Abstract
Introduction
Virtual fracture clinics (VFCs) are being increasingly used to offer safe and efficient orthopaedic review without the requirement for face-to-face contact. With the onset of the COVID-19 pandemic, we sought to develop an online referral pathway that would allow us to provide definitive orthopaedic management plans and reduce face-to-face contact at the fracture clinics.
Methods
All patients presenting to the emergency department from 21March 2020 with a musculoskeletal injury or potential musculoskeletal infection deemed to require orthopaedic input were discussed using a secure messaging app. A definitive management plan was communicated by an on-call senior orthopaedic decision-maker. We analyzed the time to decision, if further information was needed, and the referral outcome. An analysis of the orthopaedic referrals for the same period in 2019 was also performed as a comparison.
Results
During the study period, 295 patients with mean age of 7.93 years (standard error (SE) 0.24) were reviewed. Of these, 25 (9.8%) were admitted, 17 (5.8%) were advised to return for planned surgical intervention, 105 (35.6%) were referred to a face-to-face fracture clinic, 137 (46.4%) were discharged with no follow-up, and seven (2.4%) were referred to other services. The mean time to decision was 20.14 minutes (SE 1.73). There was a significant difference in the time to decision between patients referred to fracture clinic and patients discharged (mean 25.25 minutes (SE 3.18) vs mean 2.63 (SE 1.42); p < 0.005). There were a total of 295 referrals to the fracture clinic for the same period in 2019 with a further 44 emergency admissions. There was a statistically significant difference in the weekly referrals after being triaged by the VFC (mean 59 (SE 5.15) vs mean 21 (SE 2.17); p < 0.001).
Conclusion
The use of an electronic referral pathway to deliver a point of care virtual fracture clinic allowed for efficient use of scarce resources and definitive management plan delivery in a safe manner.
Cite this article: Bone Joint Open 2020;1-6:293–301.
Introduction
Trauma and Orthopaedic Surgery performs the greatest volume of outpatient reviews in Ireland with almost 400,000 outpatient attendances per annum.1 The fracture clinic makes up a significant proportion of these attendances, and often the demands placed on the fracture service outstrip the available capacity. Delays in the initiation of appropriate management plans may adversely affect outcomes.2
Virtual fracture clinics (VFCs) have emerged as a novel, efficient, and cost-effective way of managing stable fractures which do not require ongoing orthopaedic intervention.2-6 They offer the ability for the orthopaedic service to remotely review and advise on injuries without the requirement for face-to-face outpatient visits. In our institution, a paediatric university hospital, the fracture and elective clinics run concurrently. The VFC had previously been demonstrated to reduce numbers in the outpatient setting, therefore, allowing for an increase in elective outpatient capacity.7
In institutions which have implemented VFCs, the reported reduction in fracture clinic workload is 22% to 33%.6,7 Others have similarly reduced the average number of outpatient attendances per fracture from 1.76 to 0.17–0.3 attendances.4,8 There are significant social effects of attending a fracture clinic with Breathnach et al9 demonstrating that 68% of the patients seen in the VFC would have had to take time off work to attend the fracture clinic and Morris and Bell10 showing that for every 100 attendances there were 54 days of school and 25 days of work lost. In the paediatric setting, the impact on education from missed school days is a particularly important factor.
The British Orthopaedic Association Standards for Trauma (BOAST) guidelines recommend that every new referral to the fracture clinic is seen within 72 hours of referral.11 VFCs offer the potential to achieve BOAST compliance by having a senior orthopaedic decision-maker review referrals and make appropriate onward management plans.12 The VFC also allows for the removal of inappropriate or unnecessary referrals to the fracture clinic.2 Up to 15% of all referrals to the fracture clinic are unnecessary,13 and our institution demonstrated 37% of fracture clinic referrals had no radiological evidence of fracture, and 25% of the fractures required no formal orthopaedic review.14 Other institutions have shown that up to 47% of referrals do not have definite evidence of a fracture.15 Removing these patients from the fracture clinic reduces waiting times for patients while maintaining patient-reported satisfaction scores from 78% to 98%.4,6,8,16-19
Changing the structure of any established service is difficult and involves input from multiple stakeholders,20 which can be fraught with planning difficulties. With the onset of the COVID-19 pandemic and the resulting cessation of all but essential outpatient activities and the requirement to reduce face-to-face contacts given the disease transmission mechanism, this offered a unique situation that required a technological solution.
The VFC model used at other sites was not implementable at our unit as we were unable to recruit senior nursing staff and physiotherapists, or have dedicated VFC times given the pandemic status. Therefore, a specific technological solution for our institution was designed using pre-existing technology, which we termed the Trauma and Orthopaedics ePlatform (TOP). Siilo (Siilo, Amsterdam, the Netherlands), a secure health care communication app which allowed for the discussion of cases in real-time, was identified. Clinical information, examination findings, and imaging were provided in a standard format on the online platform and a definitive plan set in place. Patients were admitted, discharged, given a date for planned day of surgery admission (DOSA) or brought for a face-to-face contact fracture clinic based on their TOP information. All patients were provided with a fracture specific information leaflet on discharge from the emergency department, and a copy of the ePlatform conversation uploaded to their electronic patient record.
We hypothesised that the use of TOP would result in a reduction in fracture clinic attendances, a reduction in the time taken to provide definitive management plans, and a higher discharge rate of stable fractures. We also believed this would be associated with a reduction in missed school days and loss of earnings for referred patients without an increase in complications or resources.
Methods
The aim was to explore a potential virtual solution that encompassed the safe discharge of patients from our emergency department (ED). A current patient flow map for potential orthopaedic trauma patients was constructed (Figure 1). By analyzing the pathway, applying a Lean methodology21 and utilizing an electronic platform, we were able to formulate a new referral approach for all orthopaedic presentations to the ED. These changes had to be implemented with no additional resources in a time-sensitive manner due to the COVID-19 pandemic that was driving change.
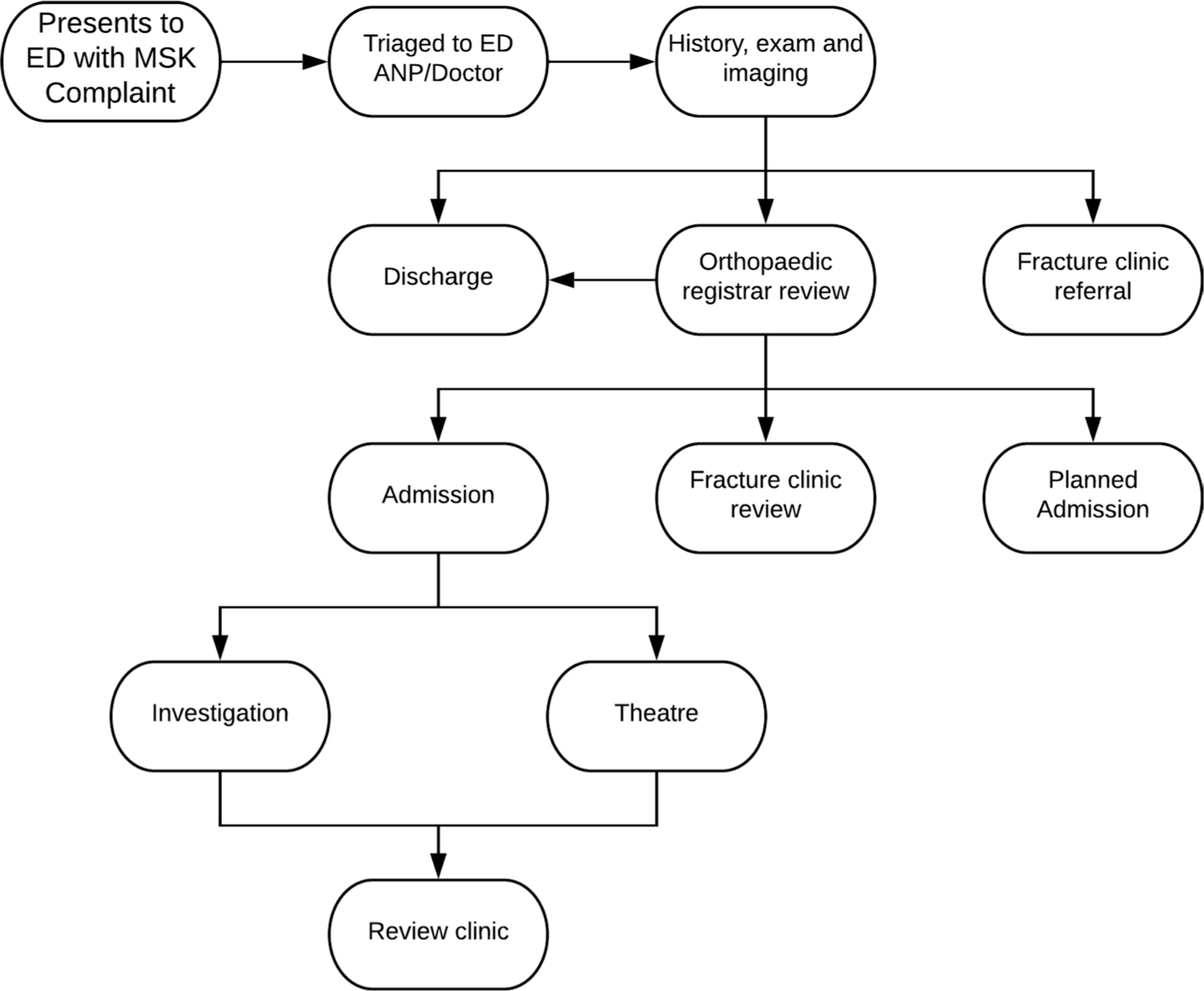
Fig. 1
Process map showing traditional orthopaedic referral pathway.
On 21 March 2020, all referrals to the fracture clinic were moved to the technological platform. A group discussion for all orthopaedic and ED medical teams was constructed. All referrals were made via this platform to senior on-call orthopaedic decision-makers (orthopaedic registrar and consultant). A secure communication app Siilo was identified. It complies with the General Data Protection Regulation (GDPR),22,23 has an interface that is intuitive to a new user, requires no additional training, and can structure referral messages into case files which are exportable as a PDF to the patients’ electronic patient record. Participants in the TOP group were added by consultants in emergency medicine and orthopaedic surgery, maintaining a closed network communication group. A new process map was constructed to represent this change and is presented in Figure 2. Any patient who the ED team felt required orthopaedic review was discussed using the TOP. There were 295 total referrals made in the period. 168 (56.95%) of these referrals were female patients, and 127 male (43.05%). The mean age was 7.93 years (0.24) (see Table I).
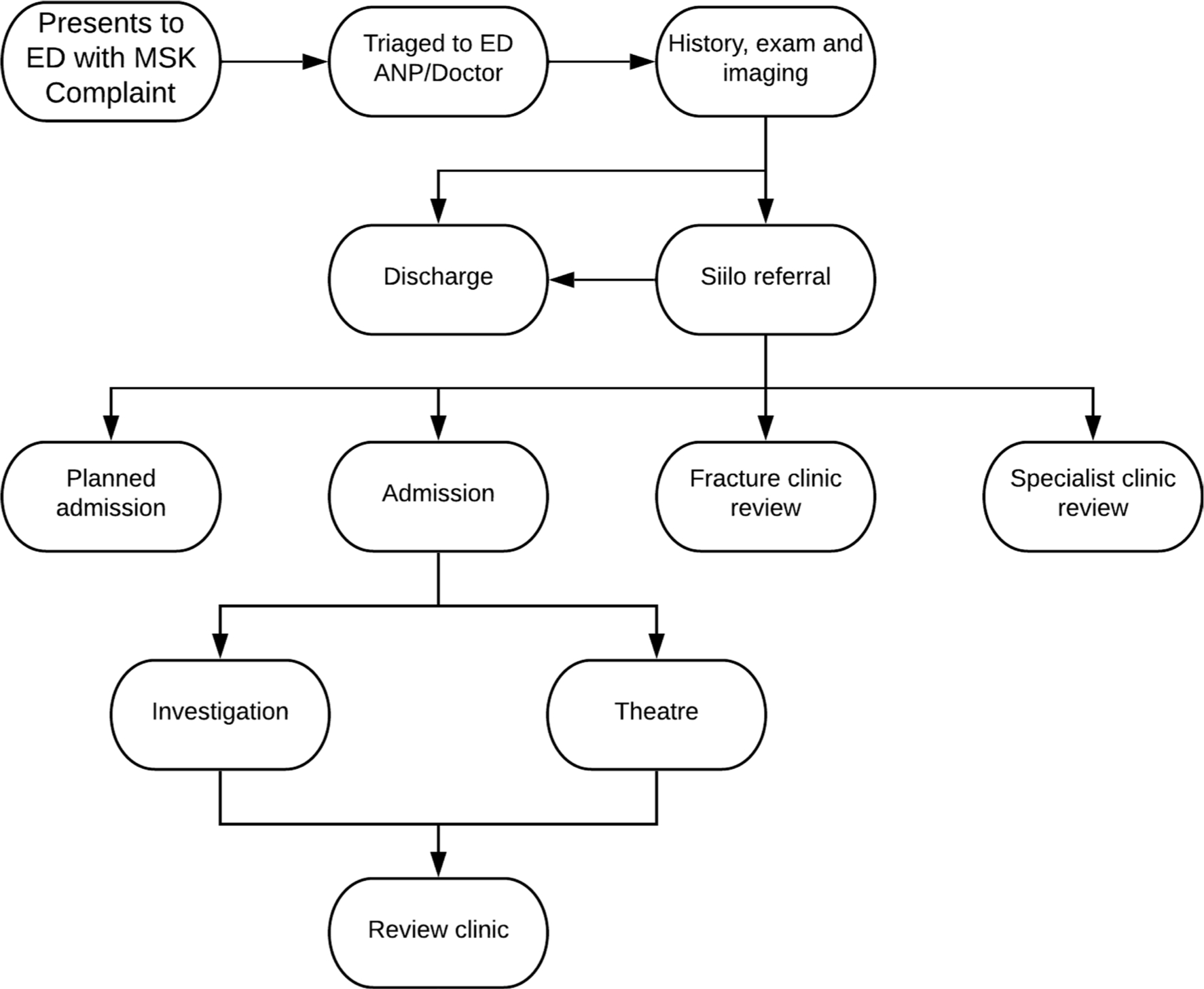
Fig. 2
Process map showing new referral pathway after implementation of the Trauma and Orthopaedic ePlatform (TOP). ANP, Advanced Nurse Practitioner; ED, emergency department; MSK, musculoskeletal.
Table I.
Patient demographics
| Demographics | Total |
|---|---|
| Female sex, n (%) | 168 (56.95) |
| Mean age (SE) | 7.93 (0.24) |
-
SE, standard error.
A separate anonymised database, created using Excel (Microsoft, Washington, USA), was used to prospectively collate the demographic and specific information about each referral made, including date of birth, time of referral, time of response, fracture characteristics, and outcome for all referrals for the first five weeks of the programme (from 21 March 2020 to 26 April 2020). Statistical analysis was performed using SPSS v. 26.0 (IBM, Armonk, New York, USA). Independent-samples t-tests and one-way ANOVA with Tukey post-hoc corrections were performed. Averages are presented as mean and standard error (SE). All data were stored on a secure Health Service Executive (HSE) server.
An interrupted time series (ITS) analysis was used to evaluate the effectiveness of the virtual intervention. Data about clinic attendances were collected for the equivalent time period in 2019 (25 March 2019 to 27 April 2019) and after the implementation of the TOP. The benefit of ITS analysis is that observed changes can be attributed to the intervention itself rather than by a separate trend in data.2
Results
Referral Outcomes
In total, 29 (9.8%) patients were reviewed by the on-call orthopaedic team and admitted directly from the emergency department, with all remaining patients returning home. A further 17 patients (5.8%) were given a date to return for a planned DOSA, 105 (35.6%) patients were given outpatient face-to-face fracture clinic appointments to ensure adequate healing, to monitor for growth disturbance or for removal of cast, seven patients (1.5%) were referred to a specialist clinic, and 137 (46.4%) were discharged with no need for orthopaedic follow-up (Table II).
Table II.
Outcomes of referrals on day of surgery admission (DOSA).
| Outcome | n (%) |
|---|---|
| Admitted | 29 (9.8) |
| Fracture clinic | 105 (35.6) |
| No orthopaedic follow-up | 137 (46.4) |
| Planned DOSA | 17 (5.8) |
| Referred to specialist clinic | 7 (2.4) |
| Total | 295 (100) |
Presence of fracture
Of the 295 referrals, 81 (27.5%) patients had no evidence of a fracture. A summary of the common types of fracture is shown in Table III. The presence of fracture by referral outcome is illustrated in Figure 3. Overall, 11 patients were admitted without the presence of a fracture. Nine of these patients were admitted as part of an infectious workup, one was admitted for investigation of a potential nonaccidental injury, and the remaining patient was a late presentation of Perthes’ disease24 admitted for MRI. One patient with no fracture returned for wound debridement, irrigation, and closure.
Table III.
Summary of injury location as referred from the emergency department.
| Site | Total, n | Fracture, n (%) | No fracture, n (%) |
|---|---|---|---|
| Upper Limb | |||
| Clavicle | 10 | 10 (100) | 0 (0) |
| Humerus | 9 | 7 (77.8) | 2 (22.2) |
| Elbow | 62 | 44 (71) | 18 (29) |
| Both bone forearm | 11 | 11 (100) | 0 (0) |
| Distal radiusradii | 46 | 42 (91.3) | 4 (8.7) |
| Phalanx/metacarpal | 9 | 9 (100) | 0 (0) |
| Thumb (PP, DP) | 11 | 11 (100) | 0 (0) |
| Lower Limb | |||
| Hip | 13 | 0 (0) | 13 (100) |
| Knee | 14 | 0 (0) | 14 (100) |
| Tibia | 30 | 21 (70) | 9 (30) |
| Ankle | 27 | 19 (70.4) | 8 (29.6) |
| Midfoot | 22 | 13 (59.1) | 9 (40.9) |
| Phalanx/metatarsal | 12 | 10 (83.3) | 2 (16.7) |
| Other | 19 | 14 (73.7) | 5 (26.3) |
-
DP, distal palanx; PP, proximal phalanx.
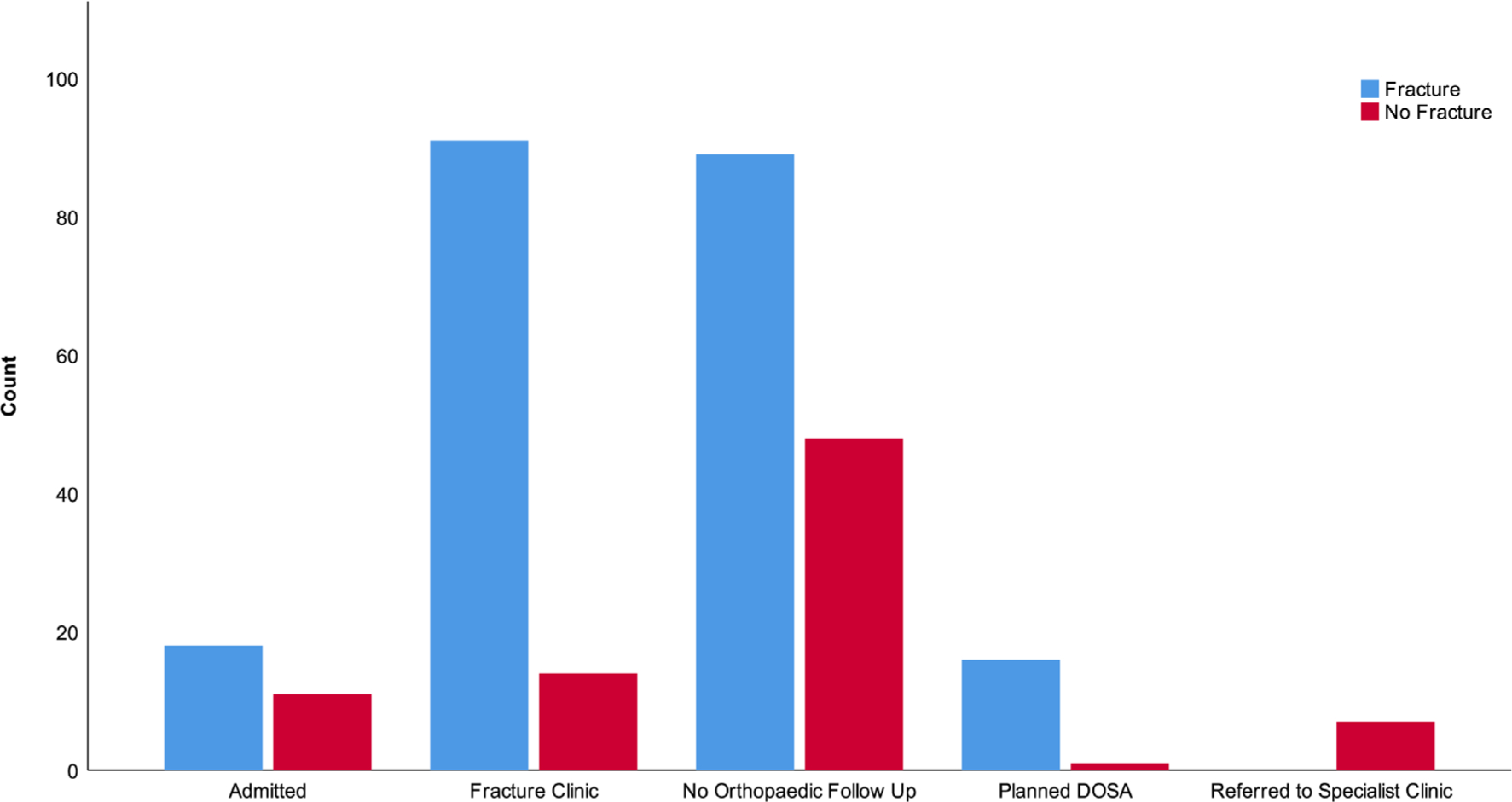
Fig. 3
Referral outcome by presence of fracture
Manipulation under conscious sedation in the ED
Overall, 17 patients underwent manipulation under conscious sedation in the ED for the application of a moulded cast. One patient (5.9%) was admitted post-manipulation for compartment review; the remaining patients were discharged from the ED to attend the fracture clinic. There was no return to theatre for further manipulation under anaesthesia of those discharged.
Time to management decision
The mean time to decision was 20.14 minutes (SE 1.73). In total, 265 (89.8%) cases required no further information while 26 (8.8%) required a mean 4.08 messages (SE 0.49) to reach a decision. A statistically significant difference in the time to decision was noted between the two groups (p = 0.013, independent-samples t-test). The average time for those requiring no further information and those requiring clarification were 17.56 minutes (SE 1.50) and 46.42 (SE 10.68), respectively. We note that our data is positively skewed (see Figure 4), and the median time to decision was 10 minutes (interquartile range (IQR) 8 to 23). Outlier data was assessed. On three occasions the on-call team were scrubbed and unavailable to answer via Siilo. On one occasion, a response time of 227 minutes was recorded; however, the on-call team had made reviewed the patient in ED but had not updated the Siilo case file.
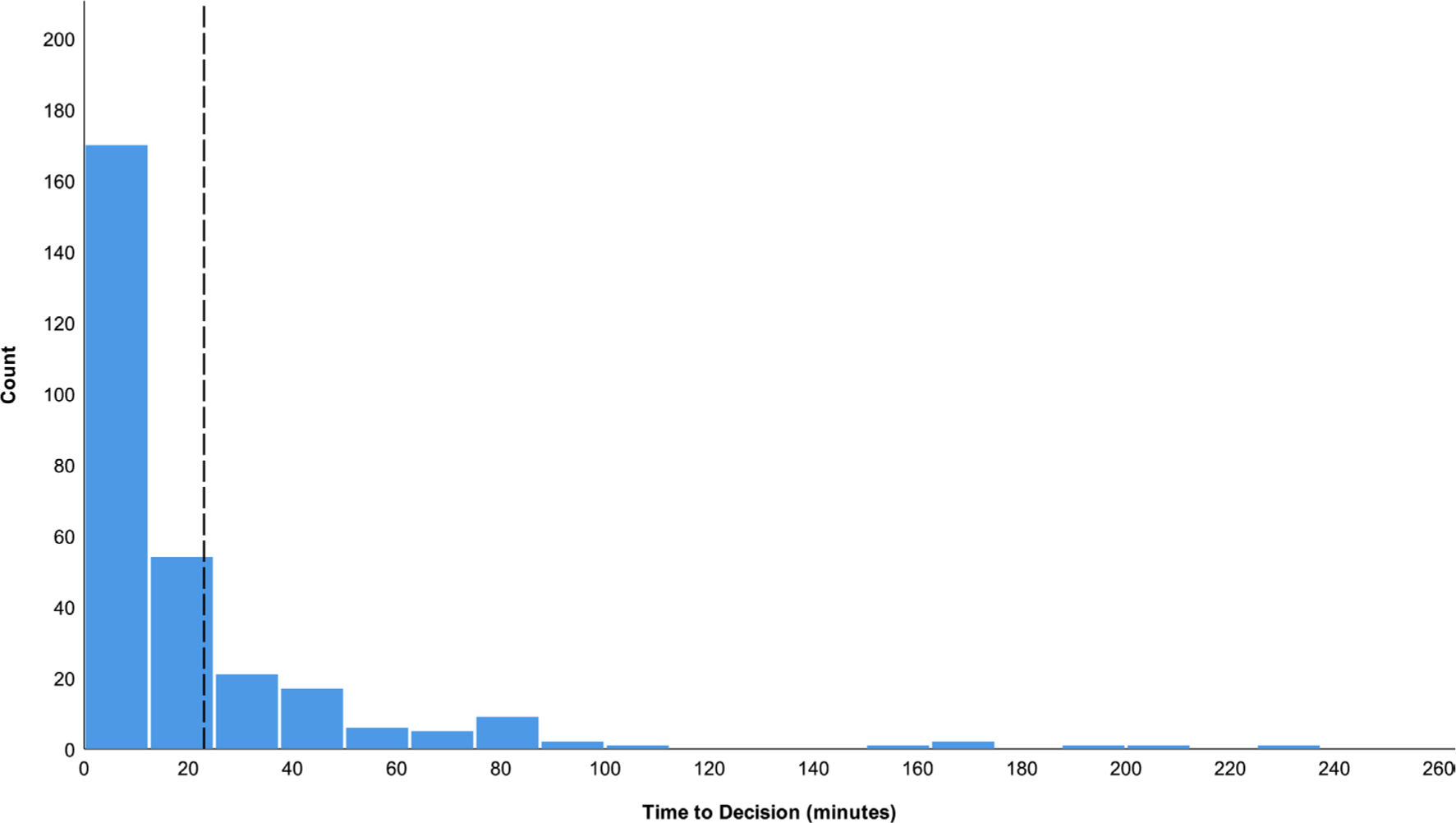
Fig. 4
Distribution of times to decision. The dashed black line represents 75% of patients referred.
Time to decision by outcome
The mean times to decision by outcome are shown in Figure 5 and listed in Table IV. There was a statistically significant difference noted between patients who were referred to specialist clinics and all other groups on one-way ANOVA (p < 0.001). A significant difference was also noted in time to decision between patients referred to the fracture clinic and those requiring no follow-up (p < 0.005).
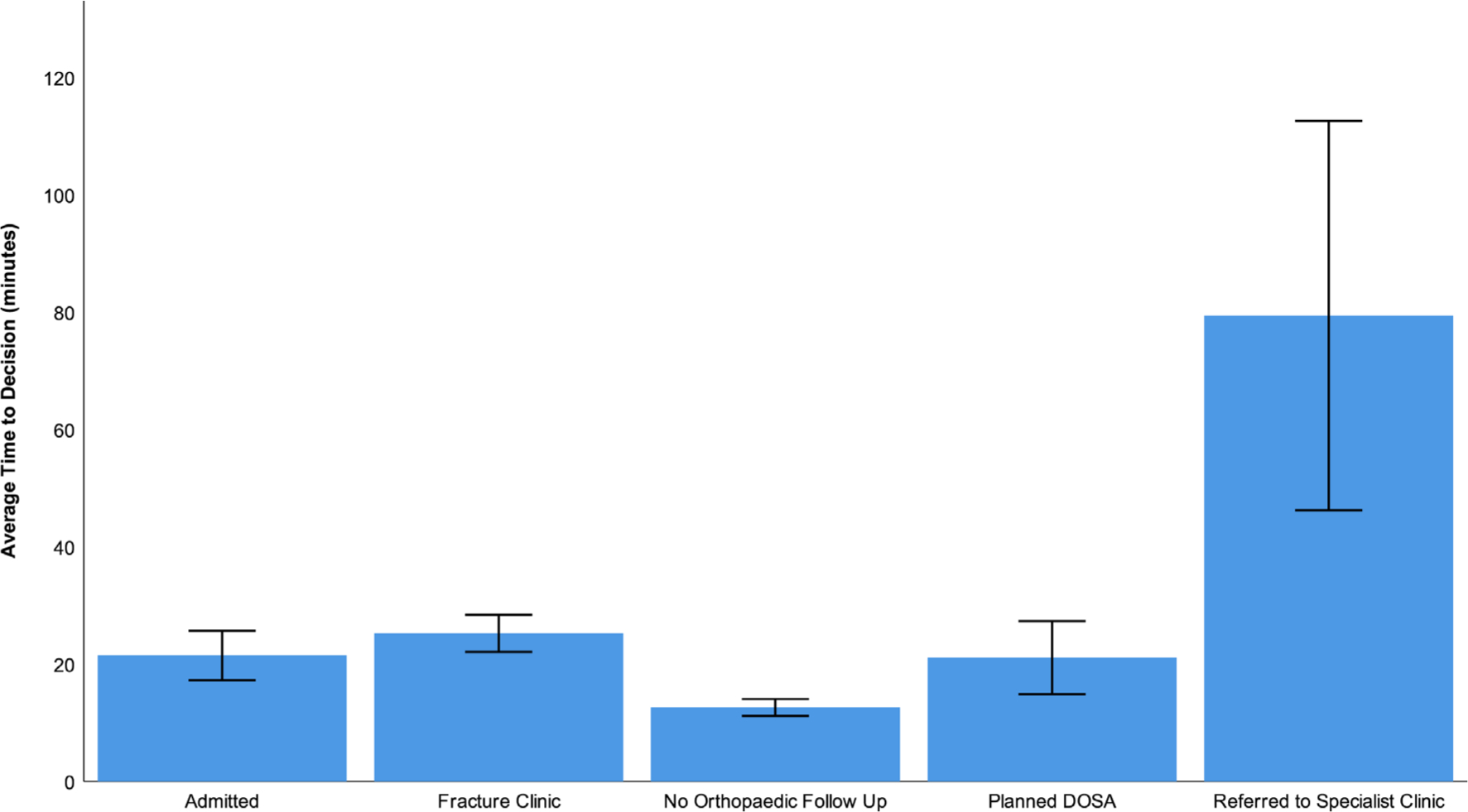
Fig. 5
Average time to decision by outcome (mean ± SEM)
Table IV.
Time to decision by outcome.
| Outcome | Time to decision, mins (SE) |
|---|---|
| Admitted | 21.48 (4.20) |
| Fracture clinic | 25.25 (3.18) |
| No orthopaedic follow-up | 12.63 (1.42) |
| Planned DOSA | 21.13 (6.22) |
| Referred to specialist clinic | 79.42 (33.17) |
| Total | 20.14 (1.73) |
-
DOSA, day of surgery admission
Reattendance rates
Four patients reattended the emergency department after being discharged. Two were due to joint stiffness following at-home removal of a soft cast; one child had their soft cast removed in error by the parent, and one reattended after breaking their cast. No patients were readmitted, and none of the patients who reattended had their management altered.
Number of fracture clinic referrals
During the initial data collection period, a total of 105 patients were referred to the fracture clinic, seven referred to other specialist clinics, and 137 patients were discharged directly. Traditionally, all 249 of these patients would have been referred to the fracture clinic (“potential referrals”). During the equivalent period in 2019, 295 new referrals were made to the fracture clinic, and 44 emergency admissions occurred. There was no significant difference between the weekly number of referrals in 2019 and the potential referrals in 2020 (59.0 (SE 5.15) vs 49.8 (SE 6.86); p = 0.315, independent samples t-test). However, there was a statistically significant difference between the number of referrals in 2019 and the actual number of referrals (59 (SE 5.15) vs 21 (SE 2.17); p < 0.001, independent samples t-test) (Figure 6).
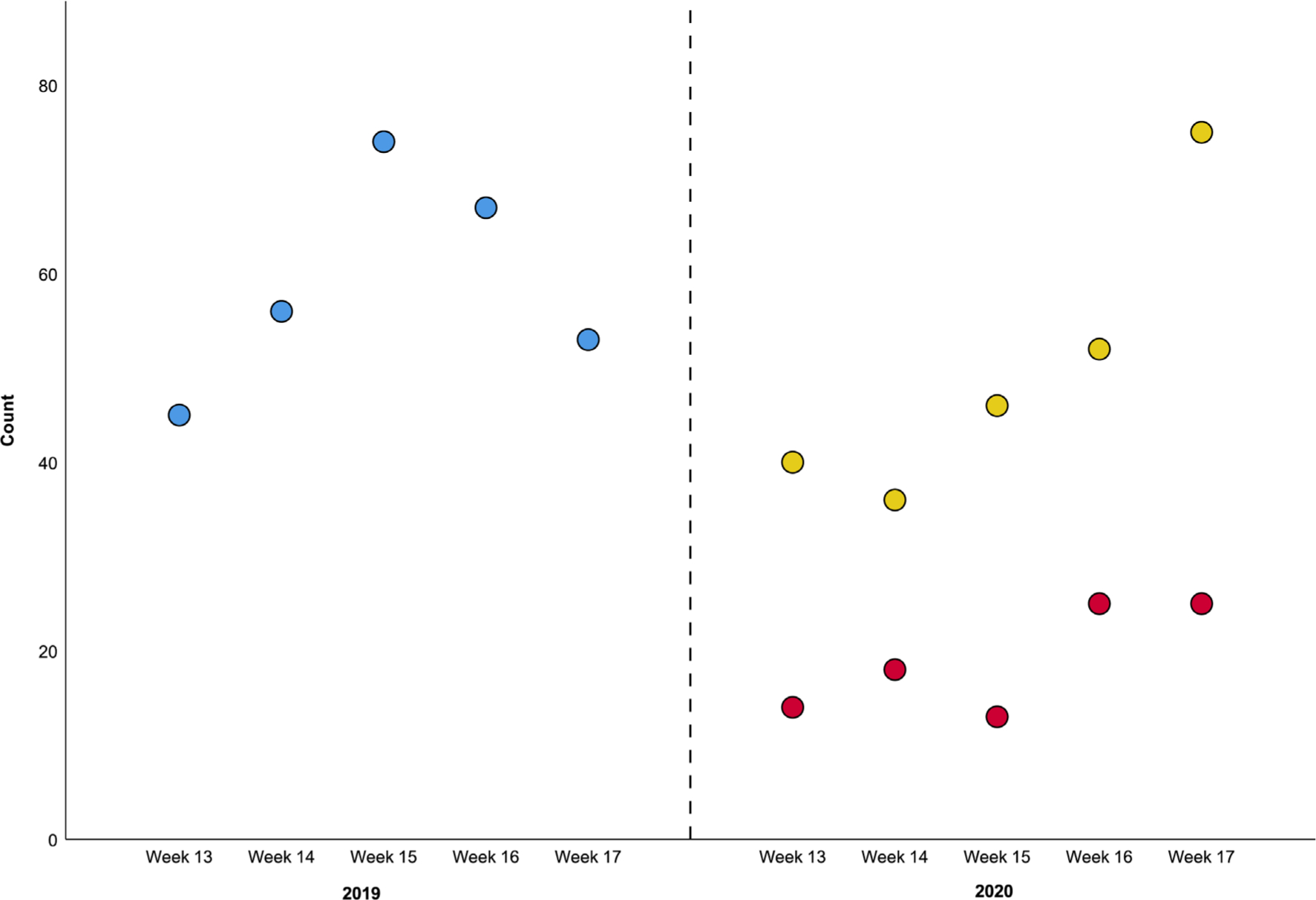
Fig. 6
Count of referrals for the equivalent period in 2019 and the reference period. Blue dots representreferrals to the fracture clinic in 2019; yellow dots represent potential referrals, and red dots the number of actual referrals in 2020
Discussion
The main findings of this study are that the TOP led to a significant discharge rate direct from the ED, a reduction in face-to-face clinic contact with definitive management decisions made in a timely fashion with financial and time savings for parents. To our knowledge, this is the first prospective analysis of an app-based trauma referral and orthopaedic management service in the literature.
The COVID-19 pandemic necessitated widespread adoption of social distancing protocols, something which is impossible in the typical orthopaedic outpatient setting. Since the first case in December 2019,25 there has been an unprecedented strain on healthcare systems. The main aim of our redesign was to adapt to these new pressures without compromising on our standard of care with no extra resources. A usual redesign requires multiple stakeholders and the involvement of other allied health services. However, due to the pandemic and inability to recruit staff, this intervention used readily-available secure communication software which needed no formal training to use correctly. This allowed us to create an “off-the-shelf” solution which could be quickly adopted in other institutions to deliver a similar service.
Prior to the introduction of the TOP, referrals to the orthopaedic team were made through the hospital switchboard. This synchronous communication is cumbersome for the referring team. The switch operator may be engaged or the on-call orthopaedic surgeon scrubbed or engaged in direct patient care at the time. It is similarly frustrating for the orthopaedic surgeon when they miss the call as they are unable to ascertain who attempted to contact them and must wait for the referrer to try again. On receipt of the call, the receiver may have to move location to access relevant imaging. TOP allows for real time asynchronous communication using a standard format, including imaging, which can be responded to immediately, or once whatever task at hand is completed, by the on-call orthopaedic registrar or consultant. Almost 90% of referrals required no further information. A contemporaneous electronic record is also generated on the app which is exported by the ED team and added to the patient’s record.
Traditionally at our institution, the ED would refer all fractures to the fracture clinic for definitive orthopaedic management. During the busy summer period, this can lead to significant strain on resources. Given COVID19 restrictions and the added public health effect of patients having multiple interactions with the hospital, use of public transport to attend clinics and the potential opportunities for spreading or contracting COVID-19, any reduction in risk is to be welcomed. While there may have been an increase in workload for the on-call orthopaedic team as every potential fracture referral was being discussed, there was a significant reduction in the number of face-to-face reviews. This frontloading was time efficient for patients with most having a decision within 10 minutes, obviating the need for return.
Of the 295 referrals made in the five weeks, 137 (46.4%) were discharged with a stable fracture or soft tissue injury management plan that required no formal follow-up, while still maintaining BOAST compliance.11 As paediatric patients are accompanied by their parents, and often siblings, this represents a reduction in almost 300 people attending the outpatient department in the data collection period of five weeks.
Previous research has identified that up to 48% of all referrals to the fracture clinic do not have radiological evidence of a fracture.15 Our institution has previously published an audit into this, and it was found that up to 37% had no fracture and up to a quarter of referrals were unnecessary.14 However, while 27.5% of our referrals had no fracture on radiograph, 38.9% (n = 11) of our admissions also had no evidence of fracture but were admitted for septic arthritis or osteomyelitis treatment, or debridement or investigation of potential non-accidental injury. Similarly, patients with patellar dislocation and potential cruciate ligament injuries were referred to the fracture clinic using the TOP. This highlights how the fracture clinic sees more than just fractures.
Other institutions have shown that utilizing a VFC reduces the need for repeat radiographs,26 and the extra time it afforded increased elective clinic work by 24%.7 Given the current reduction in capacity for all outpatient activity due to social distancing, we believe that every effort should be made to reduce unnecessary reviews. The fracture and specialist orthopaedic clinics run concurrently at our institution with a shared waiting room and typically have upwards of 90 patients attending within a five hour clinic window. With the reduction in waiting area space for patients and parents, it is not feasible to run an elective orthopaedic clinic service given the traditional fracture clinic workload and maintain social distancing.
Despite the reduction in the need for face to face reviews, there were no reported adverse events during the study. Four patients made an unexpected return to the ED, but this was not due to the new pathway. The timely instigation of a definitive management plan does not delay the majority of patents in the ED. Except for cases that required clarity on clinical examination or waiting for blood work, the average time to decision was 20 minutes. Half of patients had a decision within 10 minutes of being listed on the TOP and 75% within 23 minutes.
One limitation of our study is that it is reliant on having timely access to senior orthopaedic decision makers at all times. We are a paediatric tertiary referral centre with onsite orthopaedics, however we believe the readily customisable nature of the system is adaptable to other institutions.
The implementation of the TOP is achievable using readily available technology, without any additional resources, is novel and reduces the need for face-to-face review. Further evaluation of the impact of TOP on both patient and medical team satisfaction, along with an economic analysis, will be valuable.
References
1. Plunkett O , Hegarty I , Nugent C , Dunne T , Crossan V . Strategy for the design of integrated outpatient services 2016-2020 . Int J Integr Care . 2017 ; 17 ( 5 ): 6 . Google Scholar
2. McKirdy A , Imbuldeniya AM . The clinical and cost effectiveness of a virtual fracture clinic service: an interrupted time series analysis and before-and-after comparison . Bone Jt Res England . 2017 ; 6 ( 5 ): 259 – 269 . Crossref PubMed Google Scholar
3. Vardy J , Jenkins PJ , Clark K , et al. Effect of a redesigned fracture management pathway and 'virtual' fracture clinic on ED performance . BMJ Open . 2014 ; 4 ( 6 ): e005282 . Crossref PubMed Google Scholar
4. Brogan K , Bellringer S , Akehurst H , et al. Virtual fracture clinic management of fifth metatarsal, including Jones', fractures is safe and cost-effective . Injury . 2017 ; 48 ( 4 ): 966 – 970 . Crossref PubMed Google Scholar
5. Anderson GH , Jenkins PJ , McDonald DA , et al. Cost comparison of orthopaedic fracture pathways using discrete event simulation in a Glasgow Hospital . BMJ Open . 2017 ; 7 ( 9 ): e014509 . Crossref PubMed Google Scholar
6. O' Reilly M , Breathnach O , Conlon B , Kiernan C , Sheehan E . Trauma assessment clinic: virtually a safe and smarter way of managing trauma care in Ireland . Injury . 2019 ; 50 ( 4 ): 898 – 902 . Crossref PubMed Google Scholar
7. Kelly M , O'Keeffe N , Francis A , et al. Connolly Hospital trauma assessment clinic (Tac): a virtual solution to patient flow . Ir J Med Sci . 2020 ; 189 ( 2 ): 425-429 . Crossref PubMed Google Scholar
8. Ferguson KB , McGlynn J , Jenkins P , et al. Fifth metatarsal fractures – is routine follow-up necessary? Injury . 2015 ; 46 ( 8 ): 1664 – 1668 . Crossref PubMed Google Scholar
9. Breathnach O , O'Reilly M , Morrissey K , Conlon B , Sheehan E . Electronic referrals for virtual fracture clinic service using the National integrated medical imaging system (NIMIS) . Ir J Med Sci . 2019 ; 188 ( 2 ): 371 – 377 . Crossref PubMed Google Scholar
10. Morris MWJ , Bell MJ . The socio-economical impact of paediatric fracture clinic appointments . Injury . 2006 ; 37 ( 5 ): 395 – 397 . Crossref PubMed Google Scholar
11. British Orthopaedic Association . Fracture clinic services . 2013 . Google Scholar
12. Holgate J , Kirmani S , Anand B . Virtual fracture clinic delivers British orthopaedic association compliance . Ann R Coll Surg Engl England . 2017 ; 99 ( 1 ): 51 – 54 . Crossref PubMed Google Scholar
13. Huntley JS . Paediatric fracture clinic design – current practice and implications for change . BMC Res Notes . 2014 ; 7 ( 1 ): 96 . Google Scholar
14. Ramasubbu B , McNamara R , Deiratany S , Okafor I . An evaluation of the accuracy and necessity of fracture clinic referrals in a busy pediatric emergency department . Pediatr Emerg Care . 2016 ; 32 ( 2 ): 69 – 70 . Crossref PubMed Google Scholar
15. Robinson PM , Sim F , Latimer M , Mitchell PD . Paediatric fracture clinic re-design: incorporating a virtual fracture clinic . Injury . 2017 ; 48 ( 10 ): 2101 – 2105 . Crossref PubMed Google Scholar
16. Jayaram PR , Bhattacharyya R , Jenkins PJ , Anthony I , Rymaszewski LA . A new "virtual" patient pathway for the management of radial head and neck fractures . J Shoulder Elbow Surg . 2014 ; 23 ( 3 ): 297 – 301 . Crossref PubMed Google Scholar
17. Gamble D , Jenkins PJ , Edge MJ , et al. Satisfaction and functional outcome with "self-care" for the management of fifth metacarpal fractures . Hand . 2015 ; 10 ( 4 ): 607 – 612 . Crossref PubMed Google Scholar
18. Bhattacharyya R , Jayaram PR , Holliday R , et al. The virtual fracture clinic: reducing unnecessary review of clavicle fractures . Injury . 2017 ; 48 ( 3 ): 720 – 723 . Crossref PubMed Google Scholar
19. Mackenzie SP , Carter TH , Jefferies JG , et al. Discharged but not dissatisfied: outcomes and satisfaction of patients discharged from the Edinburgh trauma triage clinic . Bone Joint J . 2018 ; 100-B ( 7 ): 959 – 965 . Google Scholar
20. Logishetty K . Adopting and sustaining a virtual fracture clinic model in the district hospital setting – a quality improvement approach . BMJ Qual Improv Rep . 2017 ; 6 ( 1 ): u220211.w7861 . Google Scholar
21. Rotter T , Plishka C , Lawal A , et al. What is lean management in health care? development of an operational definition for a Cochrane systematic review . Eval Health Prof . 2019 ; 42 ( 3 ): 366 – 390 . Crossref PubMed Google Scholar
22. Siilo . Siilo | GDPR Compliance . www.siilo.com . 2018 . https://www.siilo.com/blog/checklist-gdpr-compliance-for-healthcare-messaging-apps (date last accessed 05/04/2020 ). Google Scholar
23. Official Journal of the European Union . Regulation (EU) 2016/679 of the European Parliament and of the Council of 27 April 2016 on the protection of natural persons with regard to the processing of personal data and on the free movement of such data, and repealing Directive 95/46/EC (General Data Protection Regulation) (Text with EEA relevance) . 2016 . http://data.europa.eu/eli/reg/2016/679/oj/eng (date last accessed 10/06/2020 ). Google Scholar
24. Divi SN , Bielski RJ . Legg-Calvé-Perthes disease . Pediatr Ann . 2016 ; 45 ( 4 ): e144 – e149 . Crossref PubMed Google Scholar
25. Zhou P , Yang X-L , Wang X-G , et al. A pneumonia outbreak associated with a new coronavirus of probable bat origin . Nature . 2020 ; 579 ( 7798 ): 270 – 273 . Crossref PubMed Google Scholar
26. Seewoonarain S , Babu S , Sangoi D , Avasthi A , Ricketts D . Introducing a virtual fracture clinic increases efficiency and reduces costs in Torus fracture management . Pediatr Qual Saf . 2019 ; 4 ( 6 ): e202 . Crossref PubMed Google Scholar
Author contributions
T. V. McIntyre: Wrote the manuscript.
E. G. Kelly: Assisted with statistics, Edited the manuscript.
T. Clarke: Maintained referrals database, Edited the manuscript.
C. J. Green: Edited the manuscript.
Funding statement
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
Acknowledgements
The authors would like to thank the staff in the Emergency Department in Children's Health Ireland at Temple Street for their immediate engagement with and support for the new initiative.
© 2020 Author(s) et al. This is an open-access article distributed under the terms of the Creative Commons Attributions licence (CC-BY-NC-ND), which permits unrestricted use, distribution, and reproduction in any medium, but not for commercial gain, provided the original author and source are credited.









