) with a mean age of 74 years (55 to 84) were assessed at a mean follow-up of 31 months (24 to 60). The inclusion criteria were painful cuff tear arthropathy with normal deltoid function and a non-degenerative subscapularis muscle and tendon and a preserved teres minor.
Outcome was assessed using the University of California Los Angeles score, the Japanese Orthopaedic Association score, and the Oxford Shoulder Score. Radiographic measurements included the centre of rotation distance and the length of the deltoid.
All clinical scores were significantly improved post-operatively. The active flexion and external rotation improved significantly at the most recent follow-up (p < 0.035). Although the mean centre of rotation distance changed significantly (p < 0.001), the mean length of the deltoid did not change significantly from the pre-operative value (p = 0.29). The change in the length of the deltoid with < 100° flexion was significantly less than that with > 100° (p < 0.001).
Progressive erosion of the glenoid was seen in four patients. No patient required revision or further surgery.
A combination of partial subscapularis tendon transfer and small-head hemiarthroplasty effectively restored function and relieved pain in patients with rotator cuff arthropathy.
Cite this article: 2015;97-B:1090–5.
The treatment of severe rotator cuff tear arthropathy (CTA) is challenging. Recent studies have shown that reverse total shoulder arthroplasty (RSA) produces satisfactory results, especially in terms of the range of movement (ROM).1-3 Boileau et al1 reported that re-tensioning the deltoid muscle and medialising the centre of rotation increased the deltoid lever arm and the proportion of the deltoid fibres that function as abductors of the shoulder. However, issues, such as insufficient glenoid bone and young age at the time of surgery may preclude the use of RSA. Therefore, other options might be proposed for such patients.1
Hemiarthroplasty remains a viable option in the treatment of CTA, especially in patients who have coped with a rotator cuff deficiency and have retained a functional ROM.4 However, some consider hemiarthroplasty to provide partial pain relief but poor function5,6 as assessed by Neer et al’s7 limited goals. We consider that functional cuff reconstruction with management of the centre of rotation and the length of the deltoid muscle are important factors for improving the ROM after hemiarthroplasty.
The aims of this retrospective study were to evaluate the clinical and functional outcomes of partial subscapularis tendon transfer and small-head hemiarthroplasty in a consecutive series of patients with CTA. We hypothesised that a smaller humeral head would help in functional reconstruction using the effective partial subscapularis tendon transfer created by displacement of the centre of rotation in a medial and caudal direction.
Secondly, we wished to investigate the -relationship between the post-operative ROM, the centre of rotation and the length of the deltoid muscle.
Patients and Methods
Between May 2005 and February 2011, 52 shoulders in 52 patients underwent partial subscapularis tendon transfer and small-head hemiarthroplasty for CTA. The inclusion criteria were painful CTA with normal deltoid function and a non-degenerative subscapularis muscle and tendon. A total of eight patients with a degenerative subscapularis tendon and nine patients with a severe external rotation lag and atrophy of teres minor were excluded. Four patients were lost to follow-up, and one had insufficient pre--operative evaluation, leaving 30 patients in the study (Fig. 1).
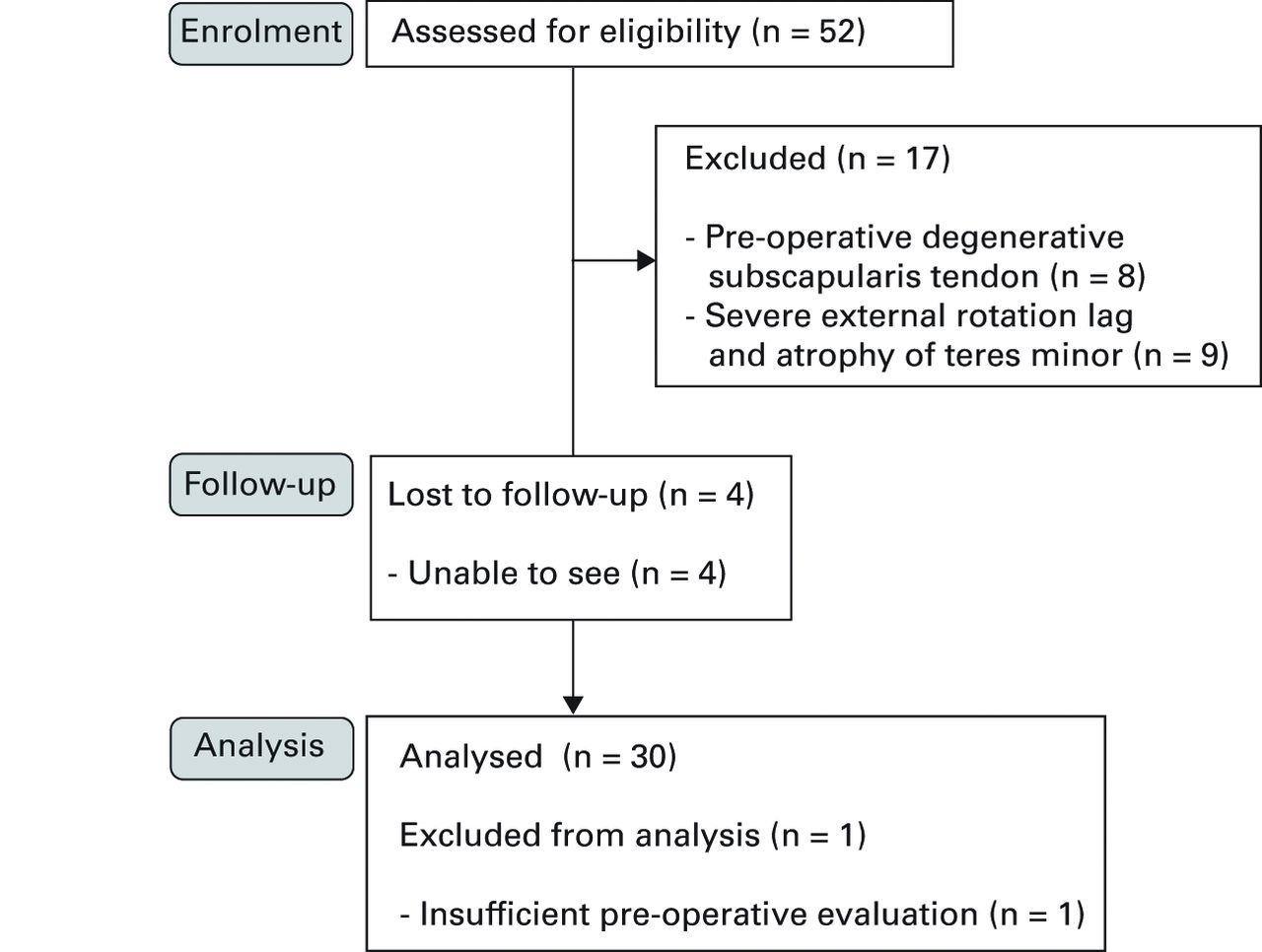
Fig. 1
CONSORT flow diagram
There were eight men and 22 women, with a mean age of 74 years (55 to 84) at the time of the operation (Table I).8 Two patients had undergone previous arthroscopic rotator cuff repair which had failed. All procedures were performed by a single surgeon (NS) using the uncemented Global Advantage system (Depuy, Warsaw, Indiana) (Fig. 2).


Figs. 2a - 2b
Anteroposterior radiographs a) pre- and b) post-operatively of a 72-year-old patient who received a right small-head hemiarthroplasty for treatment of cuff tear arthropathy.
Table I
Patient characteristics
| Characteristic | |
|---|---|
| n | 30 |
| Mean age (yrs; range) | 74 (55 to 84) |
| Gender | |
| Male/female | 8/22 |
| Mean follow-up (mths; range) | 31 (24 to 60) |
| Seebauer’s classification8 | |
| 1A | 15 |
| 1B | 3 |
| 2A | 7 |
| 2B | 5 |
| Fatty infiltration* (range) | |
| SSC | 1.1 (0 to 2) |
| SSP | 2.9 (2 to 4) |
| ISP | 2.8 (2 to 4) |
| TM | 1.2 (0 to 4) |
-
* Grade 0, no fatty deposits; grade 1, some fatty streaks; grade 2, more muscle than fat; grade 3, as much muscle as fat; grade 4, less muscle than fat SSC, subscapularis; SSP, supraspinatus; ISP, infraspinatus; TM, teres minor
All patients were assessed pre- and post-operatively by physiotherapists using the 35-point University of California at Los Angeles (UCLA) shoulder scoring system,9 the 100-point Japanese Orthopaedic Association (JOA) score,10 and the 48-point Oxford Shoulder Score (OSS).11 The results were also graded according to the limited-goals criteria described by Neer.12
The pre-operative radiographs were evaluated for stability and integrity of the glenohumeral joint according to Visotsky et al’s8 classification. Pre-operative fatty infiltration of the rotator cuff muscles was evaluated by MRI according to the criteria described by Goutallier et al13 and modified by Fuchs et al14 at the most lateral section of the oblique sagittal image, where the scapular spine remains in continuity with the body of the scapula forming a Y-shape. The distribution of patients according to these classifications is shown in Table I.
The length of the deltoid was assessed by measuring the distance between the inferolateral tip of the acromion and the midpoint of the deltoid tuberosity with the arm in neutral rotation and 0° of abduction (Fig. 3), on an antero-posterior radiograph of the scapula as described previously.15,16 The centre of rotation of the glenohumeral joint was the centre of the best-fit circle overlaid on the articular surface of the humeral head using a Picture Archive and Communication System in each hospital. The centre of rotation was defined as the perpendicular distance from the deltoid line to the centre of rotation (Fig. 3). Erosion of the glenoid was evaluated radiographically as described by Sirveaux et al.3


Figs. 3a - 3b
Radiographic measurement of the length of the deltoid and the centre of rotation. The length of the deltoid from the inferolateral aspect of the tip of the acromion to the midpoint of the deltoid tuberosity is shown pre- a) and post-operatively b). The centre of rotation was defined as the perpendicular distance from the line of the length of the deltoid to the centre of rotation.
Surgical technique
The procedure was performed under general anaesthetic with the patient in the beach-chair position. An anterosuperior approach, as described by Neviaser17 and Mac-Kenzie,18 was used for hemiarthroplasty. A 6 cm sabre-type incision over the anterolateral aspect of the acromion was used. The anterior and middle fibres of the deltoid were detached subperiosteally along the direction of the fibres. As exposure of the glenoid was not required, release of the deltoid could be kept to a minimum. Although the lateral edge and spur of the acromion were resected, the medial part of the coraco-acromial arch was preserved as much as possible to avoid subsequent migration of the humeral head anterosuperiorly. A tenotomy of the long head of the biceps tendon was performed when degeneration and fraying of the tendon were seen.
A pilot hole was created at the top of the humerus, in line with its long axis and 10 mm to 15 mm posterior to the bicipital groove. The hole was reamed until one of the reamers began to bite into the cortex, and the appropriate sized trial stem was introduced. The humeral head was resected along the angle of the undersurface of the head of the trial stem, with the arm in 40° of external rotation. The trial was introduced in between 30° to 40° of retroversion to prevent anterosuperior migration. A small humeral head (40 mm × 15 mm or 40 mm × 18 mm) was tested, and the appropriate size was determined by the inability to translate the humeral head anteriorly or inferiorly beyond the rim of the glenoid. We defined a small head as being one size smaller than the size of the humeral head. After implantation, the excess bony edge of the calcar was resected to avoid impingement with the glenoid rim. If there was an unacceptable gap between the implant and the bony edge following resection, an offset modular component was used. Repair of the rotator cuff was not possible even though a small-head replacement was used. A partial subscapularis tendon transfer using a modification of the procedure described by Cofield19 was undertaken, in which the cranial two thirds of the tendon were transferred upward and dorsally (Fig. 4) and sutured to the greater tuberosity and to the cranial border of the tendon of teres minor with No. 2 non-absorbable sutures (Ethibond; Ethicon, Somerville, New Jersey). The congruity of the glenohumeral joint was assessed by observing the passive ROM under image intensification. The attachment of the deltiod was repaired through the bone tunnels.
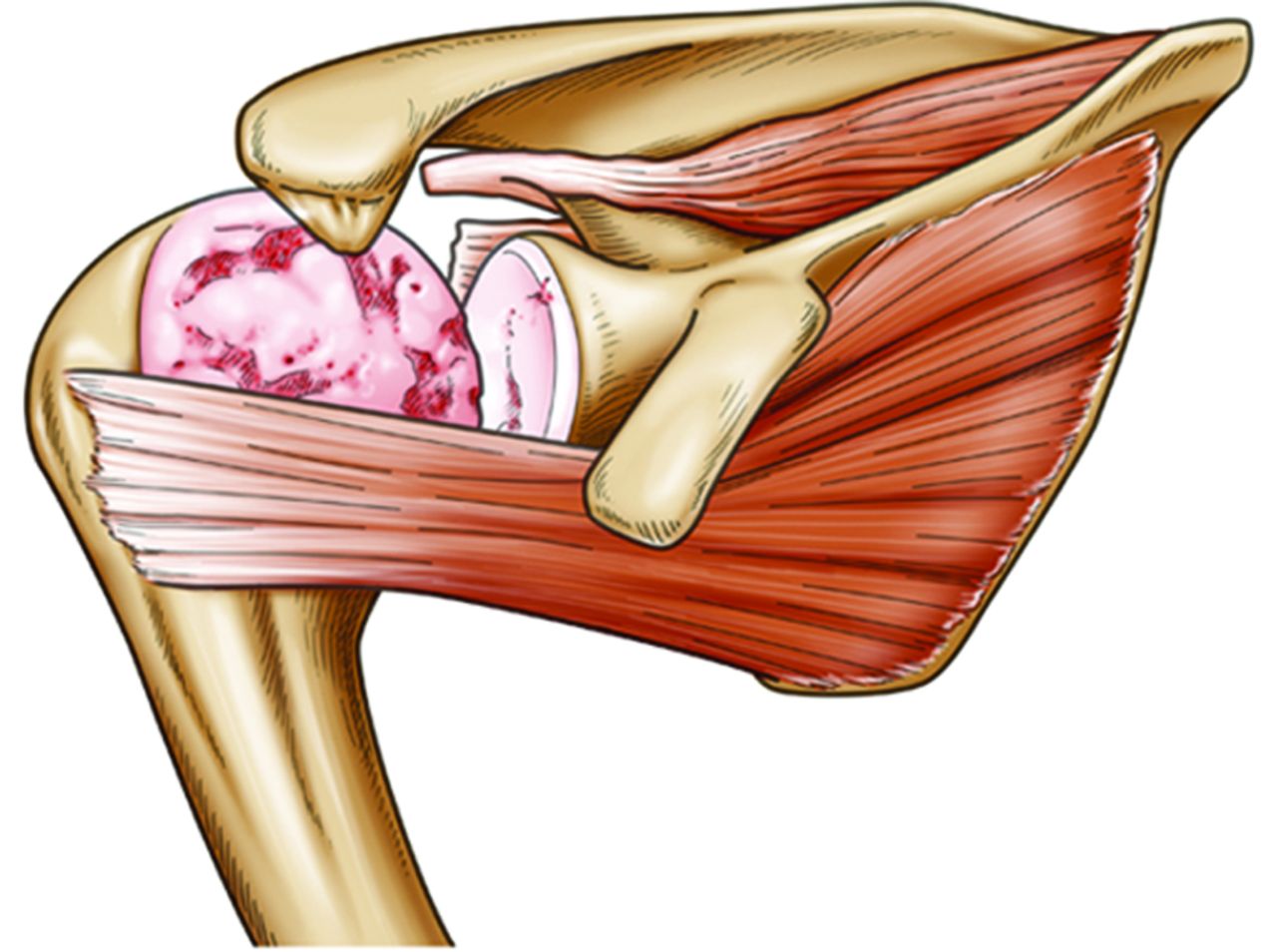
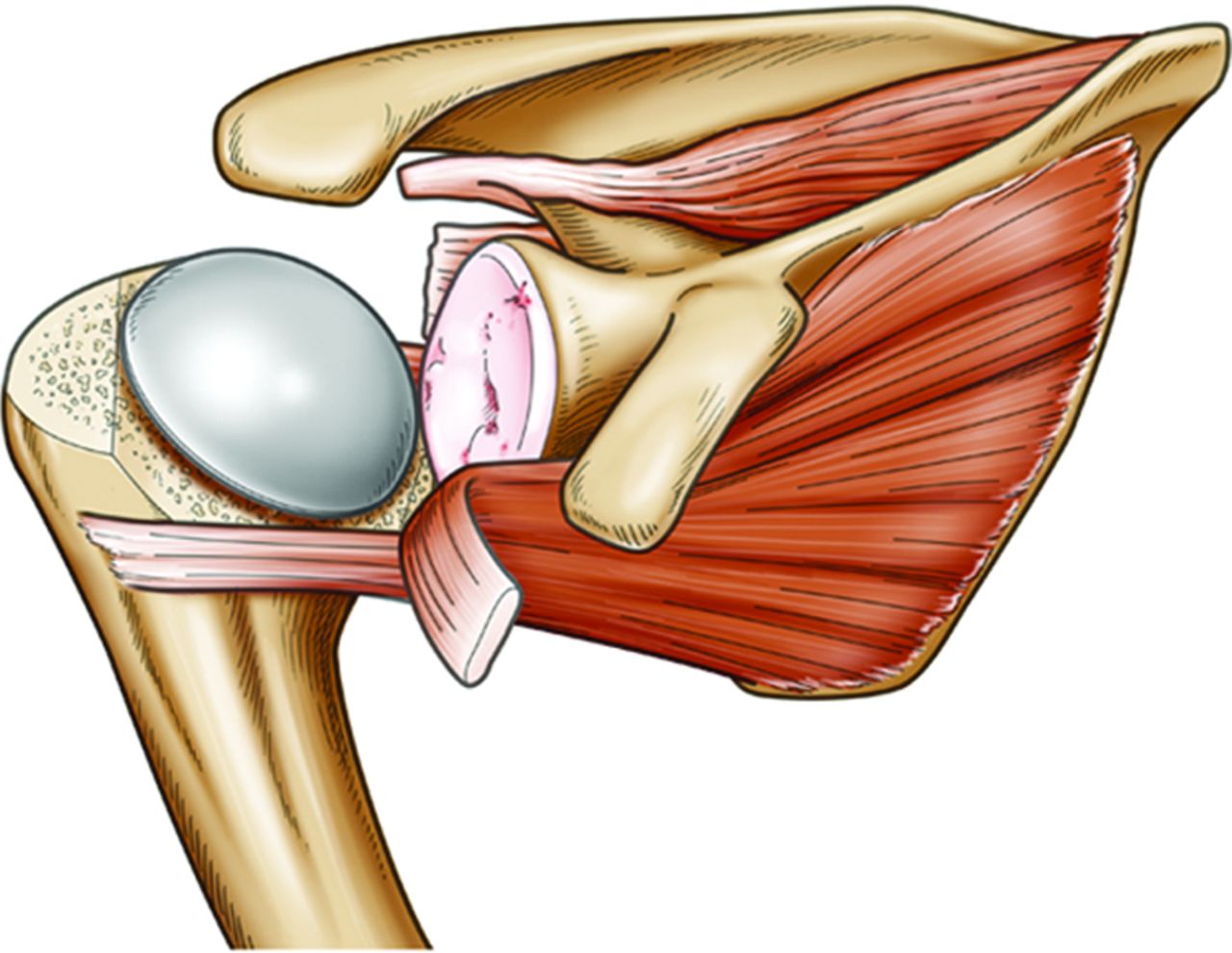
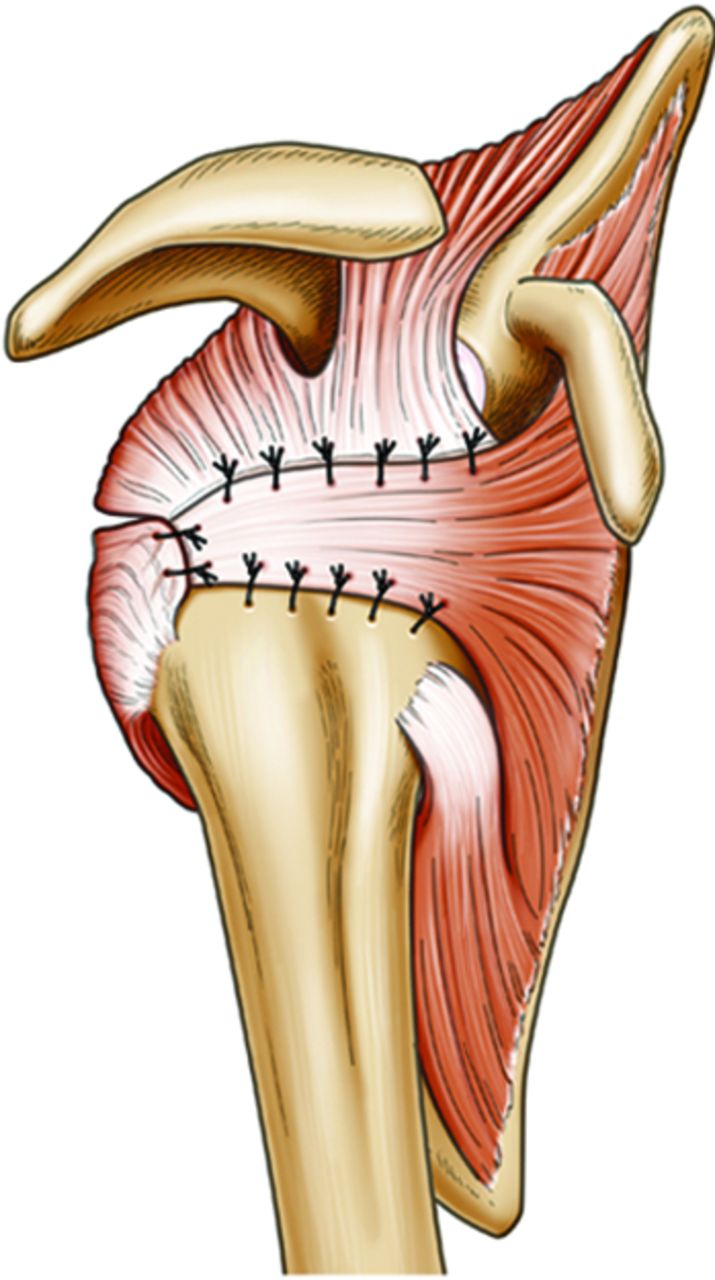
Figs. 4a - 4c
Diagrams showing partial transfer of the subscapularis tendon using the modified Cofield procedure19 with small-head hemiarthroplasty:a) pre--operative rotator cuff tear arthropathy, b) the humeral head was resected and a small humeral head was introduced and c) two thirds of the subscapularis tendon was transferred upwardly and dorsally
An abduction pillow was used for eight weeks post-operatively. Patients completed a systematic rehabilitation programme under guidance from a physiotherapist comprising passive exercises starting two weeks after surgery. Active flexion of the shoulder from the adducted position in a sitting position was allowed ten weeks post-operatively. Heavy work or sports were allowed six months after the operation.
Statistical analysis
All statistical analyses were performed with Excel 2000 (Microsoft Corp., Redmond, Washington) and JMP 8.0 software (SAS Institute, Cary, North Carolina). Changes in continuous or ordinal variables were assessed using the paired -test. A p-value < 0.05 was considered to be significant.
Results
The mean follow-up was 31 months (24 to 60). There were significant improvements in functional outcomes and pain relief at this time with significant improvements in the mean UCLA, JOA and OSS scores (Table II). The mean active flexion improved significantly from 75° (20° to 120°) to 136° (60° to 170°; p < 0.001). The mean active external rotation improved significantly from 18° (-10° to 60°) to 30° (0° to 60°) (p = 0.035; Table II). According to Neer’s12 limited-goals criteria, 25 shoulders (83%) were evaluated as excellent or satisfactory.
Table II
Comparison of the pre- and post-operative clinical scores and radiographic measurements (-tests)
| Assessment | Pre-operative | Final follow-up | Change | p-value |
|---|---|---|---|---|
| Mean (range) | Mean (range) | Mean (range) | ||
| Clinical score | ||||
| UCLA | 12 (6 to 20) | 27 (7 to 32) | 15 (- 3 to 27) | < 0.001 |
| JOA | 39 (16 to 61) | 78 (40 to 93) | 39 (1 to 52) | < 0.001 |
| OSS | 14 (5 to 22) | 40 (16 to 45) | 26 (4 to 40) | < 0.001 |
| Range of movement | ||||
| Flexion (°) | 75 (20 to 120) | 136 (60 to 170) | 56 (-10 to 140) | < 0.001 |
| External rotation (°) | 18 (-10 to 60) | 30 (0 to 60) | 12 (-40 to 60) | 0.035 |
| Radiographic measurements | ||||
| Centre of rotation distance (mm) | 12.5 (4.4 to 21.2) | 16.6 (8.9 to 28.6) | 4.1 (-3.9 to 11.1) | < 0.001 |
| Deltoid length (mm) | 126.0 (105.6 to 154.0) | 126.9 (102.8 to 152.2) | 0.9 (-18.0 to 11.9) | 0.29 |
-
UCLA, University California Los Angeles; JOA, Japanese Orthopaedic Association; OSS, Oxford Shoulder Score
The results of the radiographic measurements are shown in Table II. The mean centre of rotation distance changed significantly post-operatively (p < 0.001). The mean length of the deltoid did not change significantly (p = 0.29). Changes in the radiographic measurements are shown in Table III, with the patients divided into two groups, the 24 shoulders which regained > 100° of flexion and the six with < 100°. The deltoid muscle was > 8 mm shorter in all those with < 100° active flexion.
Table III
Radiographic assessments as mean (range) (-tests)
| Characteristic | Total | Flexion ≥ 100° | Flexion < 100° | p-value |
|---|---|---|---|---|
| n (%) | 30 | 24 | 6 ( | |
| Change in the centre of rotation distance (mm) | 4.1 (-3.9 to 11.1) | 4.2 (-1.7 to 11.1) | 3.7 (-3.9 to 10.1) | 0.44 |
| Change in the length of the deltoid (mm) | 0.8 (-18.0 to 11.9) | 3.3 (-4.3 to 12) | -9.8 (-16.2 to 0) | < 0.001 |
There was deterioration in the condition of the glenoid in four patients. The change was from type E0 to E2 in three patients and from E0 to E3 in one.3 By contrast, the degree of erosion of the glenoid in the other 26 patients, including six type E1 and two type E2 pre-operatively, was unchanged at final review.
No patient underwent revision surgery for implant failure, dislocation, or fracture. No patient developed an infection and there were no stem-related radiolucent lines at the final follow-up.
Discussion
RSA is a well-established and reliable treatment for CTA. However, complications include rupture of the deltoid, fracture of the spine of the acromion and loosening of the glenosphere.2,20-22 Favard et al22 showed that function deteriorated progressively after eight years post-operatively and that radiographic abnormalities of the humeral or glenoid components, such as a glenoid notch, fracture, or lysis around the screw or the central peg, and lysis around the humeral component, increased after five years. Moreover, there are few revision options available when a RSA fails. They suggested that caution should be used when recommending RSA, and that other options for the treatment of symptomatic CTA should be considered.
In the current study, we found satisfactory results after partial subscapularis tendon transfer combined with a small-head hemiarthroplasty in these patients. We believe that achieving an adequate ‘force couple’23 provides a larger active ROM compared with normal-sized head hemiarthroplasty for CTA. VY-plasty using a modification of the method of Cofield19 appeared to achieve an adequate force couple in patients with an irreparable posterosuperior defect of the rotator cuff. Successful repair of a severely degenerated rotatator cuff does not appear to influence the outcome, as flexion is not reliably restored after repair.5
We suggest that it is important to suture the tendon to the bone securely and to prevent too much stress at the site of transfer of the tendon.
The advantage of using a small head is that it helps functional reconstruction of the cuff by reducing the volume of the humeral head and the length of the deltoid. The reduced height of the humeral head makes it easy to close the cuff defect by a partial subscapularis tendon transfer in the presence of an intact teres minor. Hemiarthroplasty in this manner also allows for later revision to a conventional arthroplasty without the problems associated with loss of glenoid and humeral bone stock engendered by RSA.
However, small-head replacement is associated with biomechanical concerns. We investigated the relationship between post-operative flexion and radiographic factors. Where cranial migration of the humeral head has occurred pre-operatively, we consider that normalisation of the -centre of rotation is required to produce a good ROM, however, the use of a small head risks shortening the length of the deltoid. We believe that preservation of this length is an important feature of the procedure (Table III). In the current study, a shorter length of deltoid may have been caused by over-resection of the humeral head, use of a hemiarthroplasty that was too small, post-operative contracture of the deltoid or failure of the reconstruction of the rotator cuff. Care is required to avoid resecting too much of the humeral head intra-operatively. We always confirm the balance between the size of the humeral head and the length of the deltoid fluoroscopically. When too much humeral head is resected, the eccentric modular head can be rotated superiorly- to increase the height of the prosthetic humeral head without increasing its diameter.
Alteration of the centre of rotation after implanting a humeral head of small diameter may be another important factor in producing a satisfactory result. Although media-lisation of the centre of rotation is a rationale for the use of a RSA, the amount of medialisation we obtained did not seem to be related to the post-operative flexion in the -current study, which appears to correlate with Jobin et al’s16 findings. In contrast, a more anatomical centre of rotation may provide more glenohumeral movement because of improvement in the tension in the remaining rotator cuff.24
Use of the small head may have led to a concentration of stress on the surface of the glenoid. Erosion of the glenoid had progressed in four shoulders (13%), similar to a previous study,25 and in one shoulder the erosion was extensive (E3 type). Although the follow-up period for this patient was 40 months, we remain concerned about potential difficulties for future revision surgery. The extent of erosion of the glenoid was not related to the clinical outcome, active flexion, or external rotation.
The present study has several limitations. First, the efficacy of rotator cuff function is a key factor for improving the ROM. However, we have no imaging of the rotator cuff after hemiarthroplasty about which we can be confident of its integrity. We believe that muscle atrophy and fatty infiltration should be investigated in a long-term study. -Secondly, the appropriate size of the humeral head implant could not be determined in the current study because the same size of implant (40 mm × 15 mm) was used in most cases. The size of the humeral head would affect the extent of the medialisation and the length of the deltoid. The size of the head which we used may be almost anatomical in a patient with a small physique, and a smaller head might be required for such a patient. Biomechanical and clinical studies are needed to investigate this further. Thirdly, we did not directly compare the clinical results of our procedure with those of RSA. Finally, the study group was small and the follow up was short. Young et al26 reported that the length of follow-up was the most significant factor associated with secondary rotator cuff dysfunction following RSA assessed after five years.
In conclusion, functional reconstruction of the rotator cuff and the use of a small-head hemiarthroplasty for CTA effectively restored function and relieved pain in this series. Preservation of the length of the deltoid is an important factor in improving flexion post-operatively. Despite the limitations of this study, the findings suggest that the combination of tendon transfer and small-head hemiarthroplasty is a viable option for improving the outcomes in the treatment of selected patients with CTA. The reinforcement of concentric loading using a confluent non-degenerative subscapularis and teres minor, and the adaptation of their action in active flexion and external rotation by control of the centre of rotation relative to the deltoid, appeared to improve the function of the shoulder.
1 Boileau P , WatkinsonDJ, HatzidakisAM, BalgF. Grammont reverse prosthesis: design, rationale, and biomechanics. J Shoulder Elbow Surg2005;14(suppl S):147S–161S.CrossrefPubMed Google Scholar
2 Frankle M , SiegalS, PupelloD, et al.The Reverse Shoulder Prosthesis for glenohumeral arthritis associated with severe rotator cuff deficiency. A minimum two-year follow-up study of sixty patients. J Bone Joint Surg [Am]2005;87-A:1697–1705.CrossrefPubMed Google Scholar
3 Sirveaux F , FavardL, OudetD, et al.Grammont inverted total shoulder arthroplasty in the treatment of glenohumeral osteoarthritis with massive rupture of the cuff. Results of a multicentre study of 80 shoulders. J Bone Joint Surg [Br]2004;86-B:388–395.CrossrefPubMed Google Scholar
4 Nam D , MaakTG, RaphaelBS, et al.Rotator cuff tear arthropathy: evaluation, diagnosis, and treatment: AAOS exhibit selection. J Bone Joint Surg [Am]2012;94-A:34.CrossrefPubMed Google Scholar
5 Goldberg SS , BellJE, KimHJ, et al.Hemiarthroplasty for the rotator cuff-deficient shoulder. J Bone Joint Surg [Am]2008;90-A:554–559.CrossrefPubMed Google Scholar
6 Sanchez-Sotelo J , CofieldRH, RowlandCM. Shoulder hemiarthroplasty for glenohumeral arthritis associated with severe rotator cuff deficiency. J Bone Joint Surg [Am]2001;83-A:1814–1822.CrossrefPubMed Google Scholar
7 Neer CS II , CraigEV, FukudaH. Cuff-tear arthropathy. J Bone Joint Surg [Am]1983;65-A:1232–1244. Google Scholar
8 Visotsky JL , BasamaniaC, SeebauerL, RockwoodCA, JensenKL. Cuff tear arthropathy: pathogenesis, classification, and algorithm for treatment. J Bone Joint Surg [Am]2004;86-A(Suppl2):35–40.PubMed Google Scholar
9 Ellman H , HankerG, BayerM. Repair of the rotator cuff. End-result study of factors influencing reconstruction. J Bone Joint Surg [Am]1986;68-A:1136 -1144:.PubMed Google Scholar
10 Ide J , TakagiK. Early and long-term results of arthroscopic treatment for shoulder stiffness. J Shoulder Elbow Surg2004;13:174–179.CrossrefPubMed Google Scholar
11 Dawson J , FitzpatrickR, CarrA. Questionnaire on the perceptions of patients about shoulder surgery. J Bone Joint Surg [Br]1996;78-B:593–600.PubMed Google Scholar
12 Neer CS Shoulder reconstruction. Philadelphia: WB Saunders; 1990:262. Google Scholar
13 Goutallier D , PostelJM, BernageauJ, LavauL, VoisinMC. Fatty muscle degeneration in cuff ruptures: pre- and post-operative evaluation by CT scan. Clin Orthop Relat Res1994;304:78–83. Google Scholar
14 Fuchs B , WeishauptD, ZanettiM, HodlerJ, GerberC. Fatty degeneration of the muscles of the rotator cuff: assessment by computed tomography versus magnetic resonance imaging. J Shoulder Elbow Surg1999;8:599–605.CrossrefPubMed Google Scholar
15 De Wilde L , AudenaertE, BarbaixE, AudenaertA, SoudanK. Consequences of deltoid muscle elongation on deltoid muscle performance: a computerised study. Clin Biomech (Bristol, Avon)2002;17:499–505.CrossrefPubMed Google Scholar
16 Jobin CM , BrownGD, BahuMJ, et al.Reverse total shoulder arthroplasty for cuff tear arthropathy: the clinical effect of deltoid lengthening and center of rotation medialization. J Shoulder Elbow Surg2012;21:1269–1277.CrossrefPubMed Google Scholar
17 Neviaser JS . Surgical approaches to the shoulder. Clin Orthop Relat Res1973;91:34–40.PubMed Google Scholar
18 MacKenzie DB . The anterosuperior exposure for total shoulder replacement. Orthop Trauma1993;2:71–77. Google Scholar
19 Cofield RH . Subscapular muscle transposition for repair of chronic rotator cuff tears. Surg Gynecol Obstet1982;154:667–672.PubMed Google Scholar
20 Boileau P , GonzalezJF, ChuinardC, BicknellR, WalchG. Reverse total shoulder arthroplasty after failed rotator cuff surgery. J Shoulder Elbow Surg2009;18:600–606.CrossrefPubMed Google Scholar
21 Boileau P , WatkinsonD, HatzidakisAM, HovorkaI. Neer Award 2005: The Grammont reverse shoulder prosthesis: results in cuff tear arthritis, fracture sequelae, and revision arthroplasty. J Shoulder Elbow Surg2006;15:527–540.CrossrefPubMed Google Scholar
22 Favard L , LevigneC, NerotC, et al.Reverse prostheses in arthropathies with cuff tear: are survivorship and function maintained over time?Clin Orthop Relat Res2011;469:2469–2475.CrossrefPubMed Google Scholar
23 Hsu JE , ReutherKE, SarverJJ, et al.Restoration of anterior-posterior rotator cuff force balance improves shoulder function in a rat model of chronic massive tears. J Orthop Res2011;29:1028–1033.CrossrefPubMed Google Scholar
24 Frankle M , LevyJC, PupelloD, et al.The reverse shoulder prosthesis for glenohumeral arthritis associated with severe rotator cuff deficiency. a minimum two-year follow-up study of sixty patients surgical technique. J Bone Joint Surg [Am]2006;88-A(Suppl1Pt2):178–190.CrossrefPubMed Google Scholar
25 Pape G , BrucknerT, LoewM, ZeifangF. Treatment of severe cuff tear arthropathy with the humeral head resurfacing arthroplasty: two-year minimum follow-up. J Shoulder Elbow Surg2013;22:1–7.CrossrefPubMed Google Scholar
26 Young AA , WalchG, PapeG, GohlkeF, FavardL. Secondary rotator cuff dysfunction following total shoulder arthroplasty for primary glenohumeral osteoarthritis: results of a multicenter study with more than five years of follow-up. J Bone Joint Surg [Am]2012;94-A:685–693.CrossrefPubMed Google Scholar
Author contributions:
A. Urita: Data collection.
T. Funakoshi: Data analysis, Writing the paper.
N. Suenaga: Performed surgeries.
N. Oizumi: Data collection.
N. Iwasaki: Data analysis.
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
This article was primary edited by G. Scott and first proof edited by J. Scott.









