Abstract
Aims
Within the UK, around 70,000 patients suffer neck of femur (NOF) fractures annually. Patients presenting with this injury are often frail, leading to increased morbidity and a 30-day mortality rate of 6.1%. COVID-19 infection has a broad spectrum of clinical presentations with the elderly, and those with pre-existing comorbidities are at a higher risk of severe respiratory compromise and death. Further increased risk has been observed in the postoperative period. The aim of this study was to assess the impact of COVID-19 infection on the complication and mortality rates of NOF fracture patients.
Methods
All NOF fracture patients presenting between March 2020 and May 2020 were included. Patients were divided into two subgroup: those with or without clinical and/or laboratory diagnosis of COVID-19. Data were collected on patient demographics, pattern of injury, complications, length of stay, and mortality.
Results
Overall, 132 patients were included. Of these, 34.8% (n = 46) were diagnosed with COVID-19. Bacterial pneumonia was observed at a significantly higher rate in those patients with COVID-19 (56.5% vs 15.1%; p =< 0.000). Non respiratory complications such as acute kidney injury (30.4% vs 9.3%; p =0.002) and urinary tract infection (10.9% vs 3.5%; p =0.126) were also more common in those patients with COVID-19. Length of stay was increased by a median of 21.5 days in patients diagnosed with COVID-19 (p < 0.000). 30-day mortality was significantly higher in patients with COVID-19 (37.0%) when compared to those without (10.5%; p <0.000).
Conclusion
This study has shown that patients with a neck of femur fracture have a high rate of mortality and complications such as bacterial pneumonia and acute kidney injury when diagnosed with COVID-19 within the perioperative period. We have demonstrated the high risk of in hospital transmission of COVID-19 and the association between the infection and an increased length of stay for the patients affected.
Cite this article: Bone Joint Open 2020;1-11:669–675.
Take home message
COVID-19-positive hip fracture patients have a significantly higher risk of mortality than their negative counterparts.
The incidence of superadded bacterial pneumonia and acute kidney injury is high in hip fracture patients diagnosed with COVID-19.
There is a potentially high risk of in hospital transmission of COVID-19.
Introduction
The severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), also known as COVID-19, is a novel coronavirus first identified in December 2019 and has a broad spectrum of clinical presentations.1 Patients who are elderly, immunocompromised and those with pre-existing comorbidities are at a higher risk of severe complications and death from COVID-19 particularly in the postoperative period.2
Hip fractures are often a manifestation of increasing frailty and patients usually have multiple medical conditions. They have a significant 30 day mortality of around 10% and a mortality at one year at around 33%.3 Due to the complex needs of these patients and the significant associated mortality and morbidity, innovations have been devised to care for hip fracture patients. This includes multidisciplinary pathways and the best practice tariff that describe best standards of care. These include; surgery within 36 hours, joint orthopaedic/geriatric care, as well as bone protection and falls assessments.4
As a result of their frailty, hip fracture patients are at particularly high risk of severe complications if they contract COVID-19. The majority of patients admitted with hip fractures are not considered candidates for level two or three care due to frailty, and so for many of these patients the scope for intervention where there is respiratory compromise is more limited. Therefore, when exposed to a virus that can cause severe hypoxaemia there is a very real anticipated risk to life.5
This study collates is the largest dataset of hip fracture patients in one centre during the COVID-19 pandemic in the UK; collating perioperative clinical information on hip fracture patients and comparing postoperative outcomes and complications in those with and without COVID-19. The primary aim of the study was to identify the effect of COVID-19 on postoperative mortality. Further to this, the study sought to quantify the rates of complications, in particular those causing respiratory compromise.
Methods
Case identification
Cases were identified by contacting the hospital information services team who provided retrospective lists of patients under the care of the orthopaedic team who had tested positive by polymerase chain reaction (PCR) for COVID-19 on a rolling weekly basis. The data were collected in a period between 1 March 2020 and 31 May 2020. This was then cross-referenced with departmental lists of patients with a diagnosis of neck of femur fracture. Patients were separated into two groups: proven positive COVID-19 swabs or clinically suspected COVID-19, and patients with a negative swab and no clinical suspicion of COVID-19. Patients were included as positive if they were diagnosed between seven days pre-admission and 30 days post-admission. Patients who were negative on PCR testing but had clinical and radiological features of COVID-19 were identified by the orthogeriatric team. Definitions of hospital versus community transmitted infection are seen in Figure 1.6
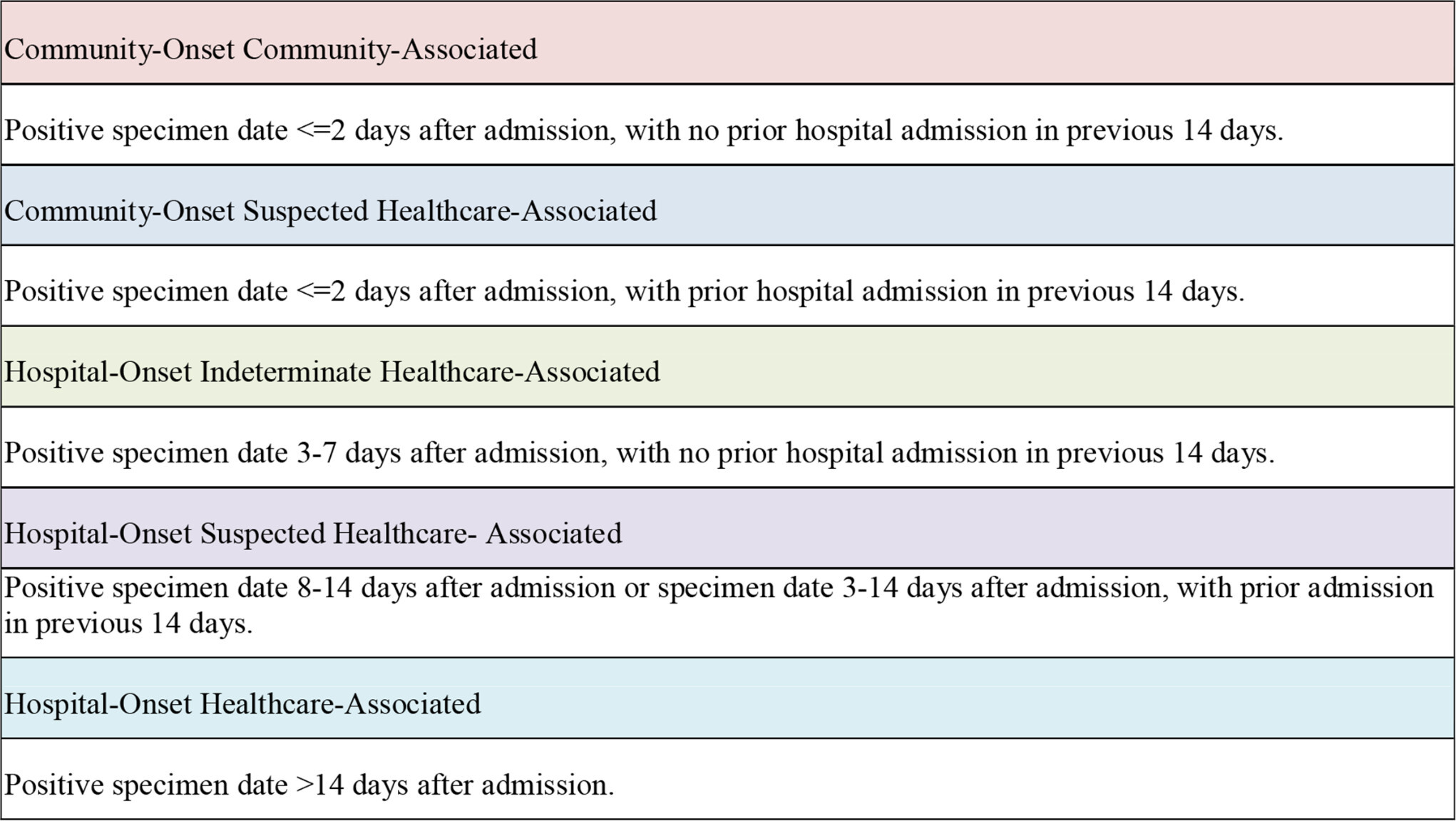
Fig. 1
Definitions of community versus hospital-acquired infection.6
Ethics
The study data were collected following approval from the clinical effectiveness unit based within Sheffield Teaching Hospitals (References STH21372 and 9921).
Outcomes
The primary outcome for this study was mortality at 30 days post-admission. Secondary outcomes to be assessed include rates of respiratory complications, including bacterial pneumonia, other complications, reintervention, and also the impact of infection on patient length of stay.
Data collection
Data were collected on patient demographics, comorbidities and social history. Further information was collected about any recent admissions, timing of symptoms and management of fracture.
Statistical analysis
Patient demographics were compared using simple statistical analysis. The incidence of outcomes such as mortality and complications were compared using chi squared or Fisher’s exact test where appropriate. Continuous data was compared using Mann-Whitney U test to be resilient to outliers. Significance was set at p < 0.05.
Results
Patient demographics
Over the study period, 132 patients with neck of femur fracture were admitted. In all, 46 patients (34.8%) had a clinical diagnosis of COVID-19, with the majority being confirmed on laboratory testing (n = 41, 89.1%). The mean age of patients identified was 82.1 years (49 to 100), and 27.3% (n = 36) of patients were male (Table I).
Table I.
Patient demographics.
| Variable | COVID-19-positive patients (n = 46) | Non-COVID-19-positive patients (n = 86) | All patients (n = 132) | p-value |
|---|---|---|---|---|
| Age yrs, mean ± SD | 83.4 ± 9.8 | 81.4 ± 10.7 | 82.1 ± 10.5 | 0.229* |
| Male, n (%) | 12 (26.1) | 24 (27.9) | 36 (27.3) | 0.822† |
| Residency, n (%) | ||||
| Own home/sheltered housing | 33 (71.7) | 68 (79.1) | 101 (76.5) | 0.343† |
| Residential/care home | 13 (28.3) | 17 (19.8) | 30 (22.7%) | 0.267† |
| Other institution | 0 (0.0) | 1 (1.2) | 1 (0.8) | 1.000† |
| ASA, n (%) | ||||
| 2 | 1 (2.2) | 12 (14.0) | 13 (9.8) | 0.009† |
| 3 | 33 (71.7) | 40 (46.5) | 73 (55.3) | |
| 4 | 12 (26.1) | 34 (39.5) | 46 (34.8) | |
| Clinical Frailty Score, n (%) | ||||
| 1 to 3 | 1 (2.2) | 10 (11.6) | 11 (8.3) | 0.009† |
| 4 to 6 | 19 (41.3) | 49 (57.0) | 68 (51.5) | |
| 7 to 9 | 26 (56.5) | 27 (31.4) | 53 (40.2) | |
| Nottingham Hip Fracture Score, n (%) | ||||
| Not applicable ( < 65 years) | 1 (2.2) | 1 (1.2) | 2 (1.6) | 0.957† |
| 0.7% | 1 (2.2) | 1 (1.2) | 2 (1.6) | |
| 1.1% | 1 (2.2) | 4 (4.8) | 5 (3.8) | |
| 1.7% | 0 (0.0) | 1 (1.2) | 1 (0.8) | |
| 2.7% | 1 (2.2) | 6 (7.0) | 7 (5.3) | |
| 4.4% | 6 (13.2) | 15 (17.4) | 21 (15.9) | |
| 6.9% | 11 (23.9) | 21 (24.4) | 32 (24.2) | |
| 11% | 9 (19.6) | 16 (18.6) | 25 (18.9) | |
| 16% | 14 (30.5) | 14 (16.3) | 28 (21.2) | |
| 24% | 2 (4.4) | 5 (5.8) | 7 (5.3) | |
| 34% | 0 (0.0) | 2 (2.3) | 2 (1.6) | |
| Diabetes mellitus, n (%) | 8 (19.4) | 17 (19.8) | 25 (18.9) | 0.739† |
| Pulmonary disease, n (%) | 15 (32.6) | 18 (20.9) | 33 (25) | 0.139† |
| Chronic kidney disease, n (%) | 9 (19.6) | 17 (19.8) | 26 (19.7) | 0.977† |
| Ischaemic heart disease, n (%) | 39 (84.8) | 46 (53.5) | 85 (64.4) | 0.0003† |
| Dementia, n (%) | 23 (50) | 29 (33.7) | 52 (39.4) | 0.068† |
| Active cancer, n (%) | 10 (21.7) | 13 (15.1) | 23 (17.4) | 0.339† |
-
*
Mann-Whitney U test.
-
†
Chi squared.
Patient comorbidities and social history
The most common comorbidity overall was ischaemic heart disease which was present in 64.4% of all patients and was observed at a significantly higher rate in the COVID-19 positive subgroup (p= 0.0003) (Table I). Similar rates of diabetes and chronic kidney disease were observed between the two groups with non-significantly higher rates of diagnoses of pulmonary disease and active cancer being observed in the COVID-19 group. The majority of patients were from their own home (75%). For those patients admitted from care there was no significant difference between the two groups, with 28% of COVID-19-positive patients coming from care/nursing homes in comparison to 21% of COVID-19-negative patients (p = 0.267).
On admission to hospital, the patient’s Clinical Frailty score (CFS) and Nottingham Hip Fracture score (NHFS) scores were calculated. Of the COVID-19-positive patients, a significantly higher proportion of patients had higher CFS than their negative COVID-19 counterparts (p= 0.009). The range of NHFS were similar between the two groups (p = 0.957).
Injury pattern and fracture management
Within both subgroups there were a similar proportion of patients with intertrochanteric fractures with more variation in the fracture anatomy seen in extracapsular injuries (Table II). The majority of patients were managed operatively with five patients (3.8%) being treated conservatively due to being unfit for surgery, one due to severity of COVID-19 infection on admission. Full details of operation types are seen in Table III. Of the patients fit enough for operative management, 81.1% had their operation within 36 hours of admission (n = 103). Of the remaining 24 patients, ten required medical optimization/reversal of anticoagulants, nine needed to wait for theatre space, three required further imaging/investigations and two waited for an appropriate surgeon to undergo a total hip arthroplasty. Of the patients who were COVID-19-negative, 22% (n = 18) had a delay to theatre in comparison to 13.3% (n = 6) of those who were positive (p = 0.263).
Table II.
Fracture pattern (p = 0.208).
| Site of fracture | COVID-19-positive patients (n = 46), n (%) |
Non-COVID-19-positive patients (n = 86), n (%) |
All patients (n = 132), n (%) |
|---|---|---|---|
| Intracapsular | 26 (56.5) | 47 (54.7) | 73 (55.3) |
| A1 pertrochanteric | 8 (17.4) | 7 (8.1) | 15 (11.4) |
| A2 pertrochanteric | 6 (13.0) | 22 (25.6) | 28 (21.2) |
| A3 pertrochanteric | 6 (13.0) | 10 (11.6) | 16 (12.1) |
Table III.
Fracture management (p = 0.114).
| Intervention | COVID-19-positive patients (n = 46), n (%) |
Non-COVID-19-positive patients (n = 86), n (%) |
All patients (n = 132), n (%) |
|---|---|---|---|
| Total arthroplasty | 1 (2.2) | 11 (12.8) | 12 (9.1) |
| Hemiarthroplasty | 23 (50.0) | 27 (31.4) | 50 (37.9) |
| Dynamic hip screw | 13 (28.3) | 34 (39.5) | 47 (35.6) |
| Cannulated hip screw | 3 (6.5) | 3 (3.5) | 6 (4.5) |
| Intramedullary nail | 5 (10.9) | 7 (8.1) | 12 (9.0) |
| Non-operative | 1 (2.2) | 4 (4.7) | 5 (3.8) |
In the postoperative period, one COVID-19-negative patient had a planned admission to the high dependency unit (1.2%). They had a CFS of 7 and an ASA of 4, with increasing oxygen demands due to pre-existing lung disease. This decision was made proactively via multi-disciplinary discussion involving the orthopaedic, orthogeriatric and anaesthetic teams.
Timing of diagnosis of COVID-19
Nine patients had symptoms of COVID-19 upon admission to hospital (19.6%). The timing of diagnosis for the majority of patients (n = 28; 60.8%) suggested in hospital transmission due to current length of stay or recent prior admission (Figure 1 and Table IV).
Table IV.
Hospital versus community transmission.
| Site of transmission | COVID-19-positive patients (n = 46), n (%) |
|---|---|
| Community-onset community-associated | 8 (17.4) |
| Community-onset suspected healthcare-associated | 4 (8.7) |
| Hospital-onset indeterminate healthcare-associated | 6 (13.0) |
| Hospital-onset suspected healthcare-associated | 18 (39.1) |
| Hospital-onset healthcare-associated | 10 (21.7) |
30-day mortality
In all, 37% (n = 17) of COVID-19 positive patients died within 30 days of sustaining a hip fracture compared to 10.5% (n = 9) of COVID-19 negative patients (chi squared; p <0.000). Of the COVID-19-positive patients who passed away, all but three of the patients had COVID-19 listed on their death certificate as a contributing factor (n = 14; 30.4%). Overall, 26 out of 132 patients (19.7%) died within 30 days of their injury.
Pulmonary complications
Within 30 days after operation, five patients developed pulmonary embolism (3.8%). Two of these patients had a diagnosis of COVID-19 as opposed to three who did not (chi squared p = 1.000). COVID-19 patients, however, demonstrated significantly increased rates of bacterial pneumonia treated with antibiotics according to trust protocol (56.5% vs 15.1%; chi squared p = < 0.00001) and acute respiratory distress syndrome (8.7% vs 0%; Fishers exact test p = 0.014) compared to patients who did not have COVID-19.
Other complications
Overall, 16.7% of patients with a hip fracture developed an acute kidney injury (AKI). 30.4% of CV19 patients developed an AKI, as opposed to 9.3% of non-COVID-19 patients who developed an AKI (chi squared p = 0.002). A single patient had a cerebrovascular accident and another required surgical reintervention in the COVID-19 group. No non-COVID-19 patients experienced these complications (Table V). Overall, COVID-19 patients had a rate of 87% for developing any complication, compared to 33.7% in non-COVID-19 patients (chi squared p < 0.01).
Table V.
Complication and mortality rates.
| Complication | COVID-19-positive patients (n = 46), n (%) |
Non-COVID-19-positive patients (n = 86) |
All patients (n = 132), n (%) |
p-value |
|---|---|---|---|---|
| Superficial wound infection | 1 (2.2) | 0 (0) | 1 (0.8) | 0.353* |
| Deep wound infection | 0 (0) | 0 (0) | 0 (0) | 1.000* |
| Wound dehiscence | 0 (0) | 0 (0) | 0 (0) | 1.000* |
| Pulmonary embolism | 2 (4.3) | 3 (3.5) | 5 (3.8) | 1.000* |
| Bacterial pneumonia | 26 (56.5) | 13 (15.1) | 39 (29.5) | < 0.000† |
| Acute respiratory distress syndrome | 4 (8.7) | 0 (0) | 4 (3.0) | 0.014* |
| Acute kidney injury | 14 (30.4) | 8 (9.3) | 22 (16.7) | 0.002† |
| Urinary tract infection | 5 (10.9) | 3 (3.5) | 8 (6.1) | 0.126* |
| Myocardial infarction | 0 (0) | 0 (0) | 0 (0) | 1.000* |
| Cerebrovascular accident | 1 (2.2) | 0 (0) | 1 (0.8) | 0.353* |
| Reintervention | 1 (2.2) | 0 (0%) | 1 (0.8) | 0.353* |
| Death within 30 days | 17 (37.0) | 9 (10.5) | 26 (19.7) | < 0.000† |
| Overall number of patients with complications (including death) | 40 (87.0) | 29 (33.7) | 69 (52.3) | < 0.000† |
-
*
Fishers exact test.
-
†
Chi squared.
Length of stay
Patients with a diagnosis of COVID-19 had an extended median length of stay of 21.5 days (1 to 75) compared to a median of ten days (2 to 67) in patients who were not diagnosed with COVID-19 (Mann-Whitney U test, p < 0.000).
Discussion
COVID-19 infection in hip fracture patients is associated with a higher 30-day mortality compared to COVID-19-negative counterparts. Our study has shown that over a third of patients (37%, n = 17) with a COVID-19-positive diagnosis died within 30 days of their admission to hospital. Our findings of increased 30-day mortality in COVID-19-positive hip fracture patients are consistent with other studies in the UK and USA showing early mortality rates between 30% to 56%.7-9 Within this study, however, high rates of diagnosis of IHD were observed in the COVID-19-positive subgroup (p= 0.0003). This has not been observed in previously published studies and may have contributed to the higher rate of mortality in those infected with COVID-19.10
For the COVID-19-positive patients included in this study, there was a significantly higher rate of bacterial pneumonia and/or respiratory distress in comparison to their COVID-19-negative counterparts (p= 0.0004). The 56.5% rate seen within this cohort is similar to what has been observed within an international pan-surgical study, where 512.% (n = 577) of patients suffered with bacterial pneumonia (diagnosed clinically and treated according to local microbiology protocols) and/or acute respiratory distress within the perioperative period.2 However, within the hip fracture specific literature, these high rates have not been previously observed with studies demonstrating comparable rates to 201911 and much lower rates of 13.4%.7
With regards to non-pulmonary complications, there was a significantly increased rate of perioperative AKI for patients who were diagnosed as COVID-19-positive (p = 0.002). It has been documented within the literature that the infection has an impact on renal function with more than 40% of patients having abnormal proteinuria at the time of being diagnosed as COVID-19 positive. This condition has been associated with increased risk of inpatient mortality with more elderly, male and those patients with comorbidities being at a higher risk of death.11 Careful fluid input and output monitoring has been advocated within guidance produced by the National Institute of Clinical Excellence (NICE)12 to reduce the risk of this complication; however, the pathophysiology is not yet fully understood.13
The extended patient length of stay within this study may be due to the increased morbidity associated with the complications of COVID-19. This seems to be in concordance with current literature; a study by Kayani et al7 demonstrated an extended length of stay in COVID-19 patients, with inpatient admissions being double that of COVID-19-negative patients. In this study, another factor affecting the length of stay for care and nursing home patients were ever-evolving changes in criteria for patient flow to intermediate community rehabilitation services. Due to the emerging evidence on COVID-19 infection, the criteria for patients to successfully step down to a community rehabilitation bed kept constantly changing, including the introduction of criteria including a wait of 14 days in hospital. As well as the change in guidelines, the increased incidence of co-morbidities like IHD and increased frailty (CFS) within the COVID-19-positive subgroup may have led patients to require a longer length of stay and therefore predisposed them to nosocomial COVID-19. This is an area which requires further research.
Within this study, 17.4% (n = 8) of hip fracture patients were admitted with symptoms of COVID-19 and became symptomatic within two days with no prior hospital admission. This rate is lower than what has been previously observed, with 26% of patients having been symptomatic in a national multicentre study.14 One challenge of COVID-19, is the long incubation periods which some patients experience, being much longer than that of influenza (1.4 days).15 Typically, the incubation period of COVID-19 is five to six days but has been reported to be as long as 14 to 19 days.16,17 This has the potential to lead to some patients becoming symptomatic during their inpatient stay, despite being infected prior to admission. This long incubation period, in combination with the potential for spread from asymptomatic or paucisymptomatic patients, also makes COVID-19 a potent nosocomial threat, especially in an environment containing a large proportion of elderly or comorbid individuals. In this study, many patients appear to have contracted COVID-19 within the hospital environment, despite adoption of cohort bays and wards18 and staff personal protective equipment being used in line with UK government guidance.19 The multidisciplinary team (consisting of orthopaedics, orthogeriatrics, microbiology, infection control, and senior nursing staff) also proactively identified the risks of nosocomial transmission, reporting weekly figures and adjusting cohort ward and bay use accordingly.
Within our cohort of patients, 80.3% (n = 103) of patients were operated on within 36 hours who were treated operatively which is comparable to other studies.14,20 Five patients in our cohort were treated non-operatively; four patients were not fit for an anaesthetic secondary to respiratory compromise (one patient was COVID-19-positive) and one patient being bed bound and comfortable. During COVID-19, the theatre capacity within our establishment changed significantly with initially only having one theatre list per day but demand resulted in increasing this capacity during the latter stages of COVID-19 to a maximum of three trauma lists on some days due to hip fracture care and other general orthopaedic trauma. There were 24 patients who did not receive operative intervention within 36 hours (nine due to lack of time; four patients required 48 hours following anticoagulation; two patients awaiting MRI; two patients awaiting surgery for total hip arthroplasty; six patients required further optimization medically; one awaiting COVID-19 swab preoperatively). Our COVID-19 swab precautions changed throughout, with patients initially having to wait for COVID-19 swab results prior to operative treatment, but this was only during the early stages of COVID-19. Swab results did not result in delays in the latter stages of COVID-19 due to increased access to testing.
It should be considered when analyzing the data that it was collected from clinical notes and electronic patient systems. The accuracy of data collected was based on what had been documented by the medical team, but as they are used to direct clinical practice it can be expected that they are at an established standard. COVID-19 PCR sensitivity can vary based on specimen quality and test performed.21 During the study period, a dual target assay with high sensitivity and specificity was used at Sheffield Teaching Hospitals.22 Due to an international shortage of extraction reagents, extraction-free PCR was run on a large proportion of samples from mid-April, with an approximate 5% reduction in diagnostic sensitivity as a consequence.
This study has shown that patients with a neck of femur fracture have a high rate of mortality and complications such as bacterial pneumonia and AKI when diagnosed with COVID- 19 within the perioperative period. We have demonstrated the high risk of in hospital transmission of COVID-19 and the association between the infection and an increased length of stay for the patients affected.
References
1. Sun P , Lu X , Xu C , Sun W , Pan B . Understanding of COVID-19 based on current evidence . J Med Virol . 2020 ; 92 ( 6 ): 548 – 551 . Crossref PubMed Google Scholar
2. Nepogodiev, Dmitri, COVIDSurg Collaborative . Mortality and pulmonary complications in patients undergoing surgery with perioperative SARS-CoV-2 infection: an international cohort study . Lancet . 2020 ; 396 ( 10243 ): 27 – 38 . Crossref PubMed Google Scholar
3. Moran CG , Wenn RT , Sikand M , Taylor AM . Early mortality after hip fracture: is delay before surgery important? J Bone Joint Surg Am . 2005 ; 87 ( 3 ): 483 – 489 . Crossref PubMed Google Scholar
4. British Orthopaedic Association and the British Geriatric Society . The care of patients with fragility fracture. blue book publication by the British orthopaedic association , 2007 . Google Scholar
5. Gattinoni L , Chiumello D , Caironi P , et al. COVID-19 pneumonia: different respiratory treatments for different phenotypes? Intensive Care Med . 2020 ; 46 ( 6 ): 1099 – 1102 . Crossref PubMed Google Scholar
6. Meredith LW , Hamilton WL , Warne B , et al. Rapid implementation of SARS-CoV-2 sequencing to investigate cases of health-care associated COVID-19: a prospective genomic surveillance study . Lancet Infect Dis . 2020 ( 14 ): S1473-3099(20)30562 – S1473-3099(20)30564 . Crossref PubMed Google Scholar
7. Kayani B , Onochie E , Patil V , et al. The effects of COVID-19 on perioperative morbidity and mortality in patients with hip fractures . Bone Joint J . 2020 ; 102-B ( 9 ): 1136 – 1145 . Crossref PubMed Google Scholar
8. Williams JT , Kumar A . The effect of the COVID-19 pandemic on hip fracture care. British orthopaedic association . 2020 . https://www.boa.ac.uk/policy-engagement/journal-of-trauma-orthopaedics/journal-of-trauma-orthopaedics-and-coronavirus/the-effect-of-the-covid-19-pandemic-on-hip.html (date last accessed 9 October 2020 ). Google Scholar
9. LeBrun DG , Konnaris MA , Ghahramani GC , et al. Hip fracture outcomes during the COVID-19 pandemic: early results from New York . J Orthop Trauma . 2020 ; 34 ( 8 ): 403 – 410 . Crossref PubMed Google Scholar
10. Macey ARM , Butler J , Martin SC , et al. 30-Day outcomes in hip fracture patients during the COVID-19 pandemic compared to the preceding year . Bone & Joint Open . 2020 ; 1 ( 7 ): 415 – 419 . Crossref PubMed Google Scholar
11. Cheng Y , Luo R , Wang K , et al. Kidney disease is associated with in-hospital death of patients with COVID-19 . Kidney Int . 2020 ; 97 ( 5 ): 829 – 838 . Crossref PubMed Google Scholar
12. NICE guidelines . COVID-19 rapid guideline: acute kidney injury in hospital . 2020 . https://www.nice.org.uk/guidance/ng175/resources/covid19-rapid-guideline-acute-kidney-injury-in-hospital-pdf-66141962895301 (date last accessed 9 October 2020 ). Google Scholar
13. Ronco C , Reis T , Husain-Syed F . Management of acute kidney injury in patients with COVID-19 . Lancet Respir Med . 2020 ; 8 ( 7 ): 738 – 742 . Crossref PubMed Google Scholar
14. Hall AJ , Clement ND , Farrow L , et al. IMPACT-Scot report on COVID-19 and hip fractures . Bone Joint J . 2020 ; 102-B ( 9 ): 1219 – 1228 . Crossref PubMed Google Scholar
15. Lessler J , Reich NG , Brookmeyer R , et al. Incubation periods of acute respiratory viral infections: a systematic review . Lancet Infect Dis . 2009 ; 9 ( 5 ): 291 – 300 . Crossref PubMed Google Scholar
16. Zhai P , Ding Y , Wu X , et al. The epidemiology, diagnosis and treatment of COVID-19 . Int J Antimicrob Agents . 2020 ; 55 ( 5 ): 105955 . Crossref PubMed Google Scholar
17. Backer JA , Klinkenberg D , Wallinga J . Incubation period of 2019 novel coronavirus (2019-nCoV) infections among travellers from Wuhan, China, 20-28 January 2020. Euro surveillance: bulletin Europeen sur les maladies transmissibles (European communicable disease bulletin) , 2020 . Google Scholar
18. Public Health England . COVID-19: infection prevention and control guidance . 2020 . https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/893320/COVID-19_Infection_prevention_and_control_guidance_complete.pdf (date last accessed 9 October 2020 ). Crossref PubMed Google Scholar
19. Chu DK , Akl EA , Duda S , et al. Physical distancing, face masks, and eye protection to prevent person-to-person transmission of SARS-CoV-2 and COVID-19: a systematic review and meta-analysis . Lancet . 2020 ; 395 ( 10242 ): 1973 – 1987 . Crossref PubMed Google Scholar
20. Malik-Tabassum K , Crooks M , Robertson A , et al. Management of hip fractures during the COVID-19 pandemic at a high-volume hip fracture unit in the United Kingdom . J Orthop . 2020 ; 20 : 332 – 337 . Crossref PubMed Google Scholar
21. Arevalo-Rodriguez I et al. False-Negative results of initial RT-PCR assays for Covid-19: a systematic review . medRxiv . 2020 : 04.16.20066787 . Crossref PubMed Google Scholar
22. Colton H , Ankcorn M , Yavuz M , et al. Improved sensitivity using a dual target, E and RdRP assay for the diagnosis of SARS-CoV-2 infection: experience at a large NHS Foundation trust in the UK . J Infect . 2020 : S0163-4453(20)30339-X . Crossref PubMed Google Scholar
Author contributions
A. E. Ward: Undertook statistical analysis, Wrote and reviewed the manuscript.
D. Tadross: Carried out statistical analysis, Wrote and reviewed the manuscript.
F. Wells: Carried out statistical analysis, Wrote and reviewed the manuscript.
L. Majkowski: Wrote and reviewed the manuscript.
U. Naveed: Wrote and reviewed the manuscript.
R. Jeyapalan: Wrote and reviewed the manuscript.
D. G. Partridge: Wrote and reviewed the manuscript.
S. Madan: Wrote and reviewed the manuscript.
C. M. Blundell: Wrote and reviewed the manuscript.
Funding statement
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
Acknowledgements
The authors would like to thank Cristina Lagaron-Manso for her assistance with data collection.
Follow A. E. Ward @Ward89A
© 2020 Author(s) et al. This is an open-access article distributed under the terms of the Creative Commons Attribution Non-Commercial No Derivatives (CC BY-NC-ND 4.0) licence, which permits the copying and redistribution of the work only, and provided the original author and source are credited. See https://creativecommons.org/licenses/by-nc-nd/4.0/.









