Abstract
Objectives
“Virtual fracture clinics” have been reported as a safe and effective alternative to the traditional fracture clinic. Robust protocols are used to identify cases that do not require further review, with the remainder triaged to the most appropriate subspecialist at the optimum time for review. The objective of this study was to perform a “top-down” analysis of the cost effectiveness of this virtual fracture clinic pathway.
Methods
National Health Service financial returns relating to our institution were examined for the time period 2009 to 2014 which spanned the service redesign.
Results
The total staffing costs rose by 4% over the time period (from £1 744 933 to £1 811 301) compared with a national increase of 16%. The total outpatient department rate of attendance fell by 15% compared with a national fall of 5%. Had our local costs increased in line with the national average, an excess expenditure of £212 705 would have been required for staffing costs.
Conclusions
The virtual fracture clinic system was associated with less overall use of staff resources in comparison to national cost data. Adoption of this system nationally may have the potential to achieve significant cost savings.
Cite this article: P. J. Jenkins. Fracture clinic redesign reduces the cost of outpatient orthopaedic trauma care. Bone Joint Res 2016;5:33–36. doi: 10.1302/2046-3758.52.2000506
Article focus
-
The cost effectiveness of a redesigned pathway for the management of orthopaedic trauma in the outpatient department.
Key messages
-
The staffing costs at our institution’s orthopaedic outpatient department rose by 4%, compared with a national average of 16%.
-
A cost saving of £212 705 was achieved, when compared with the national average.
-
National adoption of the redesigned fracture pathway may have resulted in a cost saving of £3 535 808 over the time period.
Strengths and limitations
-
A strength was the use of national data that are open and freely available for analysis.
-
A limitation was the lack of resolution of the national financial data that are only available at the level of the orthopaedic outpatient department and are not split between trauma and elective costs.
-
A further limitation was the inability to assess the costs of consumables and other allocated expenses due to differences in the methods of apportionment between health boards.
Introduction
Our institution introduced a service redesign in 2010 that was primarily focused on improving the management of minor orthopaedic trauma.1-5 The delivery of outpatient fracture care has not changed significantly since guidelines were set by the British Medical Association in 1935.6 These historical guidelines were a response to wide variation and poor practice in the management of common injuries. The care of fractures has changed since this time in line with the improvement in our understanding of outcomes of fractures, and identification of those requiring surgical management. Whereas patients traditionally attend fracture clinics at regular fixed periods, our redesign emphasised accurate triage to ensure patients attended only when and where necessary, to reduce therapeutic inertia. Although this service redesign was primarily focused on improving the quality of care, we hypothesised that there would be associated cost savings.
The National Health Service is under immense pressure to reduce costs, with savings of £15 to £20 billion demanded since 2009.7 Costs can be saved by improving commissioning (in NHS England), improving organisational and business processes, and, finally, by improving the efficacy and efficiency of clinical care.8 Concern has been expressed that cost savings from small projects and service redesign cannot deliver significant savings at the macro scale.8 It is also thought that to save money following a service redesign, there need to be major changes to staffing and estates which equate to job losses and closures.8
There are different methods of attempting to quantify costs savings, each with its advantages and limitations. A ‘bottom-up’ approach seeks to quantify the unit costs of time and material and quantify changes in costs based on utilisation. A ‘top-down’ approach seeks to examine high-level administrative financial data to identify overall high-level trends.
The aim of this study was to examine whether ‘high-level’ NHS cost data could be used to examine change in patient attendance and cost over time at local orthopaedic outpatient clinics, and to determine whether savings could be identified after orthopaedic outpatient service redesign.
Materials and Methods
The Scottish Costs Book (Information Services Division, ISD) was used to obtain the cost of outpatient department (OPD) and nurse-led clinics (NLC) at our institution from 2009 to 2014.9 Each year’s financial statement is published in or around November and reports the financial year ending on March of that year. Direct costs include medical and nursing staff costs, pharmacy, supplies and laboratory costs. These can be directly attributed to the department in question through standard accounting techniques. The costs do not include administration, portering, facilities, utilities and depreciation, which are ‘allocated’ to the department as a proportion of the overall hospital running costs through a standardised procedure of apportionment.10 Detailed annual costs are provided in the SFR (standard financial returns) tables. The SFR 5.7 table was used to examine outpatient department (OPD) costs and the SFR 5.7N table was used to examine nurse-led clinic (NLC) costs.9 These accounts report the total number of patients and associated costs for each orthopaedic department in Scotland. The apportionment of allocated costs may vary between hospitals and NHS boards, and therefore allocated costs were not examined further. Outpatient departments are also charged a proportion of hospital laboratory costs that again vary between units. Some units such us our institution may have tertiary laboratory services and these costs may be allocated to departments not directly responsible. Thus, we did not examine the allocated laboratory costs. There were also changes over the duration of the study in the attribution of costs of items such as wound dressings, hence these costs were also not examined.
We therefore only examined the total staffing costs, comprised of medical, nursing and associated healthcare professionals (AHPs). These were added together to derive a total staffing cost. Costs were reported for our institution and compared with the overall national average. Staffing was also recorded in the SFRs as medical and nursing whole-time equivalent (WTE) posts, and these have also been reported. Differences over time have been compared by calculating the percentage difference each year from the 2009 baseline, prior to the service redesign. The cost (direct staffing) per attendance was calculated by dividing the total annual cost by the annual number of attendances.
Results
The total staffing cost at our institution rose from £1.74 million in 2009 to £1.81 million in 2014, a rise of 4% (Table I, Fig. 1) compared with an average national rise of 16%. The medical staffing cost rose by 8%, while the nursing staffing cost fell by 4% and the AHP cost fell by 11% (Table II). The total number of OPD attendances fell by 15%, while those in Scotland as a total fell by 5%. Had our local costs increased at the average national rate an excess spend of £212 705 would have been required over the time period. Had the national average replicated our local increase, a national cost saving of £3 535 808 would have been achieved.
Table I.
Total staff costs for the orthopaedic outpatient department at our institution compared with the national average. The percentages represent change from the 2009 baseline.
| Study institution |
National average |
|||
|---|---|---|---|---|
| Year | Staff cost (£) (%) | % Change | Staff cost (£) (%) | % Change |
| 2009 | 1 744 933 | 29 213 145 | ||
| 2010 | 1 664 126 | -5 | 30 686 629 | 5 |
| 2011 | 1 733 230 | -1 | 32 508 444 | 11 |
| 2012 | 1 930 048 | 11 | 35 513 636 | 22 |
| 2013 | 1 845 820 | 6 | 33 663 199 | 15 |
| 2014 | 1 811 301 | 4 | 33 861 804 | 16 |
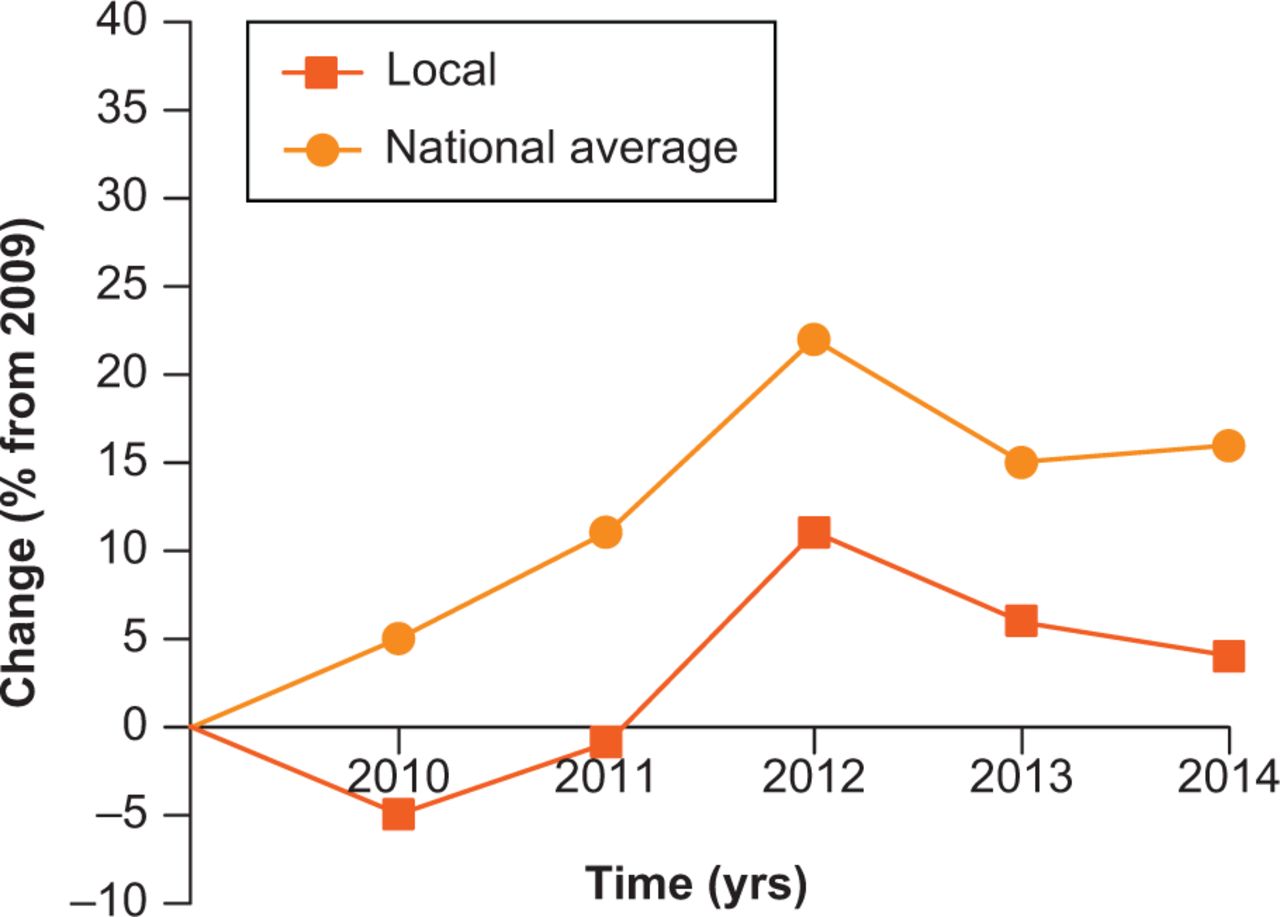
Fig. 1
Percentage change (percentage change compared with initial year, 2009) in OPD staffing costs for our institution, and the national average.
Table II.
Percentage change 2009 to 2014 in outpatient department (OPD) and nurse-led clinics (NLC) staffing and costs, along with attendances.
| Local (%) | National average (%) | |
|---|---|---|
| OPD staff cost | ||
| Medical | 8 | 29 |
| Nursing | -4 | -1 |
| AHP | -11 | -54 |
| TOTAL | 4 | 16 |
| Staffing | ||
| Medical WTE | -8 | 25 |
| Nursing WTE | -12 | -15 |
| NLC staffing and cost | ||
| NLC Cost | -3 | 31 |
| NLC WTE | -8 | 16 |
| Capacity OPD | ||
| Total OPD Attendances | -15 | -5 |
| Total NLC Attendances | -4 | 39 |
-
AHP, associated healthcare professionals; WTE, whole-time equivalent; OPD, outpatient department, NLC, nurse-led care
The fall in attendance was not associated with an increase in nurse-led services; the total NLC attendances also fell at our institution by 4% over the same period. This compared with a 39% increase for Scotland.
The ratio of return to new patients fell from 1.78 to 1.63, demonstrating that fewer patients returned to follow-up clinics. The national figure varied minimally from 1.77 to 1.78 over the same time period.
The increase in direct staffing cost per attendance at our institution was similar to the national figure: £64 to £77 (20.3% increase) over the time period compared with a figure of £56 to £68 (21.4%).
Discussion
The main aim of this redesign process was to improve the quality of outpatient fracture patient care. We planned to reduce unneccesary attendance following orthopaedic trauma. The clinical safety of this approach has been examined through prospective data collection and audit. To date, we have published evidence about the satisfaction and clinical outcome of radial head fractures and mallet finger injuries.1-5 We have also previously demonstrated that the system resulted in improvements in the flow of patients in the Emergency Department (ED), with no adverse effects of providing more information at the first point of contact in order to reduce the number of follow-up visits.5 This “balance” measure demonstrates that this redesigned pathway has not had a harmful effect on our linked units.
Our absolute cost per patient attendance started from a higher figure than the national average. This may reflect a historical difference in the unit staffing, or differences in the experience profile of our staff and their consequent level on the relevant medical and nursing pay scales. The triage element ensured that patients saw the correct specialist for their injury, at the appropriate time point, with fewer wasted appointments and associated unnecessary investigations such as radiographs. There have been wider benefits to our department as, following redesign, three of our consultants do not undertake fracture clinics, and instead provide additional elective capacity for musculoskeletal oncology and the orthopaedic spinal service. Furthermore, two consultants have been able to develop a “Joint School” to enhance the pre-operative communication and education of patients about to undergo hip and knee replacement. These benefits occurred without the need for additional investment.
A limitation of this study is that financial data were recorded at an overall unit level, and not divided between elective and trauma services. During the time period, there were no significant service re-organisations other than the fracture pathway redesign. It is therefore likely that the differences found reflect this effect. Another limitation is the inability to conclusively prove a causal relationship. At most, these can be considered associations until further work is performed.
A potential hurdle to the implementation of this system is the method of health service funding. Our service is provided in a healthcare system where there is a “block grant” for the provision of services, rather than a tariff-based payment per episode. Tariff-based payment may lead to inappropriate increases in activity and further induced demand.11 Visitors to our unit have voiced concern that reduction in face-to-face contact may lead to overall reduction in income, and consequently to loss of staff and services. There are mechanisms that exist in the NHS England funding arrangements to reward such quality improvement through the “Commissioning for Quality and Innovation” (CQUIN) payment framework.12,13 It is therefore essential that when redesign is planned, early dialogue is commenced with local clinical commissioning groups (CCGs) to quantify the necessary financial resources and potential savings.
Further “bottom-up” research will provide complementary data to re-examine the cost effectiveness of the virtual fracture pathway. Methods such as discrete element simulation may also provide suitable tools to assist such evaluations.14 Future research should investigate the virtual fracture pathway in a prospective manner, with treatment allocation via randomisation to reduce bias. A comprehensive study should examine both clinical and cost effectiveness, along with patient satisfaction. Treatment allocation to such a service re’design may not be possible at an individual patient level without significant ‘Hawthorne’ effects, and a cluster design may be more appropriate, with randomisation at a unit level.15
In conclusion, high-level national financial data have been used to investigate the costs associated with a redesign of orthopaedic outpatient care, and have demonstrated reduced local costs compared with the national average.
Funding Statement:
This study has been supported by the Scottish Government Quality and Efficiency Support Team (QuEST) – Whole System Patient Flow Project.
ICMJE conflict of interest:
None declared
References
1. Brooksbank K , JenkinsPJ, AnthonyIC, et al.. Functional outcome and satisfaction with a “self-care” protocol for the management of mallet finger injuries: a case-series. J Trauma Manag Outcomes2014;8:21. Google Scholar
2. Ferguson KB , McGlynnJ, JenkinsP, et al.. Fifth metatarsal fractures - Is routine follow-up necessary?Injury2015;46:1664-1668.CrossrefPubMed Google Scholar
3. Gamble D , JenkinsP, EdgeM, et al.. Satisfaction and functional outcome with “self-care” for the management of fifth metacarpal fractures. Hand (NY)2015;10:607-612. Google Scholar
4. Jayaram PR , BhattacharyyaR, JenkinsPJ, AnthonyI, RymaszewskiLA. A new “virtual” patient pathway for the management of radial head and neck fractures. J Shoulder Elbow Surg2014;23:297-301. Google Scholar
5. Vardy J , JenkinsPJ, ClarkK, et al.. Effect of a redesigned fracture management pathway and ‘virtual’ fracture clinic on ED performance. BMJ Open2014;4:e005282. Google Scholar
6. No authors listed. British Medical Association. Report of Committee on Fractures. BMJ1935;1581(suppl):s53-s62.[[bibmisc]] Google Scholar
7. No authors listed. The Year: NHS Chief Executive’s Annual Report 2008/2009. London, 2009http://www.healthcare-today.co.uk/doclibrary/documents/pdf/215_the_year_2008-09.pdf (date last accessed 15 October 2015).[[bibmisc]] Google Scholar
8. Marshall M , ØvretveitJ. Can we save money by improving quality?BMJ Qual Saf2011;20:293-296.CrossrefPubMed Google Scholar
9. No authors listed. ISD Scotland. Scottish Health Service Costs (Costs Book). 2014. http://www.isdscotland.org/Health-Topics/Finance/Costs/. 29/12/2014 (date last accessed 30 October 2015).[[bibmisc]] Google Scholar
10. No authors listed. Scotland ISD. Scottish Health Service Costs. Bookman. 2014. http://www.isdscotland.org/Health-Topics/Finance/Publications/2014-12-02/2014-12-02-Costs-Report.pdf (date last accessed 15 October 2015).[[bibmisc]] Google Scholar
11. Mannion R , MariniG, StreetA. Implementing payment by results in the English NHS: changing incentives and the role of information. J Health Organ Manag2008;22:79-88.CrossrefPubMed Google Scholar
12. Mays N . Evaluating the Labour Government’s English NHS health system reforms: the 2008 Darzi reforms. J Health Serv Res Policy2013;18(2 Suppl):1-10. Google Scholar
13. Abma I , JayantiA, BayerS, MitraS, BarlowJ. Perceptions and experiences of financial incentives: a qualitative study of dialysis care in England. BMJ Open2014;4:e004249.CrossrefPubMed Google Scholar
14. Fone D , HollinghurstS, TempleM, et al.. Systematic review of the use and value of computer simulation modelling in population health and health care delivery. J Public Health Med2003;25:325-335.CrossrefPubMed Google Scholar
15. Bland JM , KerrySM. Statistics notes. Trials randomised in clusters. BMJ1997;315:600.CrossrefPubMed Google Scholar









