Abstract
Primary total knee arthroplasty (TKA) is a reliable procedure with reproducible long-term results. Nevertheless, there are conditions related to the type of patient or local conditions of the knee that can make it a difficult procedure. The most common scenarios that make it difficult are discussed in this review. These include patients with many previous operations and incisions, and those with severe coronal deformities, genu recurvatum, a stiff knee, extra-articular deformities and those who have previously undergone osteotomy around the knee and those with chronic dislocation of the patella.
Each condition is analysed according to the characteristics of the patient, the pre-operative planning and the reported outcomes.
When approaching the difficult primary TKA surgeons should use a systematic approach, which begins with the review of the existing literature for each specific clinical situation.
Cite this article: Bone Joint J 2015;97-B(10 Suppl A):30–9.
Total knee arthroplasty (TKA) has shown excellent results at long-term follow-up with a small complication rate in many series during the last three decades.1-4 However, there are conditions which may affect the outcome of TKA because of the complexity of the surgery or specific states of the affected limb. When the surgeon is dealing with an unusual deformity of the bone or soft-tissue envelope around the knee, the complication rate of TKA can rise to between 5% and 41%, which significantly affects the outcome.5-16 These conditions are relatively uncommon. The operative training of surgeons should be supported by knowledge of reported series describing the specific conditions which lead to difficult procedures. The aim of this paper is to review the conditions which may adversely affect the usually excellent outcome of TKA.
In order to identify relevant papers dealing with the different aspects that characterise a ‘difficult patient’ we carried out a research of English language literature using the MEDLINE database with the search items “total knee arthroplasty AND wound problems”, “total knee arthroplasty AND severe valgus OR severe varus”, “total knee arthroplasty AND recurvatum”, “total knee arthroplasty AND stiff knee”, “total knee arthroplasty AND extra-articular deformity”, “total knee arthroplasty AND osteotomy” and “total knee arthroplasty AND neglected patellar dislocation”. Additional papers were identified by checking the references. A total of 330 papers were extracted. Two authors (GB and VF) independently reviewed each abstract. Once a paper was identified as likely to be included, full-text versions were obtained. Conflict about the inclusion of a paper was resolved by further evaluation which was undertaken by the senior author (AB). A total of 264 papers were excluded from the analysis for the following reasons: 11 were case reports, 45 did not evaluate the outcome of TKA, 20 were not in English, 169 were not related to the research and in 19 papers the abstract was not available. Therefore, 66 papers were finally included (Fig. 1).
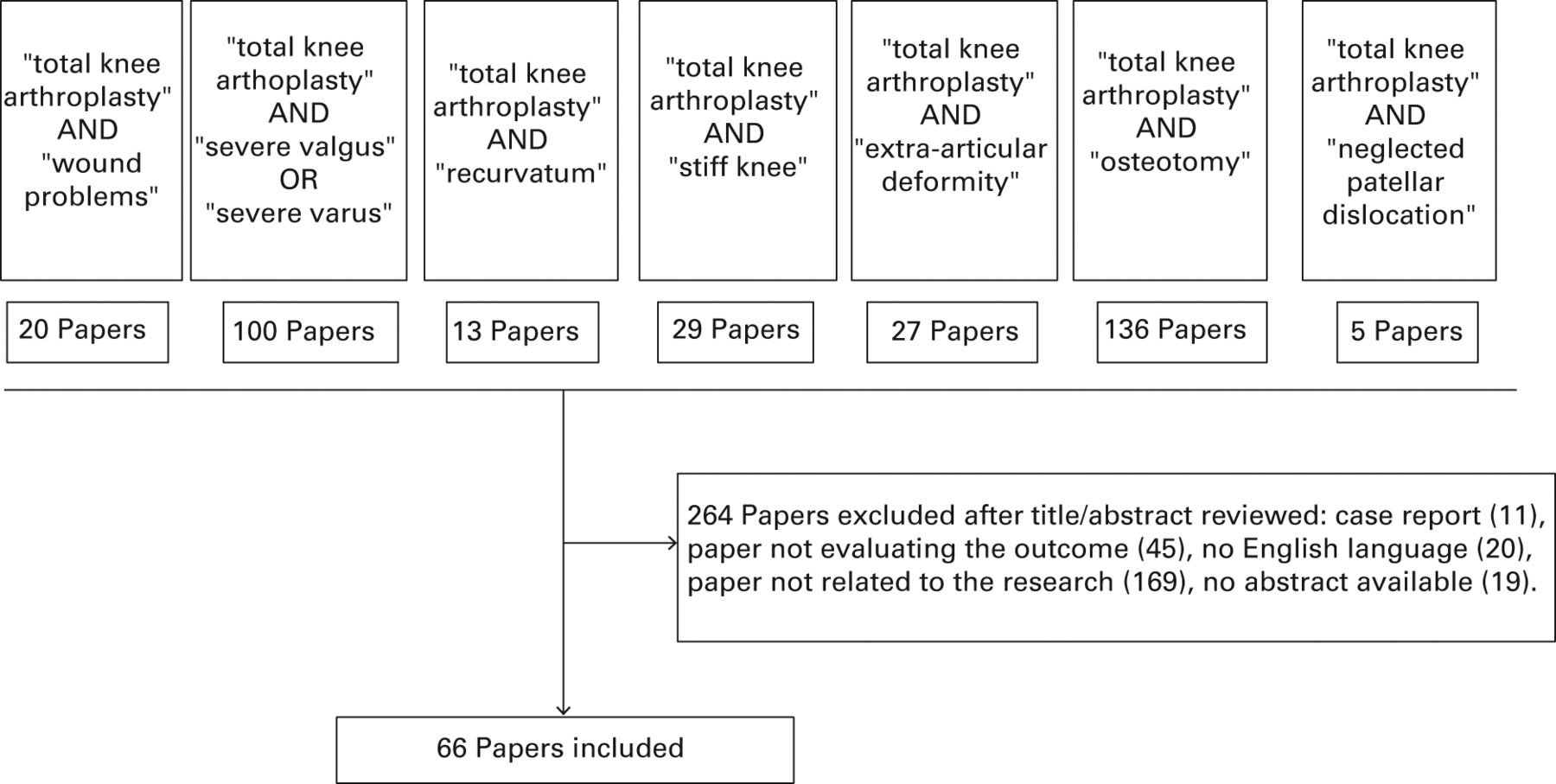
Fig. 1
Flow chart of randomised controlled trials and cohort studies identified for the review.
In each section, the typical characteristics of the patients, the pre-operative planning and the reported outcome in the literature are described.
Patients with many previous incisions
Previous incisions might be present after procedures such as open reduction and internal fixation (ORIF) for fractures, ligamentous reconstruction, open meniscectomy and osteotomy. The skin must be evaluated for previous fistulae or sites of infection, and adhesion of the skin to the bone is a source of concern.17 It is important to evaluate the elasticity of the skin, as scarring and stiffness increase the tension of the wound and can affect the oxygen tension of the flaps during flexion, leading to delayed healing and possible breakdown during flexion.17 Other characteristics of the patients which may lead to delayed wound healing should be recorded including smoking,18 obesity,19 renal and liver insufficiency,19 corticosteroid use20 and diabetes.21
Four choices are possible: a new incision, the same incision, part of the same incision, or a prophylactic flap. A new medial incision is chosen when there is a safe distance from a parallel lateral incision. Several authors suggest 6 cm, but there is no particular evidence to support this distance.22,23 This distance does not apply for incisions around the ankle in the treatment of tibial plafond fractures,24 and others suggest an empirical threshold of 5 cm in TKA.25 Distally, the new incision can be extended laterally towards the tibial tuberosity, avoiding the creation of too narrow a bridge of skin between the incisions. A good rule of thumb is the 2 to 1 ratio which applies to the use of random fasciocutaneous flaps.26 If a Judet arthrolysis27 has been performed previously, we suggest using a lateral approach, as the extent of soft-tissue damage from the previous surgery is not known. If there are three or more parallel previous incisions, the most lateral should be chosen. When approaching a stiff knee through a lateral incision, the surgeon must be ready to perform an extensile approach. Proximal adhesions should be removed and medial-lateral gutters should be opened before extending the approach proximally and distally. The combination of stiffness and a lateral approach usually requires a distal extension with a tibial tubercle osteotomy (TTO). In patients in whom a medial and lateral ‘hockey stick’ approach has been previously used for fixation of a bicondylar tibial plateau fracture, the incision can be midline as the transverse components of the previous scars make a physiological flap with the new incision. Again, distally it should fuse with the distal part of the lateral one. A full thickness skin flap can be developed up to the tuberosity medially to allow the usual medial para-patellar approach. Scott et al5 reported a higher risk for necrosis with hockey stick incisions, but it was not specified if hardware was removed during the surgery because this might affect the revascularisation of soft tissues. In the presence of several previous incisions and scarring, adhesion to the capsule or previous skin grafting to the periosteum, the use of a prophylactic local or free flap might be considered. This allows good soft-tissue cover and wound healing. Casey et al25 have shown that a prophylactic flap gives better results than a salvage flap and have proposed a useful algorithm for selecting the high-risk patients that could benefit from this procedure.
The choice of the approach in the presence of many previous incisions is vital to the survival of the soft-tissue cover, and despite the widespread recommendations of several authors about the importance of this issue, little has been written on the subject, with few practical suggestions. The rate of wound complications after primary TKA following failure of ORIF for the treatment of fractures, including superficial infection, dehiscence and necrosis in primary TKA, varies between 4.8% and 13%.5-7 Saleh et al28 reported no wound complications in 15 patients, but a sham incision was used in two patients and one required flap cover. In a study by Casey et al,25 the complication after the use of prophylactic flap cover occurred in 11 of 23 patients (48%) but soft-tissue cover was achieved and all patients underwent successful TKA subsequently with no wound complications.
Severe coronal deformities
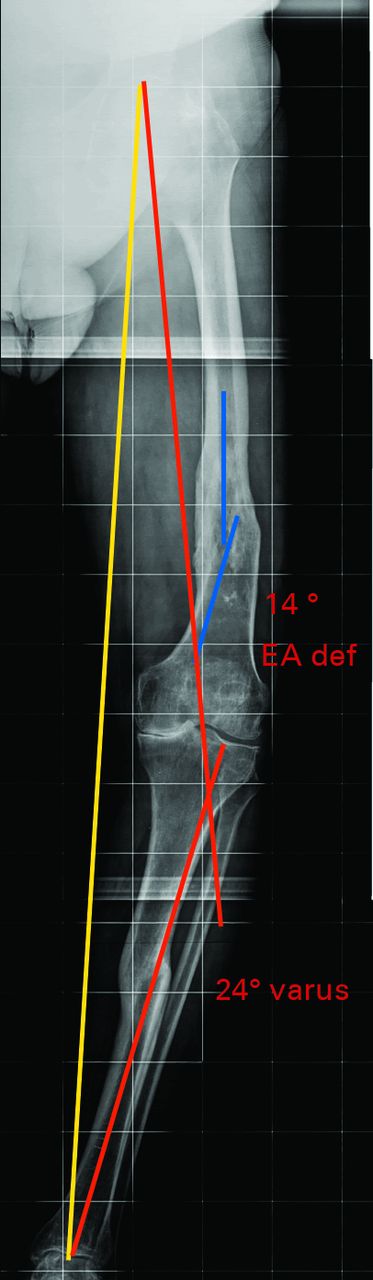
A severe coronal deformity may be defined as one which involves fixed varus or valgus deviation of ≥ 20° from the neutral mechanical axis on weight-bearing films.29-33 Such a deformity may be intra-articular because of cartilage or bone loss, stress fractures, malunions/nonunions, or extra-articular (metaphyseal or diaphyseal) owing to a previous fracture, femoral bowing or a previous osteotomy (Fig. 2).34 Patients with a significant coronal deformity typically have some bone erosion and/or condylar dysplasia on the concave side of the deformity, while the opposite, convex side of the joint is affected by tension forces with stretched soft-tissues.35 In addition, significant varus/valgus deformities are often associated with abnormalities in the sagittal plane or torsional deformities. Patients with significant malalignment often have extra-articular deforming forces, which have a role in the development or maintenance of the deformity.




Figs. 2a - 2d
Pre-operative a) anteroposterior (AP) and b) lateral radiographs of a severe valgus deformity with a retained Kuntscher nail in the tibia; and post-operative c) AP and d) lateral radiographs showing correction of the deformity using a ‘pie-crusting’ technique through a medial parapatellar approach. The Kuntscher nail could be retained by using a short-pegged tantalum-coated tibial component with cemented fixation because of poor bone quality
Accurate pre-operative planning is essential. In particular, the study of the patterns of gait in patients with severe varus/valgus deformity can add useful information. Those with a varus knee and high adduction moments without a flexion contracture with a lateral thrust of the tibia during walking will have severe laxity of the lateral soft tissues.35 As a consequence of the extensive medial release that is performed in order to balance the elongated lateral side, an opening of the flexion and extension gaps is generated; a standard tibial bone cut will result in larger gaps which need to be filled by thicker polyethylene inserts.35 Koninckx et al36 showed that it is possible to manage a severe deformity without implanting a constrained articulation performing minimal bone resection and ligament release. When planning tibial resection in patients with a constitutional varus deformity, the proximal centre of the tibial cutting jig generally faces the lateral tibial spine in order to match the tibial anatomical axis.37 Patients with a valgus knee and a plano-valgus foot who walk with a high abduction moment, may stretch the medial collateral ligament (MCL) after surgery if the deformity of the foot is not addressed by surgery or insoles. In patients with a bilateral severe valgus deformity, after one side is corrected with TKA, the contralateral valgus non-operated knee may induce a high adduction moment in the operated knee.38 Under these circumstances, if non-constrained components have been used with an extensive lateral release, the adduction moment generated by the contralateral limb may predispose to a varus angulation (windswept deformity).38,39 Depending on the severity, bone defects may be addressed with cement, metal augments or bone graft. In a valgus knee, hypoplasia of the lateral femoral condyle and the possible need for augmentation should be considered.35 The femoral entry point for the intramedullary guide should be planned on both full-limb anteroposterior (AP) and lateral views to avoid mistakes in the amount of angular correction which is achieved. Although it is commonly believed to range between 5° and 7°, different studies have highlighted the extreme variability of this parameter, and particularly in patients with a severe varus/valgus deformity.40,41 Tibial resection in the valgus knee should take into account the extra-articular deformity which may often be present at the diaphyseal level.For this reason, the proximal positioning of the tibial jig is often medial relative to the metaphyseal centre and should be calculated at pre-operative planning.42
Coronal alignment in primary TKA represents an important predictor of the long-term outcome and survivorship.43,44 Karachalios et al45 compared the outcome of 51 knees with a coronal deformity of > 20° with a control group with only a slight deformity. After a minimum follow-up of 5.5 years, there was no difference in the clinical outcome. However, residual coronal malalignment was significantly associated with a poorer outcome and the study group had twice as many poor results as the control group. The authors concluded that consistently good results in severely deformed joints were harder to achieve. Ritter et al30 compared a series of 75 patients with a pre-operative deformity of > 20° with a matched control group treated with a cruciate retaining (CR) TKA, and showed no difference in knee score, alignment or rate of revision. The survival rate of those with a severe deformity at 12 years was 98.8%. In a ten-year follow-up study, Laskin et al29 supported the use of a posterior stabilised (PS) TKA for 50 patients with a coronal deformity of > 15°. In these patients the use of a CR TKA was associated with an increased incidence of pain and revision. Mullaji et al32 described their experience of 173 PS TKAs performed on patients with > 20° of varus deformity. Their technique consisted of a combination of selective soft-tissue medial release and downsizing of the tibial component through a reduction osteotomy of the posteromedial tibial flare. In the presence of a severe extra-articular deformity, a proximal tibial osteotomy was also performed. Three patients had loosening of the tibial component and none had instability at a mean follow-up of 2.6 years. Aglietti et al46 studied the efficacy of a ‘pie-crusting’ technique in 53 patients with a valgus knee who underwent TKA and were followed-up for a minimum of five years. One patient had varus instability in extension, but no revision was reported. Excellent results at long-term follow-up have been reported following the use of a varus-valgus constrained (VVC) TKA for fixed valgus deformities.47 Anderson et al48 recently reviewed 70 primary non-stemmed VVC TKAs for valgus deformity of > 15°. After a mean follow-up of 44.5 months (2 to 6 years) no radiographic loosening or wear was observed.
Genu recurvatum
Arthritic knees with genu recurvatum or hyperextension > 5° may be secondary to various conditions including a congenital lack of distal femoral condylar bone, post-traumatic or post-septic osteoarthritis (OA), limb shortness, rheumatic diseases or after a high tibial osteotomy (HTO) where not infrequently there is a reverse sloping of the tibial plateau. Premature anterior tibial physial closure may also cause recurvatum.49 A quadriceps avoidance gait may cause recurvatum. For instance, patients with chronic patellar pain, a previous patellectomy or obese patients may adopt the stiff legged gait, pushing the knee backwards during walking to avoid an excessive load on the patella, while stretching the posterior capsule and creating a progressive hyperextension. A similar mechanism causes recurvatum in neurological disorders such as poliomyelitis.
A personalised balance between pain, expected function, life expectancy, degree of OA and the risk of complications should determine the decision to undergo TKA.50 Understanding the causes of these deformities is important in order to obtain sufficient stability and to avoid residual pain post-operatively.
Planning TKA in patients with recurvatum should include analysis of gait and clinical and radiographic examination. The pattern of gait is useful to detect a possible leg-length discrepancy and the status of the surrounding joints with special attention to an equinus deformity of the ankle or foot. The degree of recurvatum is assessed and whether it is combined with medial or lateral instability, checking also the reducibility of any valgus or varus deformity and the pre-operative range of movement (ROM).
Besides the coronal alignment, the examination should include patellar tracking, looking for torsional deformity and grading the strength against gravity.
Radiographic analysis will indicate if the bony deformity affects the femur or tibia, especially when recurvatum is associated with valgus alignment and hypoplasia of the lateral femoral condyle. In the sagittal plane, the meta-diaphyseal area of the tibia and femur and the tibial slope and tibial tubercle (TT) are often dysplastic. An extra-articular deformity of the proximal tibia with inversion of the sagittal slope can be managed with tibial resection up to 15°, if the deformity is greater a simultaneous corrective osteotomy of the sagittal deformity should be planned.51 In patients with a neuromuscular disorder, a hinged TKA is recommended. This will require careful planning of the dimension of the extended stems and positioning in the narrow, distorted canals. Meding et al52 reported the results of 57 CR TKAs at a mean follow-up of 4.5 years, performed in patients with a mean pre-operative recurvatum of 11° and a well-functioning extensor mechanism. Their overall results were excellent and only two patients had a recurrent deformity. Mullaji et al49 reported the results of 45 PS TKAs at a mean follow-up of two years performed in patients with a mean pre-operative recurvatum of 11° and a well-functioning extensor mechanism. Their overall results were also excellent with no recurrent deformity. The largest series on TKA in patients with polio, by Jordan et al,8 included 17 TKAs (eight semiconstrained, eight PS, one hinged); at mid-term follow-up, none were loose. Stiffness was reported as a complication in two knees. Giori et al9 from The Mayo clinic described 11 TKAs in patients with polio. Their complication rate was higher with two periprosthetic fractures, one patellar tendon avulsion, four instabilities, and one transient peroneal nerve palsy. Tigani et al53 reported excellent results with the use of rotating hinges in ten TKAs at a mean follow-up of four years. TKA for patients with a hyperextension deformity can therefore achieve results which are similar to those after routine TKA. When the strength of the quadriceps is less than antigravity, results may deteriorate and hinged components become necessary.
Stiff knee
Stiffness of the knee can involve limited flexion or extension, or can be combined. The aetiology can be post-traumatic, septic arthritis or aggressive OA. Impingement owing to osteophytes and soft-tissue contracture is a consequence of progressive joint stiffness.10 Soft-tissue contraction involves the posterior capsule, collateral ligaments and the extensor mechanism. Fixed contractures affect the patient’s ability to walk before generating inflammation and increasing contractures.10,11,54,55 Major flexion contractures may follow the prolonged use of a wheelchair.54 The sequelae of fractures affect both flexion and extension. Septic arthritis affects flexion more than extension causing progressive arthrofibrosis of the suprapatellar pouch and thickening the capsule. Patients with a stiff knee may have many skin incisions relating to previous trauma or surgery.17 These patients require detailed pre-operative counselling underlying all the strategies that will be undertaken after the procedure to address the functional limitation. Appropriate expectations, and possible intra- and post-operative complications should be explained to the patient. The details of the post-operative regime should be outlined including the possible need for braces or ‘drop-out’ casting. For major flexion contractures, the drop-out cast seems to be a better solution because the three-point pressure on the extensor moment is more reliable than with an extension brace.56 Coaching a patient’s relative may often help if a particularly long and difficult recovery is anticipated.
Radiographic examination can be misleading when there is a flexion contracture. AP radiographs should be centred on the obliquity of the tibial plateau. Malrotation of the joint can also affect the coronal measurements on the full-limb radiograph. Magnification of the joint can be greater than normal because the knee is closer to the beam, making pre-operative measurements difficult. Pre-operative exercise to improve flexibility including stretching and sometimes the use of a brace to recover extension, should be used.57 This is particularly important in patients with a soft end point and those in whom the stiffness is of recent onset.57 Bone healing in the meta-diaphyseal femoral area after fractures or osteotomies often produces residual scarring with adhesions of the extensor mechanism to the bone. Intra- and extra-articular sites of scarring should be identified pre-operatively.58 MRI scans of the joint and the thigh can help identify the sites of adhesion and will demonstrate the quality and vitality of the muscle belly of the quadriceps. MR elastography has provided useful information about muscle stiffness in experimental and clinical settings.59
All reports have shown a satisfactory recovery of movement and function with a significant improvement after surgery, even if the outcome is worse than after TKA in flexible knees.10,11,54,55 Complications were significantly higher in this group and patients should be informed of this before surgery. Post-operative stiffness is a major complication, especially in patients with a pre-operative flexion deficit > 50°.10,11,54,55 The possible need for manipulation under anaesthesia after surgery should be described to these patients. Berend et al10 reported the results of 52 knees with a fixed flexion contracture of ≥ 20°. Full correction was achieved intra-operatively. In total, 94% of TKAs had a residual contracture of < 10° at mid-term. One was revised for instability. Montgomery et al54 reported the results of 82 stiff knees (ROM < 50°) at mid-term. Full correction was achieved intra-operatively. The mean ROM at follow-up was 93°. Two patients had a transient peroneal nerve palsy and two had recurrent knee stiffness. Rajgopal et al55 reviewed 84 TKAs, with OA and severe stiffness pre-operatively (mean ROM was 14°; 0° to 20°) at a mean follow-up of nine years. The mean ROM at final follow-up was 75°. McAuley et al11 reported a high complication rate of 41% with a rate of revision of 18% at six years in a series of 21 patients (27 TKAs) with a stiff knee who underwent TKA. Three of the revisions involved loosening for failure of cementless components fixation. In another two cases, revision was necessary because of extensive osteolysis, progressive stiffness and pain.
The significance of these studies is that patients with limited ROM pre-operatively can have an improved quality of life after TKA, reflected by an increased walking tolerance, increased function, and decreased pain, but in association with a high risk of complications and subsequent revision.
Extra-articular deformities
Proper alignment helps to balance the forces across the knee that are usually responsible for the failure of arthroplasty.60 Extra-articular deformities are located beyond the attachment of the collateral ligaments, thereby involving the femur proximal to the epicondyles or the tibia distal to the tip of the fibula.60 Such deformities may have either a genetic, a developmental (osteogenesis imperfecta, skeletal dysplasia, Paget’s disease, osteopetrosis), a metabolic (rickets), an iatrogenic (overcorrection or undercorrection of a previous HTO or distal femoral osteotomy (DFO)), or a traumatic (malunion) origin.
These extra-articular deformities can be uni-, bi-, or tri-planar, depending on whether they are an isolated or a combined deformity in the coronal (varus-valgus), sagittal (flexion-extension), or transverse (rotational) plane and on whether they are associated with intra-articular instability.61
Little information is available about the best approach for performing TKA under these circumstances. The primary goal remains a well-aligned and stable TKA without pain and with a good ROM. In order to correct extra-articular deformities, surgeons can choose to operate either inside or outside the knee joint or both (Fig. 3).
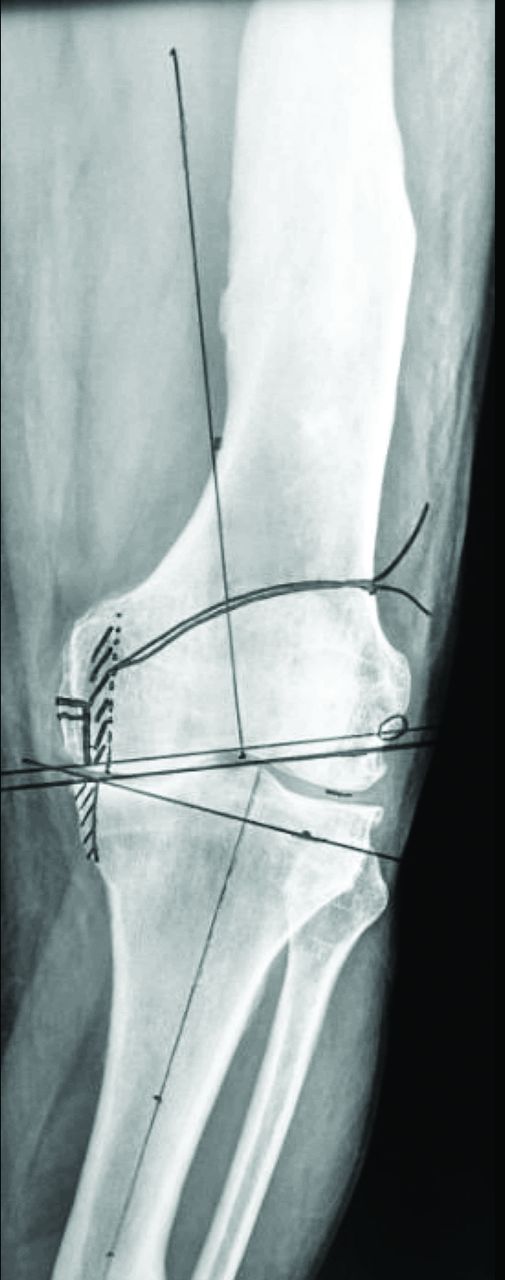
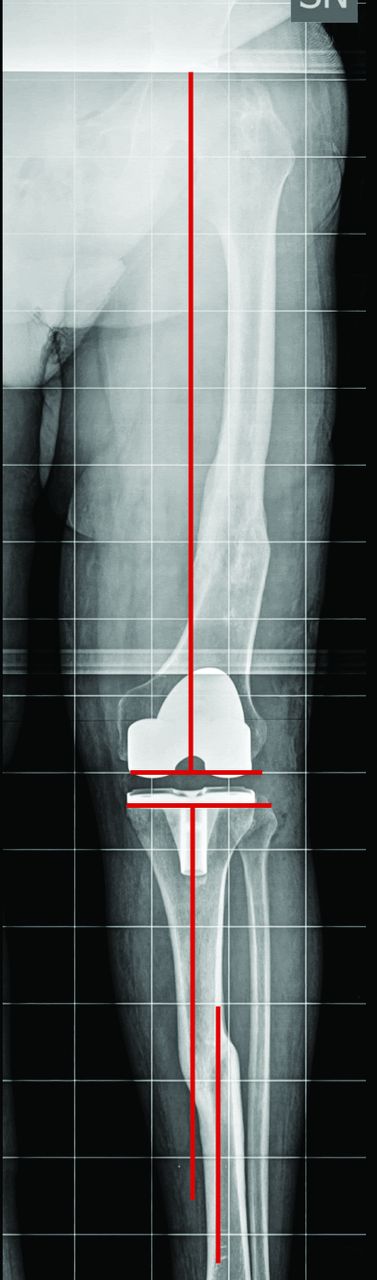

Figs. 3a - 3d
Radiographs showing a) severe varus knee with extra-articular deformities of the femur and tibia after fracture malunions; b) anteroposterior (AP) view of the pre-operative plan of the femoral and tibial resections. Planning of medial tibial bone resection and epicondylar osteotomy is shown; c) post-operative AP long-film with correction of the malalignment with a posterior-stabilised total knee arthroplasty. The ligamentous balance has been achieved with subperiosteal release of the deep medial collateral ligament (MCL) and semimembranosus, release of the posterior fibres of the superficial MCL and fine tuning the final balance with needle puncturing (16G needle) of the deep and superficial MCL; and d) post-operative lateral view of the knee. EA def, extra-articular deformity.
A severely deformed knee may be managed by following six pre-operative considerations: to quantify and locate the deformity; to establish whether the correction will take place within or outside the joint; to consider that intra-articular correction, alone or in combination with osteotomy, requires less bony procedures, but larger soft-tissue release to balance the gaps; to consider that extra-articular deformity may require concomitant osteotomy and to decide the method of fixation (plate, intramedullary nail); to consider the role of newer techniques such as computer-assisted surgery and personalised instrumentation.
The exact site of deformity, the degree of angulation, and the most appropriate surgical approach to correct it are identified pre-operatively from the radiographs by assessment of the axis and degree of the deformity. How to correct the axial alignment and how to balance the gaps is planned, as well as how to stabilise the joint. Finally, the type of prosthesis is chosen.
A major breakthrough in determining the type of deformity was made by Dror Paley, who defined the site of deformities with the concept of the centre of rotation of angulation.62 Surgeons now identify the apex of angulation, or the centre of deformity in order to understand and to plan surgery for any type of deformity of the leg. Wolff et al60 showed trigonometrically that the closer the deformity is to the knee, the greater its importance. This should not, however, distract our attention from the mechanical axis. Deformities cannot be ignored simply because they are distant from the knee joint. The extent to which the limb deviates from the neutral mechanical axis must be assessed. Full-length weight-bearing radiographs are required to show enough of the medullary canal to evaluate the mechanical and anatomical axes and to perform conventional navigation anticipating the ideal bone resections. Extramedullary guide systems and navigation systems or patient-specific instruments may all be used when performing the DFO if the deformity is in the mid-third of the femur, or when an intramedullary rod fails to pass through the angular deformity.63-65 When planning the distal femoral and tibial resection, it is necessary to decide whether it is possible to preserve the insertions of the collateral ligaments, and whether a corrective osteotomy is required. For the knee with an extra-articular deformity of the tibia, the surgeon must determine whether the anatomical axis of the distal fragment passes within the plateau, thereby limiting the correction to an intra-articular resection.
An evaluation of deformity in the sagittal plane of the femur or tibia is also mandatory. Although minor sagittal deformities may be compensated for, a deviation of > 15° needs to be corrected with an osteotomy.51 Supracondylar distal femoral fractures are typically associated with a varus deformity of the fragment and internal rotation because of traction of the adductor muscles. When an axial deformity is suspected, a pre-operative CT scan will help to define the rotation of the posterior femoral condyles relative to the femoral neck. In general, rotatory malunions that are located beyond the attachments of collateral ligaments should not be corrected by changing the rotation of either the femoral or tibial component.66 A semiconstrained option should be available for these patients which usually require an extensive ligamentous release.
So far, the literature on intra-articular versus extra-articular correction is almost entirely limited to a few case series and most of these studies report the long-term results of intra-articular correction only.61,67 Promising results of TKA in combination with intra-articular resection and soft-tissue balancing have been obtained in patients with OA of the knee associated with an extra-articular deformity of < 20° in the coronal plane in the femur and tibia.60,61,64 These results have also been confirmed in those with deformities in the sagittal plane.67,68 These studies indicate that intra-articular resection of bone combined with TKA is feasible in patients with OA and can accommodate up to 15° of recurvatum and 16° of procurvatum of the femur in addition to varus deformities.51,68 Recently, computer-assisted navigation systems and patient-specific instrumentation have been used as an alternative approach to TKA in patients with extra-articular deformity.13,65,69 So far, the largest series with 34 patients has been published by Mullaji et al.13 The results of TKA combined with an osteotomy have been reported by Lonner et al.12 In this study 11 patients with a mean varus deformity of 25° underwent combined surgery, with good overall results. There were two major complications: one pulmonary embolism and one nonunion. Radke and Radke69 performed a single-stage closing wedge tibial osteotomy in ten patients undergoing TKA with a mean extra-articular varus or valgus deformity of 20°. The mean Knee Society score for these patients improved from 28 points pre-operatively to 81 points at a mean follow-up of 2.5 years (1 to 4) after the operation. There was one delayed union and one nonunion.
Post-osteotomy (tibial and femoral)
Distal femoral and high tibial osteotomies create extra-articular deformities of varying degrees close to the knee joint. Although large extra-articular deformities may require simultaneous or staged osteotomies to restore the mechanical alignment at the time of TKA, in most patients undergoing TKA after an osteotomy, proper alignment and stability can be obtained with routine bone cuts and soft-tissue balancing alone.70
Previous skin incisions after osteotomy usually do not present an issue. Tibial incisions, if transverse, can be safely crossed, and if medial longitudinal are not at risk with a new parallel lateral incision.71 Lateral tibial incisions are usually an inverted ‘J’ and can be incorporated partly in the new one. If the patient has adhesions or dystrophic areas, removal of hardware should be staged in order to anticipate wound-healing problems before the TKA. A lateral plate after DFO can be removed through a long midline incision and a standard medial parapatellar approach if the extensor mechanism has sufficient flexibility.
When planning a TKA after a previous osteotomy, variations of the normal anatomy related to the previous surgery must be taken into account. After a closing wedge HTO, there is lateral inclination of the articular line with a higher medial than lateral plateau.72 Lateral tibial bone deficiency may require the use of augmentations or grafting, and this should be anticipated by radiographic analysis. Stem extensions are often used after osteotomy to bypass the weakened tibial metaphysis. Proximal tibial meta-diaphyseal mismatch after a closing wedge HTO should be identified in order to predict possible cortical contact with the tibial stem and the need for an offset. The tibial slope after HTO may be neutral, or even inverted. Calculation of the amount of resection of the posterior tibia with an inverted slope should be undertaken on the sagittal radiograph. After varus DFO, the femoral anatomical axis usually intersects the lateral femoral condyle instead of the intercondylar notch. Therefore, when an intramedullary guide is used, the entry point should be planned where the femoral anatomical axis intersects the distal aspect of the femur at the knee. We also suggest an extramedullary intra-operative check of alignment with localisation of the femoral head before the distal femoral cut in order to obtain proper coronal alignment.58 The patellar height should be evaluated because patella baja is common after HTO and this may affect the surgical approach.
Conflicting results have been reported concerning the clinical outcome and survivorship of TKA carried out after previous femoral or tibial osteotomies.14,58,70,73,74 Some authors report poorer results,14,58 while others report comparable results in patients with and without a previous osteotomy.70,73 Parvizi et al14 studied the outcome after TKA following a HTO in 115 patients at a mean follow-up of 15.1 years. They showed that the overall functional and radiographic outcomes were slightly inferior, owing to higher rates of malalignment, instability, radiolucent lines and revision. Following opening-wedge HTO, Erak et al74 found inferior results after subsequent TKA because of persistent pain and a slightly lower clinical score. A systematic review by van Raaij et al15 pooled the results of eight randomised controlled trials. They did not find statistically significant differences between those undergoing primary TKA and those undergoing TKA after a HTO. They reported, however, that each paper outlined the increased surgical difficulties represented by the exposure, ligamentous balancing, and longer duration on the procedure in the latter group.
Neglected patellar dislocation
Chronic lateral dislocation of the patella is uncommon and usually congenital. Acquired recurrent dislocations have been reported secondary to trauma.75 In most patients, the chronic dislocation is irreducible. Deformities such as genu valgum and external tibial torsion with OA are commonly associated with this condition.75 Chronic dislocations can be neglected because of functional adaptations. A valgus knee and external rotation with tight lateral structures allows the MCL to stabilise the joint in extension during walking, compensating for the weak quadriceps tendon. Diagnosis is often late and mainly related to degenerative changes in the tibio-femoral joint. Some patients have a history of recurrent dislocation of the patella with a number of failed procedures in an attempt to re-align it. The significant symptoms are pain, instability and difficulty on stairs. Patients with OA and chronic dislocation of the patella require TKA in order to regain a biomechanically valid extensor mechanism.
It is important to establish on examination whether the patello-femoral and femoro-tibial deformities are fixed or reducible, and the state of the ligaments. Radiographic examination includes full-limb weight-bearing films with axial patellar views and CT scans. In order to anticipate the need for a distal re-alignment procedure combined with TKA, it is helpful to evaluate the TT-trochlear groove (TG) distance. This distance reflects the lateral deviation of the TT in relationship to the TG.76 An increased distance (> 20 mm) is common in patients with a dislocated patella.77 The most common scenario which combines valgus deformity, a dislocated patella and increased TT-TG, may require a lateral surgical approach with or without a combined TTO to address the tri-planar deformity, avoiding devascularisation of the extensor mechanism. This approach is recommended even in patients with a pre-existing anterolateral skin incision.
TKA in patients with chronic dislocation of patella has been reported infrequently. The larger series by Hau et al described 15 TKAs.16 The preferred surgical treatment was an isolated patellofemoral joint arthroplasty or a TKA through a lateral parapatellar approach. Three TTOs were performed. A proximal re-alignment with vastus medialis advancement and lateral patellar retinacular release was performed in all medial parapatellar approaches. At a mean follow-up of 29 months (18 to 120) the authors described complications in four knees. Two patients had recurrent instability treated with subsequent vastus medialis obliquus advancement and TTO. One patient had pain and instability managed with a liner exchange and lateral retinacular release, and one had stiffness that required a manipulation under anaesthesia.
Several authors, in case reports or small series, recommend a proximal re-alignment procedure with an additional extensive lateral release at the time of TKA.75,78-80 Most do not favour TTO when possible. Bullek et al75 described five patients with chronic dislocation of the patella and OA, genu valgum, fixed flexion, and an external rotation deformity with a satisfactory outcome at a mean follow-up of 40 months. Restoration of axial alignment was achieved using constrained components and re-aligning the patella with an extensive proximal re-alignment and medialising the patellar button.
1 Font-Rodriguez DE , ScuderiGR, InsallJN. Survivorship of cemented total knee arthroplasty. Clin Orthop Relat Res1997;345:79–86.PubMed Google Scholar
2 Meftah M , RanawatAS, RanawatCS. Ten-year follow-up of a rotating-platform, posterior-stabilized total knee arthroplasty. J Bone Joint Surg [Am]2012;94-A:426–432.CrossrefPubMed Google Scholar
3 Meding JB , MedingLK, RitterMA, KeatingEM. Pain relief and functional improvement remain 20 years after knee arthroplasty. Clin Orthop Relat Res2012;470:144–149.CrossrefPubMed Google Scholar
4 Pavone V , BoettnerF, FickertS, SculcoTP. Total condylar knee arthroplasty: a long-term followup. Clin Orthop Relat Res2001;388:18–25.CrossrefPubMed Google Scholar
5 Scott CE , DavidsonE, MacDonaldDJ, WhiteTO, KeatingJF. Total knee arthroplasty following tibial plateau fracture: a matched cohort study. Bone Joint J2015;97-B:532–538.CrossrefPubMed Google Scholar
6 Lizaur-Utrilla A , Collados-MaestreI, Miralles-MuñozFA, Lopez-PratsFA. Total Knee Arthroplasty for Osteoarthritis Secondary to Fracture of the Tibial Plateau. A Prospective Matched Cohort Study. J Arthroplasty2015;30:1328–1332.CrossrefPubMed Google Scholar
7 Weiss NG , ParviziJ, TrousdaleRT, BryceRD, LewallenDG. Total knee arthroplasty in patients with a prior fracture of the tibial plateau. J Bone Joint Surg [Am]2003;85-A:218–221.CrossrefPubMed Google Scholar
8 Jordan L , KligmanM, SculcoTP. Total knee arthroplasty in patients with poliomyelitis. J Arthroplasty2007;22:543–548.CrossrefPubMed Google Scholar
9 Giori NJ , LewallenDG. Total knee arthroplasty in limbs affected by poliomyelitis. J Bone Joint Surg [Am]2002;84-A:1157–1161.CrossrefPubMed Google Scholar
10 Berend KR , LombardiAV Jr, AdamsJB. Total knee arthroplasty in patients with greater than 20 degrees flexion contracture. Clin Orthop Relat Res2006;452:83–87.CrossrefPubMed Google Scholar
11 McAuley JP , HarrerMF, AmmeenD, EnghGA. Outcome of knee arthroplasty in patients with poor preoperative range of motion. Clin Orthop Relat Res2002;404:203–207.CrossrefPubMed Google Scholar
12 Lonner JH , SiliskiJM, LotkePA. Simultaneous femoral osteotomy and total knee arthroplasty for treatment of osteoarthritis associated with severe extra-articular deformity. J Bone Joint Surg [Am]2000;82-A:342–348.CrossrefPubMed Google Scholar
13 Mullaji A , ShettyGM. Computer-assisted total knee arthroplasty for arthritis with extra-articular deformity. J Arthroplasty2009;24:1164–1169.CrossrefPubMed Google Scholar
14 Parvizi J , HanssenAD, SpangehlMJ. Total knee arthroplasty following proximal tibial osteotomy: risk factors for failure. J Bone Joint Surg [Am]2004;86-A:474–479.CrossrefPubMed Google Scholar
15 van Raaij TM , ReijmanM, FurlanAD, VerhaarJA. Total knee arthroplasty after high tibial osteotomy. A systematic review. BMC Musculoskelet Disord2009;10:88.CrossrefPubMed Google Scholar
16 Hau RC , NewmanJH. Knee replacement for osteoarthritis secondary to chronic patellar dislocation and trochlear dysplasia. Knee2008;15:447–450.CrossrefPubMed Google Scholar
17 Vince KG , AbdeenA. Wound problems in total knee arthroplasty. Clin Orthop Relat Res2006;452:88–90.CrossrefPubMed Google Scholar
18 Møller AM , VillebroN, PedersenT, TønnesenH. Effect of preoperative smoking intervention on postoperative complications: a randomised clinical trial. Lancet2002;359:114–117.CrossrefPubMed Google Scholar
19 Patel VP , WalshM, SehgalB, et al.Factors associated with prolonged wound drainage after primary total hip and knee arthroplasty. J Bone Joint Surg [Am]2007;89-A:33–38.CrossrefPubMed Google Scholar
20 Jones RE , RussellRD, HuoMH. Wound healing in total joint replacement. Bone Joint J2013;95-B (suppl A):144–147.CrossrefPubMed Google Scholar
21 Namba RS , InacioMC, PaxtonEW. Risk factors associated with deep surgical site infections after primary total knee arthroplasty: an analysis of 56,216 knees. J Bone Joint Surg [Am]2013;95-A:775–782.CrossrefPubMed Google Scholar
22 Dennis DA , BerryDJ, EnghG, et al.Revision total knee arthroplasty. J Am Acad Orthop Surg2008;16:442–454.PubMed Google Scholar
23 Gooding CR , GarbuzDS, MasriBA. Extensile surgical exposures for revision total knee replacement. In: Scott WN, ed. Insall & Scott Surgery of the knee . Philadelphia: Elsevier Inc., 2012:1320–1326. Google Scholar
24 Howard JL , AgelJ, BareiDP, BenirschkeSK, NorkSE. A prospective study evaluating incision placement and wound healing for tibial plafond fractures. J Orthop Trauma2008;22:299–305.CrossrefPubMed Google Scholar
25 Casey WJ III , RebeccaAM, KrochmalDJ, et al.Prophylactic flap reconstruction of the knee prior to total knee arthroplasty in high-risk patients. Ann Plast Surg2011;66:381–387.CrossrefPubMed Google Scholar
26 Pontén B . The fasciocutaneous flap: its use in soft tissue defects of the lower leg. Br J Plast Surg1981;34:215–220.CrossrefPubMed Google Scholar
27 Judet R . Mobilisation of the stiff knee. J Bone Joint Surg [Br]1959;41-B:856–857. Google Scholar
28 Saleh KJ , ShermanP, KatkinP, et al.Total knee arthroplasty after open reduction and internal fixation of fractures of the tibial plateau: a minimum five-year follow-up study. J Bone Joint Surg Am2001;83-A:1144–1148.CrossrefPubMed Google Scholar
29 Laskin RS . The Insall Award. Total knee replacement with posterior cruciate ligament retention in patients with a fixed varus deformity. Clin Orthop Relat Res1996;331:29–34.CrossrefPubMed Google Scholar
30 Ritter MA , FarisGW, FarisPM, DavisKE. Total knee arthroplasty in patients with angular varus or valgus deformities of > or = 20 degrees. J Arthroplasty2004;19:862–866. Google Scholar
31 Ranawat AS , RanawatCS, ElkusM, et al.Total knee arthroplasty for severe valgus deformity. J Bone Joint Surg [Am]2005;87-A(Pt 2) (suppl 1):271–284.CrossrefPubMed Google Scholar
32 Mullaji AB , PadmanabhanV, JindalG. Total knee arthroplasty for profound varus deformity: technique and radiological results in 173 knees with varus of more than 20 degrees. J Arthroplasty2005;20:550–561.CrossrefPubMed Google Scholar
33 De Muylder J , VictorJ, CornuO, KaminskiL, ThienpontE. Total knee arthroplasty in patients with substantial deformities using primary knee components. Knee Surg Sports Traumatol Arthrosc 2014. (Epub ahead of print) PMID: 25246172.CrossrefPubMed Google Scholar
34 Mullaji A , MarawarS, SharmaA. Correcting varus deformity. J Arthroplasty2007;22 (suppl 1):15–19.CrossrefPubMed Google Scholar
35 Baldini A Correction of fixed deformities with total knee arthroplasty. In: Scott WN, ed. Surgery of the knee. Fifth ed. Philadelphia: Churchill Livingstone, 2011:1100–1107. Google Scholar
36 Koninckx A , SchwabPE, DeltourA, ThienpontE. The minimally invasive far medial subvastus approach for total knee arthroplasty in valgus knees. Knee Surg Sports Traumatol Arthrosc2014;22:1765–1770.CrossrefPubMed Google Scholar
37 Bae DK , SongSJ, YoonKH, ShinSM. The position of the tibial component affecting the postoperative mechanical axis in total knee arthroplasty. J Arthroplasty2010;25:1131–1136.CrossrefPubMed Google Scholar
38 Baldini A , TraversoFTips and pearls in primary total knee arthroplasty. In: Rossi R, Bruzzone M, eds. Soft tissue balancing in primary total knee arthroplasty. Torino: Edizioni Minerva Medica, 2012:13–23. Google Scholar
39 Meding JB , AndersonAR, RitterMA, FarisPM, KeatingEM. Windswept deformity in bilateral total knee arthroplasty. J Arthroplasty2000;15:562–566.CrossrefPubMed Google Scholar
40 Mullaji AB , ShettyGM, KannaR, VadapalliRC. The influence of preoperative deformity on valgus correction angle: an analysis of 503 total knee arthroplasties. J Arthroplasty2013;28:20–27.CrossrefPubMed Google Scholar
41 Shi X , LiH, ZhouZ, et al.Individual valgus correction angle improves accuracy of postoperative limb alignment restoration after total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc2015. (Epub ahead of print) PMID: 25552406.CrossrefPubMed Google Scholar
42 Alghamdi A , RahméM, LavigneM, MasséV, VendittoliPA. Tibia valga morphology in osteoarthritic knees: importance of preoperative full limb radiographs in total knee arthroplasty. J Arthroplasty2014;29:1671–1676.CrossrefPubMed Google Scholar
43 Gioe TJ , KilleenKK, GrimmK, MehleS, ScheltemaK. Why are total knee replacements revised?: analysis of early revision in a community knee implant registry. Clin Orthop Relat Res2004;428:100–106.PubMed Google Scholar
44 Sharkey PF , LichsteinPM, ShenC, TokarskiAT, ParviziJ. Why are total knee arthroplasties failing today--has anything changed after 10 years?J Arthroplasty2014;29:1774–1778.CrossrefPubMed Google Scholar
45 Karachalios T , SarangiPP, NewmanJH. Severe varus and valgus deformities treated by total knee arthroplasty. J Bone Joint Surg [Br]1994;76-B:938–942.PubMed Google Scholar
46 Aglietti P , LupD, CuomoP, BaldiniA, De LucaL. Total knee arthroplasty using a pie-crusting technique for valgus deformity. Clin Orthop Relat Res2007;464:73–77.CrossrefPubMed Google Scholar
47 Easley ME , InsallJN, ScuderiGR, BullekDD. Primary constrained condylar knee arthroplasty for the arthritic valgus knee. Clin Orthop Relat Res2000;380:58–64.CrossrefPubMed Google Scholar
48 Anderson JA , BaldiniA, MacDonaldJH, PellicciPM, SculcoTP. Primary constrained condylar knee arthroplasty without stem extensions for the valgus knee. Clin Orthop Relat Res2006;442:199–203.CrossrefPubMed Google Scholar
49 Mullaji A , LingarajuAP, ShettyGM. Computer-assisted total knee replacement in patients with arthritis and a recurvatum deformity. J Bone Joint Surg [Br]2012;94-B:642–647.CrossrefPubMed Google Scholar
50 Vince KG . Diagnosis and management of patients with instability of the knee. Instr Course Lect2012;61:515–524.PubMed Google Scholar
51 Wang JW , ChenWS, LinPC, HsuCS, WangCJ. Total knee replacement with intra-articular resection of bone after malunion of a femoral fracture: can sagittal angulation be corrected?J Bone Joint Surg [Br]2010;92-B:1392–1396.CrossrefPubMed Google Scholar
52 Meding JB , KeatingEM, RitterMA, FarisPM, BerendME. Total knee replacement in patients with genu recurvatum. Clin Orthop Relat Res2001;393:244–249.CrossrefPubMed Google Scholar
53 Tigani D , FoscoM, AmendolaL, BorianiL. Total knee arthroplasty in patients with poliomyelitis. Knee2009;16:501–506.CrossrefPubMed Google Scholar
54 Montgomery WH III , InsallJN, HaasSB, BeckerMS, WindsorRE. Primary total knee arthroplasty in stiff and ankylosed knees. Am J Knee Surg1998;11:20–23.PubMed Google Scholar
55 Rajgopal A , AhujaN, DolaiB. Total knee arthroplasty in stiff and ankylosed knees. J Arthroplasty2005;20:585–590.CrossrefPubMed Google Scholar
56 Logerstedt D , SennettBJ. Case series utilizing drop-out casting for the treatment of knee joint extension motion loss following anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther2007;37:404–411.CrossrefPubMed Google Scholar
57 Ulrich SD , BhaveA, MarkerDR, SeylerTM, MontMA. Focused rehabilitation treatment of poorly functioning total knee arthroplasties. Clin Orthop Relat Res2007;464:138–145.PubMed Google Scholar
58 Nelson CL , SalehKJ, KassimRA, et al.Total knee arthroplasty after varus osteotomy of the distal part of the femur. J Bone Joint Surg [Am]2003;85-A:1062–1065.CrossrefPubMed Google Scholar
59 Dresner MA , RoseGH, RossmanPJ, et al.Magnetic resonance elastography of skeletal muscle. J Magn Reson Imaging2001;13:269–276.CrossrefPubMed Google Scholar
60 Wolf AM , HungerfordDS, PepeCL. The effect of extra-articular varus and valgus deformity on total knee arthroplasty. Clin Orthop Relat Res1991;271:135–151. Google Scholar
61 Wang JW , WangCJ. Total knee arthroplasty for arthritis of the knee with extra-articular deformity. J Bone Joint Surg [Am]2002;84-A:1769–1774.CrossrefPubMed Google Scholar
62 Paley D , HerzenbergJE, TetsworthK, McKieJ, BhaveA. Deformity planning for frontal and sagittal plane corrective osteotomies. Orthop Clin North Am1994;25:425–465.PubMed Google Scholar
63 Baldini A , AdravantiP. Less invasive TKA: extramedullary femoral reference without navigation. Clin Orthop Relat Res2008;466:2694–2700.CrossrefPubMed Google Scholar
64 Catani F , DigennaroV, EnsiniA, LeardiniA, GianniniS. Navigation-assisted total knee arthroplasty in knees with osteoarthritis due to extra-articular deformity. Knee Surg Sports Traumatol Arthrosc2012;20:546–551.CrossrefPubMed Google Scholar
65 Thienpont E , PaternostreF, PietschM, HafezM, HowellS. Total knee arthroplasty with patient-specific instruments improves function and restores limb alignment in patients with extra-articular deformity. Knee2013;20:407–411.CrossrefPubMed Google Scholar
66 Berger RA , RubashHE, SeelMJ, ThompsonWH, CrossettLS. Determining the rotational alignment of the femoral component in total knee arthroplasty using the epicondylar axis. Clin Orthop Relat Res1993;286:40–47.PubMed Google Scholar
67 Mann JW , InsallJN, ScuderiGR. Total knee arthroplasty in patients with associated extra-articular deformity. Orthop Trans1997;21:59. Google Scholar
68 Kim KI , RamtekeAA, BaeDK. Navigation-assisted minimal invasive total knee arthroplasty in patients with extra-articular femoral deformity. J Arthroplasty2010;25:658–617.CrossrefPubMed Google Scholar
69 Radke S , RadkeJ. Total knee arthroplasty in combination with a one-stage tibial osteotomy: a technique for correction of a gonarthrosis with a severe (> 15 degrees) tibial extra-articular deformity. J Arthroplasty2002;17:533–537. Google Scholar
70 Kosashvili Y , GrossAE, ZywielMG, et al.Total knee arthroplasty after failed distal femoral varus osteotomy using selectively stemmed posterior stabilized components. J Arthroplasty2011;26:738–743.CrossrefPubMed Google Scholar
71 Cerciello S , VassoM, MaffulliN, et al.Total knee arthroplasty after high tibial osteotomy. Orthopedics2014;37:191–198.CrossrefPubMed Google Scholar
72 Amendola L , FoscoM, CenniE, TiganiD. Knee joint arthroplasty after tibial osteotomy. Int Orthop2010;34:289–295.CrossrefPubMed Google Scholar
73 Meding JB , WingJT, RitterMA. Does high tibial osteotomy affect the success or survival of a total knee replacement?Clin Orthop Relat Res2011;469:1991–1994.CrossrefPubMed Google Scholar
74 Erak S , NaudieD, MacDonaldSJ, et al.Total knee arthroplasty following medial opening wedge tibial osteotomy: technical issues early clinical radiological results. Knee2011;18:499–504.CrossrefPubMed Google Scholar
75 Bullek DD , ScuderiGR, InsallJN. Management of the chronic irreducible patellar dislocation in total knee arthroplasty. J Arthroplasty1996;11:339–345.CrossrefPubMed Google Scholar
76 Goutallier D , BernageauJ, LecudonnecB. The measurement of the tibial tuberosity. Patella groove distanced technique and results (author’s transl). Rev Chir Orthop Reparatrice Appar Mot1978;64:423–428. (In French). Google Scholar
77 Dejour H , WalchG, Nove-JosserandL, GuierC. Factors of patellar instability: an anatomic radiographic study. Knee Surg Sports Traumatol Arthrosc1994;2:19–26.CrossrefPubMed Google Scholar
78 Marmor L . Total knee arthroplasty in a patient with congenital dislocation of the patella. Case report. Clin Orthop Relat Res1988;226:129–133.PubMed Google Scholar
79 Hudson J , ReddyVR, KriklerSJ. Total knee arthroplasty for neglected permanent post-traumatic patellar dislocation--case report. Knee2003;10:207–212.CrossrefPubMed Google Scholar
80 Bergquist PE , BaumannPA, FinnHA. Total knee arthroplasty in an adult with congenital dislocation of the patella. J Arthroplasty2001;16:384–388.CrossrefPubMed Google Scholar
This is an open-access article distributed under the terms of the Creative Commons Attributions licence CC-BY-NC, which permits unrestricted use, distribution, and reproduction in any medium, but not for commercial gain, provided the original author and source are credited.
Author contributions:
A. Baldini: Wrote part of the paper, edited the manuscript, addressed the review.
L. Castellani: Wrote part of the paper.
F. Traverso: Writing part of the paper.
A. Balatri: Wrote part of the paper.
G. Balato: Wrote part of the paper, took care of the references style and order addressed the review.
V. Franceschini: Wrote part of the paper, took care of the references style and order addressed the review.
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
This article was primary edited by J. Scott.









