Abstract
Aims
Highly polished stems with force-closed design have shown satisfactory clinical results despite being related to relatively high early migration. It has been suggested that the minimal thickness of cement mantles surrounding the femoral stem should be 2 mm to 4 mm to avoid aseptic loosening. The line-to-line cementing technique of the femoral stem, designed to achieve stem press-fit, challenges this opinion. We compared the migration of a highly polished stem with force-closed design by standard and line-to-line cementing to investigate whether differences in early migration of the stems occur in a clinical study.
Methods
In this single-blind, randomized controlled, clinical radiostereometric analysis (RSA) study, the migration pattern of the cemented Corail hip stem was compared between line-to-line and standard cementing in 48 arthroplasties. The primary outcome measure was femoral stem migration in terms of rotation and translation around and along with the X-, Y-, and Z- axes measured using model-based RSA at three, 12, and 24 months. A linear mixed-effects model was used for statistical analysis.
Results
Results from mixed model analyses revealed a lower mean retroversion for line-to-line (0.72° (95% confidence interval (CI) 0.38° to 1.07°; p < 0.001), but no significant differences in subsidence between the techniques (-0.15 mm (95% CI -0.53 to 0.227; p = 0.429) at 24 months. Radiolucent lines measuring < 2 mm wide were found in three and five arthroplasties cemented by the standard and line-to-line method, respectively.
Conclusion
The cemented Corail stem with a force-closed design seems to settle earlier and better with the line-to-line cementing method, although for subsidence the difference was not significant. However, the lower rate of migration into retroversion may reduce the wear and cement deformation, contributing to good long-term fixation and implant survival.
Cite this article: Bone Joint J 2022;104-B(1):19–26.
Take home message
For implantation of cemented hip stems, choosing the optimal combination of cementing technique, geometrical implant design, and surface roughness seems to be paramount.
Line-to-line cementing in combination with a force-closed design seems to reduce early retroversion of the stem.
Introduction
To reduce aseptic loosening (ASL) and stem revision, the minimal thickness of modern complete cement mantles is generally 2 mm to 4 mm.1,2 This knowledge is challenged by the paradoxical results obtained with two French-designed cemented stems: Charnley-Kerboull (CK) (Orthinox, Stryker Howmedica, France) and Ceraver Osteal (Ceraver, France).3 These are cemented line-to-line as a press-fit and not with the recommended 2 mm to 4 mm of surrounding cement.1 The best results were achieved with the polished and rectangular double-tapered CK mark I and II.2,4,5
An in vitro study demonstrated the worst-case scenario with mechanical failure if the stem is undersized and the cement is not adequately pressurized. The stem was found to create high cement stresses, resulting in cracking of the full-thickness cement.6 In an in vitro controlled research study, we have previously shown that line-to-line cementing generates higher cement pressure and increased cement penetration into cancellous bone, resulting in a thinner composite mantle, but better interdigitation than standard cementing.7
Fixation models of cemented hip stems are commonly characterized as force-closed and shape-closed.8,9 Shape-closed designs are meant to be contained by the cement mantle and have a rough surface texture, collars, and curved shape. Like the cemented Corail (DePuy Synthes, USA), force-closed designs are intended to subside in the mantle and have a polished surface finish, are tapered, wedged, and sometimes straight. They are designed to subside gradually postoperatively. Their stability is provided by subsidence under load, like with a press-fit cone.
Standard cementing with oversized broaching has shown good long-term survival with shape-closed design and force-closed design, respectively. However, it is not necessarily true that this technique provides the optimal outcome for force-closed design.3,9-12
Interpretation and understanding of the context between migration pattern, early ASL, and long-time survival in correlation to stem design, cementing technique, and mantle quality can be obtained from radiostereometric analysis (RSA) studies.13-16 With RSA, a long-term prediction could be made of prosthetic loosening based on the 24-month follow-up RSA data.14,16-19 Several studies have investigated the line-to-line cementing technique versus the standard cementing technique. However, to our knowledge, the relationship between the migrations of the hip stem with the two cementing techniques has not been previously explored.
This clinical research study was designed as a prospective, single-blind, randomized controlled clinical trial. The aim of the study was to investigate the differences in migration pattern of the force-closed femoral stem design by comparing standard and line-to-line broaching and cementing of the polished taper-shaped Corail stem. We hypothesized that there is no significant difference in the pattern of migration of the hip stem on RSA between the line-to-line and standard cementing techniques.
Methods
This study (Clinical Trials NCT 01952067) was performed at the department of orthopaedic surgery at Kristiansund Hospital, Kristiansund, Norway. Between April 2013 and June 2015, 48 patients were included by orthopaedic hip surgeons at our outpatient unit. The last two-year follow-up was in June 2017. A total of 48 total hip arthroplasties (THAs) in 48 patients were randomized; of these, 25 received line-to-line and 23 received standard cementing (Figure 1). The inclusion criteria were male and female patients aged between 55 and 75 years with a diagnosis of primary or secondary osteoarthritis (OA) or avascular necrosis (AVN). The following patients were excluded: those who could not sign the consent form; required revision THA, cementless THA, or THA for reasons other than OA or AVN; prior osteotomy of the femur; BMI > 35 kg/m2; and a diagnosis of suspected infection or malignancy.
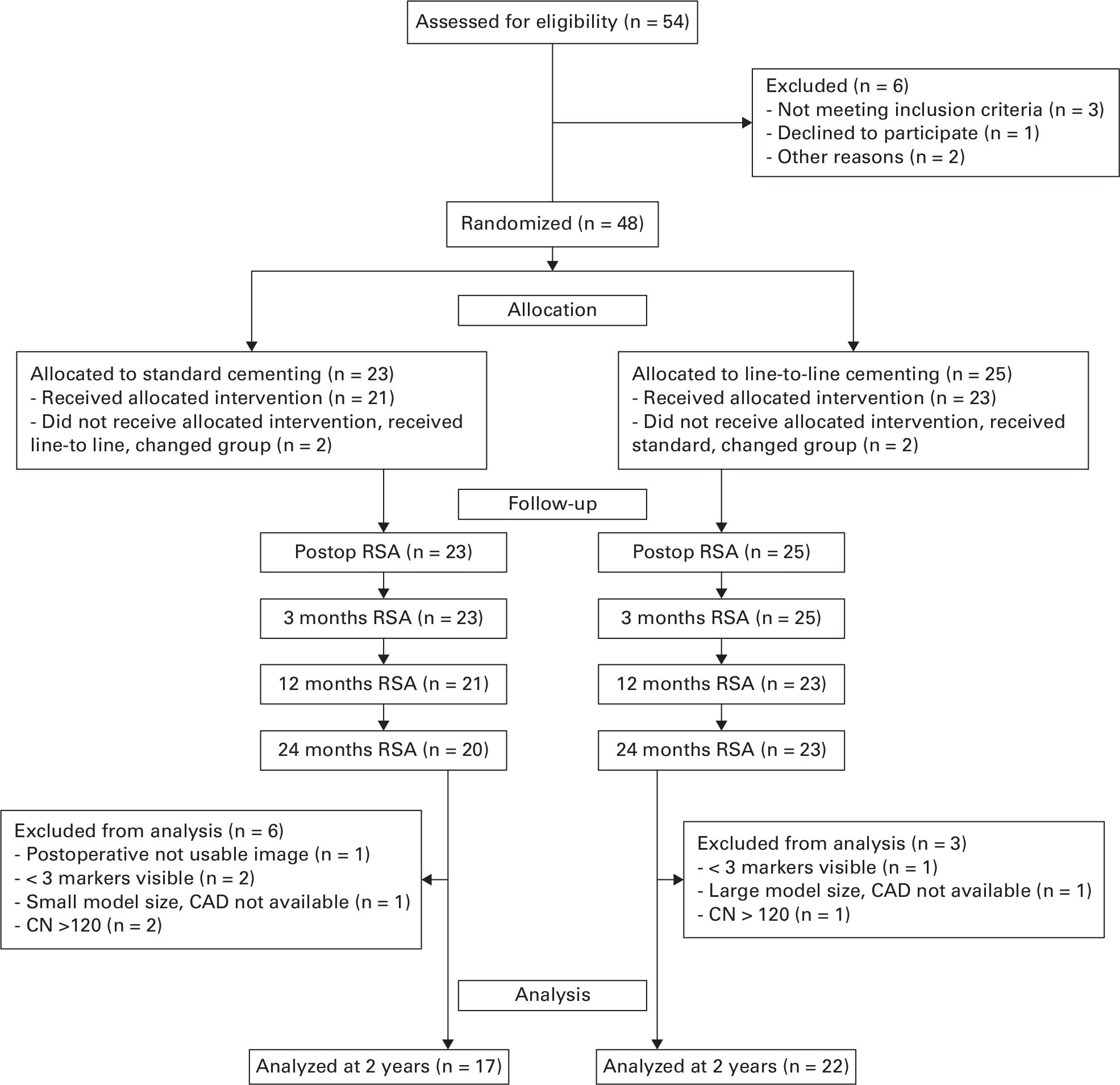
Fig. 1
CONSORT flowchart. CAD, computer-aided design; CN, condition number; RSA, radiostereometric analysis.
Patients were randomized to receive either the standard or the line-to-line cementing of the Corail hip stem. Block random allocation was performed by a computer-generated randomization program (Unit for Applied Clinical Research, Norwegian University of Science and Technology, Norway). The patients and independent examiners performing the RSA and the clinical assessment were blinded to the applied type of cementing technique. Two experienced consultant hip surgeons (KMF, ØBL) carried out the procedure using the direct Hardinge lateral approach in a single department.20 For standard cementing, the corresponding implant (i.e. 1 mm undersized in all directions) was used, and for line-to-line cementing, an implant with the same geometrical size as the broach was used. The patients received a standard collarless cemented Corail hip stem with standard offset, a 28 mm Alumina Biolox Forte Ceramic Head (DePuy Synthes), and a cemented polyethylene Marathon acetabular component (DePuy Synthes). Cemex Genta Fast Bone Cement (Tecres, Italy)21-25 was inserted using a third-generation cementing technique with pulsatile lavage and closed mixing, retrograde injection, proximal seal, and pressurization. The cement was inserted at two minutes and the stems implanted at three minutes after mixing, respectively. Patients were evaluated at inclusion, within one week, and at three, 12, and 24 months postoperatively. At each evaluation, RSA acquisitions and conventional anteroposterior and lateral images were obtained. The primary endpoint was stem migration at two years measured by RSA.
The study was planned and executed according to the tenets of the World Medical Association Declaration of Helsinki.26 The participants received written information regarding the study and signed an informed consent form prior to surgery.
For RSA measurements, eight tantalum markers (ø = 0.8 mm) were inserted into the proximal femur. These reference bone markers form a rigid body that is the basis for all RSA calculations. RSA acquisitions were obtained using a set-up with the patient supine over a uniplanar calibration cage (CanonCage; RSA Biomedical, Sweden). All RSA images were made with a fixed (Discovery XR 656; General Electric Company, USA) and mobile (Optima XR22amx; General Electric Company) roentgen tube. The first acquisition was made within one week postoperatively, and the relative position of the stem to the bone was set to serve as the baseline for all further examinations. If the markers’ configuration was inadequate or too few markers (< three) had been used, the patient was excluded from the RSA analyses.
Computer-aided design (CAD) details of the stem were used to represent the femoral component.27-30 A 3D model of the cemented Corail prosthesis, based on CAD information, was combined with a 3D sphere model. This integrated model was used to determine the stem’s 3D position in the RSA set-up. Translations and rotations of the prosthesis in the orthogonal axes (Figure 2) were calculated with a model-based RSA software (Model-Based RSA software v. 4.11; RSAcore, Leiden University Medical Centre, The Netherlands). RSA analyses were performed by a third party (RSAcore).
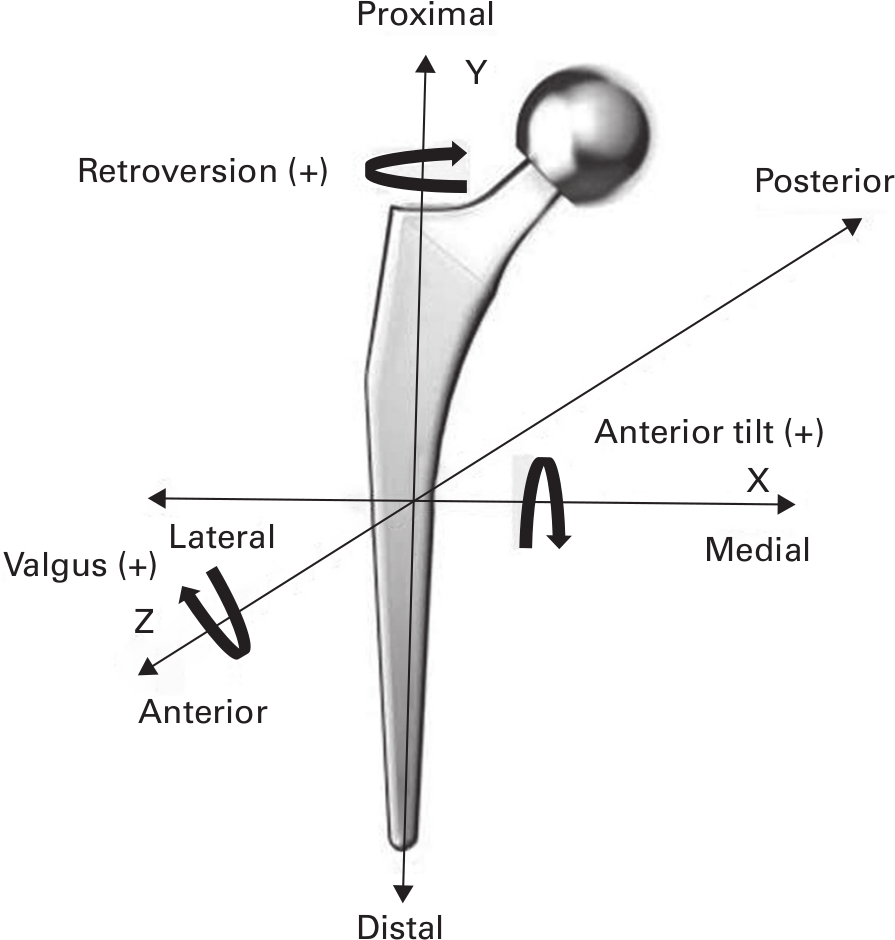
Fig. 2
Orientation of the migration coordinate system with the Corail stem (DePuy Synthes, USA).
To determine the precision of the RSA set-up, a double set of RSA examinations during the 12-month follow-up was acquired. As actual migration within the short time interval in between the double examinations is expected to be zero, the calculated migration for these double examinations represents the measurement error. The standard deviation (SD) is a measure for the precision (i.e. the upper limit of 95% confidence interval (CI) of the measurements (Table I).13,31,32
Table I.
Precision results of 31 double migration measurements of the patient standard radiostereometric migration analysis (upper limits of 95% confidence interval). X, Y, and Z refer to orthogonal axes. Translation is given in mm and rotation in degrees.
| Tx | Ty | Tz | Rx | Ry | Rz |
|---|---|---|---|---|---|
| 0.06 | 0.15 | 0.16 | 0.30 | 0.73 | 0.12 |
-
R, rotation; T, translation
For all examinations, the mean rigid body error (ME) of the RSA markers was 0.15 mm (SD 0.065), and the mean condition number of the RSA markers was 61.1 (SD 23.2). Markers that moved by > 0.5 mm with respect to other markers were considered unstable and excluded from the analyses.
The prosthetic migration was calculated with respect to the largest set of available matching bone markers, in all follow-up moments (minimum three markers) and meeting the International Organization for Standardization criteria for rigid body matching. The ME was < 0.35 mm and the condition number (CN) was < 120 m-1 (ISO16087:2013).32
The femoral component’s orientation was evaluated as recommended by Johnston et al33 using the prosthesis, the proximal lateral cement mantle and the trochanter major as landmarks. Cement grading was evaluated using the grading of Barrack, Mulroy, and Harris, as described in previous studies assessed from the postoperative radiographs (Table II).34,35 The two-year postoperative radiographs were evaluated according to Engh, Bobyn, and Glassman for the presence of cement fractures and local endosteal lysis at the cement-bone interface in all 14 Gruen zones.36,37 Radiolucent lines were measured on radiographs according to Kobayashi et al.38 All image acquisitions were obtained from the local picture archiving and communication system (PACS).
Table II.
Characteristics, implant parameters, and cement grading in patients with complete radiographs.
| Characteristic | Standard | Line-to-line |
|---|---|---|
| Total, n | 17 | 22 |
| Sex, n (%) | ||
| Female | 10 (58.82) | 15 (68.18) |
| Male | 7 (41.18) | 7 (31.82) |
| Mean BMI, kg/m2 (SD) | 26.2 (3.0) | 27.0 (2.9) |
| Mean age, yrs (SD) | 65.5 (4.5) | 65.5 (6.2) |
| Side, n | ||
| Left | 9 | 10 |
| Right | 8 | 12 |
| Stem size, n | ||
| 9 | 3 | 1 |
| 10 | 1 | 1 |
| 11 | 6 | 5 |
| 12 | 6 | 7 |
| 13 | 0 | 3 |
| 14 | 1 | 4 |
| 15 | 0 | 1 |
| Stem orientation, n | ||
| Varus | 2 | 4 |
| Neutral (> 3°) | 15 | 17 |
| Valgus | 0 | 1 |
| Barrack cement grading, n | ||
| A | 14 | 17 |
| B | 3 | 5 |
| C | 0 | 0 |
| D | 0 | 0 |
-
SD, standard deviation.
Statistical analysis
Assuming a difference in stem subsidence of 0.6 mm (SD 0.6) and 0.7° y-rotation of the stem (SD 0.7) represents a clinically significant difference which is associated with increased risk of early failure.13,39 Accordingly, 17 patients would be needed to detect a potential effect with a statistical power of 80% and a significance level of 5%.23,40-42 This is in accordance with other RSA THA studies, which include a minimum sample size of approximately 12 to 15 participants.13
Descriptive statistics were presented as the mean and SD for continuous variables and absolute and relative frequencies for categorical variables. Estimates are reported as the mean and 95% CI where appropriate. Throughout the follow-up period, migration was analyzed using a linear mixed model (LMM) with an intercept for each patient. This model deals with the correlation induced by repeated measurements. For each outcome the linear mixed model was adjusted for the following baseline characteristics; age, sex, BMI, time, and stem size. A p-value < 0.05 was considered to indicate statistical significance. All analyses were performed using SPSS Statistics for Windows v. 25.0 (IBM, USA).
Results
There were no clinically relevant differences between the two groups regarding implant parameters, cement grading, or demographic data (Table II).
The stems migrated by subsidence and retroversion, which appeared mainly within the first three months but continued throughout the 24-month follow-up period. The pattern of migration along and around the orthogonal axes showed that the stems cemented using the standard technique subsided more distally and rotated more in retroversion than the stems cemented using the line-to-line technique. The measurement precision was 0.01 mm for subsidence along the y-axis and 0.02° for rotation around the y-axis.
Retroversion
At three, 12, and 24 months, the migration in retroversion of the stems was significantly higher with standard than line-to-line cementing. Within the first three months, stems with standard and line-to-line cementing migrated in retroversion by a mean of 1.08° (SD 0.70°) and 0.46° (SD 0.43°), respectively. At 12 months, the stems with standard and line-to-line cementing had migrated in retroversion by a mean of 2.06° (SD 1.41°) and 0.94° (SD 0.49°), respectively. At 24 months, the total rate of migration of stems in retroversion for the standard and line-to-line cementing were 2.36° (SD 1.15°) and 1.13° (SD 0.59°) respectively (Table III). All stems continued to migrate throughout the observation period (Figure 3). Results from mixed model analyses revealed a lower mean retroversion (Ry) for line-to-line (0.77° (95% CI 0.39° to 1.15°); p < 0.001) (Table IV).
Table III.
Mean monthly migration.
| Mean monthly migration (95% CI) | Translation, mm | Rotation, ° | ||||
|---|---|---|---|---|---|---|
| X | Y | Z | X | Y | Z | |
| 0 to 3 mths | ||||||
| Standard | 0.01 (-0.06 to 0.09) | -0.48 (-0.70 to -0.25) | -0.04 (-0.14 to 0.05) | -0.04 (-0.22 to 0.13) | 1.08 (0.73 to 1.43) | -0.01 (-0.11 to 0.09) |
| Line to line | -0.02 (-0.09 to 0.05) | -0.42 ( -0.71 to -0.13) | -0.02 (-0.12 to 0.07) | -0.05 (-0.26 to 0.16) | 0.46 (0.25 to 0.67) | -0.01 (-0.13 to 0.11) |
| 12 to 24 mths | ||||||
| Standard | 0.01 (-0.12 to 0.14) | -0.89 (-1.25 to -0.52) | -0.16 (-0.31 to 0.00) | -0.35 (-0.58 to -0.12) | 2.06 (1.34 to 2.78) | -0.08 (-0.25 to 0.09) |
| Line to line | -0.05 (-0.16 to 0.07) | -0.71 (-1.16 to -0.26) | -0.05 (-0.17 to 0.08) | -0.06 (-0.25 to 0.12) | 0.94 (0.71 to 1.18) | -0.01 (-0.21 to 0.19) |
| 24 mths | ||||||
| Standard | -0.03 (-0.15 to 0.09) | -1.22 (-1.72 to -0.72) | -0.20 (-0.37 to -0.04) | -0.36 (-0.68 to -0.04) | 2.36 (1.75 to 2.96) | -0.04 (-0.25 to 0.16) |
| Line to line | -0.07 (-0.19 to 0.05) | -0.86 (-1.32 to -0.39) | -0.1 (-0.23 to 0.03) | -0.13 (-0.34 to 0.08) | 1.13 (0.85 to 1.41) | -0.048 (-0.26 to 0.19) |
| Precision | -0.00 (-0.01 to 0.00) | 0.01 (-0.02 to 0.03) | 0.02 (-0.01 to 0.04) | -0.02 (-0.07 to 0.03) | -0.02 (-0.13 to 0.08) | -0.01 (-0.03 to 0.01) |
-
CI, confidence interval.
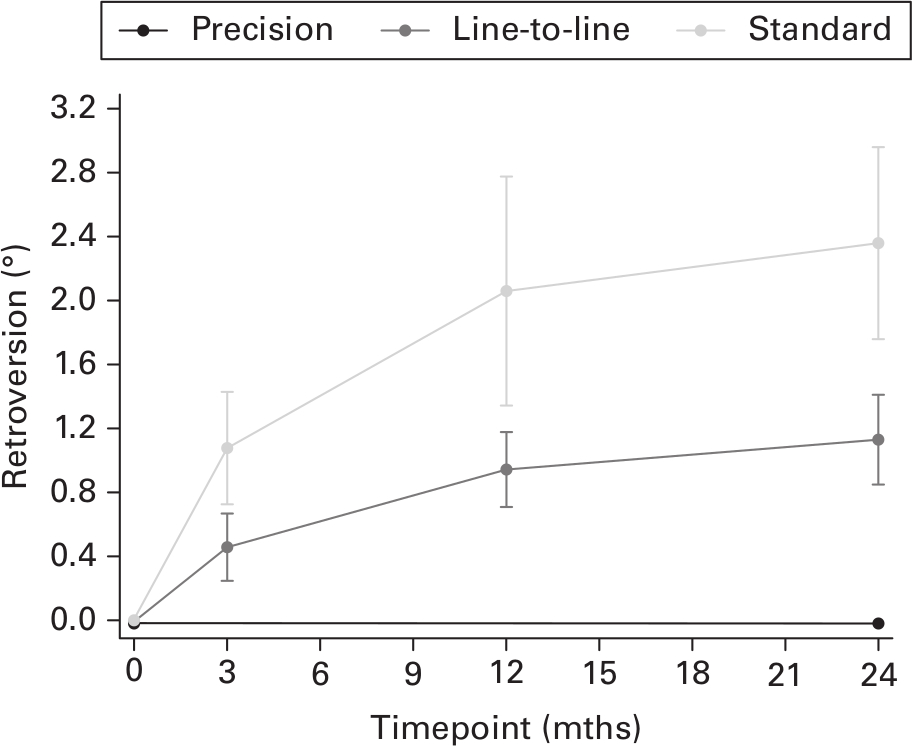
Fig. 3
Mean retroversion (°) with standard and line-to-line cementing of the Corail stem compared with the precision of rotation around the y-axis. Line-to-line retroversion rate 12 to 24 months: 0.187 (95% confidence interval (CI) -0.031 to 0.404); standard retroversion rate 12 to 24 months: 0.369 (95% CI 0.022° to 0.717).
Table IV.
Results of the mixed effects model. Reported coefficient estimates from linear mixed model analysis comparing line-to-line to standard technique. Estimates adjusted for age, sex, BMI, time, and stem size.
| Axis | Coefficient (95% CI) | p-value |
|---|---|---|
| TX | 0.090 (-0.008 to 0.189) | 0.074 |
| TY | -0.198 (-0.413 to 0.373) | 0.921 |
| TZ | -0.078 (-0.203 to 0.045) | 0.215 |
| RX | -0.071 (-0.279 to 0 .136) | 0.499 |
| RY | 0.770 (0.390 to 1.151) | < 0.001 |
| RZ | 0.063 (-0.092 to 0.220) | 0.424 |
-
CI, confidence interval; R, rotation; T, translation.
Subsidence
At three months, subsidence of the stems was similar. At 12 and 24 months, mean subsidence was higher with standard cementing than line-to-line cementing. Within the first three months, stems with standard cementing subsided by a mean of 0.48 mm (SD 0.46). The corresponding value for line-to-line cementing was 0.42 mm (SD 0.67). At 12 months, stems in the standard and line-to-line cementing groups showed subsidence by a mean of 0.89 mm (SD 0.75) and 0.71 mm (SD 1.05), respectively. Similarly, at 24 months, stems in the standard and line-to-line cementing groups showed subsidence by a mean of 1.22 mm (SD 0.99) and 0.86 mm (SD 1.09), respectively (Table III). All stems continued to migrate throughout the observation period (Figure 4).
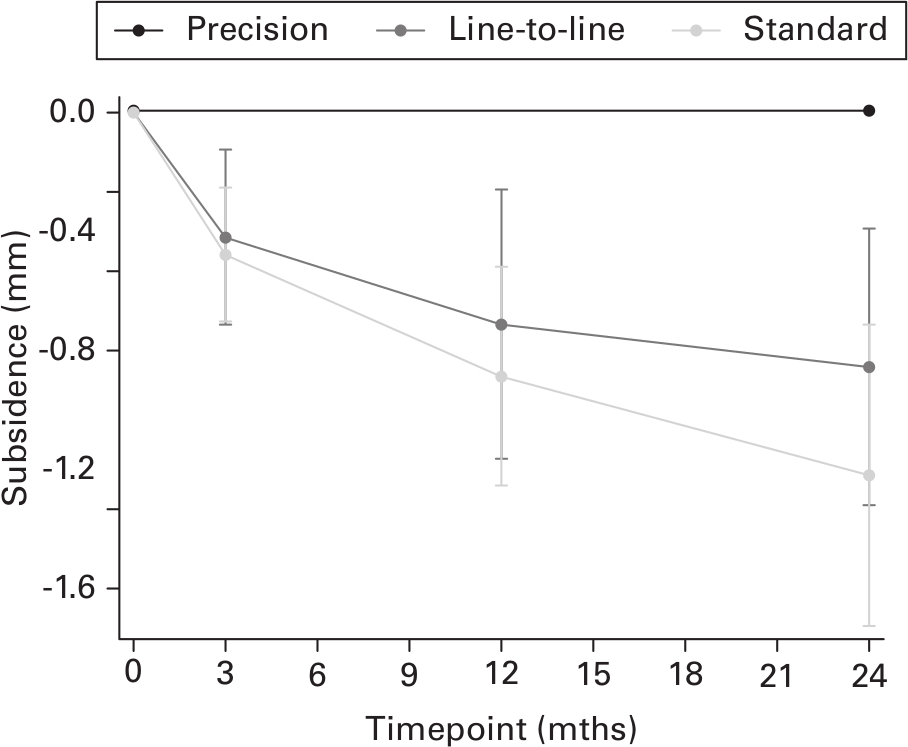
Fig. 4
Mean subsidence (mm) with standard and line-to-line cementing of the Corail stem compared with the precision of translation along the y-axis. Line-to-line subsidence rate 12 to 24 months: -0.143 (95% confidence interval (CI) -0.207 to 0.078); standard subsidence rate 12 to 24 months: -0.287 (95% CI -0.475 to -0.099).
Results from mixed model analyses revealed no significant differences in subsidence (Ty) between the techniques (-0.19 mm (95% CI -0.41 to 0.377); p = 0.921) (Table IV).
Radiological outcomes
Radiolucent lines were found in three and five THAs cemented by standard and line-to-line technique, respectively. However, their width was < 2 mm, and they all appeared in one Gruen zone only. Cement fractures and osteolytic lesions were not detected in any THA.
Survival and complications
After two years of follow-up, no revision surgery was required in any patient. None of the study participants experienced adverse events, and no postoperative complications were recorded during the study period. Due to misunderstandings between surgical staff who used the randomization program and the surgeons, there were four patients who did not receive the allocated method. Thus, results were analyzed according to the intention-to-treat principle.
Discussion
To our knowledge, this is the first randomized RSA study to compare the migration patterns of polished hip stems cemented using the standard and line-to-line techniques. The main finding was that the highly polished cemented Corail stem migrated significantly less in retroversion with the line-to-line technique compared to the standard technique. The stems subsided less with the line-to-line compared to the standard; however, this difference was not statistically significant. For both techniques, the main migration (subsidence and retroversion) took place during the first three months and continued during the observation period of 24 months.
For both cementing techniques, the mean distal subsidence at two years was less than 1.2 mm. This is in accordance with other studies of highly polished stems.43-46 The very low distal subsidence of 0.86 mm in the line-to-line group is quite similar to that reported at two years with the Exeter (Stryker, USA) stem.47 Furthermore, the subsidence at two years for both cementing techniques in the present study was less than that reported with the C-stem (DePuy Synthes).46,48 The significantly lower rate of retroversion in the line-to-line cementing group in our study can be explained by the cementing technique, which is crucial when a highly polished Corail stem is used. In a previous in vitro study comparing the two cementing techniques, we have shown that the line-to-line technique generated an adequate and similar cement mantle thickness by interdigitating the cement deep into the cancellous bone within the internal surface of the cortex.7 In that study, we found a higher cement pressure with the line-to-line technique than the standard technique. The phenomena of deep cement interdigitation may be beneficial in stabilizing the cemented Corail stem, which is double-tapered with a rectangular proximal shape. The corners of the rectangle are rounded, and the distal tip has a blunter shape than the Exeter and C-stem stems. The deep interdigitation into the cancellous bone creates a composite that may be beneficial for stabilizing highly polished stems. This geometrical factor may explain the increased retroversion of this stem when combined with standard cementing. Retroversion at two years with the line-to-line technique is also comparable to the results of Murray et al,47 where the Exeter stem was combined with standard cementing. However, in our study, a cemented Corail stem with the standard technique showed increased retroversion compared to other studies.
The low number of radiolucent lines in our study is acceptable. However, it can be interpreted as complete white-out or a Mach-effect indicating edge enhancement between areas of different densities on radiological images.34,49 Cement fractures and osteolytic lesions were not observed in any THA and may indicate low implant wear at 24 months. High-viscosity cement was used in the present study, which possibly created higher pressure and subsequent better penetration into corticocancellous bone.7
Precise cut-off values for the degree of early migration of the stem assumed to be related to ASL have not been characterized. The pattern of early migration considered to be pathological seems to vary with different implant designs. With wedged, highly polished taper-shaped stems, the RSA findings of a high level of early subsidence and retroversion are an expected finding in stems of this design.50,51 This is contrary to other designs where such findings may be interpreted as predicting early failure.15,52 Different RSA studies of similar stems show variation in the degree of migration reported (Supplementary Table i).
This study was conducted according to the ISO16087:2013 requirements for clinical assessment of migration of orthopaedic implants using RSA.32 RSA is a highly accurate technique to measure the migration of prosthesis components relative to bone. It uses a lower radiation dose than regular radiographs, but achieves a much higher precision in measuring relative prosthesis pose changes. Another strength of this study is that it was designed and performed as a prospective, single-blinded, randomized controlled trial.
The main limitation of this study was missing data, mainly by the exclusion of RSA images that did not match the predefined quality standards (missing cage markers, unusable postoperative image, high CN, and CAD-models not available). Missing data may introduce selection bias and cause type 2 error, resulting in reduced precision of variable estimates. However, missing data in our study were assumed to be random and thus unrelated to the outcome variables. Patients aged > 75 years were not included.
The results and conclusions only apply to the cemented Corail implant with force-closed design. Other stems with comparable design features were not investigated.
In conclusion, the line-to-line cementing technique provides significantly reduced migration in retroversion when used in combination with the Corail highly polished hip stem. The results of this study indicate that for wedged taper-shaped highly polished hip stems with force-closed design, line-to-line cementing is a promising procedure, but long-term clinical outcomes are warranted.
References
1. Langlais F , Kerboull M , Sedel L , Ling RSM . The “French Paradox.” J Bone Joint Surg Br . 2003 ; 85-B ( 1 ): 17 – 20 . Google Scholar
2. El Masri F , Kerboull L , Kerboull M , Courpied JP , Hamadouche M . Is the so-called “French Paradox” a reality?: long-term survival and migration of the Charnley-Kerboull stem cemented line-to-line . J Bone Joint Surg Br . 2010 ; 92-B ( 3 ): 342 – 348 . Google Scholar
3. Skinner JA , Todo S , Taylor M , Wang JS , Pinskerova V , Scott G . Should the cement mantle around the femoral component be thick or thin? J Bone Joint Surg Br . 2003 ; 85-B ( 1 ): 45 – 51 . Google Scholar
4. Kerboull M . L’Arthroplastie Totale de Hanche . Maîtrise Orthopédique . 1999 ; 83 : 6 – 10 . [Article in French]. Google Scholar
5. Laboudie P , El Masri F , Kerboull L , Hamadouche M . Short vs standard-length femoral stems cemented according to the “French Paradox”: a matched paired prospective study using ein bild roentgen analyze femoral component at two-year follow-up . J Arthroplasty . 2021 ; 36 ( 3 ): 1043 – 1048 . Google Scholar
6. Janssen D , van Aken J , Scheerlinck T , Verdonschot N . The “French Paradox” exposed: a finite element analysis of cement philosophy on implant stability and crack formation in the cement mantle . Trans Orthop Res Soc . 2007 ; 32 : 280 . Google Scholar
7. Sevaldsen K , Schnell-Husby O , Lain ØB , Schnell-Husby V . Does the line-to-line cementing technique of the femoral stem create an adequate cement mantle? Hip Int . 2020 . 1120700020934368 Crossref PubMed Google Scholar
8. Huiskes R , Verdonschot N , Nivbrant B . Migration, stem shape, and surface finish in cemented total hip arthroplasty . Clin Orthop Relat Res . 1998 ; 355 : 103 – 112 . Crossref PubMed Google Scholar
9. Scheerlinck T , Casteleyn PP . The design features of cemented femoral hip implants . J Bone Joint Surg Br . 2006 ; 88-B ( 11 ): 1409 – 1418 . Crossref PubMed Google Scholar
10. Clauss M , Breusch SJ . The “French paradox” may not be a paradox after all - but for what reason? Bone Joint Res . 2019 ; 8 ( 1 ): 1 – 2 . Google Scholar
11. Breusch S , Malchau H . The Well-Cemented Total Hip Arthroplasty . Berlin, Heidelberg : Springer . 2005 . Google Scholar
12. Numata Y , Kaneuji A , Kerboull L , et al. Biomechanical behaviour of a French femoral component with thin cement mantle: The ‘French paradox’ may not be a paradox after all . Bone Joint Res . 2018 ; 7 ( 7 ): 485 – 493 . Google Scholar
13. Valstar ER , Gill R , Ryd L , Flivik G , Börlin N , Kärrholm J . Guidelines for standardization of radiostereometry (RSA) of implants . Acta Orthop . 2005 ; 76 ( 4 ): 563 – 572 . Crossref PubMed Google Scholar
14. Karrholm J , Borssen B , Lowenhielm G , Snorrason F . Does early micromotion of femoral stem prostheses matter? 4-7-year stereoradiographic follow-up of 84 cemented prostheses . J Bone Joint Surg Br . 76-B ( 6 ): 912 – 917 . PubMed Google Scholar
15. Hauptfleisch J , Glyn-Jones S , Beard DJ , Gill HS , Murray DW . The premature failure of the Charnley Elite-plus stem: A confirmation of RSA predictions . J Bone Joint Surg Br . 88-B ( 2 ): 179 – 183 . Crossref PubMed Google Scholar
16. Nieuwenhuijse MJ , Valstar ER , Kaptein BL , Nelissen RG . Good diagnostic performance of early migration as a predictor of late aseptic loosening of acetabular cups: results from ten years of follow-up with Roentgen stereophotogrammetric analysis (RSA) . J Bone Joint Surg Am . 2012 ; 94-A ( 10 ): 874 – 880 . Crossref PubMed Google Scholar
17. Pijls BG , Nieuwenhuijse MJ , Schoones JW , Middeldorp S , Valstar ER , Nelissen RGHH . RSA prediction of high failure rate for the uncoated interAx TKA confirmed by meta-analysis . Acta Orthop . 2012 ; 83 ( 2 ): 142 – 147 . Crossref PubMed Google Scholar
18. Ryd L , Albrektsson B , Carlsson L , et al. Roentgen stereophotogrammetric analysis as a predictor of mechanical loosening of knee prostheses . J Bone Joint Surg Br . 1995 ; 77-B ( 3 ): 377 – 383 . PubMed Google Scholar
19. van der Voort P , Pijls BG , Nieuwenhuijse MJ , et al. Early subsidence of shape-closed hip arthroplasty stems is associated with late revision. A systematic review and meta-analysis of 24 RSA studies and 56 survival studies . Acta Orthop . 2015 ; 86 ( 5 ): 575 – 585 . Crossref PubMed Google Scholar
20. Hardinge K . The direct lateral approach to the hip . J Bone Joint Surg Br . 1982 ; 64-B ( 1 ): 17 – 19 . Google Scholar
21. Furnes O , Engesæther L , Hallan G , et al. 2017 Annual Report . Norwegian National Advisory Unit on Arthroplasty and Hip Fractures . 2017 . http://nrlweb.ihelse.net/eng/Rapporter/Report2020_english.pdf ( date last accessed 23 November 2021 ). PubMed Google Scholar
22. Kärrholm J , Rogmark C , Nauclér E , et al. Swedish Hip Arthroplasty Register Annual Report 2019 . Swedish Hip Arthroplasty Register . 2019 . http://dx.doi.org/10.18158/H1BdmrOWu ( date last accessed 10 November 2021 ). Google Scholar
23. Söderlund P , Dahl J , Röhrl S , Nivbrant B , Nilsson KG . 10-year results of a new low-monomer cement . Acta Orthop . 2012 ; 83 ( 6 ): 604 – 608 . Crossref PubMed Google Scholar
24. Nivbrant B , Kärrholm J , Röhrl S , Hassander H , Wesslén B . Bone cement with reduced proportion of monomer in total hip arthroplasty: preclinical evaluation and randomized study of 47 cases with 5 years’ follow-up . Acta Orthop Scand . 2001 ; 72 ( 6 ): 572 – 584 . Google Scholar
25. Gallart X , Martínez F , García S , et al. Radiologic evaluation of the cement mantle in the femoral shaft. A comparative study using a fast-set or a standard-set cement . Hip Int . 2007 ; 17 ( 4 ): 205 – 211 . Crossref PubMed Google Scholar
26. World Medical Association . World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects . JAMA . 2013 ; 310 ( 20 ): 2191 – 2194 . PubMed Google Scholar
27. Kaptein BL , Valstar ER , Spoor CW , Stoel BC , Rozing PM . Model-based RSA of a femoral hip stem using surface and geometrical shape models . Clin Orthop Relat Res . 2006 ; 448 : 92 – 97 . Crossref PubMed Google Scholar
28. Prins AH , Kaptein BL , Stoel BC , Nelissen R , Reiber JHC , Valstar ER . Handling modular hip implants in model-based RSA: Combined stem-head models . J Biomech . 2008 ; 41 ( 14 ): 2912 – 2917 . Crossref PubMed Google Scholar
29. Koster LA , Meinardi JE , Kaptein BL , Van der Linden-Van der Zwaag E , Nelissen RGHH . Two-year RSA migration results of symmetrical and asymmetrical tibial components in total knee arthroplasty: A randomized controlled trial . Bone Joint J . 2021 ; 103-B ( 5 ): 855 – 863 . Crossref PubMed Google Scholar
30. van Ooij B , Sierevelt IN , van der Vis HM , Hoornenborg D , Haverkamp D . What is the role of cemented fixation in total knee arthroplasty? The two-year results of a randomized RSA controlled trial . Bone Joint J . 2021 ; 103-B ( 1 ): 98 – 104 . Crossref PubMed Google Scholar
31. Ranstam J , Ryd L , Onsten I . Accurate accuracy assessment: Review of basic principles . Acta Orthop Scand . 1999 ; 70 ( 4 ): 319 – 321 . Crossref PubMed Google Scholar
32. No authors listed . ISO 16087: Implants for surgery: Roentgen stereophotogrammetric analysis for the assessment of migration of orthopaedic implants . International Organization for Standardization Geneva . 2013 . https://www.iso.org/standard/55662.html ( date last accessed 10 November 2021 ). Google Scholar
33. Johnston RC , Fitzgerald RH , Harris WH , Poss R , Müller ME , Sledge CB . Clinical and radiographic evaluation of total hip replacement. A standard system of terminology for reporting results . J Bone Joint Surg Am . 1990 ; 72-A ( 2 ): 161 – 168 . PubMed Google Scholar
34. Garcia FL , Sugo AT , Picado CHF . Radiographic grading of femoral stem cementation in hip arthroplasty . Acta Ortop Bras . 2013 ; 21 ( 1 ): 30 – 33 . Crossref PubMed Google Scholar
35. Barrack RL , Mulroy RD , Harris WH . Improved cementing techniques and femoral component loosening in young patients with hip arthroplasty. A 12-year radiographic review . J Bone Joint Surg Br . 1992 ; 74-B ( 3 ): 385 – 389 . Crossref PubMed Google Scholar
36. Engh CA , Bobyn JD , Glassman AH . Porous-coated hip replacement. The factors governing bone ingrowth, stress shielding, and clinical results . J Bone Joint Surg Br . 1987 ; 69-B ( 1 ): 45 – 55 . Crossref PubMed Google Scholar
37. Gruen TA , McNeice GM , Amstutz HC . “Modes of failure” of cemented stem-type femoral components: a radiographic analysis of loosening . Clin Orthop Relat Res . 1979 ; 141 : 17 – 27 . Google Scholar
38. Kobayashi S , Takaoka K , Saito N , Hisa K . Factors affecting aseptic failure of fixation after primary Charnley total hip arthroplasty: multivariate survival analysis . J Bone Joint Surg Am . 1997 ; 79-A ( 11 ): 1618 – 1627 . Google Scholar
39. Kärrholm J , Herberts P , Hultmark P , Malchau H , Nivbrant B , Thanner J . Radiostereometry of hip prostheses . Clin Orthop Relat Res . 1997 ; 344 ( 344 ): 94 . PubMed Google Scholar
40. Röhrl SM , Nivbrant B , Ström H , Nilsson KG . Effect of augmented cup fixation on stability, wear, and osteolysis: A 5-year follow-up of total hip arthroplasty with RSA . J Arthroplasty . 2004 ; 19 ( 8 ): 962 – 971 . Crossref PubMed Google Scholar
41. Pakvis D , Luites J , van Hellemondt G , Spruit M . A cementless, elastic press-fit socket with and without screws . Acta Orthop . 2012 ; 83 ( 5 ): 481 – 487 . Crossref PubMed Google Scholar
42. Flatøy B , Röhrl SM , Bøe B , Nordsletten L . No medium-term advantage of electrochemical deposition of hydroxyapatite in cementless femoral stems. 5-year RSA and DXA results from a randomized controlled trial . Acta Orthop . 2016 ; 87 ( 1 ): 42 – 47 . Crossref PubMed Google Scholar
43. Alfaro-Adrián J , Gill HS , Murray DW . Should total hip arthroplasty femoral components be designed to subside? A radiostereometric analysis study of the charnley elite and exeter stems . J Arthroplasty . 2001 ; 16 ( 5 ): 598 – 606 . Crossref PubMed Google Scholar
44. Alfaro-Adrian J , Gill H , Murray D . Cement migration after THR: a comparison of Charnley Elite and Exeter femoral stems using RSA . J Bone Joint Surg Br . 81-B ( 1 ): 130 – 134 . Google Scholar
45. Stefánsdóttir A , Franzén H , Johnsson R , Ornstein E , Sundberg M . Movement pattern of the Exeter femoral stem; a radiostereometric analysis of 22 primary hip arthroplasties followed for 5 years . Acta Orthop Scand . 2004 ; 75 ( 4 ): 408 – 414 . Crossref PubMed Google Scholar
46. Sundberg M , Besjakov J , von Schewelow T , Carlsson A . Movement patterns of the C-stem femoral component: An RSA study of 33 primary total hip arthroplasties followed for two years . J Bone Joint Surg Br . 87-B ( 10 ): 1352 – 1356 . Crossref PubMed Google Scholar
47. Murray DW , Gulati A , Gill HS . Ten-year RSA-measured migration of the Exeter femoral stem . Bone Joint J . 2013 ; 95-B ( 5 ): 605 – 608 . Crossref PubMed Google Scholar
48. von Schewelov T , Carlsson A , Sanzén L , Besjakov J . Continuous distal migration and internal rotation of the c-stem prosthesis without any adverse clinical effects: An RSA study of 33 primary total hip arthroplasties followed for up to ten years . Bone Joint J . 2014 ; 96-B ( 5 ): 604 – 608 . Crossref PubMed Google Scholar
49. Chan J , Khoriati AA , Chiang CH , Hadithy NA . Understanding, interpreting and reporting a total hip arthroplasty radiograph . Orthop Muscular Syst . 2017 ; 06 ( 3 ). Google Scholar
50. Nieuwenhuijse MJ , Valstar ER , Kaptein BL , Nelissen R . The Exeter femoral stem continues to migrate during its first decade after implantation: 10-12 years of follow-up with radiostereometric analysis (RSA ). Acta Orthop . 2012 ; 83 ( 2 ): 129 – 134 . Crossref PubMed Google Scholar
51. Carrington NC , Sierra RJ , Gie GA , Hubble MJW , Timperley AJ , Howell JR . The Exeter Universal cemented femoral component at 15 to 17 years: An update on the first 325 hips . J Bone Joint Surg Br . 2009 ; 91-B ( 6 ): 730 – 737 . Crossref PubMed Google Scholar
52. Kiernan S , Hermann KL , Wagner P , Ryd L , Flivik G . The importance of adequate stem anteversion for rotational stability in cemented total hip replacement: A radiostereometric study with ten-year follow-up . Bone Joint J . 2013 ; 95-B ( 1 ): 23 – 30 . Crossref PubMed Google Scholar
Author contributions
K. Sevaldsen: Conceptualization, Methodology, Project administration, Resources, Investigation, Data curation, Formal analysis, Validation, Visualization, Writing – original draft.
O. S. Husby: Conceptualization, Methodology, Project administration, Supervision, Validation, Writing – original draft.
Ø. B. Lian: Conceptualization, Methodology, Project administration, Supervision, Writing – original draft.
K. M. Farran: Conceptualization, Methodology, Investigation, Validation, Writing – original draft.
V. Schnell Husby: Conceptualization, Methodology, Project administration, Supervision, Investigation, Validation, Writing – original draft.
Funding statement
K. Svaldsen declares a grant from The Liaison Committee for Education, Research and Innovation in Central Norway, Norwegian University of Science and Technology (grant number 46055500-6), related to this study. No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
Acknowledgements
We thank Tor Åge Myklebust for statistical assistance and Lennard Koster for performing the RSA-analysis. We also thank Head Nurse-Operating Room, Birgitte Arnøy for her contribution during surgery and research nurse Myrthle Slettvåg Hoel for help with inclusion and follow-up.
Ethical review statement
Ethical approval: Reference code REK 2009/1986 4.2009.958.
Open access funding
Helse Møre og Romsdal Health Trust, Ålesund, Norway (grant number 2021/5696).
Open access statement
This is an open-access article distributed under the terms of the Creative Commons Attribution Non-Commercial No Derivatives (CC BY-NC-ND 4.0) licence, which permits the copying and redistribution of the work only, and provided the original author and source are credited. See https://creativecommons.org/licenses/by-nc-nd/4.0/
Trial registration number
NCT 01952067
This article was primary edited by G. Scott.
Follow Helse MøreogRomsdal @HelseMR
Follow Norwegian University of Science and Technology @NTNU
Supplementary material
Table showing radiostereometric migration results from studies on force-closed design.









