Abstract
Aims
Slipped upper femoral epiphysis (SUFE) has well documented biochemical and mechanical risk factors. Femoral and acetabular morphologies seem to be equally important. Acetabular retroversion has a low prevalence in asymptomatic adults. Hips with dysplasia, osteoarthritis, and Perthes’ disease, however, have higher rates, ranging from 18% to 48%. The aim of our study was to assess the prevalence of acetabular retroversion in patients presenting with SUFE using both validated radiological signs and tomographical measurements.
Methods
A retrospective review of all SUFE surgical cases presenting to the Royal Children’s Hospital, Melbourne, Australia, from 2012 to 2019 were evaluated. Preoperative plain radiographs were assessed for slip angle, validated radiological signs of retroversion, and standardized postoperative CT scans were used to assess cranial and mid-acetabular version.
Results
In all, 116 SUFEs presented in 107 patients who underwent surgical intervention; 47 (52%) were male, with a mean age of 12.7 years (7.5 to 16.6). Complete radiological data was available for 91 patients (99 hips) with adequate axial CT imaging of both hips. Overall, 82 patients (82%) underwent pinning in situ (PIS), with subcapital realignment surgery (SRS) performed in 17 patients (18%) (slip angles > 75°). Contralateral prophylactic PIS was performed in 72 patients (87%). On the slip side, 62 patients (68%) had one or more radiological sign of retroversion. Tomographical acetabular retroversion was more pronounced cranially than caudally of the acetabulum on both the affected side and the contralateral side (p < 0.001) as expected in the normal population. Increasing severity of the slip was found to be directly proportional to the degree of reduction in cranial and central acetabular version (p < 0.05) in the SUFE hips.
Conclusion
Acetabular retroversion is more prevalent in patients with SUFE than previously reported, and have been shown be correlated to the severity of the slip presentation. The presence of radiological signs of acetabular retroversion could be used to justify prophylactic contralateral pinning.
Cite this article: Bone Jt Open 2022;3(2):158–164.
Take home message
Acetabular retroversion has increased prevalence in patients presenting with slipped upper femoral epiphysis.
Patients with severe slips have increased acetabular retroversion.
The presence of radiological signs of acetabular retroversion in contralateral hips can be used as justification for prophylactic pinning.
Introduction
Slipped upper femoral epiphysis (SUFE) is the most common disorder affecting the hips of adolescents, with an estimated annual incidence in the USA of 8.8 to 10.8 cases per 100,000 children aged 8 to 15 years.1,2 It is unilateral at initial presentation in 80% of cases, but contralateral slip occurs in up to 41% of patients during follow-up.3 Surgical treatment is warranted for most cases, with different techniques described and related to the severity, stability, and chronicity of the slip, bony anatomy, and surgeon experience.
There are well documented risk factors for SUFE, which are both mechanical and patient-related.4-6 The latter includes endocrinological disorders such as hypogonadism and hypothyroidism, male sex, and low vitamin D.4-6 Obesity ans femoral and acetabular morphological abnormalities play the mechanical counterpart in the aetiology of SUFE. On the acetabular side, femoral head over-coverage with coxa profunda and acetabular retroversion have been related to the epiphyseal separation.7-12 These acetabular dysmorphisms increase the shear forces through the hypertrophic layer of the physis, leading to the characteristic anteriorisation and external rotation of the femoral neck relative to the epiphysis, which remains within the acetabulum.7,9,11,13 On the femoral side, retroversion, physeal orientation, epiphyseal extension, and position/height of the epiphyseal tubercle are the main identified factors related to SUFE.14-18
Radiological signs of acetabular retroversion are commonly identified on the contralateral hip when patients are admitted for surgical treatment of unilateral SUFE. Most common signs include the ischial spine sign (ISS), posterior wall sign (PWS), and crossover sign (COS).14,19,20 A further radiological sign described as the ‘elephant ear sign’, with flared iliac wings has also been shown to be indicative of acetabular retroversion.21 CT-based studies have shown scarce reproducibility and important variation in the measurement of retroversion obtained either preoperatively or postoperatively.11,22 Identifying a hip “at risk” for subsequent SUFE might allow for a single surgical procedure for both hips, potentially preventing a more severe slip at secondary presentation.
The primary aim of this study was to identify the prevalence of acetabular retroversion in patients presenting with SUFE in the affected and contralateral hips using radiological signs and standardized CT measurements. The secondary objective was to correlate the slip severity to the degree of acetabular retroversion.
Methods
After receiving institutional review board approval (Royal Children’s Hospital, Melbourne; ref 66528), we performed a retrospective analysis of our institutional database from 31 January 2012 to 31 January 2019, identifying all cases of SUFE admitted and surgically managed. Patient demographics included age, sex, and weight centile (age-adjusted) are summarized in Table I. Standardized AP and frog leg radiographs were performed; slip severity was determined using the Southwick method,23 and the stability of the slip noted according to Loder3 (Table II). Patients were admitted to the orthopaedic service and underwent surgical management following parental consent. Surgeries performed included pinning in situ (PIS) using cannulated screws (Synthes, Germany), immediate open reduction, capsulotomy and pinning as described by Parsch24 or subcapital realignment using the modified Dunn technique.25 Prophylactic contralateral pinning was performed if the presenting slip was classified as severe or there were other risk factors including younger age (< 11 years), diagnosed endocrinological disorders, obesity with BMI > 95th centile or significant geographical distance from residence to the tertiary medical facility difficulting postoperative follow-up.
Table I.
Cohort characteristics of slipped upper femoral epiphysis (SUFE) patients (n = 91).
| Characteristic | Data |
|---|---|
| Sex, n (%) | |
| Male | 47 (52) |
| Female | 44 (48) |
| BMI percentile, n (%) | |
| > 95th (obese) | 46 (51) |
| 85th to < 95th (overweight) | 23 (25) |
| 5th to 85th (healthy weight) | 22 (24) |
| < 5th (underweight) | 0 (0) |
| Mean age, yrs (SD) | |
| All subjects | 12.6 (1.70) |
| Female | 11.8 (1.35) |
| Male | 12.9 (2.10) |
-
SD, standard deviation.
Table II.
Slipped upper femoral epiphysis (SUFE) characteristics (n = 99).
| Characteristics | N (%) |
|---|---|
| Slip laterality | |
| Left | 49 (54) |
| Right | 34 (37) |
| Bilateral | 8 (9) |
| Slip severity | |
| Mild | 58 (58) |
| Moderate | 20 (21) |
| Severe | 21 (21) |
| Slip stability | |
| Stable | 65 (65) |
| Unstable | 34 (35) |
| SUFE management | |
| Pinning in situ | 78 (78) |
| Immediate closed reduction and pinning | 4 (4) |
| Subcapital realignment | 17 (18) |
| Contralateral hip management (n = 83) | |
| Prophylactic pinning | 72 (83) |
| No intervention | 11 (17) |
During the postoperative hospital admission, all patients underwent a standardized pelvic CT in a neutral pelvic position from the fourth lumbar vertebra down to the lesser trochanters, with lower limbs maintained in neutral rotation (patellae pointing upwards). This was standardized protocol at the host institution to ensure the articular cartilage had not been breached by metalware intraoperatively. Measurements of acetabular version were performed using the method described by Dandachli et al.26 Slight variations in pelvic tilt and rotation were corrected by reformatting the images and defining the planes using standard anatomical references; aligning the left and right anterosuperior iliac spines (ASIS) in the axial plane, the superior portions of the iliac spines in the coronal plane, and the pubic symphysis and the ASIS in the sagittal plane.10
In the re-orientated images, acetabular version was determined as the angle measured in the axial plane between a vertical line (perpendicular to the horizontal axis of the pelvis) and a line connecting the most anterior and posterior points of the acetabular anterior and posterior walls respectively (Figure 1).27 This measurement was conducted at two distinct levels, as described in previous studies: cranially (5 mm from top of acetabulum), determining the superior acetabular version (AVsup) and at the mid acetabular level where the head has the largest diameter (equator), configuring the central acetabular version (AVcen) for both affected and contralateral hips.

Fig. 1
Measurements of the central acetabular version, as published by Dandachli et al.26
Plain radiographs were assessed for adequacy by ensuring the distance from the tip of the coccyx to the superior edge of the symphysis was 2 to 3 cm and that the obturator foramen were symmetrical.28 The radiographs were assessed for radiological signs of acetabular retroversion, as validated by Kawahara et al29 in Perthes' disease patients including, the COS,19 ISS,20 and PWS,14 in addition to assessing the severity of slip at initial presentation30 (Figure 2).

Fig. 2
Anteroposterior radiograph of patient with right slipped upper femoral epiphysis, demonstrating ischial spine sign on the solid line, posterior wall sign on the dashed line, and cross over sign on the dotted line.
All images were reviewed twice, with a minimum two week interval between measurements, by a board-certified orthopaedic surgeon (DS) with an interest in hip preservation. The average value of measurements was taken and used for analysis. Negative values were noted to be true retroversion of the acetabulum; positive values represented acetabular anteversion.
Statistical analysis
Data was handled using Excel version for Mac OS X (Microsoft, USA). For statistical analysis, the paired t-test was used to compare measurements between the affected (slip) and unaffected (non-slip) sides. One-way analysis of variance (ANOVA) was used to identify difference in acetabular version between the mild, moderate, and severe cases. The chi-squared test was performed to determine the difference in the number of radiological signs among patients with increasing slip severity. Intraobserver agreement for version measurements was assessed using the paired t-test and Pearson correlation coefficient (r). Statistical analysis was performed using SPSS version 25 (SPSS, USA). The level of significance used for statistical analysis was p < 0.05.
Results
During our study period, there were 116 SUFEs reported in 107 patients. Complete radiological data with appropriate CT imaging and radiographs were available for 91 patients (99 slips). The mean patient age was 12.6 years (7.5 to 16.6), and 47 patients (52%) were male. The median BMI of patients was in the 95th percentile (interquartile range 82 to 98, weight-adjusted for ages). The left side was affected in 49 patients (54%), and bilateral slips at initial presentation was seen in eight patients (9%). Cohort and SUFE characteristics are shown in Table I and Table II.
Slip severity was mild in 58 hips (58%), moderate in 20 hips (21%), and severe in 21 hips (21%). PIS using 6.5/7.3 mm cannulated hip screws (Synthes, Germany) was performed in all mild and moderate slips. Four severe slips were treated by immediate reduction, with capsulotomy and percutaneous screw fixation as described by Parsch et al24 on the day of presentation. The remaining 17 severe slips underwent subcapital realignment using a modified Dunn technique.25 Prophylactic pinning was performed in 72 of 83 patients (87%).
Tomographical acetabular retroversion was more pronounced in the cranial than in the central portion of the acetabulum on both the affected side (-8.2° (standard deviation (SD) 6.7°) versus 10.3° (SD 4.4°) (p < 0.001, paired t-test), and the contralateral side (-7° (SD 7.2°) versus 11° (SD 4.9°) (p < 0.001, paired t-test). There was no significant difference noted between the slip and non-slip measurements for both AVsup (p = 0.262) and AVcen (p = 0.284) or between males and females (p = 0.421 and p = 0.328, paired t-test, respectively). There was no significant intraobserver difference noted in version measurements (p = 0.340, Kappa test).
One-way ANOVA test confirmed that the increasing severity of the slip was directly proportional to the degree of cranial and central acetabular version (p < 0.05) on the slip side (n = 99). There was no significant difference in the same measurements on the contralateral side (n = 83). (Figure 3 and Figure 4).

Fig. 3
Measurements of cranial acetabular version for slip side (n = 99) and contralateral (non-slip) side (n = 83) by presenting severity of slip. No statistically significant relationship was noted between slip and non-slip side (p = 0.262). *One-way analysis of variance demonstrated increasing retroversion (p = 0.008) on slip side with increasing severity.
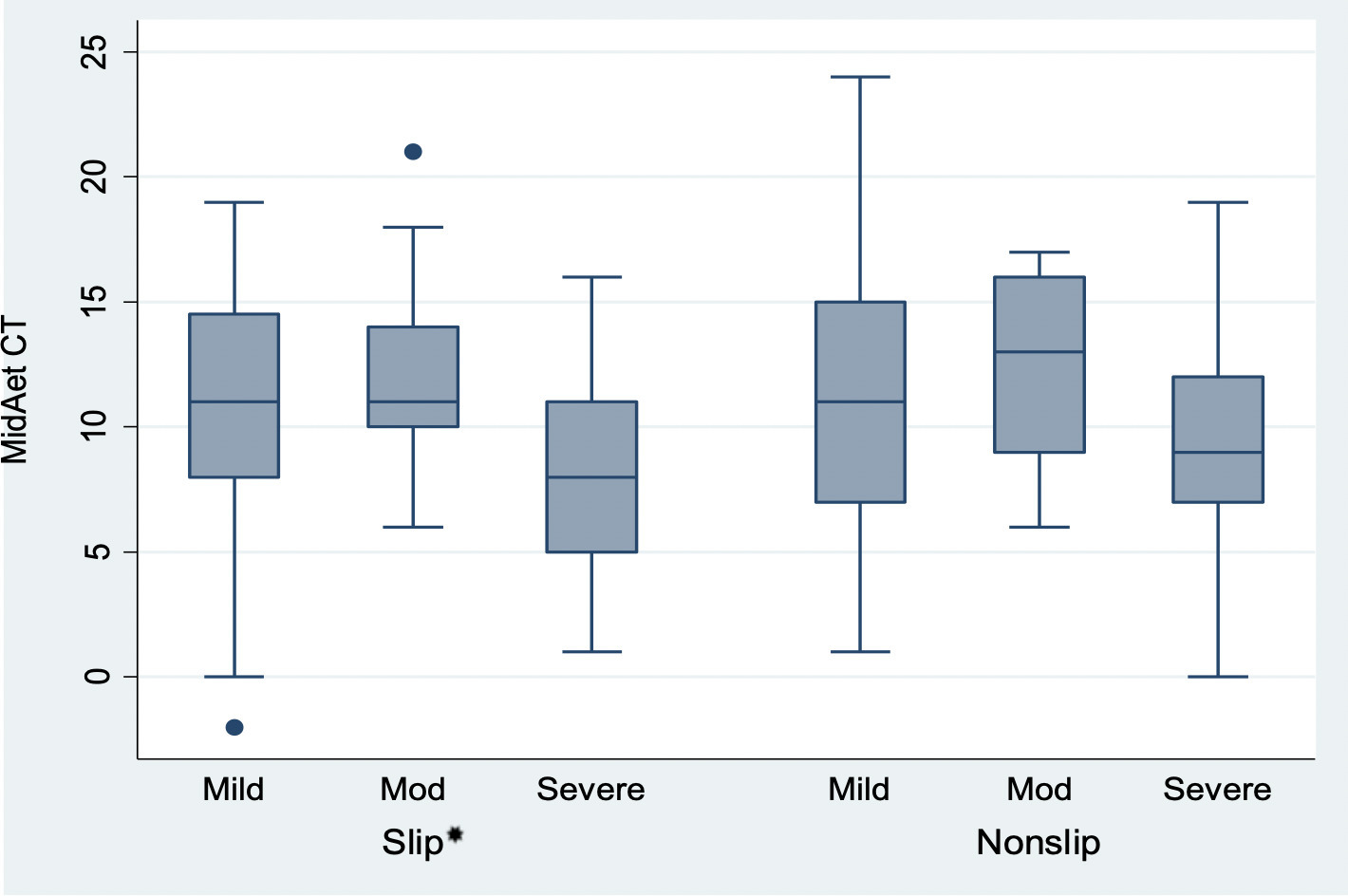
Fig. 4
Measurements of mid-acetabular version for slip side (n = 99) and contralateral (non-slip) side (n = 83) by presenting severity of slip. No statistically significant relationship was noted between slip and non-slip side (p = 0.284). *One-way analysis of variance demonstrated increasing retroversion (p = 0.004) on slip side with increasing severity.
Radiological signs of acetabular retroversion, including COS, ISS, and PWS, were identified in 68% of the hips, with all three signs present in 18%. The presence of the individual radiological signs was not shown to be related to the incidence of slips (p = 0.352, chi-squared test) (Table III and Table IV).
Table III.
Radiological findings on the affected hip.
| SUFE Hips(n=99) | COS, % | PWS, % | ISS, % | One sign, % | Three signs, % | AVsup, ° | AVcen, ° |
|---|---|---|---|---|---|---|---|
| Mild | 44 | 40 | 33 | 63 | 14 | -7.2 | 10.6 |
| Moderate | 41 | 36 | 55 | 82 | 18 | -6.5 | 12.1 |
| Severe | 45 | 55 | 50 | 65 | 30* | -12.1† | 7.7† |
-
Prevalence of radiological signs.
-
*
Increasing severity of slip related to cumulative increase in radiological signs of retroversion; p = 0.020, chi-squared test.
-
†
Statistical difference; p < 0.05, one-way analysis of variance test.
-
AVcen, mid-acetabular version; AVsup, superior acetabular version; COS, cross over sign; ISS, ischial spine sign; PWS, posterior wall sign; SUFE, slipped upper femoral epiphysis.
Table IV.
Prevalence of radiological findings on the contralateral (unaffected) hip.
| Contralateral hips (n = 83) | COS, % | PWS, % | ISS, % | One sign, % | Three signs, % | AVsup, ° | AVcen, ° |
|---|---|---|---|---|---|---|---|
| Mild | 41 | 35 | 27 | 59 | 12 | -6.2 | 11.5 |
| Moderate | 36 | 29 | 36 | 57 | 21 | -7.2 | 12.3 |
| Severe | 35 | 45 | 35 | 65 | 15 | -8.5 | 9.2 |
-
AVcen, mid-acetabular version; AVsup, superior acetabular version; COS, cross over sign; ISS, ischial spine sign; PWS, posterior wall sign.
The PWS was the only radiological sign found to be more prevalent in severe slips compared to mild and moderate slips (p = 0.038, chi-squared test). Using chi-squared test, patients with increasing severity of slips were likely to have a cumulative increase in radiological signs present on plain radiographs (p = 0.021) (Table V).
Table V.
Correlation between the number of radiological signs of acetabular retroversion and the severity of slipped capital femoral epiphysis.
| Radiological signs, n | Mild slip | Moderate slip | Severe slip | Total |
|---|---|---|---|---|
| 0 | 22 | 4 | 6 | 32 |
| 1 | 13 | 10 | 2 | 25 |
| 2 | 14 | 6 | 5 | 25 |
| 3 | 7 | 2 | 8* | 17 |
| Total | 56 | 22 | 21 | 99 |
-
*
Increasing severity of slip related to cumulative increase in radiological signs of retroversion; p = 0.020, chi-squared test.
-
ISS, ischial spine sign; PWS, posterior wall sign; COS, crossover sign.
Discussion
The acetabulum is physiologically anteverted with a mean of 20.7° (SD 3°) equatorially in adults,31 with increasing anteversion noted more caudally.32 Retroversion of the acetabulum is a posterior malrotation in the horizontal plane,6 and has been associated with the development of femoroacetabular impingement and early osteoarthritis of the hip.5,33 Developmental dysplasia of the hip, osteonecrosis, and Perthes' disease have all been shown to have an association with acetabular retroversion.29,34-36 It has been postulated that acetabular retroversion in adolescents can be attributed to insufficient growth of the posterior wall.32 In the largest tomographical study to date on the relationship between acetabular retroversion and SUFE, we have found a statistically significant association, as well as a correlation between increasing retroversion and the severity of the presenting slip.
Podeszwa et al12 described acetabular depth as a risk factor for SUFE in 232 patients, but did not find a relationship between a deep acetabulum and a contralateral slip. More recent studies have not found the depth as a common attribute of SUFE hips, but instead have reported an increased acetabular surface area and pointed to a close relationship between acetabular retroversion and SUFE.4,14,37 We have therefore focused on that factor.
In our sample, hips with SUFE had an mean of 8.2° true cranial acetabular retroversion. This is supported by the findings of Maranho et al4 who in 2020 performed an analysis of 250 patients. Their study, however, was based on one radiological sign of retroversion (the COS), which was found to be an independent factor associated with the development of a contralateral slip. Sankar et al11 found a relationship between acetabular retroversion and SUFE using the radiological COS and PWS, with more recent studies showing an increased incidence of the same signs when compared to a matched control population.38
Radiological measurements are less precise than tomographical measurements of acetabular version, with low intraobserver and interobserver agreement.39 Uncorrected pelvic tilt has the potential to overestimate acetabular retroversion.28,40 Moreover, an MRI-based study demonstrated that the posterior acetabular wall ossifies at a later age than the anterior wall, fusing just prior to closure of the triradiate cartilage. This can make radiological imaging inaccurate in the determination of retroversion in young patients. Therefore, tomographical acetabular measurements tend to be more accurate for version analysis.15
A matched cohort study by Hesper et al14 used tomographical measurement of acetabular version, and found the mean cranial version was lower for SUFE hips (2.7°) compared to the contralateral (6.6°) or control hips (9.6°). These findings were similar to those previously published by Monazzam et al.13 Moreover, in the former study, the version at the equator of the joint was also found to be inferior in SUFE hips than on the other two groups, and there was a direct relationship between severe slips and higher retroversion. Their findings are concurrent with our findings, albeit that a higher magnitude of retroversion compared to typical values were found in our measurements. That difference may be related to populational differences, as demonstrated in a recent paper from Venkatadass et al.41
Our study sample had demographic characteristics that corresponded to the typical age and sex distribution previously described in the literature, except for the fact that we had a larger number of affected females.9,42 We believe BMI evaluation has importance since it has been previously shown that obesity may increase shear forces enough to overcome the yield point of the physis.43 Moreover, the influence of obesity-related hormones, such as insulin, in the growth plate might also help in weakening the latter and predispose to SUFE.44 Even though bilateral slips are present in up to 60% of patients in the follow-up of the index operation, we prophylactically fixed 87% of our patients. That is mostly related to the fact that the hospital where we conducted the study receives patients from distant rural areas, making close follow-up difficult.
Limitations of the study include the lack of comparison of acetabular version measurements of the normal population from the institution, as well as the limitations present in a retrospective analysis of a heterogenous cohort of patients, with potential selection biases. The single reviewer of radiological signs and measurements (DS) did also not allow for the determination of interobserver reliability; however, previous literature has shown excellent levels of interobserver agreement when conducting these measurements with variation of < 1°.32
This study is the largest cohort to date with combined radiological and tomographical evaluation of acetabular retroversion in SUFE patients. The timely tomographical analysis allows for improved understanding, providing accurate measurement of acetabular version at the time of presentation, and questioning the theory that acetabular retroversion is a pathological response to SUFE. In addition, we have shown a relationship between the increasing severity of slip with acetabular retroversion measurements and with the number of radiological signs present on the presenting anteroposterior radiograph, previously not described in the literature.
In conclusion, our study documents acetabular retroversion is prevalent in patients presenting with SUFE in comparison to published literature. The degree of retroversion can be correlated to the severity of the slip presentation: severe slips are found to have acetabuli that are at least 4° more retroverted than those in mild or moderate slips at both the cranial and central level. Further work is required to assess if acetabular retroversion is truly a risk factor for SUFE; however, the presence of radiological signs could allow for the justification of prophylactic contralateral pinning in patients presented with SUFE.
References
1. Larson AN , Yu EM , Melton LJ 3rd , Peterson HA , Stans AA . Incidence of slipped capital femoral epiphysis: a population-based study . J Pediatr Orthop B . 2010 ; 19 ( 1 ): 9 – 12 . Crossref PubMed Google Scholar
2. Lehmann CL , Arons RR , Loder RT , Vitale MG . The epidemiology of slipped capital femoral epiphysis: an update . J Pediatr Orthop . 2006 ; 26 ( 3 ): 286 – 290 . Crossref PubMed Google Scholar
3. Loder RT , Richards BS , Shapiro PS , Reznick LR , Aronson DD . Acute slipped capital femoral epiphysis: the importance of physeal stability . J Bone Joint Surg Am . 1993 ; 75-A ( 8 ): 1134 – 1140 . Crossref PubMed Google Scholar
4. Maranho DA , Miller P , Kim Y-J , Novais EN . Contralateral slip after unilateral slipped capital femoral epiphysis is associated with acetabular retroversion but not increased acetabular depth and overcoverage . J Pediatr Orthop B . 2020 ; 29 ( 3 ): 275 – 282 . Google Scholar
5. Kim WY , Hutchinson CE , Andrew JG , Allen PD . The relationship between acetabular retroversion and osteoarthritis of the hip . J Bone Joint Surg Br . 2006 ; 88-B ( 6 ): 727 – 729 . Crossref PubMed Google Scholar
6. Reynolds D , Lucas J , Klaue K . Retroversion of the acetabulum: a cause of hip pain . Bone Joint J . 1999 ; 81-B ( 2 ): 281 – 288 . Google Scholar
7. Loder RT , Wittenberg B , DeSilva G . Slipped capital femoral epiphysis associated with endocrine disorders . J Pediatr Orthop . 1995 ; 15 ( 3 ): 349 – 356 . Crossref PubMed Google Scholar
8. Madhuri V , Arora SK , Dutt V . Slipped capital femoral epiphysis associated with vitamin D deficiency: a series of 15 cases . Bone Joint J . 2013 ; 95-B ( 6 ): 851 – 854 . Crossref PubMed Google Scholar
9. Perry DC , Metcalfe D , Lane S , Turner S . Childhood obesity and slipped capital femoral epiphysis . Pediatrics . 2018 ; 142 ( 5 ): e20181067 . Crossref PubMed Google Scholar
10. Kitadai HK , Milani C , Nery CA , Filho JL . Wiberg’s center-edge angle in patients with slipped capital femoral epiphysis . J Pediatr Orthop . 1999 ; 19 ( 1 ): 97 – 105 . Google Scholar
11. Sankar WN , Brighton BK , Kim Y-. J , Millis MB . Acetabular morphology in slipped capital femoral epiphysis . J Pediatr Orthop . 2011 ; 31 ( 3 ): 254 – 258 . Crossref PubMed Google Scholar
12. Podeszwa DA , Gurd D , Riccio A , De La Rocha A , Sucato DJ . Increased acetabular depth may influence physeal stability in slipped capital femoral epiphysis . Clin Orthop Relat Res . 2013 ; 471 ( 7 ): 2151 – 2155 . Crossref PubMed Google Scholar
13. Monazzam S , Krishnamoorthy V , Bittersohl B , Bomar JD , Hosalkar HS . Is the acetabulum retroverted in slipped capital femoral epiphysis? Clin Orthop Relat Res . 2013 ; 471 ( 7 ): 2145 – 2150 . Crossref PubMed Google Scholar
14. Hesper T , Bixby SD , Kim Y-. J , et al. Acetabular retroversion, but not increased acetabular depth or coverage, in slipped capital femoral epiphysis: A matched-cohort study . J Bone Joint Surg Am . 2017 ; 99-A ( 12 ): 1022 – 1029 . Google Scholar
15. Morris WZ , Chen JY , Cooperman DR , Liu RW . Characterization of ossification of the posterior rim of acetabulum in the developing hip and its impact on the assessment of femoroacetabular impingement . J Bone Joint Surg Am . 2015 ; 97-A ( 3 ): e11 . Crossref PubMed Google Scholar
16. Bellemore JM , Carpenter EC , Yu NYC , Birke O , Little DG . Biomechanics of slipped capital femoral epiphysis: Evaluation of the posterior sloping angle . J Pediatr Orthop . 2016 ; 36 ( 6 ): 651 – 655 . Crossref PubMed Google Scholar
17. Maranho DA , Davila-Parrilla A , Miller PE , Kim Y. J , Novais EN , Millis MB . Acetabular morphology in slipped capital femoral epiphysis: comparison at treatment onset and skeletal maturity . J Child Orthop . 2018 ; 12 ( 5 ): 444 – 453 . Crossref PubMed Google Scholar
18. Novais EN , Hosseinzadeh S , Emami SA , Maranho DA , Kim YJ , Kiapour AM . What is the association among epiphyseal rotation, translation, and the morphology of the epiphysis and metaphysis in slipped capital femoral epiphysis? Clin Orthop Relat Res . 2021 ; 479 ( 5 ): 935 – 944 . Crossref PubMed Google Scholar
19. Jamali AA , Mladenov K , Meyer DC , et al. Anteroposterior pelvic radiographs to assess acetabular retroversion: High validity of the “cross-over-sign.” J Orthop Res . 2007 ; 25 ( 6 ): 758 – 765 . Google Scholar
20. Kalberer F , Sierra RJ , Madan SS , Ganz R , Leunig M . Ischial spine projection into the pelvis : a new sign for acetabular retroversion . Clin Orthop Relat Res . 2008 ; 466 ( 3 ): 677 – 683 . Crossref PubMed Google Scholar
21. Tian S , Vahedi H , Goswami K , Parvizi J . Elephant’s ear sign: a new radiographic finding indicative of acetabular retroversion . Arthroplasty Today . 2020 ; 6 ( 1 ): 59 – 61 . Google Scholar
22. Bauer JP , Roy DR , Thomas SS . Acetabular retroversion in post slipped capital femoral epiphysis deformity . J Child Orthop . 2013 ; 7 ( 2 ): 91 – 94 . Crossref PubMed Google Scholar
23. Southwick WO . Osteotomy through the lesser trochanter for slipped capital femoral epiphysis . J Bone Joint Surg Am . 1967 ; 49-A ( 5 ): 807 – 835 . PubMed Google Scholar
24. Parsch K , Weller S , Parsch D . Open reduction and smooth Kirschner wire fixation for unstable slipped capital femoral epiphysis . J Pediatr Orthop . 2009 ; 29 ( 1 ): 1 – 8 . Crossref PubMed Google Scholar
25. Leunig M , Slongo T , Kleinschmidt M , Ganz R . Subcapital correction osteotomy in slipped capital femoral epiphysis by means of surgical hip dislocation . Open Orthop Traumatol . 2007 ; 19 : 389 – 410 . Crossref PubMed Google Scholar
26. Dandachli W , Ul Islam S , Tippett R , Hall-Craggs MA , Witt JD . Analysis of acetabular version in the native hip: comparison between 2D axial CT and 3D CT measurements . Skeletal Radiol . 2011 ; 40 ( 7 ): 877 – 883 . Crossref PubMed Google Scholar
27. Direito-Santos B , França G , Nunes J , et al. Acetabular retroversion: Diagnosis and treatment . EFORT Open Rev . 2018 ; 3 ( 11 ): 595 – 603 . Crossref PubMed Google Scholar
28. Siebenrock KA , Kalbermatten DF , Ganz R . Effect of pelvic tilt on acetabular retroversion: A study of pelves from cadavers . Clin Orthop Relat Res . 2003 ; 407 : 241 – 248 . Crossref PubMed Google Scholar
29. Kawahara S , Nakashima Y , Oketani H , et al. High prevalence of acetabular retroversion in both affected and unaffected hips after Legg-Calvé-Perthes disease . J Orthop Sci . 2012 ; 17 ( 3 ): 226 – 232 . Crossref PubMed Google Scholar
30. Diaz-Ledezma C , Novack T , Marin-Peña O , Parvizi J . The relevance of the radiological signs of acetabular retroversion among patients with femoroacetabular impingement . Bone Joint J . 2013 ; 95-B ( 7 ): 893 – 899 . Crossref PubMed Google Scholar
31. Krebs V , Incavo SJ , Shields WH . The anatomy of the acetabulum: what is normal? Clin Orthop Relat Res . 2009 ; 467 ( 4 ): 868 – 875 . Crossref PubMed Google Scholar
32. Hingsammer AM , Bixby S , Zurakowski D , Yen YM , Kim YJ . How do acetabular version and femoral head coverage change with skeletal maturity? Clin Orthop Relat Res . 2015 ; 473 ( 4 ): 1224 – 1233 . Crossref PubMed Google Scholar
33. Giori NJ , Trousdale RT . Acetabular retroversion is associated with osteoarthritis of the hip . Clin Orthop Relat Res . 2003 ; 417 : 263 – 269 . Crossref PubMed Google Scholar
34. Ezoe M , Naito M , Inoue T . The prevalence of acetabular retroversion among various disorders of the hip . J Bone Joint Surg Am . 2006 ; 88-A ( 2 ): 372 – 379 . Crossref PubMed Google Scholar
35. Fujii M , Nakashima Y , Yamamoto T , et al. Acetabular retroversion in developmental dysplasia of the hip . J Bone Joint Surg Am . 2010 ; 92-A ( 4 ): 895 – 903 . Crossref PubMed Google Scholar
36. Troelsen A , Rømer L , Jacobsen S , Ladelund S , Søballe K . Cranial acetabular retroversion is common in developmental dysplasia of the hip as assessed by the weight bearing position . Acta Orthop . 2010 ; 81 ( 4 ): 436 – 441 . Crossref PubMed Google Scholar
37. Paez CJ , Bomar JD , Farnsworth CL , Bandaralage H , Upasani VV . Three-dimensional analysis of acetabular morphology and orientation in patients with slipped capital femoral epiphysis . J Pediatr Orthop . 2021 ; 41 ( 2 ): e130 – e134 . Crossref PubMed Google Scholar
38. Galletta C , Aprato A , Giachino M , et al. Hip morphology in slipped capital femoral epiphysis . J Pediatr Orthop B . 2020 ; 30 ( 6 ): 535 – 539 . Crossref PubMed Google Scholar
39. Kappe T , Kocak T , Neuerburg C , Lippacher S , Bieger R , Reichel H . Reliability of radiographic signs for acetabular retroversion . Int Orthop . 2011 ; 35 ( 6 ): 817 – 821 . Crossref PubMed Google Scholar
40. Abel MF , Sutherland DH , Wenger DR , Mubarak SJ . Evaluation of CT scans and 3-D reformatted images for quantitative assessment of the hip . J Pediatr Orthop . 1994 ; 14 ( 1 ): 48 – 53 . Crossref PubMed Google Scholar
41. Venkatadass K , Muthukumar S , Gomathi A , Rajasekaran S . Is the acetabulum retroverted in SCFE? A study of acetabular morphology in Indian children with SCFE . Indian J Orthop . 2021 ; 55 ( 1 ): 142 – 146 . Crossref PubMed Google Scholar
42. Herngren B , Stenmarker M , Vavruch L , Hagglund G . Slipped capital femoral epiphysis: a population-based study . BMC Musculoskelet Disord . 2017 ; 18 ( 1 ). Crossref PubMed Google Scholar
43. Fishkin Z , Armstrong DG , Shah H , Patra A , Mihalko WM . Proximal femoral physis shear in slipped capital femoral epiphysis--a finite element study . J Pediatr Orthop . 2006 ; 26 ( 3 ): 291 – 294 . Crossref PubMed Google Scholar
44. Montañez-Alvarez M , Flores-Navarro HH , Cuevas-De Alba C , Arana-Hernández EI , Ramírez-Ruiz M . The role of hyperinsulinemia in slipped capital femoral epiphysis . J Pediatr Orthop . 2020 ; 40 ( 8 ): 413 – 417 . Crossref PubMed Google Scholar
Author contributions
P. Buddhdev: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Writing – original draft, Writing – review & editing.
F. Vallim: Data curation, Formal analysis, Validation, Methodology, Writing – original draft, Writing – review & editing.
D. Slattery: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Supervision, Visualization, Writing – review & editing.
J. Balakumar: Conceptualization, Methodology, Supervision, Validation, Visualization, Writing – review & editing.
Funding statement
The author(s) received no financial or material support for the research, authorship, and/or publication of this article.
ICMJE COI statement
J. Balakumar reports royalties and consulting fees from Medacata, Johnson & Johnson, and Arthrex; payment or honoraria for lectures, presentations, speakers bureaus, manuscript writing, or educational events from Mathys, and the Singapore Orthopaedic Association; support for attending meetings and/or travel from ISHA and the Singapore Orthopaedic Association; and being chairman of MEND Orthopaedic Nutrition Australia, all of which is unrelated to this work.
Ethical review statement
Institutional review board approval was obtained by Royal Children’s Hospital, Melbourne, Australia (ref 66528).
Open access funding
The authors report that the open access funding for this manuscript was self-funded.
Follow P. Buddhdev @Pranai_B
Follow J. Balakumar @BalakumarJit
Follow the Royal Children's Hospital, Melbourne, Australia @RCHMelbourne
Follow the Mid and South Essex NHS Foundation Trust @MSEHospitals
© 2022 Author(s) et al. This is an open-access article distributed under the terms of the Creative Commons Attribution Non-Commercial No Derivatives (CC BY-NC-ND 4.0) licence, which permits the copying and redistribution of the work only, and provided the original author and source are credited. See https://creativecommons.org/licenses/by-nc-nd/4.0/.









