Abstract
Arthroplasty registries are important for the surveillance of joint replacements and the evaluation of outcome. Independent validation of registry data ensures high quality. The ability for orthopaedic implant retrieval centres to validate registry data is not known. We analysed data from the National Joint Registry for England, Wales and Northern Ireland (NJR) for primary metal-on-metal hip arthroplasties performed between 2003 and 2013. Records were linked to the London Implant Retrieval Centre (RC) for validation. A total of 67 045 procedures on the NJR and 782 revised pairs of components from the RC were included. We were able to link 476 procedures (60.9%) recorded with the RC to the NJR successfully. However, 306 procedures (39.1%) could not be linked. The outcome recorded by the NJR (as either revised, unrevised or death) for a primary procedure was incorrect in 79 linked cases (16.6%). The rate of registry-retrieval linkage and correct assignment of outcome code improved over time. The rates of error for component reference numbers on the NJR were as follows: femoral head category number 14/229 (5.0%); femoral head batch number 13/232 (5.3%); acetabular component category number 2/293 (0.7%) and acetabular component batch number 24/347 (6.5%).
Registry-retrieval linkage provided a novel means for the validation of data, particularly for component fields. This study suggests that NJR reports may underestimate rates of revision for many types of metal-on-metal hip replacement. This is topical given the increasing scope for NJR data. We recommend a system for continuous independent evaluation of the quality and validity of NJR data.
Cite this article: Bone Joint J 2015;97-B:10–18.
The National Joint Registry (NJR) for England, Wales and Northern Ireland is the largest arthroplasty register in the world, with 1.6 million records.1 It was created in 2003 to identify individual patients in the event of an implant with a high failure rate.2 The Consultant Outcomes Publication (COP) in orthopaedic surgery is dependent on NJR data.3 This follows a National Clinical Audit commissioned by the Healthcare Quality Improvement Partnership (HQIP) as part of ‘Everyone Counts: Offer 2’.4 As from October 2014, the NJR will publish surgeon activity, 90-day risk-adjusted mortality and the rating of implants used for elective hip operations according to the system of the Orthopaedic Data Evaluation Panel (ODEP).3,5
With this increased scope for publication of NJR data, there is a need for independent validation of their dataset. Orthopaedic implant retrieval centres provide an opportunity for this. These are voluntary repositories where surgeons who undertake revision procedures can send failed components and allied clinical data for detailed analysis. Their primary aim is to determine the mechanism of failure,6 rather than to develop an epidemiological understanding.
The purpose of this study was to link NJR records with information about explanted components held by the London Implant Retrieval Centre (RC) using these data to validate primary metal-on-metal hip procedures recorded in the NJR from its inception on 1 April 2003 until 5November 2013.
Patients and Methods
The aims of this study were to demonstrate a methodology for the retrieval and linkage of data from the registry and to perform independent validation and quality assessment of data relating to the records of primary procedures in the NJR. We performed a cross-sectional survey of the databases of the NJR and the London Implant RC on 5 November 2013. The study had ethical approval.
A total of 67 045 primary metal-on-metal hip procedures associated with a ten-digit NHS number7 were identified from the NJR database and 929 explanted pairs of components from the RC. Procedures performed outside the geographic area or temporal remit of the NJR or missing key fields to confirm linkage were excluded. NJR recording of primary hip arthroplasties for England and Wales commenced on 1 April 2003 and Northern Ireland joined the registry on 1 February 2013.1
Linkage of NJR and RC records was performed using the NHS number and confirmed with a manual check of the patient’s name. Discrepancies were investigated using NHS Spine, which is a collection of national applications that support exchange of information across the NHS.8 Errors on the RC database were corrected at this stage using NHS Spine and/or direct liaison with the referring hospital or patient.
Linkage of the procedure was performed for patients using an exact match for the date of the operation and confirmed by manual checks of the manufacturer, type of implant, side, the size and reference number of the components and the name fields of the hospital. An exact match on four fields was required for linkage. This process was repeated to increase the number of linked records, by relaxing date constraints to +/- 12 months and including records with missing date field entries.
Linkage of the fields was achieved by identifying those which were to be paired between the two databases. RC fields were recoded to correspond with NJR codes where required (Table I).
Table I
Fields for validation
| Field name | Variable type | Comment |
|---|---|---|
| NHS number | Primary key | Unique ten-digit United Kingdom National Health Service identifier |
| First name | String | - |
| Surname | String | - |
| Date of birth | Continuous | Male or female |
| Gender | Dichotomous | - |
| Age at primary (yrs) | Continuous | - |
| Primary operation date | Continuous | - |
| Primary surgical unit description | Categorical | RC field recoded to NJR |
| Acetabular component brand | Categorical | RC field recoded to NJR |
| Acetabular component ODEP rating | Categorical | 10A, 7A, 7B, 5A, 5B, 3A, discontinued, pre-entry or unclassified |
| Component type | Dichotomous | ‘Resurfacing’ or ‘Modular’ |
| Acetabular component size /mm | Discrete | -NJR field recoded from manufacturer guides to provide outer diameter |
| -RC field from etching on component | ||
| Head size (mm) | Dichotomous | Etched on component. |
| Implant side | Dichotomous | Left or right |
| Head cat number | Categorical | -Category number indicating model of head component |
| -Referenced in manufacturer guide | ||
| -Etched on component | ||
| Head batch number | Categorical | -Batch numbers indicating time of component production |
| -Free-text field on NJR | ||
| -Etched on component | ||
| Acetabular component cat number | Categorical | -Category numbers indicating model of acetabular component |
| -Referenced in manufacturer guide | ||
| -Etched on component | ||
| Acetabular component batch number | Categorical | -Batch numbers indicating time of component production |
| -Free-text field on NJR | ||
| -Etched on component | ||
| NJR outcome code | Categorical | Revised, unrevised or died |
-
Description of field-level linkage between NJR and RC datasets. Component fields were completed at the RC from etching markings on the component NJR, National Joint Registry for England, Wales and Northern Ireland; RC, Retrieval Centre; ODEP, Orthopaedic Device Evaluation Panel
Statistical analysis and validation of data
Completeness, existence and accuracy checks on NJR and RC data fields were performed using SPSS Statistics version 22.0 (IBM, Armonk, New York) with common commands and syntax programming methods.
Stage 1: detailed data validation
Single-variable rules were applied for the variables listed in Table I for all NJR primary procedures and for linked RC records. Descriptive statistics and frequencies were analysed to check for out-of-range or invalid values. Cross-variable and multi-case rules were applied to identify duplication of data. Missing rates were calculated for each field. The focus of this study was the validation of data and not the determination of the missingness mechanism.9 There was no imputation for missing data and we did not exclude records because of missing data. Descriptive statistics were calculated for illustrative purposes only.
Stage 2: retrieval centre random sample validation
In order to evaluate the accuracy of data entry on the RC, 5% of patients (n = 49) were selected using random sampling on the SPSS program for double-keying; we entered the data twice and compared the two datasets to see if they were different. The component and referral form were re-examined, re-entered on the database and checked against the original entry. Percentage rates of error and missing rates were calculated.
Stage 3: validation of linked records
The RC database was used as the comparator. An ‘error’ was defined as a discrepancy between the RC field entry and the NJR primary database. These should only be considered as a ‘true error’ where the verification of the source was subsequently performed. Percentage rates of error were calculated by dividing the absolute number of errors by the total number of data points. Binomial distribution was used to calculate 95% confidence intervals (CI), and Fisher’s Exact test applied to 2 × 2 contingency tables where necessary.10,11 All statistical tests were two-tailed and significance was assumed at a p-value < 0.05.
Stage 4: detailed analysis of errors
Errors identified from the data validation process in stage 3 were analysed on a case-by-case basis. Patient demographic data were cross-checked against NHS Spine. Component field errors were addressed with re-examination of the implant and/or radiograph. Verification of the source was not performed for Primary Operation Date and Surgical Unit Description fields. This was due to the challenges associated with tracing case notes from up to 11 years ago from multiple hospitals across the United Kingdom.
Results
Of the 929 RC records, 52 were excluded because the primary procedure was performed before 1 April 2003 (England and Wales) or 1 February 2013 (Northern Ireland). Of the remaining 877 records, 518 (59.1%) had an NHS number that was found on the NJR database. There were 95 records that were subsequently excluded from the entire dataset due to missing primary operation date on the RC database, when linkage could not be performed. The result was that 476 of 782 (60.9%) records on the RC were successfully linked to the NJR primary database. Therefore, 306 (39.1%) records from 136 surgical units did not meet the criteria for linkage (Fig. 1). The rate of linkage improved with time.
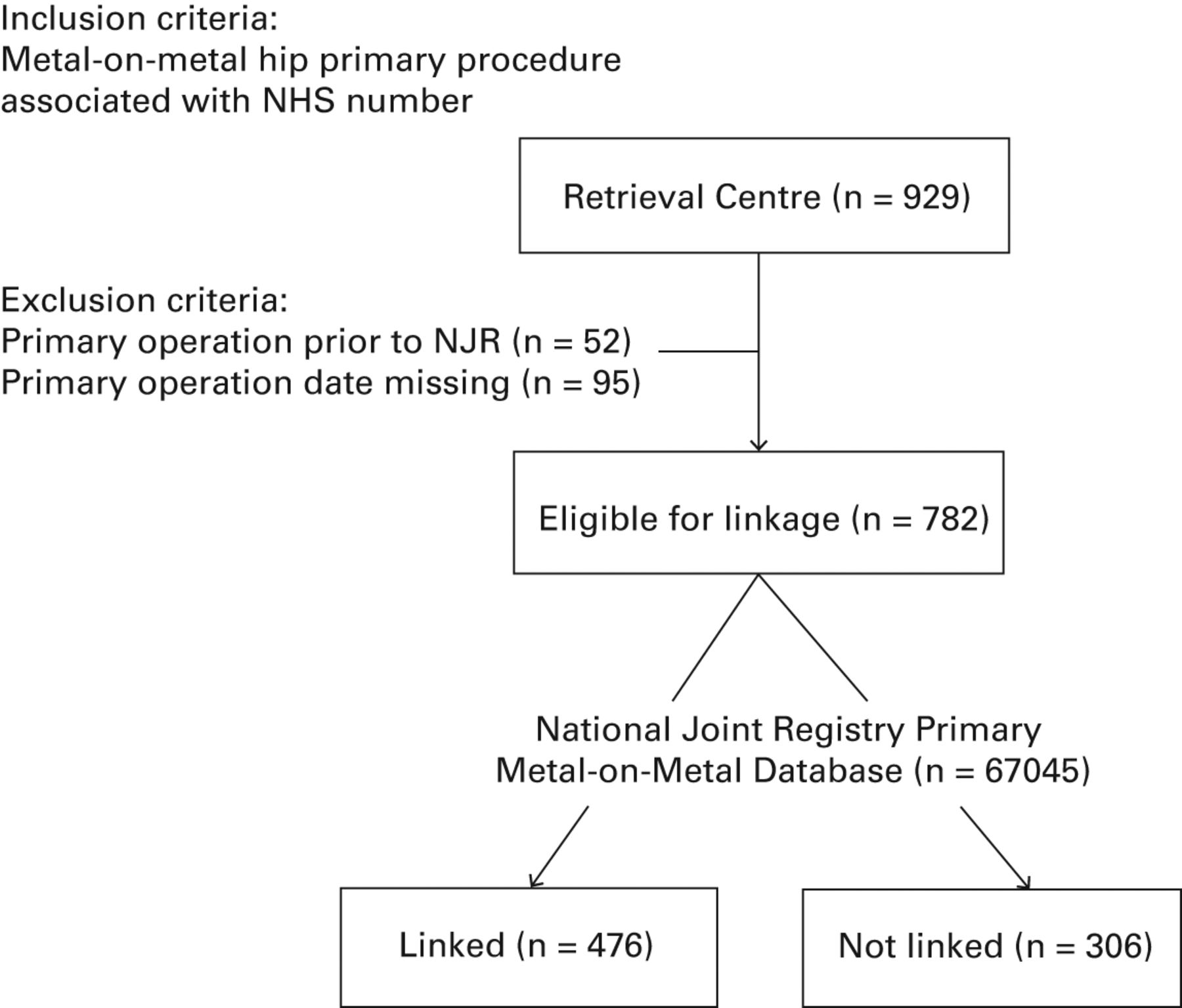
Fig. 1
Study flowchart
Data validation
Stage 1: Detailed data validation
This is provided in Tables II (NJR) and III (RC). There were no out of range or invalid values for any of the variables analysed. There were no duplicated records. The NJR had nearly perfect (> 99.9%) rates of completion of data for all fields. The lower rate for the size of the acetabular component presented in Table II was due to the use of a shell rather than a monobloc component, with only one true incomplete field entry.
Table II
Detailed data validation of National Joint Registry (NJR) primary database
| Field | Valid | OOR | Missing | Missing rate (%) | Mean/count | sd | Min | Max |
|---|---|---|---|---|---|---|---|---|
| Age at primary (yrs) | 67045 | 0 | 0 | 0.00 | 58.88 | 11.12 | 12 | 105 |
| Gender | 67040 | 0 | 5 | 0.00 | Male: 40661 | - | - | - |
| Female: 26379 | ||||||||
| Primary operation date | 67045 | 0 | 0 | 0.00 | - | - | - | - |
| Surgical unit description | 67045 | 0 | 0 | 0.00 | 417 units | - | - | - |
| Acetabular component brand | 67044 | 0 | 1 | 0.00 | 51 brands | - | - | - |
| Acetabular component ODEP rating | 67044 | 0 | 1 | 0.00 | 10A: 22240 | - | - | - |
| 7A: 13354 | ||||||||
| 7B: 144 | ||||||||
| 5A: 7497 | ||||||||
| 5B: 2 | ||||||||
| 3A: 9342 | ||||||||
| Discontinued: 6346 | ||||||||
| Pre-entry: 7372 | ||||||||
| Unclassified: 747 | ||||||||
| Component type | 67044 | 0 | 1 | 0.00 | Resurfacing: 33996 | - | - | - |
| Modular: 33048 | ||||||||
| Side | 67045 | 0 | 0 | 0.00 | Left: 31584 | - | - | - |
| Right: 35461 | ||||||||
| Head size (mm) | 67044 | 0 | 1 | 0.00 | 44.90 | 6.98 | 22.25 | 60 |
| Acetabular component size (Inner diameter) (mm) | 51309 | 0 | 15 736 (All shell only) | 23.5 | 47.95 | 4.61 | 28.00 | 64 |
| Head cat number | 67044 | 0 | 1 | 0.00 | - | - | - | - |
| Head batch number | 66958 | 0 | 87 | 0.1 | - | - | - | - |
| Acetabular component cat number | 67044 | 0 | 1 | 0.00 | - | - | - | - |
| Acetabular component batch number | 66952 | 0 | 93 | 0.1 | - | - | - | - |
| Outcome code | 67044 | 0 | 1 | 0.00 | Revised: 5615 | - | - | - |
| Unrevised: 58257 | ||||||||
| Death: 3172 | ||||||||
-
Missing rate %, number missing / total number of records x 100; Max, maximum; Min, minimum; OOR, out of range; sd, standard deviation; Valid, total number of records (n = 67 045); number OOR, number missing Descriptive statistics for 67 045 records of metal-on-metal primary procedures recorded on the National Joint Registry from 1 April 2003 to 1 November 2013. Records without NHS numbers were excluded as they were not eligible for linkage
Table III
Detailed data validation of linked Retrieval Centre (RC) records.
| Field | Valid | OOR | Missing | Missing rate (%) | Mean/count | sd | Min | Max |
|---|---|---|---|---|---|---|---|---|
| Age at primary (yrs) | 418 | 0 | 58 | 12.2 | 56.29 | 10.32 | 25 | 107 |
| Gender | 476 | 0 | 0 | 0.00 | Male: 209 | |||
| Female: 267 | ||||||||
| Primary operation date | 418 | 0 | 58 | 12.2 | - | |||
| Surgical unit description | 445 | 0 | 31 | 6.5 | 170 units | |||
| Acetabular component brand | 476 | 0 | 0 | 0.00 | 15 brands | |||
| Acetabular component ODEP rating | 476 | 0 | 0 | 0.00 | 10A: 167 | |||
| 7A: 27 | ||||||||
| 7B: 0 | ||||||||
| 5A: 77 | ||||||||
| 5B: 0 | ||||||||
| 3A: 47 | ||||||||
| Discontinued: 115 | ||||||||
| Pre-entry: 42 | ||||||||
| Unclassified: 1 | ||||||||
| Component type | 476 | 0 | 0 | 0.00 | Resurfacing: 292 | |||
| Modular: 184 | ||||||||
| Side | 466 | 0 | 10 | 2.1 | Left: 226 | |||
| Right: 240 | ||||||||
| Head size (mm) | 459 | 0 | 17 | 3.6 | 46.34 | 4.59 | 35 | 58 |
| Acetabular component size (outer diameter) (mm) | 452 | 0 | 24 | 5.0 | 53.33 | 3.91 | 44 | 66 |
| Head cat number | 241 | 0 | Total: 235 | 49.4 | - | |||
| No head: 5 | ||||||||
| Not visible: 230 | ||||||||
| Head batch number | 245 | 0 | Total: 231 | 48.5 | - | |||
| No head: 5 | ||||||||
| Not visible: 226 | ||||||||
| Acetabular component cat number | 295 | 0 | Total: 181 | 38.0 | - | |||
| No cup: 24 | ||||||||
| Not visible: 157 | ||||||||
| Acetabular component batch number | 373 | 0 | Total: 103 | 21.6 | - | |||
| No cup: 24 | ||||||||
| Not visible: 79 | ||||||||
| Outcome code | 476 | 0 | 0 | 0.00 | Revised: 476 | |||
| Unrevised: 0 | ||||||||
| Death: 0 | ||||||||
-
Missing rate %, number missing / total number of records x 100; Max, maximum; Min, minimum; OOR, out of range; sd, standard deviation; ODEP, Orthopaedic Data Evaluation Panel; Valid, total number of linked records (n = 476); number OOR, number missing Descriptive statistics for 476 records linked between National Joint Registry and RC. Linkage was performed on a patient-level using NHS number and then on a procedure-level as indicated in the methods
The RC had > 85% data completion for 11 of 15 fields. The four component reference number fields had the poorest completion of data. Missing data were mainly due to reference numbers not being visible on the retrieved component. The remaining missing data were due to only a single component from an acetabular component: femoral head pairing being sent to the RC. For missing category numbers, 157 of 181 (86.7%) references for the acetabular component and 230/235 (97.9%) references for the femoral head were due to reference numbers not being visible. Reference numbers on femoral heads were less well completed than for acetabular components, commonly due to bone on the retrieved femoral head obscuring the reference (Fig. 2). Other reasons included reference numbers scratched off (in vivo or during explantation) or never etched on the component during manufacture.
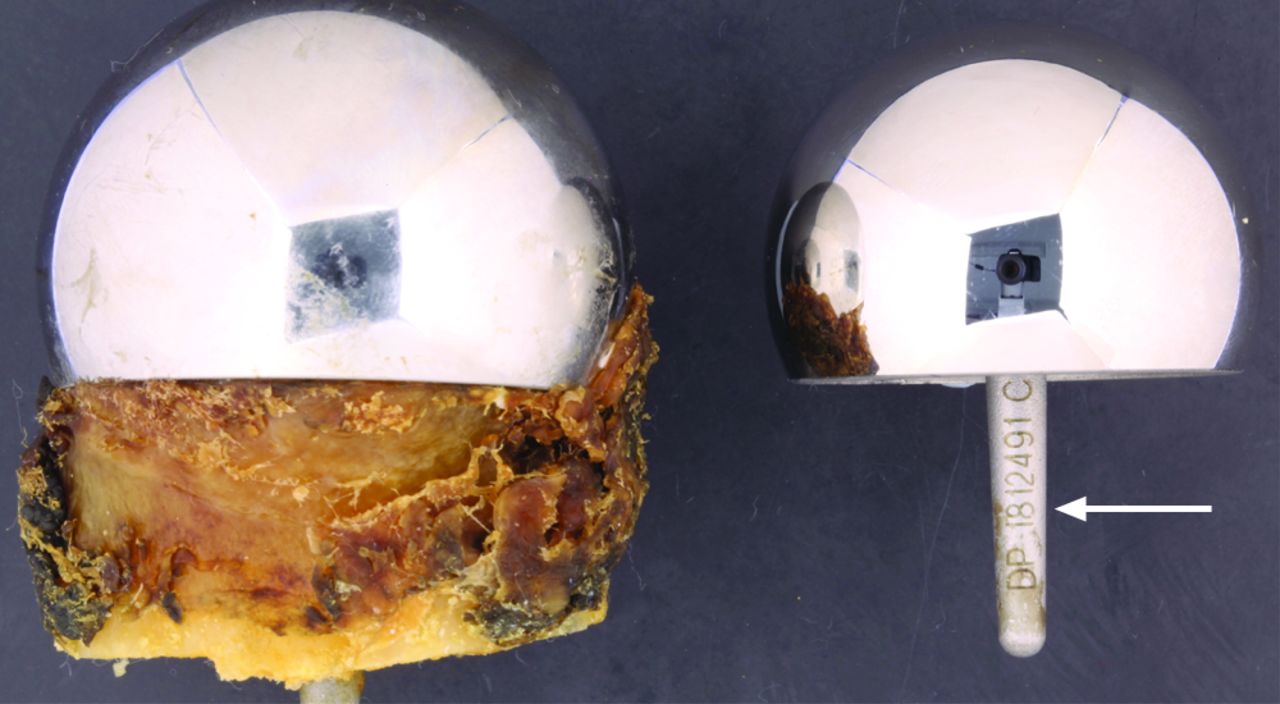

Figs. 2a - 2b
Photographic examples of retrieved components with easily readable and unreadable component reference numbers showing a) femoral head components and b) acetabular components.
Stage 2: RC random sample validation
This is summarised in Table IV. Errors of data entry were found in two of 15 fields examined. The error rates were 2/44 (4.6%) for the date of the primary operation and 1/43 (2.3%) for the description of the surgical unit. Errors were typographical or due to incorrect data re-coding during field-level linkage. No data-entry errors were detected for any component fields.
Table IV
Retrieval Centre (RC) random sample validation
| Field | Missing | Errors | Non-errors | Error rate (%) |
|---|---|---|---|---|
| Date of birth | 0 | 0 | 49 | 0.00 |
| Gender | 0 | 0 | 49 | 0.00 |
| Primary operation date | 5 | 2 | 42 | 4.55 |
| Surgical unit description | 6 | 1 | 42 | 2.33 |
| Acetabular component brand | 0 | 0 | 49 | 0.00 |
| Acetabular component ODEP rating | 0 | 0 | 49 | 0.00 |
| Component type | 0 | 0 | 49 | 0.00 |
| Side | 0 | 0 | 49 | 0.00 |
| Head size | 1 | 0 | 48 | 0·00 |
| Acetabular component size | 3 | 0 | 46 | 0.00 |
| Head cat number | 27 | 0 | 22 | 0.00 |
| Head batch number | 19 | 0 | 30 | 0.00 |
| Acetabular component cat number | 2 | 0 | 47 | 0.00 |
| Acetabular component batch number | 23 | 0 | 16 | 0.00 |
| RC outcome code | 0 | 0 | 49 | 0.00 |
-
A total of 49 records were selected at random from the RC to examine the accuracy of data entry. The component and referral form were re-examined, re-entered and then validated against the original entry. ‘Primary operation date’ errors were typographical. The ‘surgical unit description’ error reflected incorrect re-coding of the hospital during field-level linkage ODEP, Orthopaedic Data Evaluation Panel
The reasons for missing data were described above. The date of the primary procedure was frequently missing (five of 49 cases (10.2%)) due to this not being supplied by the revision surgeon. A description of the surgical unit was universally supplied, with four of 49 (8.2%) missing cases explained as ambiguous data that could not be re-coded to correspond with the NJR field codes.
Stage 3: validation of linked records
This is presented in Table V. There was a high error rate for outcome code, with 79 of 476 (16.6%) of NJR primary procedures incorrectly recorded as ‘unrevised’ or ‘death’. There were low rates of disagreement for demographic data fields (date of birth 10/476 (2.1%); gender 0/476 (0.0%); surgical unit description 5/445 (1.1%)), except for the date of the primary procedure (12.2%). For component fields, the rate of disagreement varied from 0% for the brand of the acetabular component to 21.4% for the size of the femoral head. Error rates for batch numbers tended to be higher than for category numbers.
Table V
Validation of linked records
| Field | Valid | Missing | Errors | Non-errors | Error rate (%) |
|---|---|---|---|---|---|
| Date of birth | 476 | 0 | 10 | 466 | 2.10 |
| Gender | 476 | 0 | 0 | 476 | 0.00 |
| Primary operation date | 418 | 58 | 51 | 367 | 12.20 |
| Surgical unit description | 445 | 31 | 5 | 440 | 1.12 |
| Acetabular component brand | 476 | 0 | 0 | 476 | 0.00 |
| Cup ODEP rating | 476 | 0 | 0 | 476 | 0.00 |
| Component type | 476 | 0 | 16 | 460 | 3.36 |
| Side | 405 | 71 | 9 | 396 | 2.22 |
| Head size | 459 | 17 | 98 | 361 | 21.35 |
| Acetabular component size | 439 | 37 | 13 | 426 | 2.96 |
| Head cat number | 242 | 235 | 14 | 229 | 4.98 |
| Head batch number | 245 | 232 | 13 | 232 | 5.31 |
| Acetabular component cat number | 295 | 182 | 2 | 293 | 0.68 |
| Acetabular component batch number | 371 | 106 | 24 | 347 | 6.47 |
| Outcome code | 476 | 0 | 79 | 397 | 16.60 |
-
Results of validation of 476 linked primary procedures. Retrieval Centre (RC) data were used as the reference. Errors for patient demographic data can be considered as discrepancies between the datasets, since checking to the source was not performed. Errors for component fields should be considered as ‘true’ errors, since the component was physically examined at the RC. The error rate for ‘outcome code’ represents under-reporting of component failure rate on the National Joint Registry ODEP, Orthopaedic Data Evaluation Panel
Stage 4: detailed analysis of errors
Re-examination of components did not find any errors of data entry at the RC (Table VI). Consequently all errors relating to component details were attributed to the NJR. Category number is a critical field on the NJR and automatically generates many component fields. Errors in the component fields could therefore be attributed to either the selection of an incorrect category number or an error in the catalogue. For example, 83 of 98 (84.7%) errors in the field for the size of the femoral head could be explained by an error in the Articular Surface Replacement (ASR; Depuy, Warsaw, Indiana) catalogue where odd component sizes were rounded down to the nearest even number. Examination of the outcome code field found one procedure coded as ‘death’. The remainder (n = 78) were coded as ‘unrevised’. This may be due either to the reporting of a revision to the RC only and not to the NJR, or an inability to link procedures due to lack of an NHS number.
Table VI
Detailed analysis of errors
| Field | Number of errors | Analysis performed | Source of error | Explanation |
|---|---|---|---|---|
| Date of birth | 10 | RC data-entry cross-checked with NHS Spine | RC | -Incorrect data supplied to RC by referring surgeon (n = 3) |
| -Typographical error (n = 7) | ||||
| Gender | 0 | - | - | - |
| Primary operation date | 51 | No source verification performed | NJR or RC | Data entry error on either database |
| Surgical unit description | 5 | No source verification performed | NJR or RC | Data entry error on either database |
| Acetabular component brand | 0 | - | - | - |
| Acetabular component ODEP rating | 0 | - | - | - |
| Component type | 16 | Component +/- radiograph re-examined | NJR | Error at level of NJR catalogue (incorrect component selection, catalogue entry error or both) |
| Side | 9 | No source verification performed | NJR or RC | Data entry error on either database. No radiographs available for examination for these components. |
| Head size | 98 | Component re-examined | NJR | Error at level of NJR catalogue (incorrect component selection, catalogue entry error or both) |
| Acetabular component size | 13 | Component re-examined | NJR | Error at level of NJR catalogue (incorrect component selection, catalogue entry error or both) |
| Head cat number | 12 | Component re-examined | NJR | Error at level of NJR catalogue (incorrect component selection, catalogue entry error or both) |
| Head batch number | 13 | Component re-examined | NJR | Nonsense data entered in free-text field |
| Acetabular component cat number | 2 | Component re-examined | NJR | Error at level of NJR catalogue (incorrect component selection, catalogue entry error or both) |
| Acetabular component batch number | 24 | Component re-examined | NJR | Nonsense data entered in free-text field |
| Outcome code | 79 | None required | NJR | (i) Incorrect coding of outcome as 'death' (n = 1) |
| (ii) Failure of NJR to link primary procedure to revision procedure (n = 78). Explanations: a) reporting of revision to RC only and b) absence of ‘linkability’ | ||||
-
NJR, National Joint Registry; RC, Retrieval Centre
Discussion
This study has provided the first large-scale linkage of registry and retrieval data in orthopaedic surgery. It represents an independent assessment of the quality of data in the NJR in regards to one aspect of the registry, namely primary procedures undertaken on metal-on-metal hip arthroplasties. We found that NJR data for the primary procedure had nearly perfect completion. However, we were unable to link more than one third of primary procedures recorded on the RC (306/782 procedures (39.1%)) and identified a high error rate for outcome coding on the NJR (79/476 erroneous records (16.6%)). These two findings may represent an underestimation of the rate of revision for many types of metal-on-metal components on the NJR. This is an important finding due to the influence of published NJR data on our understanding of the surgical, implant design and patient factors that affect performance in joint replacement surgery. These errors will be particularly important if the NJR expands its reporting of surgeon-level data and may be a major factor in the interpretation of the activity of a given surgeon.
The absence of a Unique Device Identifier (UDI)12 meant that we required matches on many criteria in order to create a link between a primary procedure and an explanted component. The initial ability to match on a patient-level using the unique NHS number allowed us to restrict the number of possible linkages for a given patient. This stage also excluded 359 patients from the possibility of any linkage. These patients either did not have their primary procedure reported to the NJR or had it reported without an NHS number. This may be consistent with the poor compliance and ‘linkability’ reported by the NJR in its early years. For example, compliance was only 64.7% and linkability 20% in 2003 (Fig. 3).1,2 However, the fewest number of records were entered during this period.
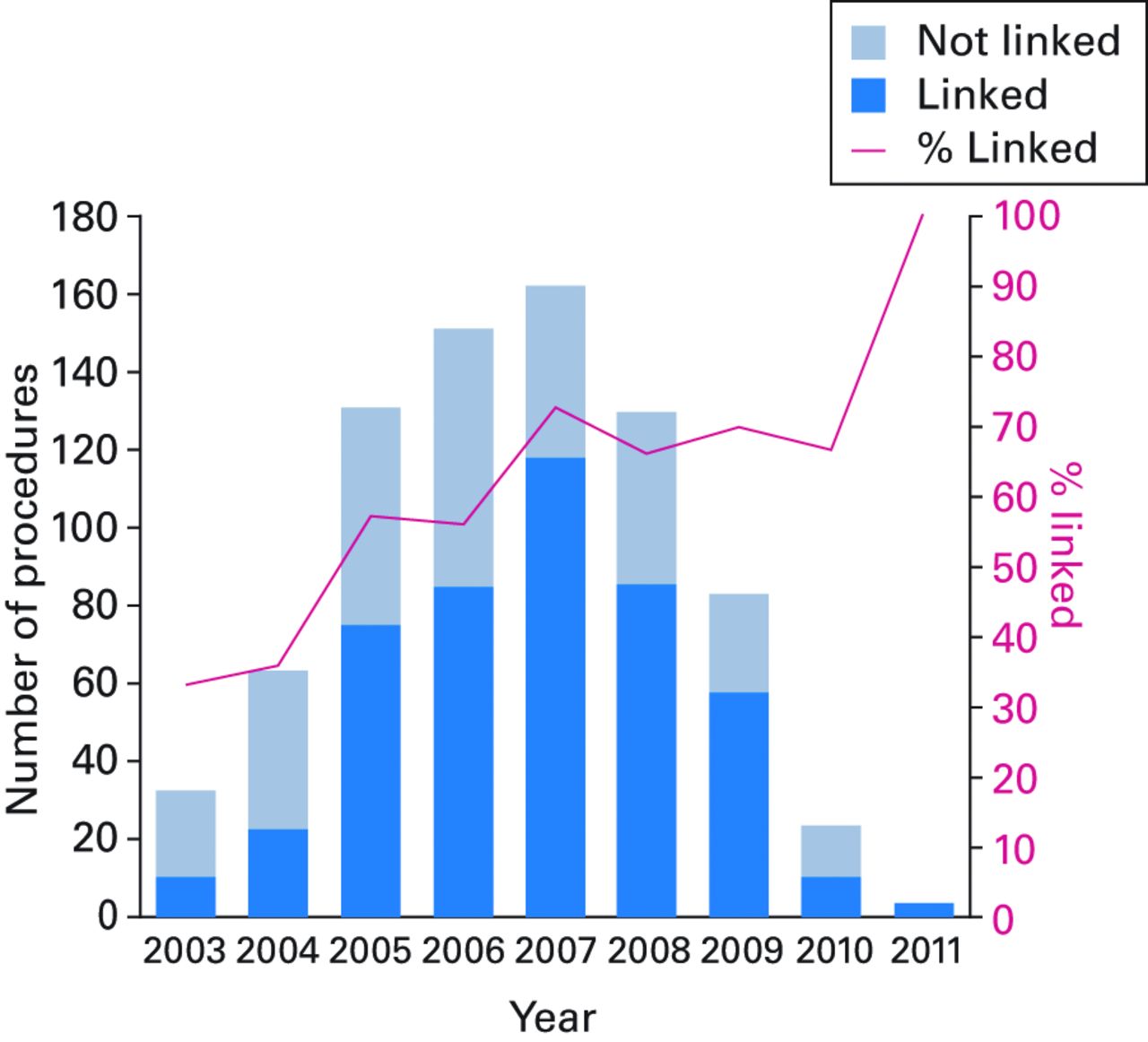
Fig. 3
Histogram showing that 476 out of 782 eligible procedures on the Retrieval Centre database were linked to a primary procedure recorded with the National Joint Registry (NJR). Linkage rates were poor for the early years of the NJR and improved considerably from 2005. This is consistent with poor compliance and linkability reported in early NJR reports.
Strict criteria to accept linkage were essential to avoid making an incorrect link. The date of the primary procedure was a key field for linkage, but was often poorly or inaccurately completed by surgeons submitting to the RC. This may be because revision surgeons were often not responsible for and/or from units remote to the primary procedure. We did not perform linkage where there was uncertainty. We are extending the verification of the source of the initial operation as part of our retrieval analyses in order to improve the recording of the date of the primary procedure.
The NJR requires linkage of a primary procedure to a revision procedure for an outcome code to be changed from ‘unrevised’. This is reliant on compliance from the unit where the revision is undertaken, patient consent and linkability. Linkability is defined as the number of records associated with an NHS number divided by the total number of records on the NJR. The NJR 11th annual report quotes compliance of 99%, patient consent of 91.8% and linkability of 95.1% for 2013/14.1
We identified one record incorrectly classified as ‘dead’, rather than ‘revised’. This is an important case to highlight given the forthcoming publication of surgeon-specific risk-adjusted mortality. We doubt that this is an isolated case, and even small numbers of errors may have a marked impact on the rates of mortality for low-volume arthroplasty surgeons. The ability of NJR data to account for confounders adequately is disputed.13 Surgeons are given the opportunity to review their data using a feedback system available through the password-protected section of the NJR website. Our findings suggest that it is advisable for surgeons to validate their own records and to inform the NJR of any discrepancies.
The number of revision procedures referred to the RC and not the NJR is difficult to quantify. It might be expected that where a surgeon has made a voluntary referral to the RC, he or she would also have fulfilled their compulsory obligation to refer to the NJR. However, whilst the RC deals almost exclusively directly with the referring surgeon, the NJR is typically provided with data through a system of data entry clerks. This chain may be responsible for some of the unlinked cases.
The highest error rate for any field was in the recording of the size of the femoral head (21.4%). Examination of these records found that 83/98 (84.7%) discrepancies were due to rounding down of odd-numbered ASR head sizes by 1 mm to the nearest even number. The two studies where NJR data were used to measure the effect of the size of the femoral head on the failure rate of metal-on-metal hip arthroplasties14,15 are unaffected by this because they used even-numbered groupings.
The remaining discrepancies for this field and errors for the category number fields are of greater clinical significance because they reflect a different component being recorded on the NJR to that which was retrieved Table VI. However, more precise quantification is required. This is an extensive process that will require analysis of individual patient records, investigation of the processes for the collection of NJR data and examination of NJR implant catalogues.
We acknowledge that failure to identify incorrect linkage is not impossible with the design of this study. However, since we used strict criteria and performed manual checks, we feel that this is unlikely. The requirement for a perfect match to link records would eliminate the problem of incorrect linkage, but would also mask errors and so was not performed.
Errors in the batch number fields were due to fictitious data being entered into free-text fields on the NJR. These are important discrepancies, because they may prevent the possibility to trace patients who have received an implant from a defective batch. We are not aware of any manufacturer that publishes guidance on how it formats batch numbers. We recommend that this information should be available in the public domain and supplied to both the NJR and RCs.
Errors in the date of birth field were exclusive to the RC and found to be easily corrected using NHS spine. This process has since been incorporated into the source verification protocols undertaken by the RC. Discrepancies in the recording of the date of the primary procedure are also likely to lie with the RC, given that referrals are from the revision surgeon, as discussed above. The NJR faces the same difficulties with unlinked procedures on their revision database. Our early analyses suggest that the RC performs similarly to the NJR revision database for this field.
This study has presented novel methodology for the validation of a hip arthroplasty register using retrieved implants. The methods can be generalised to other regions where a RC has been established and unique patient identifiers are used. The study provides particularly robust validation for component fields. The careful cataloguing of retrieved components renders them available for scrutiny indefinitely.
We acknowledge that this is a cross-sectional survey and provides observational data. However, reports from arthroplasty registers are a major influence on the interpretation of the performance of arthroplasties16 and it is essential that any data upon which reports are based are entirely accurate. We recognise the difference in scale between the RC and the NJR. Linked cases in this study represent approximately 1% of all primary metal-on-metal hip procedures recorded in the NJR.
The RC is independent of the NJR. Linkage to the NJR was not contemplated when the RC began collecting implants and the rationale for collecting implants is different to the NJR. The primary aim of the RC is to determine the mechanism, rather than the rate, of failure. In addition, it is a different type of organisation, being a surgeon-led research collaboration within an NHS hospital – university partnership, rather than a government initiative aimed at governance and funded through industry.
Registry-retrieval linkage provided a novel means for validation of one aspect of an arthroplasty register. We found nearly perfect completion for NJR records of primary metal-on-metal hip arthroplasties. However, the NJR is likely to have underestimated rates of revision for metal-on-metal hips. A record of the primary procedure was not identifiable on the NJR in 39.1% of retrieved components. The NJR incorrectly coded the outcome following primary surgery in 16.6% of linked cases. These errors are relevant given the increasing scope for the application of NJR data. We recommend a system for continuous independent evaluation of the quality and validity of NJR data. Surgeons should ensure that their information is accurately recorded.
1 No authors listed. National Joint Registry: National Joint Registry for England, Wales and Northern Ireland; 11th Annual Report, 2014. http://www.njrcentre.org.uk/njrcentre/Portals/0/Documents/England/Reports/11th_annual_report/NJR 11th Annual Report 2014.pdf (date last accessed 07 November 2014). Google Scholar
2 No authors listed. National Joint Registry: National Joint Registry for England and Wales; 1st Annual Report, 2004. http://www.njrcentre.org.uk/NjrCentre/Portals/0/Documents/England/Reports/NJR_AR_1.pdf (date last accessed 07 November 2014). Google Scholar
3 No authors listed. Healthcare Quality Improvement Partnership: Consultant Outcomes Publication, 2014. http://www.hqip.org.uk/consultant-outcomes-publication/ (date last accessed 07 November 2014). Google Scholar
4 Bridgewater B , CosgriffR, LaingHHealthcare Quality Improvement Partnership: Everyone Counts: Offer 2, 2013. http://www.hqip.org.uk/assets/Everyone-Counts/HQIP-Offer-2-report-to-NHSE-published-31.10.2013.pdf (date last accessed 07 November 2014). Google Scholar
5 No authors listed. Orthopaedic Data Evaluation Panel: ODEP Ratings, 2014. http://www.odep.org.uk/ODEPrating.aspx (date last accessed 2 December 2014). Google Scholar
6 Hirakawa K , JacobsJJ, UrbanR, SaitoT. Mechanisms of failure of total hip replacements: lessons learned from retrieval studies. Clin Orthop Relat Res2004;420:10–17.CrossrefPubMed Google Scholar
7 No authors listed. Health & Social Care Information Centre: NHS Number, 2014. http://systems.hscic.gov.uk/nhsnumber (date last accessed 07 November 2014). Google Scholar
8 No authors listed. Information Standards Boards for Health and Social Care: NHS Spine, 2014. http://www.isb.nhs.uk/use/baselines/spine (date last accessed 07 November 2014). Google Scholar
9 No authors listed. Missingness mechanisms. http://missingdata.lshtm.ac.uk/index.php?view=category& id=40%3Amissingness-mechanisms& option=com_content& Itemid=96 (date last accessed 2 December 2014). Google Scholar
10 Goldberg SI , NiemierkoA, TurchinA. Analysis of data errors in clinical research databases. AMIA Annu Symp Proc2008;242–246.PubMed Google Scholar
11 Hong MK , YaoHH, PedersenJS, et al.Error rates in a clinical data repository: lessons from the transition to electronic data transfer--a descriptive study. BMJ Open2013;3.pii:002406.CrossrefPubMed Google Scholar
12 Gross TP , CrowleyJ. Unique device identification in the service of public health. N Engl J Med2012;367:1583–1585.CrossrefPubMed Google Scholar
13 Whitehouse SL , BollandBJ, HowellJR, CrawfordRW, TimperleyAJ. Mortality following hip arthroplasty--inappropriate use of National Joint Registry (NJR) data. J Arthroplasty2014;29:1827–1834.CrossrefPubMed Google Scholar
14 Smith AJ , DieppeP, HowardPW. , Blom AW; National Joint Registry for England and Wales. Failure rates of metal-on-metal hip resurfacings: analysis of data from the National Joint Registry for England and Wales. Lancet2012;380:1759–1766. Google Scholar
15 Smith AJ , DieppeP, VernonK, et al.Failure rates of stemmed metal-on-metal hip replacements: analysis of data from the National Joint Registry of England and Wales. Lancet2012;379:1199–1204.CrossrefPubMed Google Scholar
16 Graves SE . The value of arthroplasty registry data. Acta Orthop2010;81:8–9.CrossrefPubMed Google Scholar
S. A. Sabah: Study Design, Writing report, Data Interpretation, Review of manuscript.
J. Henckel: Study Design, Writing report, Data Interpretation, Review of manuscript.
E. Cook: Statistical analysis, Preparation of tables and figures, Data Interpretation.
R. Whittaker: Preparation of figures, Review of manuscript.
H. Hothi: Review of manuscript.
Y. Pappas: Review of manuscript.
G. Blunn: Review of manuscript.
J. A. Skinner: Study Design, Writing report, Review of manuscript.
A. J. Hart: Study Design, Writing report, Data Interpretation, Review of manuscript.
We thank the Gwen Fish Charity and Dunhill Medical Trust for financial support for this study. Neither had any role in the design of the study, writing the manuscript or the decision to submit for publication.
Additionally we acknowledge the contributions of Mrs G. Lloyd, Mrs C. Page, and Ms E. Ellis who helped in the collection and preparation of the Retrieval Centre data that allowed this manuscript to be produced. Finally we would like to thank the 108 hospitals that submitted components to the London Implant Retrieval Centre and all hospitals and persons who have contributed data to the National Joint Registry. We are grateful to the Healthcare Quality Improvement Partnership (HQIP), the NJR Research Sub-Committee and staff at the NJR Centre for facilitating this work.
Disclaimer: The authors have conformed to the NJR’s standard protocol for data access and publication. The views expressed represent those of the authors and do not necessarily reflect those of the National Joint Registry Steering Committee or the Health Quality Improvement Partnership (HQIP) who do not vouch for how the information is presented.
Liability: The Healthcare Quality Improvement Partnership (‘HQIP’) and/or the National Joint Registry (‘NJR’) take no responsibility for the accuracy, currency, reliability and correctness of any data used or referred to in this report, nor for the accuracy, currency, reliability and correctness of links or references to other information sources and disclaims all warranties in relation to such data, links and references to the maximum extent permitted by legislation.
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
This article was primary edited by G. Scott and first proof edited by J. Scott.
Supplementary material. A table showing outcome coding and a list of 108 hospitals that submitted components to the London Implant Retrieval Centre and allowed this study to be performed is available alongside the online version of this article at www.bjj.boneandjoint.org.uk.









