Abstract
Aims
Hip fracture patients are at higher risk of severe COVID-19 illness, and admission into hospital puts them at further risk. We implemented a two-site orthopaedic trauma service, with ‘COVID’ and ‘COVID-free’ hubs, to deliver urgent and infection-controlled trauma care for hip fracture patients, while increasing bed capacity for medical patients during the COVID-19 pandemic.
Methods
A vacated private elective surgical centre was repurposed to facilitate a two-site, ‘COVID’ and ‘COVID-free’, hip fracture service. Patients were screened for COVID-19 infection and either kept at our ‘COVID’ site or transferred to our ‘COVID-free’ site. We collected data for 30 days on patient demographics, Clinical Frailty Scale (CFS), Nottingham Hip Fracture Scores (NHFS), time to surgery, COVID-19 status, mortality, and length of stay (LOS).
Results
In all, 47 hip fracture patients presented to our service: 12 were admitted to the ‘COVID’ site and 35 to the ‘COVID-free’ site. The ‘COVID’ site cohort were older (mean 86.8 vs 78.5 years, p = 0.0427) and with poorer CFS (p = 0.0147) and NHFS (p = 0.0023) scores. At the ‘COVID-free’ site, mean time to surgery was less (29.8 vs 52.8 hours, p = 0.0146), and mean LOS seemed shorter (8.7 vs 12.6 days, p = 0.0592). No patients tested positive for COVID-19 infection while at the ‘COVID-free’ site. We redirected 74% of our admissions from the base ‘COVID’ site and created 304 inpatient days’ capacity for medical COVID patients.
Conclusion
Acquisition of unused elective orthopaedic capacity from the private sector facilitated a two-site trauma service. Patients were treated expeditiously, while successfully achieving strict infection control. We achieved significant gains in medical bed capacity in response to the COVID-19 demand. The authors propose the repurposing of unused elective operating facilities for a two-site ‘COVID’ and ‘COVID-free’ model as a safe and effective way of managing hip fracture patients during the pandemic.
Cite this article: Bone Joint Open 2020;1-6:190–197.
Introduction
The impact of the COVID-19 pandemic on the National Health Service (NHS) is unprecedented. In these extraordinary circumstances, we are tasked with difficult decisions to ration limited NHS resources in order to provide the best possible care for all patients presenting with COVID-19 and non-COVID-19 related conditions. In order to control the spread of the novel coronavirus, clinicians are asked to balance the risks of COVID-19 infection during hospital admission and benefits of inpatient treatment.
Hip fracture patients are typically elderly, frail, live in nursing homes, and have multiple comorbidities, putting them at higher risk of developing severe COVID-19 illness.1,2 During the pandemic, the care of patients with hip fractures remains a clinical priority and necessitates urgent surgical intervention.
Confirmed or suspected COVID-19 infection is not a reason to delay or cancel urgent surgery for hip fractures.3 However, admitting ‘COVID-free’ patients into hospital puts them at risk of contracting the coronavirus. The management of hip fracture patients, therefore, mandates careful consideration. Orthopaedic services must provide prompt, high-quality multidisciplinary care for all hip fracture patients, while aiming to prevent ‘COVID-free’ patients from contracting the infection while in hospital for surgery.
We describe our experiences of setting up our two-site orthopaedic trauma service, with ‘COVID’ and ‘COVID-free’ hubs, to deliver urgent trauma care for hip fracture patients and evaluate the patient outcomes of this intervention.
The primary aims of reorganizing our trauma service were: firstly, to geographically separate COVID and non-COVID hip fracture patients to prevent in-hospital transmission of COVID-19 infection; and secondly, to offer timely hip fracture surgery and maintain the same standard of care as during non-COVID times. The secondary aim was to create bed capacity for the medical teams at our base site in preparation for surge-capacity in the event of spikes in COVID-19 admissions.
Methods
In response to the COVID-19 pandemic, all elective orthopaedic operations have been cancelled and acute trauma services reduced to accommodate the increase in medical COVID-19 patients. This has led to reassignment of acute orthopaedic wards to medical wards and left private elective orthopaedic theatres and wards unused. Our unit made the decision to establish a ‘COVID-free’ site in an unused elective orthopaedic theatre and ward in the private sector. The chosen site was conveniently located adjacent to an acute medical hospital of the same trust, previously without any trauma inpatient services. Both sites were staffed by our own orthopaedic team and supplemented by anaesthetists, operating department practitioners, scrub nurses and ancillary staff from the private hospital.
Inclusion criteria for the study were all patients referred by the emergency department (ED) with radiologically confirmed hip fractures or periprosthetic hip fractures: no patients were excluded. Patients were reviewed initially by the ED team at the base site and screened for COVID-19 symptoms. Suspected cases, as recommended by Public Health England (PHE) guidance, included patients who presented with either new onset of cough with or without pyrexia, or an influenza-like illness.4
After onward referral to our orthopaedic team, the patients were again assessed for clinical features of COVID-19 infection based on the hospital’s guidelines. Investigations included routine physiological parameters, haematological and biochemistry tests and chest radiographs. Medical team referral was sought if any abnormality was detected. At the time of the study, it was not considered routine in the UK to perform COVID-19 testing in the absence of clinical suspicion. Suspected cases remained at the base ‘COVID’ site and were isolated on a COVID ward, awaiting their surgery and swab results. Medical teams were involved early.
If patients did not show signs or symptoms suspicious for COVID-19 infection, they were transferred directly from the ED to the ‘COVID-free’ site after analgesia and orthopaedic clerking. At the ‘COVID-free’ site, patients were admitted to open bays and only moved to a sideroom if they developed COVID-19 symptoms, as per our unit’s infection control protocols.
Suspected COVID-19 patients with hip fractures had surgery at our ‘COVID’ site in a dedicated COVID-19 theatre and received postoperative care in a COVID cohort ward. COVID-free patients had surgery at the ‘COVID-free’ site in a ‘clean’ theatre and received postoperative care on a COVID-free orthopaedic ward. Hip fracture surgeries were considered aerosol-generating procedures and, therefore, at both sites full surgical personal protective equipment (PPE) as prescribed by NHS England were worn by theatre teams to protect patients and surgeons throughout.
We collected data during the COVID-19 pandemic in the UK for 30 days since launch of our two-site service on 31 March 2020. Audit approval was obtained from the department audit lead and the NHS Research Ethics Committee decision tool excluded ethics review. Electronic patient databases (Bluespier, eHandover, CyberLab, and Medway) and hip fracture proformas were used to maintain and collect accurate data.
The authors, based at each of the two sites, collected data for patient demographics, time to surgery, COVID-19 testing, length of stay (LOS), and mortality. Time to surgery was calculated from the time of first radiological confirmation of fracture to the start of anaesthesia. LOS was calculated from the day of hospital attendance to the day of discharge (or the day of death in such instances).
To objectively evaluate confounding factors between the two cohorts such as comorbidity and functional status, we also calculated the Nottingham Hip Fracture Score (NHFS) and the Clinical Frailty Scale (CFS) scores, which are both validated scoring systems.5,6 The NHFS, which ranges from 0 to 10, is a predictor of 30 day mortality and incorporates the following variables: age, sex, abbreviated mental test score, haemoglobin level on admission, place of residence (institution or other), comorbidities and if there is any evidence of active malignancy in the last 20 years. The CFS, which ranges from 0 to 9, is a predictor of inpatient mortality as well as for LOS and readmission rate in the elderly population. It incorporates the patient’s overall level of frailty and is recommended by National Institute for Health and Care Excellence (NICE) as part of the initial assessment of patients with suspected COVID-19 infection.7
Positive COVID-19 status was determined by presence of clinical symptoms and a single positive result for detection of SARS-CoV-2 S gene (VIASURE SARS-CoV-2 gene Real-Time PCR Detection Kit, CerTest Biotect) from nose or throat swab samples. COVID-19 status was considered negative in the presence of no clinical symptoms or two consecutive negative results. Method of testing is in accordance with national PHE guidance for COVID-19 testing.8
Statistical analysis of results was conducted using Fisher’s exact test for categorical data, Student’s unpaired t-test for continuous data and Grubb’s test for outliers, with significance at the 0.05 level and using both SPSS Statistics (IBM, Armonk, New York, USA) and Excel (Microsoft, Redmond, Washington, USA) software.
Results
In the 30 days after initiation of a two-site service in the COVID-19 pandemic, 47 patients presented to our trauma service with hip fractures (Figure 1). The number of monthly hip fracture admissions during the data collection period was not significantly different to that of the previous six months (mean 50.6, standard deviation (SD) 5.5, 43 to 59) (p > 0.05).
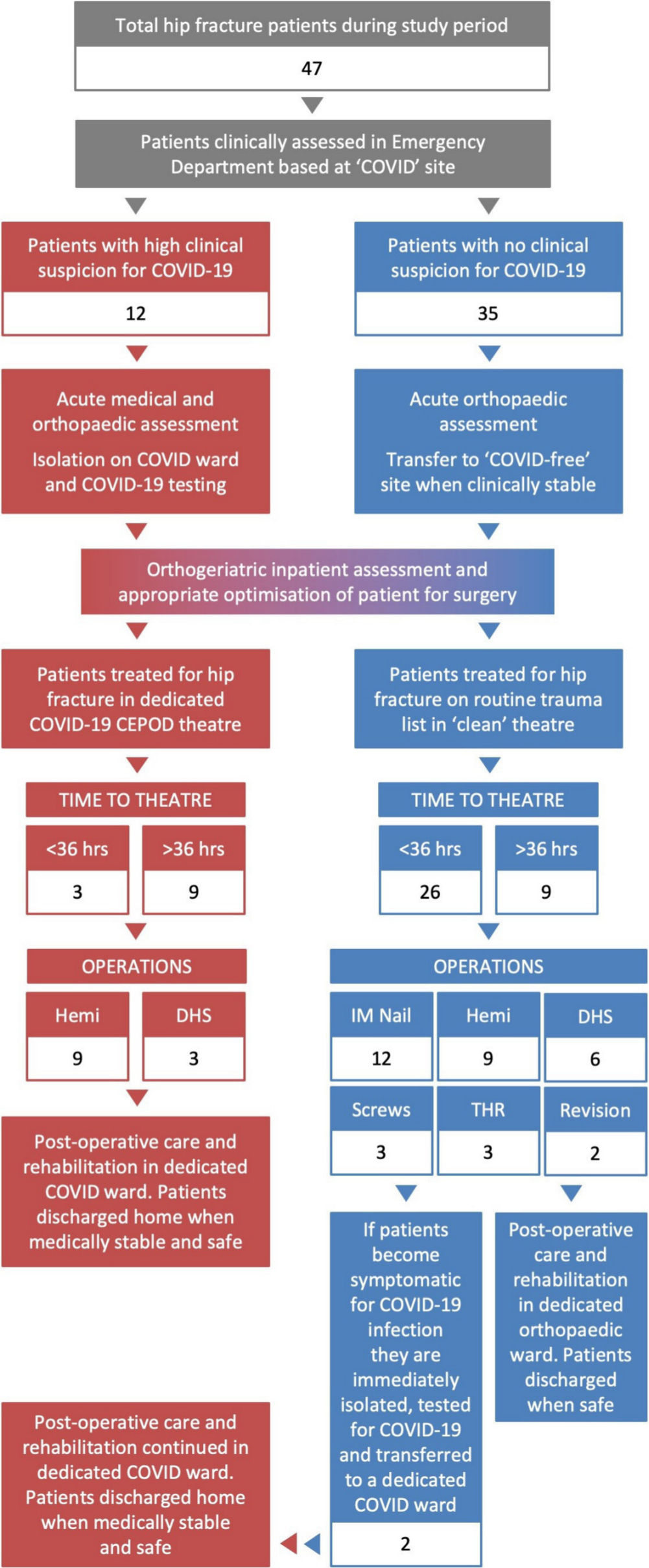
Fig. 1
Management algorithm for patients presenting with hip fractures during the 30 day study period and their flow through the two-site system. Hemi, hip hemiarthroplasty; DHS, dynamic his screw; Screws, cannulated hip screws; THR, total hip replacement; Revision, revision surgery for periprosthetic THR fracture.
Overall, 12 were admitted to the ‘COVID’ site and 35 patients admitted to the ‘COVID-free’ site. All patients received an orthogeriatric assessment within 72 hours of admission in accordance with National Institute for Health and Care Excellence (NICE) guidelines.9
At the ‘COVID site’, five (42%) males and seven (58%) females were admitted. Mean age was 86.8 years (79 to 100). At the ‘COVID-free’ site, 23 (66%) males and 12 (34%) females were admitted. Mean age was 78.5 years (37 to 96). There was a statistically significant difference between the cohort of patients at each site for age (p = 0.0427), but not for sex (p = 0.1822).
The mean CFS score at the ‘COVID’ site (5.7, 2 to 8) was higher than at the ‘COVID-free’ site (4.2, 2 to 7) (p = 0.0147). The mean NHFS score at the ‘COVID’ site (6.3, 3 to 8) was also higher than at the ‘COVID-free site (4.4, 1 to 7) (p = 0.0023).
Operations performed at both sites are presented in Table I. Statistically, no significant difference could be demonstrated between the two sites with respect to the type of operation performed (p = 0.0740).
Table I.
Summary of results from ‘COVID’ and ‘COVID-free’ sites.
| COVID Site | COVID-free Site | p-value† | |
|---|---|---|---|
| Patients (n = 47) | 12 | 35 | |
| Male | 5 | 23 | p = 0.1822 |
| Female | 7 | 12 | |
| Age (years) | |||
| Mean | 86.8 (SD 6.4) | 78.5 (SD 13.3) | p = 0.0427* |
| Range | 79 to 100 | 37 to 96 | |
| Operations | |||
| DHS | 3 | 6 | p = 0.0740 |
| Cannulated screws | 0 | 3 | |
| Hemiarthroplasty | 9 | 9 | |
| IM Nail | 0 | 12 | |
| THR | 0 | 3 | |
| Revision | 0 | 2 | |
| Time to surgery (hrs) | |||
| Mean | 52.8 (SD 30.1) | 29.8 (SD 26.1) | p = 0.0146* |
| Range | 18.8 to 119.5 | 4.6 to 152.4 | |
| Length of stay (days) | |||
| Mean | 12.6 (SD 7.7) | 8.7 (SD 3.8) | p = 0.0592 |
| Range | 4 to 28 | 3 to 24 | |
| Tested for COVID-19 | 12 | 24 | |
| Positive swab result | 6 | 0 | p = 0.0005* |
| Negative swab result | 6 | 24 | |
| Follow-up (days) | |||
| Mean | 27.3 | 24.7 | |
| Range | 12 to 41 | 12 to 41 | |
| Mortalities | 3 | 2 | p = 0.0971 |
-
DHS, dynamic hip screw; IM nail, intramedullary nail; THR, total hip arthroplasty; revision, revision operation for periprosthetic fracture or failure.
-
*
Statistically significant (p < 0.05)
-
†
Fisher’s exact test for categorical data, Student’s unpaired t-test for continuous data, and Grubb’s test for outliers.
The mean time to surgery at the ‘COVID’ site was 52.8 hours (18.8 to 119.0 hours). In comparison, the mean time to surgery at the ‘COVID-free’ site was less at 29.8 hours (4.6 to 152.4) and this was statistically significant (p = 0.0146). The mean LOS at the ‘COVID’ site was 12.6 days compared to 8.7 days at the ‘COVID-free’ site, but this was not statistically significant (p = 0.0592) (Figure 2).
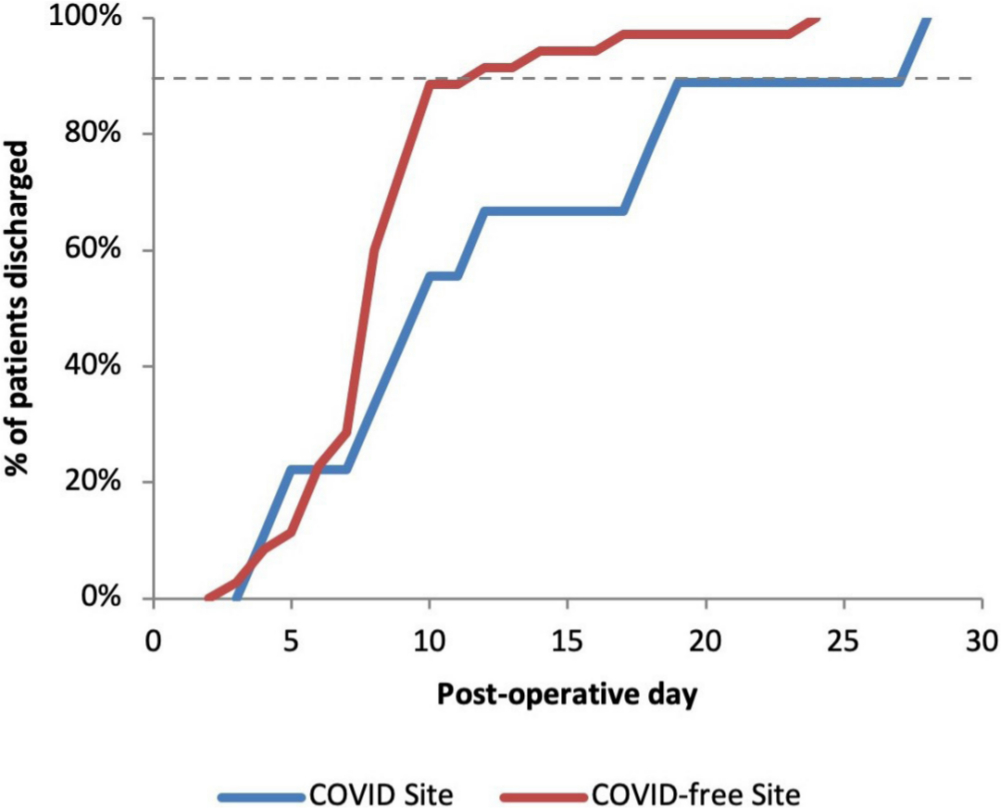
Fig. 2
Percentage of total patients discharged by postoperative day across ‘COVID’ and ‘COVID-free’ sites. At the ‘COVID-free’ site, 90% of patients were discharged by day ten and at the COVID-free site 90% were discharged by day 19.
The mean follow-up time at the ‘COVID-free’ site was 24.7 days (12 to 41 days) and at the ‘COVID’ site was 27.3 days (12 to 41). No patients at either site required high dependency unit or intensive care unit (HDU/ICU) admission. No re-admissions were recorded during the follow-up period.
Of the 12 patients treated at the ‘COVID’ site, six tested positive for COVID-19 infection (50%). Two patients at the ‘COVID’ site who had tested positive for COVID-19 infection, deteriorated with worsening respiratory symptoms. Both were managed at Level 0 (ward-based) care with palliative input and both recorded mortalities attributed to COVID-19 infection (postoperative days six and seven). A third patient who presented with symptoms suspicious for COVID-19 infection but tested negative, deteriorated with radiological features of aspiration pneumonia. This patient was also managed at Level 0 care and recorded a mortality attributed to aspiration pneumonia (postoperative day 3).
Patients at the ‘COVID-free’ site were tested only if they developed symptoms postoperatively or if it was later mandated for safe discharge into the social care system. In all, 26 of the 35 patients (74%) were tested for COVID-19 infection and none were positive. Two patients were tested after developing symptoms consistent with COVID-19 infection and both were isolated and subsequently transferred out of the ‘COVID-free’ site. Both tested negative for COVID-19 but due to ongoing deterioration, clinical suspicion of COVID-19 infection remained high and both continued to be treated as such. Treatment escalation plans were implemented with family input and both patients were treated at Level 0 care in a COVID-cohort ward. Both patients recorded mortalities (postoperative days six and eight) that were attributed to a clinical (but not virologically confirmed) diagnosis of COVID-19 infection.
There was a statistically significant difference in patients testing positive for COVID-19 infection between the two sites (p = 0.003). The total mortality rate across the two-sites was 10.6% (5/47) at mean follow-up of 24.7 days with no statistically significant difference between the two site (p = 0.0971).
Through the use of the ‘COVID-free’ site, over the 30-day study period, we were able to avoid 35 hip fracture admissions at the base ‘COVID’ site and created potential capacity for a total of 304 inpatient days for medical COVID patients.
Discussion
We identified the positive aspects of developing a two-site trauma service during the COVID-19 pandemic.
According to current NHS England guidelines, with the input of a physician, the orthopaedic team must clarify the current coronavirus status of every patient as either ‘treat as COVID-19’ or ‘treat as non-COVID-19’.3 This differentiation not only directs appropriate COVID-19 treatment to suspected or confirmed cases but, importantly, guides essential infection control measures and patient isolation. A two-site trauma service allowed ‘COVID-free’ patients to be treated separately to ‘COVID’ patients. This is akin to ‘ring-fenced’ orthopaedic beds and adheres to PHE guidance on inpatient placement to reduce the risk of transmission of COVID-19.4
We treated 47 hip fracture patients in the 30-day study period and this was not different from the number of patients treated in the previous six months (mean 50.6, p > 0.05). Therefore, the COVID-19 pandemic did not suppress the clinical demand for treating hip fracture patients.
Hip fracture patients are typically elderly, frail, live in nursing homes and have multiple comorbidities, placing them at higher risk of developing severe COVID-19 illness.1,2 The patients at the COVID site were significantly older by a mean of 8.3 years (p = 0.0427). This can be expected as there is an associated risk of COVID-19 infection with increased age.10
The mean time to surgery at the ‘COVID’ site was significantly higher than at the ‘COVID-free’ site (52.8 vs 29.8 hours respectively, p = 0.0146). This difference may be because ‘COVID’ site patients were older and required more medical optimisation for COVID-19 symptoms and for surgery. Specifically, the ‘COVID’ site cohort of patients also had significantly higher CFS and NHFS scores which both suggest poorer general health of the cohort. The NHFS, which has recently been independently validated by Rushton et al,11 is a predictor of 30-day mortality in hip fracture patients and therefore suggests that our ‘COVID’ site cohort are higher risk patients. Interestingly, of the components of the NHFS, the only significant difference (besides age as discussed previously) was the number of patients at the ‘COVID’ site normally living in an institutional setting (75% vs 14%, p = 0.0002) (Fig. 3). This might be expected given that care home residents are particularly vulnerable to COVID-19 as a consequence of their complex medical problems and advanced frailty.12
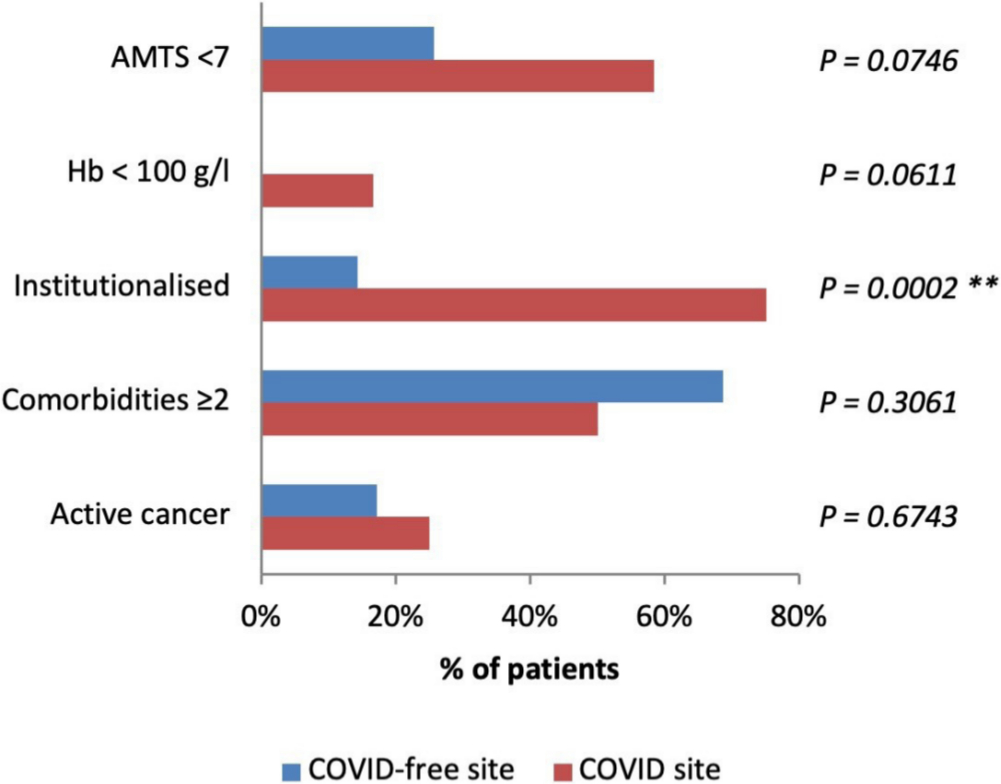
Fig. 3
Proportion of patients at the ‘COVID’ and ‘COVID-free’ sites with adverse features that contribute to a higher Nottingham Hip Fracture Score. The only statistically significant difference between the cohorts, besides age (Table 1), was the number of institutionalised patients (p = 0.0002). AMTS, abbreviated mental test score; Hb, haemoglobin; institutionalized, residing in any type of care facility; active cancer, history of active cancer in the past 20 years. **p < 0.005.
In response to the pandemic, clinical staff normally working in operating theatres were redistributed to support the increased demand. This limited the operating capacity to two emergency theatres – one COVID and one COVID-free. All specialities shared these theatres, where cases were prioritised as per the National Confidential Enquiry into Patient Outcome and Death (NCEPOD) classification for interventions and therefore contributed in delay to surgery for our hip fracture patients.
Overall, 25% of patients at the ‘COVID’ site and 74% of patients at the ‘COVID-free’ site had their hip fracture operation within the Best Practice Tariff (BPT) guidelines of 36 hours9 and this difference was statistically significant (Figure 4).
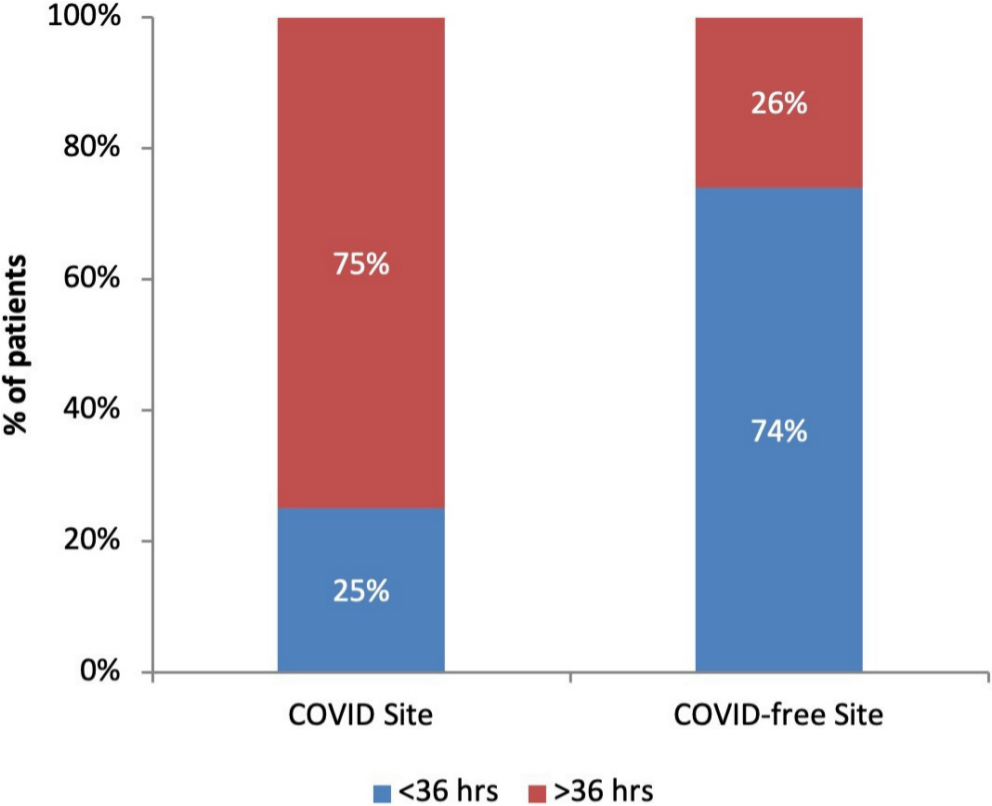
Fig. 4
Proportion of cases meeting the recommended Best Practice Tariff guidelines for time to surgery within 36 hours was significantly less at the ‘COVID’ site (25%) as compared to the ‘COVID-free’ site (74%) (p = 0.0048).
Metcalfe et al13 found that the BPT guidelines in the UK were associated with a reduced LOS and 30-day, 60-day, and 365-day mortality. A study by Leer-Salvesen et al based on the Norwegian Hip Fracture Register found that delay of surgery over 48 hours was significantly associated with increased three-day mortality and one-year mortality.14 Furthermore, prompt surgery within 24 hours of admission is shown to be independently associated with fewer pulmonary complications such as pneumonia, failure to extubate and shorter LOS.15 In the midst of an infectious respiratory disease pandemic, this correlation is crucially relevant and all measures to prevent further respiratory compromise must be considered. Timely surgical intervention for hip fracture patients is therefore a clinical priority in order to reduce morbidity and mortality. In our study, 61% (29 of 47) of patients received their surgery within 36 hours as compared to the national mean of 69% in March 2020.16 We were able to maintain provision of timely orthopaedic care despite dramatic changes to hospital operations in response to the pandemic.
Setting up a clean ‘COVID-free’ site reduces the risk of exposure of ward and theatre staff to COVID-19 and further transmission to the high-risk hip fracture patients. Furthermore, by operating in a dedicated ‘COVID-19’ theatre, we were able to reduce the time and resources needed for sufficient change in air flow and deep cleaning between ‘COVID’ and ‘COVID-free’ cases in theatre.
Since the study period, PHE advice on COVID-19 testing changed. From 16 April 2020, any patient discharged into social care should be tested and, since 27 April 2020 our local guidance changed to test all inpatients regardless of admission reason. 74% of patients at the ‘COVID-free’ site were therefore tested and none were positive. This suggests that the two-site approach is a valid infection control measure. However, it must be noted that despite none of the patients at the ‘COVID-free’ site testing positive, there were two mortalities and cause of death in both patients was clinically attributed to COVID-19 infection, despite negative swab results. This highlights the difficulty in confirming a clinical diagnosis and a high index of suspicion is crucial in preventing spread of the infection.
A retrospective multicentre study in Spain by Vives et al17 during the COVID-19 pandemic investigated the management of 136 hip fracture patients. The mean age of the patients was 85.3 years, which is comparable to our cohorts (‘COVID’ site: 86.8 years, ‘COVID-free’ site 78.5 years). As with our patients, in the Vives et al cohort, COVID-19 testing was only performed in patients with high clinical suspicion of infection. Therefore, 62 symptomatic patients were swabbed and 23 (37.1%) tested positive. In our study, all 12 patients at the ‘COVID’ site (symptomatic by definition) and two symptomatic patients from the ‘COVID-free’ site were swabbed: 6/14 (42.9%) patients tested positive. The number of symptomatic patients testing positive was not significantly different between the two studies (23/62 vs 6/14, p = 0.7645). However, overall the COVID positive rate in the Vives et al study was 16.9% (23/126) compared to 12.7% (6/47) in our cohort and this was significantly more (p = 0.0304).
By adapting our trauma service to two separate sites, we utilized human resources and a vacant private elective centre that were available due to cancellation of all elective orthopaedic operations. Crucially, this released 35 beds in the acute hospital and created capacity for a total of 304 inpatient days to support the COVID-19 demand. An alternative arrangement could have been to maintain orthopaedic services at the base site and allocate the beds and facilities at the private elective centre to the medical teams. This would meet the demand for COVID surge-planning and avoid the need for a split-site orthopaedic service. However, the two-site setup facilitated a geographical separation of ‘COVID’ and ‘COVID-free’ orthopaedic teams to reduce the risk of cross-infection between the cohorts. Furthermore, the skill mix of the staff at the private hospital were deemed better suited to managing surgical patients than COVID-19 patients.
Other groups have implemented similar models. Giorgi et al,18 based in Milan, Italy, described their experiences in reorganization of their trauma service in response to the increased demand for ICU capacity during pandemic. Orthopaedic resources were rationed in order to increase capacity for treating COVID-19 patients. COVID-19 specific ‘clean’ and ‘dirty’ pathways were set up with the aims to reduce risk of COVID-19 infection in trauma patients, time to surgery and LOS.
Delivering a two-site trauma service is not without its challenges.
Patients streamed to our ‘COVID-free’ site required ambulance transfer and with limited ambulance transportation during the pandemic, transfer time may be longer than usual. Our results showed that despite this, 74% of hip fracture patients at the ‘COVID-free’ site received their surgery within the BPT guidelines of 36 hours.9 The financial implication of missing the 36-hour target is potential loss of income for our unit.19 Currently, if all six of the BPT criteria are met (of which the 36-hour target is one), there is an additional payment of £1,335 per patient above the base tariff.19 Since 26% of cases at the ‘COVID-free’ site missed the target, this equates to approximately £12,000 of lost income in a 30-day period; as a result, much focus is placed on meeting the 36-hour target.
Four out of the five mortalities between the two sites were attributed to COVID-19 infection, with all patients having postoperative worsening of respiratory symptoms consistent with COVID-19 pneumonia. A retrospective study of 34 patients in China showed that patients who underwent surgery during the incubation period of COVID-19 developed pneumonia after surgery.20 However, in our ‘COVID’ site cohort, the patients had already been deemed symptomatic and therefore could be considered to be beyond the incubation period, making direct comparison difficult.
Orthopaedic human resources had to be divided between two sites to safely staff the operating theatres and wards, however, with elective work cancelled the impact of this was minimal. One of the challenges faced at the ‘COVID-free’ site was that staff at the repurposed private hospital were less familiar with treating acute hip fracture patients. The change presented a learning curve for the ward clinical staff, as they were asked to work outside of their areas of expertise. The orthopaedic, nursing, and anaesthesia team supported each other with camaraderie and built strong working relationships to tackle the exceptional circumstances that we faced.
Limitations
The authors recognize the data collection period was in the early stages of the COVID-19 pandemic and also that the patient numbers for comparison are low. Re-evaluation after the pandemic will certainly add more statistical power to the evaluation of the outcomes.
There are a number of confounding factors which make direct comparison of outcomes at both sites challenging. The patient cohort at the ‘COVID’ site were older, scored higher on the CFS and NHFS, had more delay in time to surgery and, of course, 50% carried the burden of COVID-19 infection.
Furthermore, the ‘COVID’ site patients received postoperative care in a general COVID-cohort ward as compared to the ‘COVID-free’ site where patients recovered in a dedicated orthopaedic ward, with specialized physiotherapy and nursing input.
Conclusion
A two-site ‘COVID’ and ‘COVID-free’ trauma service is a safe and effective way of managing hip fractures during the coronavirus pandemic. Our experience shows that patients received surgical treatment for hip fractures in a timely fashion at both sites. At the ‘COVID-free’ site, the mean time to surgery was within the 36 hours of the Best Practice Tariff guidelines and all patients across both sites received orthogeriatric assessment within 72 hours in accordance to NICE guidelines.8 We were able to create ‘ring-fenced’ beds as an infection control measure to keep COVID-19 infections low.
We took advantage of unused elective orthopaedic ward and theatre capacity from the private sector, producing significant gains in medical bed capacity in response to the COVID-19 demand. The authors propose a two-site ‘COVID’ and ‘COVID-free’ model as a viable option for treating hip fracture patients.
References
1. Centers for Disease Control and Prevention . Coronavirus disease 2019 (COVID-19): people who are at higher risk for severe illness . 2020 . https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/groups-at-higher-risk.html (date last accessed 14 May 2020 ). Google Scholar
2. CDC COVID-19 Response Team . Preliminary Estimates of the Prevalence of Selected Underlying Health Conditions Among Patients with Coronavirus Disease 2019 - United States, February 12-March 28, 2020 . MMWR Morb Mortal Wkly Rep . 2020 ; 69 ( 13 ): 382 – 386 . Crossref PubMed Google Scholar
3. . Clinical guide for the perioperative care of people with fragility fractures during the coronavirus pandemic . https://www.england.nhs.uk/coronavirus/wp-content/uploads/sites/52/2020/03/C0086_Specialty-guide-_Fragility-Fractures-and-Coronavirus-v1-26-March.pdf (date last accessed 14 May 2020 ). Google Scholar
4. Public Health England Guidance Reducing the risk of transmission of COVID-19 in the hospital setting . https://www.gov.uk/government/publications/wuhan-novel-coronavirus-infection-prevention-and-control/reducing-the-risk-of-transmission-of-covid-19-in-the-hospital-setting#patient-placement---inpatient-settings (date last accessed 14 May 2020 ). Google Scholar
5. Maxwell MJ , Moran CG , Moppett IK . Development and validation of a preoperative scoring system to predict 30 day mortality in patients undergoing hip fracture surgery . Br J Anaesth . 2008 ; 101 ( 4 ): 511 – 517 . Crossref PubMed Google Scholar
6. Rockwood K , Song X , MacKnight C , et al. A global clinical measure of fitness and frailty in elderly people . CMAJ . 2005 ; 173 ( 5 ): 489 – 495 . Crossref PubMed Google Scholar
7. COVID-19 rapid guideline . Critical care in adults NICE guideline [NG159] . https://www.nice.org.uk/guidance/ng159/chapter/1-Admission-to-hospital (date last accessed 14 May 2020 ). Google Scholar
8. GOV.UK Coronavirus (COVID-19) . Getting tested . https://www.gov.uk/guidance/coronavirus-covid-19-getting-tested#the-testing-process (date last accessed 14 May 2020 ). PubMed Google Scholar
9. National Institute for Health and Care Excellence Hip fracture . Management Clinical guideline [CG124] . https://www.nice.org.uk/guidance/cg124/chapter/Recommendations#timing-of-surgery (date last accessed 14 May 2020 ). Google Scholar
10. Kluge HHP, WHO Regional Director for Europe . Statement – Older people are at highest risk from COVID-19, but all must act to prevent community spread . http://www.euro.who.int/en/health-topics/health-emergencies/coronavirus-covid-19/statements/statement-older-people-are-at-highest-risk-from-covid-19,-but-all-must-act-to-prevent-community-spread (date last accessed 14 May 2020 ). Google Scholar
11. Rushton PRP , Reed MR , Pratt RK . Independent validation of the Nottingham hip fracture score and identification of regional variation in patient risk within England . Bone Joint J . 2015 ; 97-B ( 1 ): 100 – 103 . Crossref PubMed Google Scholar
12. British Geriatric Scoiety . COVID-19: Managing the COVID-19 pandemic in care homes for older people . https://www.bgs.org.uk/resources/covid-19-managing-the-covid-19-pandemic-in-care-homes (date last accessed 14 May 2020 ). Google Scholar
13. Metcalfe D , Zogg CK , Judge A , et al. Pay for performance and hip fracture outcomes . Bone Joint J . 2019 ; 101-B ( 8 ): 1015 – 1023 . Crossref PubMed Google Scholar
14. Leer-Salvesen S , Engesæter LB , Dybvik E , et al. Does time from fracture to surgery affect mortality and intraoperative medical complications for hip fracture patients? Bone Joint J . 2019 ; 101-B ( 9 ): 1129 – 1137 . Crossref PubMed Google Scholar
15. MC F , Boddapati V , Gausden EB , et al. Surgery for a fracture of the hip within 24 hours of admission is independently associated with reduced short-term post-operative complications . The Bone & Joint Journal . 2017 ; Sep;99-B ( 9 ): 1216 – 1222 . Crossref PubMed Google Scholar
16. NHFD - Charts & Reports . Part of the Falls and Fragility Fracture Audit Programme . https://www.nhfd.co.uk/20/NHFDCharts.nsf/vwCharts/BestPractice (date last accessed 14 May 2020 ). Google Scholar
17. Muñoz Vives JM , Jornet-Gibert M , Cámara-Cabrera J , et al. Mortality rates of patients with proximal femoral fracture in a worldwide pandemic . The Journal of Bone and Joint Surgery . 2020 ; 1 : 1 . Crossref PubMed Google Scholar
18. Di Martino A , Faldini C . Trauma service reorganization in bologna (Italy) during COVID-19 pandemic . Injury . 2020. Crossref PubMed Google Scholar
19. The National Hip Fracture Database Best Practice Tariff Guidance . https://www.nhfd.co.uk/20/nhfdcharts.nsf/vwInfo/Bestpractice (date last accessed 14 May 2020 ). Google Scholar
20. Lei S , Jiang F , Su W , et al. Clinical characteristics and outcomes of patients undergoing surgeries during the incubation period of COVID-19 infection . EClinicalMedicine . 2020 ; 100331 . Crossref PubMed Google Scholar
Author contributions
K. Chui: Wrote the paper, Collected the data.
S. Shankar: Senior editor.
A. Thakrar: Wrote the paper, Collected the data.
K. Chui and A. Thakrar contributed equally to this work.
Funding statement
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
Acknowledgements
The authors, K. Chui, A. Thakrar and S. Shankar, would like to acknowledge the contribution of all Trauma and Orthopaedic department team members at Barking, Havering and Redbridge University Hospitals NHS Trust and North East London Treatment Centre during the COVID-19 pandemic, including all anaesthetic, operating theatre, therapies, management and secretarial team members.
Consultants: A. Acharya, A. Ali, V. Beckles, K. Chin, J. Hambidge, S. Hassan, A. Kapoor, S. Masterson, G. Mazis, A. Parkar, K. Vemulapalli, J. Wong
Associate Specialists: B. Ahmed, A. Ali, I. Baloch, G. Bannerman, R. Imam, A. Majid, V. Raje, R. Ramadan, J. Salloum, R. Sriranganathan
Registrars: A. Ali, R. Cuthbert, C. Dott, D. Ferguson, G. Grammatopoulos, E. Karam, J. Peters, F. Shabani, L. Wickramarachchi, N. Woosnam
Senior House Officers: S. Akhter, A. Ali, S. Haque, P. Kariyawasam, M. Perera, M. Rahman, S. Shamah, S. Sivayoganathan, J. Skevofilax, T. Sultana
Trauma Facilitators: B. Boodoo, E. Douglas, K. Morris, C. Nazarie, J. Wilkins
Follow K. Chui @KarenKChui
Follow A. Thakrar @DrAmitThakrar
Follow S. Shankar @iShiva_Shankar
© 2020 Author(s) et al. This is an open-access article distributed under the terms of the Creative Commons Attributions licence (CC-BY-NC-ND), which permits unrestricted use, distribution, and reproduction in any medium, but not for commercial gain, provided the original author and source are credited.









