Abstract
Aims
Postoperative malalignment of the femur is one of the main complications in distal femur fractures. Few papers have investigated the impact of intraoperative malalignment on postoperative function and bone healing outcomes. The aim of this study was to investigate how intraoperative fracture malalignment affects postoperative bone healing and functional outcomes.
Methods
In total, 140 patients were retrospectively identified from data obtained from a database of hospitals participating in a trauma research group. We divided them into two groups according to coronal plane malalignment of more than 5°: 108 had satisfactory fracture alignment (< 5°, group S), and 32 had unsatisfactory alignment (> 5°, group U). Patient characteristics and injury-related factors were recorded. We compared the rates of nonunion, implant failure, and reoperation as healing outcomes and Knee Society Score (KSS) at three, six, and 12 months as functional outcomes. We also performed a sub-analysis to assess the effect of fracture malalignment by plates and nails on postoperative outcomes.
Results
The rates of nonunion and reoperation in group U were worse than those in group S (25.0% vs 14.3%; 15.6% vs 5.6%), but the differences were not significant (p = 0.180 and p = 0.126, respectively). Mean KSS in group U at all follow-up periods was significantly worse that in group S (75.7 (SD 18.8) vs 86.0 (SD 8.7); p < 0.001; 78.9 (SD 17.2) vs 89.1 (SD 9.8); p < 0.001; 85.0 (SD 11.9) vs 91.1 (SD 7.2); p = 0.002, respectively). In the sub-analysis of plates, mean KSS was significantly worse in group U at three and six months. In the sub-analysis of nails, the rate of reoperation was significantly higher in group U (28.6% vs 5.8%; p = 0.025), and mean KSS at six and 12 months was significantly worse in Group U.
Conclusion
To obtain good postoperative functional results, intraoperative alignment of the coronal plane should be accurately restored to less than 5°.
Cite this article: Bone Jt Open 2022;3(2):165–172.
Take home message
Intraoperative fracture malalignment may adversely affect postoperative fracture union and function.
The findings of the current study are consistent with the results suggested by previous retrospective studies.
Intraoperative coronal malalignment should be no more than 5° for good postoperative bone healing and functional prognosis.
Introduction
It is challenging to achieve and maintain adequate reduction of femoral fractures.1 Among the implants developed for distal femur fractures in recent decades, the locking compression plate (LCP) and retrograde intramedullary nail (RIN) are widely used to treat these fractures.2 Many studies showed almost no differences in postoperative outcomes between LCP and RIN.3,4 Some authors have concluded that preoperative planning and surgical technique are more important than which implant to use.4
One of the postoperative complications in distal femur fracture is malalignment of the femur, which may be largely related to poor intraoperative restoration. Postoperative fracture malalignment is thought to be related to functional and healing outcomes.5 However, many studies analyzed fracture malalignment as a clinical outcome, so the impact of intraoperative fracture malalignment on postoperative outcomes remains unclear.
The aims of this study were to investigate 1) the incidence of fracture malalignment after distal femoral fracture surgery and 2) how intraoperative fracture malalignment affects postoperative functional outcome and bone healing in terms of LCP and RIN use.
Methods
Subjects
Data from the hospitals of a trauma research group, named TRON, were extracted for this study. This registry collects data about all orthopaedic trauma patients referred to participating hospitals, and data have been registered annually since 2014. The hospitals participating in the database were all associated with the Department of Orthopaedic Surgery of Nagoya University, and orthopaedic surgeons performed the surgery at these hospitals, located in central Japan.
All eligible patients were registered using an opt-out consent process. Patients were provided with a letter and a brochure informing them that they had been registered, the purpose of the registration, and the procedure to remove themselves from the registry. The registry had ethical approval from all participating institutions. This study also received institutional ethical approval (reference number 2020-564).
We extracted data from the database on 439 patients who were treated with surgery for distal femur fractures from 2014 to 2019. The inclusion criteria for this study were 1) acute and unilateral fractures and 2) fractures in patients who walked without care before injury. The exclusion criteria for this study were 1) fractures in patients under 18 years old, 2) patients who died within a year after surgery, 3) follow-up of < six months, 4) fractures treated by screw or external fixation only, and 5) periprosthetic total knee arthroplasty (TKA) fractures. We divided the analyzed cases into two groups: those with coronal plane malalignment of more than 5° (Group U) and those with malalignment of less than 5° (Group S) at the fracture site on immediate postoperative radiograph (Figure 1).

Fig. 1
Patient flowchart for this study. Patients with open fractures and periprosthetic total knee arthroplasty (TKA) fractures were excluded. Finally, the analyzed cases were divided into the satisfactory and unsatisfactory groups (Group S and Group U) according to coronal plane alignment of 5° on the immediate postoperative radiograph.
Clinical evaluation
The following demographic data were extracted for each patient: 1) background factors: sex, age, BMI, Charlson Comorbidity Index,6 ASA-PS (American Society of Anesthesiologists-Physical Status),7 history of fragility fractures, smoking, walking status; 2) injury factors: injury mechanism, angular deformity of the fracture in the sagittal or coronal plane, and AO/OTA fracture classification;8 and 3) surgical factors: operating time and intraoperative blood loss. High-energy trauma was defined as anything worse than a fall from a standing position, such as traffic accidents, whereas low-energy trauma was defined as a fall from a standing position or from lying in bed.9 Fragility fractures were defined as fractures resulting from low-energy trauma that were located at the proximal humerus, distal radius, vertebra, or femoral neck.10 Walking status was evaluated with the Parker Mobility Score (PMS).11 In the PMS, the following three items are rated from 0 (not at all possible) to 3 (not difficult), with a maximum total score of 9: “able to move around the house”, “able to go out”, and “able to go shopping”.2,11
We analyzed the postoperative radiological outcomes according to implant failure, bone union, and malalignment of the femur in the coronal plane at the fracture site. Intraoperative malalignment was calculated by the residual angular deformity of the fracture in the coronal plane on immediate postoperative radiograph. Bone union was defined as bony bridging of three or four cortices on anteroposterior and lateral radiographs.12 Delayed union was defined as absence of bone union at the six-month follow-up, and nonunion was defined as absence of the progression of union in the past three months at the 12-month follow-up.13 Implant failure included broken nails and plates and loose or broken screws. Implants that were removed due to patient request without complications were excluded from this study.4
We assessed the Knee Society Score (KSS) as knee functional outcome at three, six, and 12 months after surgery. The KSS includes range of flexion, pain, alignment, flexion contracture, extension lag, and stability of the knee.14,15 We also analyzed the clinical outcomes for each surgical procedure (LCP and RIN) in a subgroup analysis. In addition, we performed a sub-analysis of the impact of fracture malalignment on the postoperative outcomes for LCP and RIN.
Patient demographic data
In total, 140 patients were analyzed. We found that 32 patients (22.8%) had intraoperative coronal malalignment of > 5°. The mean follow-up period was 18.5 months (6 to 84). The baseline characteristics and surgery data of the patients and the fractures are presented in Table I. There were no significant differences in patient characteristics, comorbidity, severity of injury mechanism, and fractures between the two groups. There were also no significant differences in mean operating time and blood loss between the two groups using Welch’s t-test (152.3 vs 165.5 mins (p = 0.406) and 165.1 vs 166.8 ml (p = 0.967), respectively, both Welch’s t-test).
Statistical analysis
Two orthopaedic trauma surgeons (YK, YT) evaluated the alignment of the femur, fracture classification, implant failure, and fracture union. We calculated intraclass correlation coefficients (continuous variable) and Kappa coefficient (categorical data) for interobserver reliability, and they were 0.73 and 0.79, respectively. All categorical variables were compared between the two groups using Fisher’s exact test; all continuous variables were analyzed using Welch’s t-test. The results of functional assessment data were presented in box plots. We used a pairwise method to exclude the missing data of functional assessment. The significance level was set at p < 0.05, and all statistical analyses were performed using EZR (Jichi Medical School, Japan).16
Results
Table I.
Patient demographic data.
| Variable | Group S | Group U | p-value |
|---|---|---|---|
| Number of patients | 108 | 32 | |
| Mean age, yrs (range) | 70.3 (25 to 93) | 70.0 (19 to 88) | 0.907* |
| Sex, n; M/F | 24/84 | 10/22 | 0.349† |
| Mean BMI, kg/m2 (range) | 23.2 (14.2 to 39.3) | 22.7 (14.2 to 30.5) | 0.598* |
| Smoking, n (%) | 9 (8.3) | 4 (12.5) | 0.724† |
| ASA, n (%) | 0.536† | ||
| I | 32 (29.6) | 13 (40.6) | |
| II | 65 (60.2) | 17 (53.1) | |
| III | 11 (10.2) | 2 (6.2) | |
| CCI, n (%) | 0.867† | ||
| Low (0) | 50 (46.3) | 15 (46.9) | |
| Medium (1 to 2) | 47 (43.5) | 13 (40.6) | |
| High (3 to 4) | 6 (5.6) | 3 (9.4) | |
| Very high (> 5) | 5 (4.6) | 1 (3.1) | |
| History of fragility fractures, n (%) | 33 (30.6) | 13 (40.6) | 0.293† |
| Mean preoperative Parker's mobility score (SD) | 8.55 (0.98) | 8.50 (0.98) | 0.815‡ |
| Injury mechanism, n (%) | 0.655† | ||
| Low-energy | 79 (72.5) | 21 (67.7) | |
| High-enegy | 30 (27.5) | 10 (32.3) | |
| AO/OTA classification, n (%) | 0.789† | ||
| A1 | 25 (23.1) | 11 (34.4) | |
| A2 | 20 (18.5) | 5 (15.6) | |
| A3 | 19 (17.6) | 6 (18.8) | |
| B1 | 5 (4.6) | 0 (0.0) | |
| B2 | 2 (1.9) | 0 (0.0) | |
| B3 | 1 (0.9) | 0 (0.0) | |
| C1 | 10 (9.3) | 5 (15.6) | |
| C2 | 22 (20.4) | 4 (12.5) | |
| C3 | 4 (3.7) | 1 (3.1) | |
| Mean angular coronal deformity at injury, ° (SD) | 8.8 (9.7) | 10.4 (10.0) | 0.392* |
| Mean angular sagittal deformity at injury, ° (SD) | 16.2 (14.4) | 21.2 (17.9) | 0.106* |
| Implant, n (%) | 0.064† | ||
| LCP | 39 (36.1) | 18 (56.2) | |
| RIN | 69 (63.9) | 14 (43.8) | |
| Mean operating time, mins (SD) | 152.3 (80.6) | 165.5 (71.6) | 0.406* |
| Mean blood loss, ml (SD) | 165.1 (197.8) | 166.8 (157.4) | 0.967* |
-
*
Welch's t-test.
-
†
Fisher's exact test.
-
‡
Mann-Whitney U test.
-
ASA, American Society of Anesthesiologists; CCI, Charlson Comorbidity Index; LCP, locking compression plate; RIN, retrograde intramedullary nail; RIN, retrograde intramedullary nail; SD, standard deviation.
We used Fisher’s exact test to compare complication rates. The number of implant failures in group S was 4/108 (3.7%), and in group U was 3/32 (9.4%) (p = 0.196, Fisher’s exact test). Nonunion occurred in 15/108 (13.2%) patients in group S and 8/32 (25.0%) patients in group U (p = 0.180, Fisher’s exact test). Reoperation was required in 6/108 (5.6%) patients in group S and 5/32 (15.6%) patients in group U (p = 0.126, Fisher’s exact test). Reasons for reoperation were implant failure in four patients (three in group S, one in group U), delayed union in six patients (three in group S, three in group U), and infection in one patient in group U. The reoperation procedures included bone grafting only in two patients, arthroplasty with plate or RIN in four, additional plating in four, and implant removal in one patient (Table II).
Table II.
Intraoperative and postoperative outcomes.
| Variable | Group S | Group U | p-value* |
|---|---|---|---|
| Number of patients | 108 | 32 | |
| Malalignment > 7° at last follow-up, n (%) | 12 (11) | 26 (83.9) | < 0.001 |
| Nonunion, n (%) | 14 (13.2) | 9 (29.0) | 0.054 |
| Implant failure, n (%) | 4 (3.7) | 3 (9.7) | 0.182 |
| Reoperation, n (%) | 6 (5.5) | 5 (16.1) | 0.066 |
| Complication, n (%) | 0.108 | ||
| Implant failure | 2 (1.8) | 2 (6.5) | |
| Delayed union | 3 (2.8) | 3 (9.7) | |
| Infection | 1 (0.9) | 0 (0.0) | |
| Procedure, n (%) | 0.403 | ||
| Bone grafting only | 2 (33.3) | 0 (0.0) | |
| Replace with plate | 2 (33.3) | 1 (20.0) | |
| Replace with RIN | 0 (0.0) | 1 (20.0) | |
| Additional plate | 1 (16.7) | 3 (60.0) | |
| Implant removal | 1 (16.7) | 0 (0.0) |
-
*
Fisher's exact test.
-
RIN, retrograde intramedullary nail.
The mean KSS in group U was significantly lower than that in group S at all follow-up periods with using Welch’s t-test each timepoint (75.7 SD 18.8) vs 86.0 (SD 8.7); p < 0.001; 78.9 (SD 17.2) vs 89.1 (SD 9.8); p < 0.001; 85.0 (SD 11.9) vs 91.1 (SD 7.2); p = 0.002, respectively) (Figure 2).
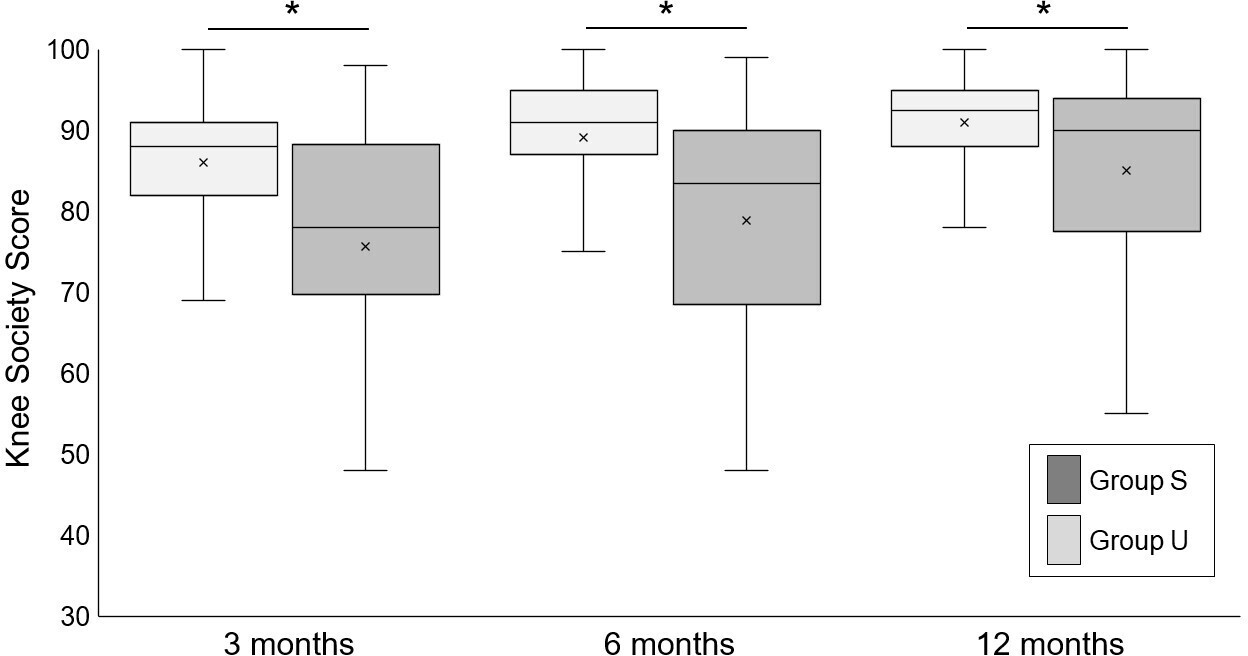
Fig. 2
Box plots for Knee Society Score (KSS) at three, six, and 12 months by intervention group. Boxes show upper and lower interquartile range with the median indicated by the black horizontal line. * indicates a significant difference between the two groups. The mean KSS in group U was significantly lower than that in group S at all follow-up periods.
In the sub-analysis of LCP, nonunion occurred in 5/39 (12.8%) patients in group S and in 4/18 (22.2%) patients in group U with using Fisher’s exact test(p = 0.442, Fisher’s exact test). There were no significant differences in the rates of reoperation and implant failure between the two groups (Supplementary Table i). The mean KSS was higher in group S at three and six months (85.2 vs 71.1; p = 0.001; 88.1 vs 79.0; p = 0.009, respectively, both Welch’s t-test), but there was a significant difference at 12 months using Welch’s t-test at each timepoint (90.5 vs 85.3; p = 0.088) (Figure 3).
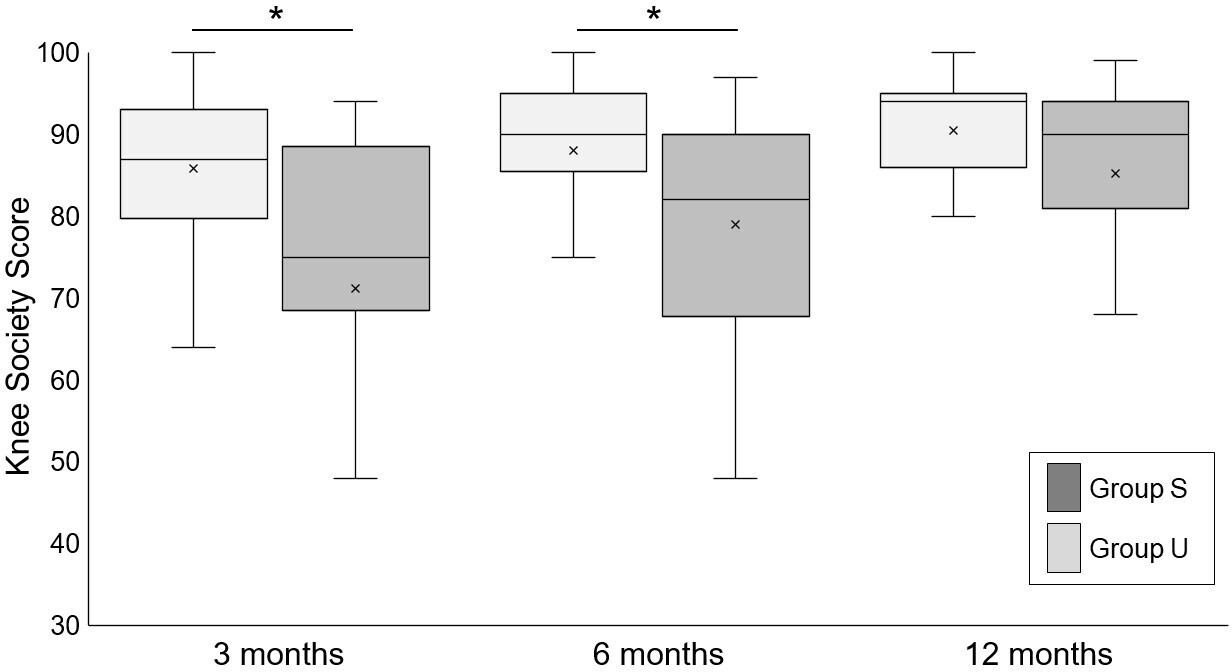
Fig. 3
Box plots for Knee Society Score (KSS) at three, six, and 12 months in the locking compression plate sub-analysis. Boxes show upper and lower interquartile range with the median indicated by the black horizontal line. * indicates a significant difference between the two groups. The mean KSS was significantly higher in group S at three and six months, but there was no significant difference at 12 months.
In the sub-analysis of RIN, the number of nonunion in group S was 10/69 (15.2%) in group S and 4/14 (28.6%) in group U with Fisher’s exact test (p = 0.254). The rate of reoperation was significantly worse in group U (5.8% vs 28.6%; p = 0.025) (Supplementary Tables ii and iii). The mean KSS was higher in group S at six and 12 months using Welch’s t-test at the each timepoint.(89.7 vs 78.7; p = 0.003; 91.4 vs 84.7; p = 0.008) (Figure 4).

Fig. 4
Box plots for Knee Society Score (KSS) at three, six, and 12 months in the retrograde intramedullary nail sub-analysis. Boxes show upper and lower interquartile range with the median indicated by the black horizontal line. * indicates a significant difference between the two groups. There was no significant difference in the mean KSS at three months between the two groups, but the scores at six and 12 months were significantly higher in group S.
Discussion
This is, to our knowledge, the first large-sample report to investigate the effect of accurate intraoperative reduction of distal femur fractures on bone healing and functional outcome. We found that 22.8% (32/140) of patients had the coronal plane malalignment of > 5° at the last follow-up, and this was similar to the results from previous studies with large sample size (22% to 28%).3,17 The present study showed that malalignment after bone healing was strongly impacted by intraoperative fracture malalignment.
There was no significant difference in the rate of nonunion between group S and group U. The rate of nonunion in group U was much higher than that reported in previous studies (25.0% vs 8% to 6%).17,18 Barei and Beingessner19 emphasized the importance of reduction status to reduce healing time. Biological studies have shown that unstable fixation delays healing of the fracture.20 A previous biomechanical study showed varus or valgus loading with greater deformity resulted in more dislocation of the fracture.21 These results suggest that intraoperative coronal plane malalignment resulted in a stronger shearing force on the fracture, making fixation more unstable, and disturbing fracture healing.
The KSS at all follow-up periods was significantly better in group S than group U. Using Neer’s scoring system,22 Zehntner et al5 showed satisfactory alignment of the femur to be compatible with a good functional result. These data indicated that intraoperative fracture malalignment was an important predictor of poor functional outcome in the early postoperative period.
The sub-analyses showed that the rate of reoperation for RIN was significantly worse in group U compared to group S, but there was no significant difference in the rate between the two groups for LCP. This result might be due to the greater stiffness of the RIN compared to the strength of bone. Previous studies using finite element analysis showed that both intramedullary nails and plates are most stressed around the distal screw. Zlowodzki et al23 showed disruption of the distal bone fragment under axial loading in a varus malalignment bone model, whereas only one of eight specimens in the LCP group had loss of fixation. Wähnert et al24 showed splitting of the distal fragment and medial screw cut-out under axial loading. They concluded that RIN was too rigid to hold the screw to the bone through deformation caused by axial loading due to bone malalignment. On the other hand, the differences in the KSS at early postoperative periods in the patients with LCP were greater than those in the patients with RIN. This might be due to the greater axial load stiffness of RIN compared to LCP. Many previous biomechanical studies showed RIN to be more resistant to axial loading than LCP.25,26 Bliemel et al26 showed that the stiffness of the RIN was higher than that of the LCP at 2,500 N axial loading (1,550 N/mm, 910 N/mm, respectively). Taylor et al27 used telemetry to investigate the load on the femur during gait and found that the peak axial force on the femur during gait in a 70 kg subject ranged between 1,487 and 1,718 N. We believe that intramedullary nails are more stable and can be loaded more comfortably in patients with fracture malalignment, thus resulting in better early postoperative functional recovery.
This study has some limitations. First, the retrospective nature of this study carries the inherent risk of observer bias, including the potential for missing data and inability to control confounding variables. Second, we did not adjust for confounding factors using propensity score matching or other methods. In our study design, the number of cases in group U was low, and we were concerned that patient matching would reduce the overall number of cases. Therefore, we excluded open fractures, which were a significant risk factor for nonunion in previous studies.18 We found no significant difference in the patients’ demographic data, so we believe that we could sufficiently reduce confounding factors. Third, we did not evaluate rotational malalignment. Previous studies revealed adverse effects of rotational malalignment in the lower limb.28 Intraoperative fluoroscopy may provide some assistance in the restoration of coronal and sagittal alignments, but there is no reliable method of assessing intraoperative rotational alignment of the lower limb.29 Therefore, we used malalignment in the sagittal and coronal planes for easier intraoperative evaluation in this study. Fourth, we did not assess the articular surface, since this was difficult to determine intraoperatively. As there are almost no papers on the postoperative effects of poor reduction of articular surface in distal femur fractures, and no clear evaluation criteria, we did not evaluate it in this study. Finally, we substituted the intraoperative assessment of malalignment with immediate postoperative radiological assessment. Although we believe this is an effective method for this study design, in actual clinical practice, intraoperative evaluation methods are important, and we were unable to make any recommendations regarding this issue. Scott et al30 proposed an effective intraoperative assessment of coronal alignment using the anatomical lateral distal femoral angle of the contralateral distal femur view.
In conclusion, we found that intraoperative coronal plane malalignment of more than 5° resulted in significantly worse impacts on postoperative functional outcomes. We advocate that the intraoperative alignment should be no more than 5° for good postoperative bone healing and functional prognosis.
References
1. von Keudell A , Shoji K , Nasr M , Lucas R , Dolan R , Weaver MJ . Treatment options for distal femur fractures . J Orthop Trauma . 2016 ; 30 ( 2 ): S25 – S27 . Crossref PubMed Google Scholar
2. Smith JRA , Halliday R , Aquilina AL , et al. Distal femoral fractures: The need to review the standard of care . Injury . 2015 ; 46 ( 6 ): 1084 – 1088 . Crossref PubMed Google Scholar
3. Hoskins W , Sheehy R , Edwards ER , et al. Nails or plates for fracture of the distal femur? data from the Victoria orthopaedic trauma outcomes registry . Bone Joint J . 2016 ; 98-B ( 6 ): 846 – 850 . Google Scholar
4. Gao K , Gao W , Huang J , et al. Retrograde nailing versus locked plating of extra-articular distal femoral fractures: comparison of 36 cases . Med Princ Pract . 2013 ; 22 ( 2 ): 161 – 166 . Crossref PubMed Google Scholar
5. Zehntner MK , Marchesi DG , Burch H , Ganz R . Alignment of supracondylar/intercondylar fractures of the femur after internal fixation by AO/ASIF technique . J Orthop Trauma . 1992 ; 6 ( 3 ): 318 – 326 . Crossref PubMed Google Scholar
6. Charlson M , Szatrowski TP , Peterson J , Gold J . Validation of a combined comorbidity index . J Clin Epidemiol . 1994 ; 47 ( 11 ): 1245 – 1251 . Crossref PubMed Google Scholar
7. Fitz-Henry J . The ASA classification and peri-operative risk . Ann R Coll Surg Engl . 2011 ; 93 ( 3 ): 185 – 187 . Crossref PubMed Google Scholar
8. Meinberg EG , Agel J , Roberts CS , Karam MD , Kellam JF . Fracture and Dislocation Classification Compendium-2018 . J Orthop Trauma . 2018 ; 32 Suppl 1 ( Suppl 1 ): S1 – S170 . Crossref PubMed Google Scholar
9. Kolmert L , Wulff K . Epidemiology and treatment of distal femoral fractures in adults . Acta Orthop Scand . 1982 ; 53 ( 6 ): 957 – 962 . Crossref PubMed Google Scholar
10. Iihara N , Ohara E , Bando Y , Yoshida T , Ohara M , Kirino Y . Fragility fractures in older people in Japan based on the National Health Insurance claims database . Biol Pharm Bull . 2019 ; 42 ( 5 ): 778 – 785 . Crossref PubMed Google Scholar
11. Parker MJ , Palmer CR . A new mobility score for predicting mortality after hip fracture . J Bone Joint Surg Br . 1993 ; 75-B ( 5 ): 797 – 798 . Crossref PubMed Google Scholar
12. Whelan DB , Bhandari M , McKee MD , et al. Interobserver and intraobserver variation in the assessment of the healing of tibial fractures after intramedullary fixation . J Bone Joint Surg Br . 2002 ; 84-B ( 1 ): 15 – 18 . Crossref PubMed Google Scholar
13. Marsh D . Concepts of fracture union, delayed union, and nonunion . Clin Orthop Relat Res . 1998 ; 355S : S22 – S30 . Crossref PubMed Google Scholar
14. Insall JN , Dorr LD , Scott RD , Norman W . Rationale of The Knee Society clinical rating system . Clin Orthop Relat Res . 1989 ; NA ( 248 ): 13 . PubMed Google Scholar
15. Gill S , Mittal A , Raj M , Singh P , Singh J , Kumar S . Extra articular supracondylar femur fractures managed with locked distal femoral plate or supracondylar nailing: a comparative outcome study . J Clin Diagn Res . 2017 ; 11 ( 5 ): RC19 – RC23 . Crossref PubMed Google Scholar
16. Kanda Y . Investigation of the freely available easy-to-use software “EZR” for medical statistics . Bone Marrow Transplant . 2013 ; 48 ( 3 ): 452 – 458 . Google Scholar
17. Vandenbussche E , LeBaron M , Ehlinger M , Flecher X , Pietu G , SOFCOT . Blade-plate fixation for distal femoral fractures: a case-control study . Orthop Traumatol Surg Res . 2014 ; 100 ( 5 ): 555 – 560 . Crossref PubMed Google Scholar
18. Rodriguez EK , Boulton C , Weaver MJ , et al. Predictive factors of distal femoral fracture nonunion after lateral locked plating: a retrospective multicenter case-control study of 283 fractures . Injury . 2014 ; 45 ( 3 ): 554 – 559 . Crossref PubMed Google Scholar
19. Barei DP , Beingessner DM . Open distal femur fractures treated with lateral locked implants: union, secondary bone grafting, and predictive parameters . Orthopedics . 2012 ; 35 ( 6 ): e843 - 6 . Crossref PubMed Google Scholar
20. Einhorn TA , Gerstenfeld LC . Fracture healing: mechanisms and interventions . Nat Rev Rheumatol . 2015 ; 11 ( 1 ): 45 – 54 . Crossref PubMed Google Scholar
21. Bong MR , Egol KA , Koval KJ , et al. Comparison of the LISS and a retrograde-inserted supracondylar intramedullary nail for fixation of a periprosthetic distal femur fracture proximal to a total knee arthroplasty . J Arthroplasty . 2002 ; 17 ( 7 ): 876 – 881 . Crossref PubMed Google Scholar
22. Neer CS , Grantham SA , Shelton ML . Supracondylar fracture of the adult femur. a study of one hundred and ten cases . J Bone Joint Surg Am . 1967 ; 49-A ( 4 ): 591 – 613 . PubMed Google Scholar
23. Zlowodzki M , Williamson S , Cole PA , Zardiackas LD , Kregor PJ . Biomechanical evaluation of the less invasive stabilization system, angled blade plate, and retrograde intramedullary nail for the internal fixation of distal femur fractures . J Orthop Trauma . 2004 ; 18 ( 8 ): 494 – 502 . Crossref PubMed Google Scholar
24. Wähnert D , Hoffmeier K , Fröber R , Hofmann GO , Mückley T . Distal femur fractures of the elderly--different treatment options in a biomechanical comparison . Injury . 2011 ; 42 ( 7 ): 655 – 659 . Crossref PubMed Google Scholar
25. Du Y-R , Ma J-X , Wang S , et al. Comparison of less invasive stabilization system plate and retrograde intramedullary nail in the fixation of femoral supracondylar fractures in the elderly: a biomechanical study . Orthop Surg . 2019 ; 11 ( 2 ): 311 – 317 . Crossref PubMed Google Scholar
26. Bliemel C , Buecking B , Mueller T , et al. Distal femoral fractures in the elderly: biomechanical analysis of a polyaxial angle-stable locking plate versus a retrograde intramedullary nail in a human cadaveric bone model . Arch Orthop Trauma Surg . 2015 ; 135 ( 1 ): 49 – 58 . Crossref PubMed Google Scholar
27. Taylor SJ , Walker PS , Perry JS , Cannon SR , Woledge R . The forces in the distal femur and the knee during walking and other activities measured by telemetry . J Arthroplasty . 1998 ; 13 ( 4 ): 428 – 437 . Crossref PubMed Google Scholar
28. Jaarsma RL , Pakvis DFM , Verdonschot N , Biert J , van Kampen A . Rotational malalignment after intramedullary nailing of femoral fractures . J Orthop Trauma . 2004 ; 18 ( 7 ): 403 – 409 . Crossref PubMed Google Scholar
29. Kim J-W , Oh C-W , Oh J-K , et al. Malalignment after minimally invasive plate osteosynthesis in distal femoral fractures . Injury . 2017 ; 48 ( 3 ): 751 – 757 . Crossref PubMed Google Scholar
30. Scott BR , Wright RD , Moghadamian ES . Intraoperative assessment of coronal alignment in distal femur fracture fixation: technical trick . J Orthop Trauma . 2019 ; 33 ( 2 ): e69 – e72 . Crossref PubMed Google Scholar
Author contributions
Y. Kuwahara: Investigation, Conceptualization, Writing – original draft.
Y. Takegami: Conceptualization, Writing – original draft.
K. Tokutake: Conceptualization, Writing – original draft.
Y. Yamada: Investigation, Writing – original draft.
K. Komaki: Investigation, Writing – original draft.
T. Ichikawa: Writing – original draft.
S. Imagama: Conceptualization, Project administration.
Funding statement
The authors received no financial or material support for the research, authorship, and/or publication of this article.
Acknowledgements
We thank both the participating hospitals for their contribution of data to this study and the members of the trauma research group. Special thanks go to Yuma Saito, Ryutaro Shibata, Yasushi Hiramatsu, Yutaro Ono, Yui Matsura, Koichiro Makihara, Saki Sakurai, Ken Mizuno, Yusuke Mori, and Reika Kaneko for data collection.
Open access funding
The authors confirm that the open access fee for this study was self-funded.
Supplementary material
Tables showing bone healing and functional outcomes for locking compression plate and retrograde intramedullary nail.
© 2022 Author(s) et al. This is an open-access article distributed under the terms of the Creative Commons Attribution Non-Commercial No Derivatives (CC BY-NC-ND 4.0) licence, which permits the copying and redistribution of the work only, and provided the original author and source are credited. See https://creativecommons.org/licenses/by-nc-nd/4.0/.









