Abstract
Aims
COVID-19 has changed the practice of orthopaedics across the globe. The medical workforce has dealt with this outbreak with varying strategies and adaptations, which are relevant to its field and to the region. As one of the ‘hotspots’ in the UK , the surgical branch of trauma and orthopaedics need strategies to adapt to the ever-changing landscape of COVID-19.
Methods
Adapting to the crisis locally involved five operational elements: 1) triaging and workflow of orthopaedic patients; 2) operation theatre feasibility and functioning; 3) conservation of human resources and management of workforce in the department; 4) speciality training and progression; and 5) developing an exit strategy to resume elective work. Two hospitals under our trust were redesignated based on the treatment of COVID-19 patients. Registrar/consultant led telehealth reviews were carried out for early postoperative patients. Workflows for the management of outpatient care and inpatient care were created. We looked into the development of a dedicated operating space to perform the emergency orthopaedic surgeries without symptoms of COVID-19. Between March 23 and April 23, 2020, we have surgically treated 133 patients across both our hospitals in our trust. This mainly included hip fractures and fractures/infection affecting the hand.
Conclusion
The COVID-19 pandemic is not the first disease outbreak affecting the UK, nor will it be the last. The current crisis has necessitated rapid development of new hospital guidelines and early adaptive strategies in our services. Protocols and directives need to be formalized keeping in mind that COVID-19 will have a long and protracted course until a definitive cure is discovered.
Introduction
We are witnessing one of the deadliest disease outbreaks of the century so far. The world has seen the third coronavirus crisis in less than 20 years. SARS-CoV emerged in 2002, followed by MERS in 2012, and most recently COVID-19 in late 2019.1-3 This viral outbreak was reported in late December 2019 as a cluster outbreak in Wuhan, China, and has been linked to a wholesale wet market, although there are a number of other theories regarding its origin.3
The novel COVID-19 strain, which originated in China, has infected more than four million globally, which contributed to more than 280,000 deaths to date.4 The disease is now rampant in 212 nations, with authorities and medical workforces struggling to control the pandemic.4 The numbers are increasing almost exponentially on a daily basis as screening and diagnostic efforts are being stepped up.
The virus has also affected thousands of health workers. As doctors, nurses, and other practitioners fall sick, there is an increased burden on an already stretched health service. Importantly, infected workers in the hospitals are increasingly being recognized as vectors for the spread of the virus. It is essential to recognize the role of surgical branches at this time.
At first glance, the role of an orthopaedic surgeon may not typically be thought of as frontline in the fight against a viral pandemic. However, there is a role for orthopaedic surgeons to play both in controlling the outbreak and in managing patients with emergency orthopaedic conditions and traumatic injuries who still require treatment.
Guidance regarding the continuation of orthopaedic procedures during the COVID-19 pandemic has come from a variety of organizations and has often been vague, putting the onus of decision-making on individual hospital systems as well as surgeons. There have been guidelines published by the British Orthopaedic Association (BOAST guidelines) and NHS England on the restructuring of outpatient services and theatres5,6 However, varying strategies have been adapted within departments, depending on the available resources and local infrastructure.
Methods
As the biggest university teaching hospital in Wales, our orthopaedic department has had to adapt dynamically to the challenges presented by the coronavirus pandemic. Surgeons needed to consider alternative ways to manage different aspects of urgent orthopaedic care. Changes to standard management plans were required to minimize both patient exposure to the virus and the overall impact on departmental resources. This article outlines the restructuring of our orthopaedic department during the coronavirus pandemic.
Five key areas were targeted within our unit:
-
Triaging and workflow of trauma patients.
-
Adaptation to theatre services.
-
Workforce reorganization.
-
Preservation of specialty training.
-
Developing an exit strategy to resume elective work.
Triaging orthopaedic patients
The two hospitals in our health board (Cardiff and Vale University Health Board (CAV UHB)) were redesignated based on where COVID-19 patients would be treated. The University Hospital of Llandough (UHL) and theatres were resourced to carry out routine trauma operating instead of elective operating. The University Hospital of Wales (UHW) was already a designated COVID-19 centre and was reserved for polytrauma, spinal injuries, and paediatric orthopaedics (based at the Children’s Hospital for Wales on the same site).
Minimizing hospital visits was of paramount importance. To achieve this, all patients were triaged virtually to reduce face-to-face contact to limit spread of coronavirus. All elective operations and elective clinics were stopped from 16 March 2020 until further notice in line with NHS guidance.
Registrar/consultant-led telephone consultations were carried out for early postoperative follow-ups to rule out early operative complications.
Virtual fracture clinic assessment (VFC) for all ambulatory trauma cases presenting to the emergency department were screened by a trauma consultant. Outcomes included either allocated appointment to trauma clinic, patient advice with access to future fracture clinic support with ‘an open access appointment’, or discharge from the clinic service. The VFC was very effective in reducing follow-up visits.
Outpatient/trauma clinics
Trauma clinics were shifted to our elective centre at UHL. Patients attending the outpatient clinic underwent screening for COVID-19 symptoms including a temperature check prior to entering the outpatient waiting area (Fig. 1). The area was re-organised to seat patients two metres apart in keeping with social distancing measures (Fig. 2). Patients followed the following workflow pattern (Fig. 3).

Fig. 1
Thermal scanning monitor.

Fig. 2
Outpatient waiting area.
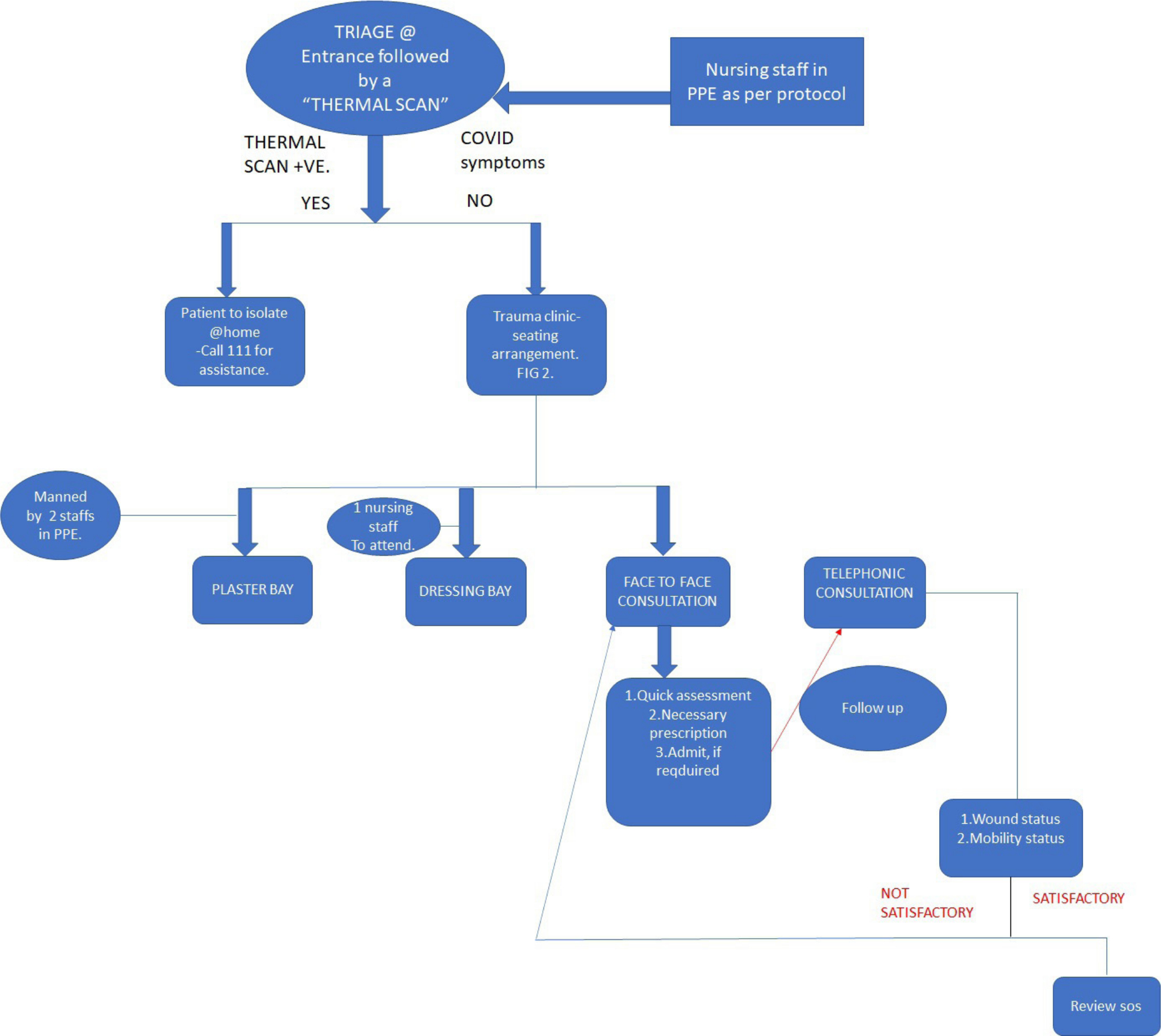
Fig. 3
Patients followed the following workflow pattern.
The patients attending A and E at UHW and requiring inpatient care followed the workflow/algorithm (Fig. 4).
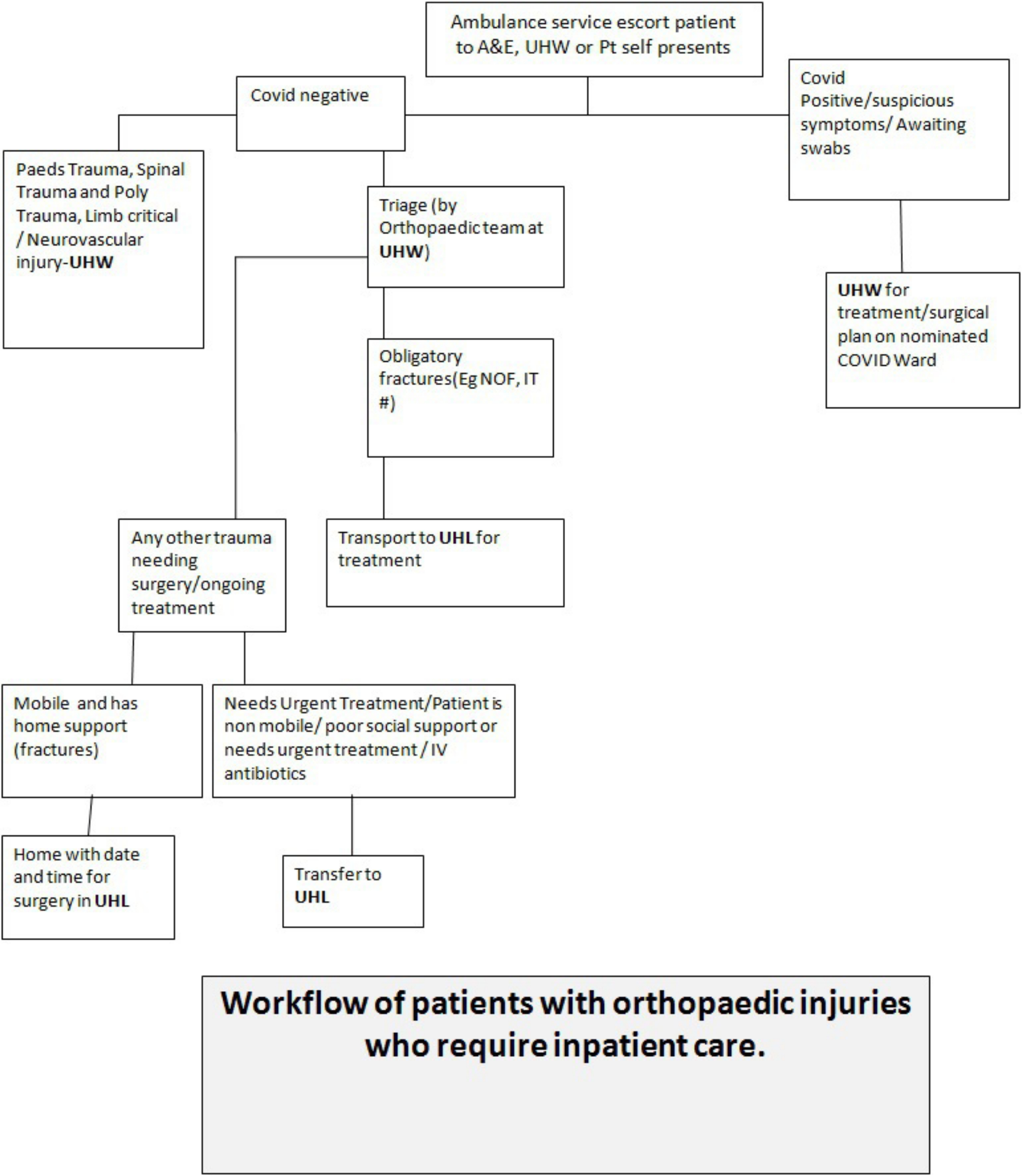
Fig. 4
Patients attending A&E at UHW and requiring inpatient care followed the workflow/algorithm.
The location for treating orthopaedic inpatients were based on whether the patient had symptoms of COVID-19. Patients who were suspected of COVID-19 or with confirmed COVID-19 requiring orthopaedic admission for surgery were treated at our main trauma hospital(UHW) Fig. 4. The rest of the inpatient care occurred at our previously elective orthopaedic centre (UHL).
The orthopaedic teams reviewed and treated the injured patients in line with national guidance published by BOAST and NHS England.6,7
Development of a dedicated operating space
Theatres were restructured to protect staff and allow patients care to be continued safely and effectively. The COVID-19 status of the patient determined the location of surgery. Patients who had symptoms of COVID-19 or were positive for COVID-19 had surgery performed at UHW. The operating theatre at UHL treated fragility fractures (including hip fractures) and ambulatory trauma. Logistically, this required trauma equipment to be procured or transferred to UHL, implant inventory to be stocked and scrub staff to be redeployed appropriately.
Our trauma meeting was conducted every morning at both sites, involving minimal medical personnel to allocate resources and prioritize the cases. This meeting included the anaesthetist designated for trauma theatre.
The operating theatres were reorganized to include a clean room, scrub room, donning area, and doffing area or dirty room.
An anteroom or clean room aided in exchange of medications, surgical trays and material for the case. Separate donning and doffing areas were designated in theatre (Fig. 5). Items such as phones and pagers were not allowed inside the theatre to reduce cross infection risk.
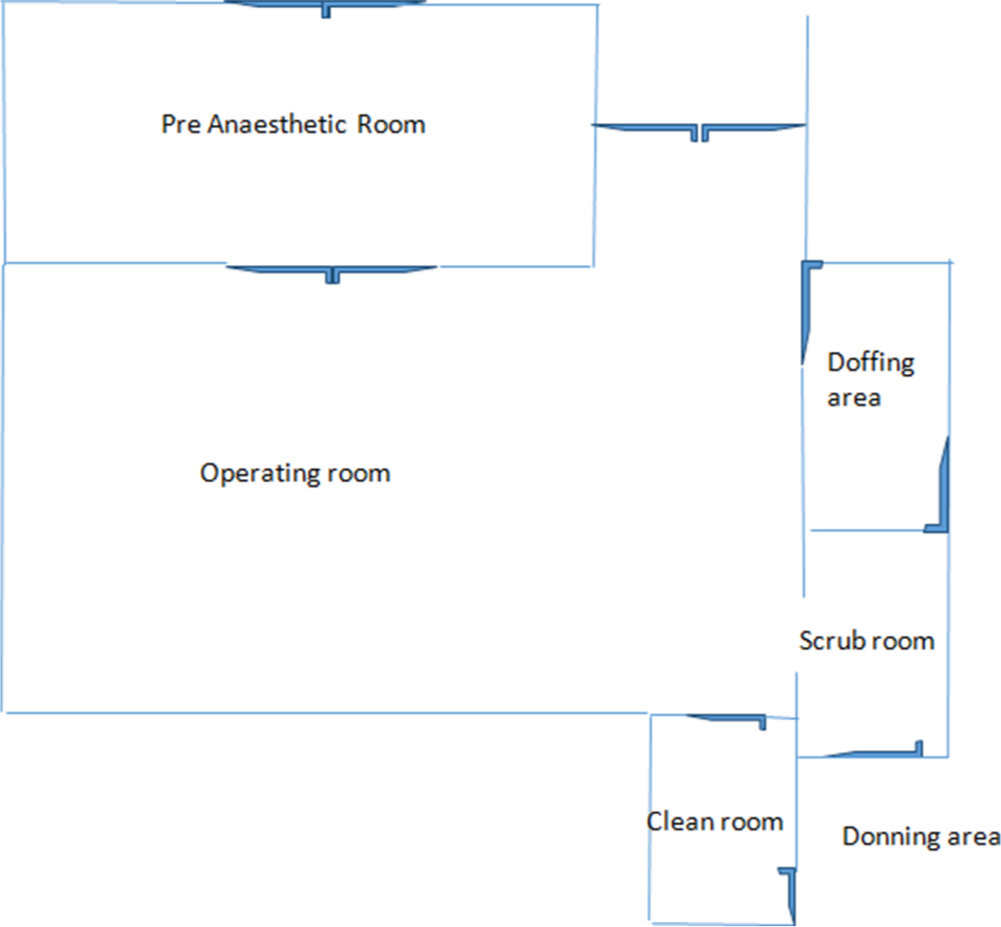
Fig. 5
Operation theatre design.
Generally positive pressure operating rooms with laminar air flow have been used in orthopaedics to lower the infection risk. There has been lively debate among orthopaedic surgeons surrounding the use of laminar flow theatres. However, no studies have concluded a clinical benefit of negative pressure over positive pressure operating rooms with regard to COVID-19.7 It is not easy to reverse engineer it either, although there are countries employing this strategy in the current scenario.8 As there were no concrete evidence or guidelines issued, we continued operating in laminar flow theatres.
All aerosol-generating surgical procedures regardless of the COVID status involved donning full PPE which included FFP3 masks, visor, surgical cap, and surgical gown as per the current guidelines. All traffic in and out of the theatre was minimized. A runner was dedicated to the operating theatre to provide all materials needed throughout the case and was stationed in the clean room. Consideration was given to surgical approaches which reduced surgical time and decreased operating staff exposure while maintaining safe practice. Procedures which involved either reaming or drilling were avoided if feasible. Surgical wounds were sutured with absorbable sutures to reduce follow-up requirements. A mobile image intensifier was used to screen intra-operatively, which reduced patient transfer distances within the hospital for peri-operative departmental radiographs. This also reduced the workload of radiographers who were increasingly required to perform portable chest radiographs for suspected/confirmed COVID-19 patients throughout the hospital. Additionally, to aid in air exchange, all providers who are not directly involved with intubation left the operating room prior to intubation and extubation. This necessary delay reduced theatre efficiency resulting in decreased utilization of theatre capacity compared to the normal elective theatre flow. Analysis and comparison of procedure times for common trauma operating such as a sliding hip screw, ankle fracture fixation and femoral nailing revealed an approximate increase of theatre time by 65% to 80%. For example, the average operative time of an ankle fracture fixation went up to three hours and 38 minutes in the current time compared to two hours in the months preceding COVID-19 . This lead to prolongation of the procedure time which is attributed to the additional time taken for donning and doffing and cleaning of theatre between cases.
The segregation of services came into effect realistically, after the announced lockdown on 23 March 2020. A total of 133 orthopaedic trauma procedures were performed across both hospital sites . In our study period (from 23 March to 23 April), 38 hip fragility fracture procedures were performed, split between UHL (63.2%, n = 24) and UHW (36.8%, n = 14), In comparison, 252 orthopaedic trauma procedures were performed at our trauma centre last year in the same time period. There were 12 patients who were positive for the RT PCR swab testing for SARS-CoV-2 RNA in the peri-operative period. Of these, four were swabbed pre-operatively. We had three COVID-19-related deaths in our cohort of operated patients across both hospital sites
On a positive note, our fragility fracture management seem to have improved with ‘ time to theatre’ for hip fracture reducing consistently and considerably as compared to the pre-COVID-19 months.
Management of orthopaedic workforce
During this unprecedented time, departments have a responsibility to ensure that NHS resources, including the availability of clinical staff, are utilized efficiently to ensure safe and effective patient care. Intra-departmental allocation and redeployment of human resources in this pandemic presented a logistical challenge. We redeployed various teams in the two hospitals based on both individual skill set and level of expertise. These included separate junior, middle grade & consultant rotas. Cancellation of elective services did free the middle grade and junior grade doctors, although an ongoing process of recruitment of junior doctors to COVID-19-related medical rotas placed extra stress on the system. Any consultants previously undertaking solely elective practice but with adequate expertise, were reinstated onto the main trauma rota. We had a 14 consultant on-call rota in place at at each of our two hospital sites in parallel. Due to the specialist nature of services offered by the spinal team at Cardiff, the consultants in the spinal unit had a separate designated spinal rota, independent from the trauma rota with their own junior support. Orthogeriatric services were shifted to UHL to support the peri-operative care of elderly and frail patients.
The changing landscape of the pandemic required a high degree of rota flexibility. A registrar was designated as ‘rota manager’ to formulate an appropriate rota every week. As of week four post-lockdown, our junior doctor (SHO) workforce had been reassigned to COVID-19 wards to care for medical patients. Staff sickness will continue to have an impact on the workforce. A clear procedure for illness reporting and staff testing is crucial to protect the health of staff and patients. Rota design required meticulous preparation and management and had to account for this with an appropriate degree of redundancy. Currently we are following a work pattern of ‘3-3-3’ which has three days and three nights with ‘cooling off period’ of three days in between. A ‘stand by’ registrar was incorporated into the rota to cover unexpected sickness absence. This schedule was applicable to the consultants as well. In both hospitals a consultant was assigned for the day to oversee the orthopaedic services along with support from a middle-grade registrar.
Speciality registrar training
It was inevitable that orthopaedic training and trainee progression would be affected. Orthopaedic subspeciality rotations and interhospital rotations had been stopped by mid-March. Currently, trainee involvement in theatre has been reduced in order to provide efficient consultant delivered care and reduce exposure times for aerosol generating procedures. With elective surgical procedures cancelled, this has had an impact on orthopaedic training and registrars surgical case logs. Creative solutions were required to maintain quality training. Attendance at online courses and webinars was encouraged. It was decided that regular teaching sessions would be conducted online through various video conferencing platforms. This negated the need for ‘gatherings’ and minimized the disruption to the teaching schedule. All case-based discussions (CBDs) critical to trainee progression are currently being conducted by trainers through these videoconferencing and online platforms.
Similar measures have commenced at other centres too.8,9 For skill-based specialities such as orthopaedics, viewing instructional videos and webinars should be encouraged and may be incorporated into the syllabus long term if found to be effective.
Strategies to restart orthopaedic elective services
There are plans afloat to think beyond the peak of this pandemic and divert attention to the urgent scheduled cases. These patients, mostly suffering from cancers and impending life-threatening conditions were discouraged to attend hospitals for fear of getting infected with viruses. Although few surgeries have continued in local private hospitals to contain the so-called ‘collateral damage’, the existing infrastructure has not allowed to deal with all urgent cases.
As an orthopaedic department, currently we have been ranked low in the ‘batting order’ as we do not deal with urgent non traumatic cases. The department has been asked to classify the current waiting list into categories where only patients with limb or career threatening conditions would be prioritised. The dilemma of subjecting patients to hospital acquired COVID-19 infection and providing them with pain relief by carrying out elective procedure is still being debated upon. Patients with progressive myelopathy are considered urgent and spinal surgeons have been allowed to operate with full personal protective equipment (PPE). Currently indication of re starting regular elective orthopaedic procedures are bleek. Our health board plans on resourcing orthopaedic theatres to deal with cardio thoracic and general surgical workload at the moment. The availability and comfort of using full PPEs including FFP3 masks for lengthy procedures are also being evaluated.
Conclusion
The COVID-19 pandemic is not the first disease outbreak affecting the UK, nor will it be the last. The role of orthopaedics in this fight should not be ignored. The current crisis has necessitated rapid development of new hospital guidelines and early adaptive strategies in our services. It has provided an opportunity for doctors to bond across different subspecialities and to work together as a unified medical fraternity.
Lessons in courage, empathy, tolerance, patience, and teamwork have been learnt. The importance of rational, pragmatic management plans while ensuring safe and effective patient care has been emphasized. At this challenging time, morale has remained high within the department with a strong culture of support, empathy, and proactivity between colleagues. Redeploying orthopaedic junior and middle-grade doctors onto medical wards gives an opportunity to revisit medical skills. For many, these may have been diluted over years of orthopaedic training but remain key skills in managing the peri-operative medical complications for our orthopaedic patients.
COVID-19 has not only been a great leveler but it has provided fantastic opportunities for continuing our professional development and education. Adapting to an ever-changing situation has been of paramount importance. Protocols and directives need to be formalized, keeping in mind that COVID-19 is here to stay for the foreseeable future and will impact both emergency and elective care.
It would be futile on our part to wait for a return to pre COVID-19 normality. The medical fraternity need to stand united and adapt their services to the ‘new normal’ in a post-COVID-19 era.
References
1. Zhong NS , Zheng BJ , Li YM , et al. Epidemiology and cause of severe acute respiratory syndrome (SARS) in Guangdong, people's Republic of China, in February, 2003 . Lancet . 2003 ; 362 ( 9393 ): 1353 – 1358 . Crossref PubMed Google Scholar
2. Al-Ahdal MN , Al-Qahtani AA , Rubino S . Coronavirus respiratory illness in Saudi Arabia . J Infect Dev Ctries . 2012 ; 6 ( 10 ): 692 – 694 . Crossref PubMed Google Scholar
3. Zhu N , Zhang D , Wang W , et al. A novel coronavirus from patients with pneumonia in China, 2019 . N Engl J Med . 2020 ; 382 ( 8 ): 727 – 733 . Crossref PubMed Google Scholar
4. Wuhan coronavirus outbreak . [Internet]2020[Cited 2020 May 10th ]. Available from: . https://www.worldometers.info/coronavirus/ Google Scholar
5. society BO . Management of patients with urgent orthopaedic conditions and trauma during the coronavirus pandemic.[Internet] 2020[cited 2020 March] Available from: . https://www.boa.ac.uk/uploads/assets/ee39d8a8-9457-4533-9774e973c835246d/COVID-19-BOASTs-Combined-v1FINAL.pdf Google Scholar
6. National Health service . Clinical guide for the management of trauma and orthopaedic patients during the coronavirus pandemic.[Internet] 2020[cited 2020 March ] Available from: . https://www.england.nhs.uk/coronavirus/wp-content/uploads/sites/52/2020/03/specialty-guide-orthopaedic-trauma-and-coronavirus-v1-16-march-2020.pdf Google Scholar
7. Baldock TE , Bolam SM , Gao R , et al. Infection prevention measures for orthopaedic departments during the COVID-2019 pandemic: a review of current evidence . Bone & Joint Open . 2020 ; 1 ( 4 ): 74 – 79 . Crossref PubMed Google Scholar
8. Liang ZC , Wang W , Murphy D , Hui JH . Novel coronavirus and orthopaedic surgery: early experiences from Singapore . JBJS Am . 2020 . Apr 7 . Crossref PubMed Google Scholar
9. Schwartz AM , Wilson J , Boden SD , et al. Managing resident workforce and education during the COVID-19 pandemic evolving strategies and lessons learned . JBJS Am . 2020 . Apr 7 . Google Scholar
Author contributions
N. J. Mathai: Conceptualization, Wrote and edited the manuscript.
A. S. Venkatesan: Conceptualization, Design, Wrote and edited the manuscript.
T. Key: Wrote and edited the manuscript.
C. Wilson: Edited the manuscript.
K. Mohanty: Conceptualization, Edited the manuscript.
Funding statement
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
ICMJE COI statement
N. Mathai reports being Senior Clinical Fellow, employed as an Orthopaedic Registrar Surgeon by Cardiff & Vale University Health Board, which is unrelated to this article. T. Key reports being employed as a Registrar Orthopaedic Surgeon at Cardiff and Vale University Health Board, which is unrelated to this article. K. Mohanty reports being a Trauma and Orthopaedic Consultant, employed as a Pelvic Trauma Surgeon by Cardiff & Vale University Health Board, which is unrelated to this article. A. Venkatesan reports being employed as Junior Clinical Fellow in trauma and orthopaedics by the Cardiff and Vale University, which is unrelated to this article. C. Wilson reports being a Trauma and Orthopaedic Consultant, employed as a Knee and Trauma Surgeon by Cardiff & Vale University Health Board, which is unrelated to this article.
Acknowledgements
None.
© 2020 Author(s) et al. This is an open-access article distributed under the terms of the Creative Commons Attributions licence (CC-BY-NC-ND), which permits unrestricted use, distribution, and reproduction in any medium, but not for commercial gain, provided the original author and source are credited.









