Abstract
Aims
Periprosthetic joint infection (PJI) occurs in approximately 1% to 2% of total knee arthroplasties (TKA) presenting multiple challenges, such as difficulty in diagnosis, technical complexity, and financial costs. Two-stage exchange is the gold standard for treating PJI but emerging evidence suggests 'two-in-one' single-stage revision as an alternative, delivering comparable outcomes, reduced morbidity, and cost-effectiveness. This study investigates five-year results of modified single-stage revision for treatment of PJI following TKA with bone loss.
Methods
Patients were identified from prospective data on all TKA patients with PJI following the primary procedure. Inclusion criteria were: revision for PJI with bone loss requiring reconstruction, and a minimum five years’ follow-up. Patients were followed up for recurrent infection and assessment of function. Tools used to assess function were Oxford Knee Score (OKS) and American Knee Society Score (AKSS).
Results
A total of 24 patients were included with a mean age of 72.7 years (SD 7.6), mean BMI of 33.3 kg/m2 (SD 5.7), and median ASA grade of 2 (interquartile range 2 to 4). Mean time from primary to revision was 3.0 years (10 months to 8.3 years). At revision, six patients had discharging sinus and three patients had negative cultures from tissue samples or aspirates. Two patients developed recurrence of infection: one was treated successfully with antibiotic suppression and one underwent debridement, antibiotics, and implant retention. Mean AKSS scores at two years showed significant improvement from baseline (27.1 (SD 10.2 ) vs 80.3 (SD 14.8); p < 0.001). There was no significant change in mean AKSS scores between two and five years (80.3 (SD 14.8 ) vs 74.1 (SD 19.8); p = 0.109). Five-year OKS scores were not significantly different compared to two-year scores (36.17 (SD 3.7) vs 33.0 (SD 8.5); p = 0.081).
Conclusion
‘Two-in-one’ single-stage revision is effective for treating PJI following TKA with bone loss, providing patients with sustained improvements in outcomes and infection clearance up to five years post-procedure.
Cite this article: Bone Jt Open 2022;3(2):107–113.
Take home message
This prospective study demonstrates that a single stage approach using the two-in-one technique for revision of infected total knee arthroplasty provides comparable outcomes at five years to current gold standard techniques.
The two-in-one single stage technique in suitable patients performs similarly to two-stage revision, with the benefits of a single procedure and hospital admission.
Introduction
Periprosthetic joint infection (PJI) is a devastating complication of arthroplasty, with the incidence estimated to be between 1% and 2% following primary knee arthroplasty.1 Despite the incidence of infection being relatively small, it presents a significant economic burden, with some revision total knee arthroplasty (TKA) procedures costing NHS England in excess of £75,000 per patient. This is due to the associated high patient morbidity, difficulty of diagnosis, and the complexity and duration of management.2
The number of knee arthroplasties performed worldwide increases year on year, with the National Joint Registry (covering England, Wales, Northern Ireland, the Isle of Man, and the States of Guernsey) recording a total of 108,506 primary procedures in 2019. This is a 33% increase from the 85,066 performed in 2011. Revision knee procedures have also increased to 7,008 in 2019 from 5,804 in 2011, equating to an increase of 21%.3
The Scottish Arthroplasty Project is a well-established quality assurance monitoring programme for total joint replacement in Scotland, serving some of the same functions as the NJR. Its annual reports show that the number of primary TKAs performed in Scotland has effectively doubled since its inception, from 3,343 in 2001 to 7,720 in 2019. There has been an equal rise in the number for revision procedures, from 249 in 2001 to 457 in 2019.4
PJI is the second most common indication for revision surgery. Revisions undertaken due to infection have a higher risk of complications with a significantly longer length of hospitalization, higher rates of readmission, and higher rates of both mortality and morbidity.5
The gold standard for infected knee arthroplasty revision is the two-stage procedure, described by Insall et al6 in 1983. This involves one operation to remove the primary implants and debride infected tissue, followed by the implantation of an antibiotic-impregnated cement spacer. This is followed by a minimum course of antibiotics of two weeks before a second operation to insert the new definitive prosthesis is undertaken. This procedure has been shown to produce reliable outcomes for the management of infection in TKA.7 Some cases are suitable to undergo explantation, washout, debridement, and re-implantation in a single procedure under single anaesthetic, referred to as a single-stage revision.8 Despite these stringent measures for both approaches to infected knee arthroplasty, current studies report the recurrence rates of between 9% to 33%.7,9
A more recent development which is gaining popularity among orthopaedic surgeons is the single-stage ‘two-in-one’ revision arthroplasty.10 The core principles of this procedure are the same as the gold standard, with extensive debridement of non-viable and infected tissue, removal of implants, and cement. The major difference is that the new definitive prosthesis is then implanted at the same sitting after a short period of time to allow redraping and the use of new, sterile instruments.7,9
Bone loss provides a major challenge in revision surgery, particularly in the context of PJI. The most widely used classification system for bone loss is the Anderson Orthopaedic Research Institute (AORI).11,12 This classification system is popular due to its relatively simplicity, reproducibility, and utility in aiding with operative decision-making. It is graded on a 1 to 3 scale, based on the degree of metaphyseal comprise of the femur and tibia. Grade 1 is minimal metaphyseal bone loss; grade 2 is metaphyseal bone loss with associated cancellous bone loss. This can be subdivided into 2A and 2B if there is unicondylar or bicondylar bone loss, in the case of the femur, or unilateral or bilateral loss of the tibial halfplate in the case of the tibia. Grade 3 is complete loss of the metaphyseal portion with both condyles/halfplates.13
The epiphyseal surface (zone 1) is often significantly comprised as a direct result of the infection, but also because of the removal of cement and the debridement that is necessary to remove the infected tissue. This can often leave a large bone defect that is insufficient for adequate fixation. The metaphyseal area (zone 2), however, tends to be relatively well preserved and offers higher-quality bone that is more suitable for fixation.14 This is a phenomenon that implant manufacturers have sought to use.
Metaphyseal sleeves have been in use since the 1970s and there are good long-term results for noninfective cases that show high rates of osseointegration, low rates of aseptic loosening, and good functional outcomes.15,16 It has been demonstrated by several authors that the use of a metaphyseal sleeve in context of revision TKA for infection shows promising short- to mid-term results.17-19 The reinfection rates are comparable to other revision techniques with low rates of aseptic loosening, high rates of osseointegration, and good functional outcomes, but longer-term data are needed.9,17
The aim of this study was to report the medium-term follow-up prospectively collected outcome data at two- and five-year follow-up for a consecutive case series of infected primary TKAs treated with a two-in-one single-stage revision using metaphyseal sleeves to address bone loss. This builds on work previously done at our institution. This work showed that the use of metaphyseal sleeves in a two-in-one single-stage revision for infected TKA with associated bone loss is a safe and effective treatment option in treating deep infection of TKA, and has a low recurrence of infection at two-year follow-up.10 The primary outcome measure was recurrence of infection. Secondary outcome measures were implant failure, reoperation rate, reinfection rate, American Knee Society Score (AKSS),20 and Oxford Knee Score (OKS).21,22
Methods
Our unit prospectively collects data on all patients undergoing primary and revision TKA with data held in a local database. From this locally held database, we identified patients presenting to our institution with infected primary TKA requiring revision between 2009 and 2017. The inclusion criteria were patients undergoing a single-stage revision for deep PJI with associated bone loss on femoral, tibial, or both surfaces. No exclusions were made for patient factors, presence of a sinus, infecting organism, or primary implant. The exclusion criteria used were: patients presenting with life-threatening sepsis requiring urgent joint washout and debridement as these patients require treatment with two-stage revision, and patients with acute infection (less than four weeks since primary procedure) who were deemed suitable for debridement, antibiotics, irrigation, and implant retention (DAIR). This decision was made by the treating consultant orthopaedic surgeon (PW, IJB). The study protocol was approved by our local research and ethics committee. The diagnosis of infection was made using clinical evaluation, blood tests, radiological findings, microscopy, and culture of joint aspirate.
Demographic data were collected for all patients including age, sex, affected side, BMI, American Society of Anesthesiologists score,23 admission pain score (visual analogue scale (VAS) from 0 (no pain) to 5 (severe pain)), AKSS, OKS, range of motion assessment, and date of primary arthroplasty. Preoperative blood serum CRP level was measured. A minimum of one knee joint aspirate was taken preoperatively under sterile conditions in theatre for microscopy and culture to identify infecting organisms. This was done for diagnostic purposes and to guide antibiotic therapy. Bone loss was quantified at the time of surgery by the lead surgeon using the AORI classification. Radiographs were taken preoperatively, one to four days postoperatively, and one year, three years, and five years post-procedure.
Surgical technique
All procedures were undertaken as single-stage revisions by one of two experienced revision knee surgeons (PW, IJB) in the unit. The indication for revision was a proven infected TKA defined by both senior surgeons. Infection was diagnosed by raised haematological inflammatory markers, positive joint aspirate, or multiple intraoperative deep tissue samples (same organism on > three samples). Primary procedures were performed in all cases between 1993 and 2016 with the mean time from primary procedure to revision 3.5 years (0.2 to 12).
The majority of the procedures (21 out of 26) were performed under spinal or epidural anaesthesia, with the remaining patients requiring a general anaesthetic. Preoperatively, all cases were discussed with a consultant microbiologist with a special interest in musculoskeletal infection. A tailored antibiotic protocol was drawn up individually for each case. All procedures were carried out with the use of a thigh tourniquet. The incision was made through the most lateral previous scar, and a medial parapatellar approach was used in all cases. The original scar was excised along with any sinus present, and the current prosthesis was removed. No cases required a tibial tubercle osteotomy. A radical debridement of the adjacent bone and soft-tissues was performed, with at least six tissue samples sent from different areas of the knee for culture and sensitivity. Thorough pulsatile lavage was carried out with a minimum of three litres of normal saline, and the intramedullary canals packed with gauze swabs soaked with chlorhexidine. The wound was temporarily closed at this stage, with all patients receiving 500 mg tranexamic acid. The tourniquet was then deflated. Antibiotic therapy was commenced, and the whole surgical team re-scrubbed and new instruments were used for the next stage.
AORI grading was carried out intraoperatively by the lead surgeon (PW, IJB) following complete removal of the primary prosthesis along with any infected bone, fibrous tissue, or necrotic tissue. Following grading, a decision was made regarding the most appropriate construct for the bone loss and collateral ligaments. A metaphyseal press-fit prosthesis (DePuy Orthopaedics, USA) was used in 25 of the 26 cases. A Noiles Hinge (DePuy Orthopaedics) knee was required in one case due to instability. This case was excluded from the study, leaving 25 cases for review. The residual femoral bone loss in each case was then assessed by the primary surgeon using the AORI grading system. The femoral component was sized, with augments being used when required. Sleeves were used in every case in the tibia and in all but two in the femur.
A stem was used at the operating surgeon’s discretion (15/25 cases in the tibia and 8/25 cases in the femur). Stems were only used for uncontained grade 2 and grade 3 defects in either the metaphysis (zone 2), or diaphysis (zone 3).14 Bone cement (Gentamicin-loaded Palacos cement; Heraeus Medical, Germany) was used only under the tibial tray and not around the sleeve or the stem. The femoral component was cemented in place with additional antibiotics in the cement (Gentamicin-loaded Palacos cement). No cement was implanted around the femoral sleeve or stem. No additional antibiotics were added to the cement. No local cement beads were used in this series. At the end of the procedure, a second 500 mg of tranexamic acid was given. Drains were not used in any of the cases.
All the patients were nursed on an orthopaedic ward with a standardized mobilization protocol allowing full weightbearing immediately. Duration of surgery, pre- and postoperative haemoglobin, transfusion rate, and complications were recorded.
All patients received postoperative anticoagulation therapy in the form of an oral factor Xa inhibitor (Rivaroxaban). This was continued for minimum of 28 days as per the standardized protocol. In cases of warfarinized patients (four cases) the warfarin was stopped preoperatively and they were given low-molecular-weight heparin perioperatively. The warfarin was then restarted at the original postoperative dose. Antibiotics were restarted immediately postoperatively and adjusted according to final microbiological results. The timing of conversion to oral antibiotics was decided by a consultant microbiologist on a case-by-case basis. This varied from eight days to six weeks. All patients were then placed on two oral agents, which were continued for four weeks after CRP had returned to normal. Serial CRP measurements were taken until the level had plateaued for four weeks at less than 10 mg/l.
Follow-up
Patients were followed up by the operating surgeon. They were seen regularly in the first six months at varying intervals until CRP was normal. They were then reviewed every six months until two years postoperatively, and yearly thereafter. No patients were discharged during the study period. Initially, preoperative scores were not collected, and in some cases pain made it difficult to measure preoperative and postoperative movement.
In addition, all patients in NHS Scotland are monitored via the Scottish Arthroplasty Project (SAP) through their hospital number, and any reoperations, complications, or mortality are recorded. Follow-up ranged from five years to 11 years. Any clinical recurrence of infection was noted. AKSS, OKS, pain, and satisfaction scores (using a five-point VAS) were completed one year postoperatively and every year following that. Only patients with at least five years’ follow-up were eligible for inclusion in the five-year follow-up cohort.
Statistical analysis
Statistical analysis was performed using SPSS Statistics Package v. 25 (IBM, USA). Paired t-tests were used for parametric continuous data, with two tailed p-values reported and statistical significance set at p < 0.05, with 95% confidence intervals. Preoperative, two-year postoperative, and five-year postoperative AKSS and OKS scores were compared using the paired t-tests (following Shapiro-Wilk test of normality) to identify significant differences.
Results
During the initial study, 31 patients met the inclusion criteria. Five of these patients required two-stage procedures, due to the presence of any polymicrobial organisms, poor bioavailability of required antibiotic, or acute sepsis-driven medical instability, and were excluded. One patient required a hinged prosthesis, and was also excluded.
This left an initial study group of 25 patients, 24 of whom were available for contact in this five-year follow-up study, with one lost to follow-up. Figure 1 illustrates all patients initially meeting entry criteria, to patients included in the final analysis.
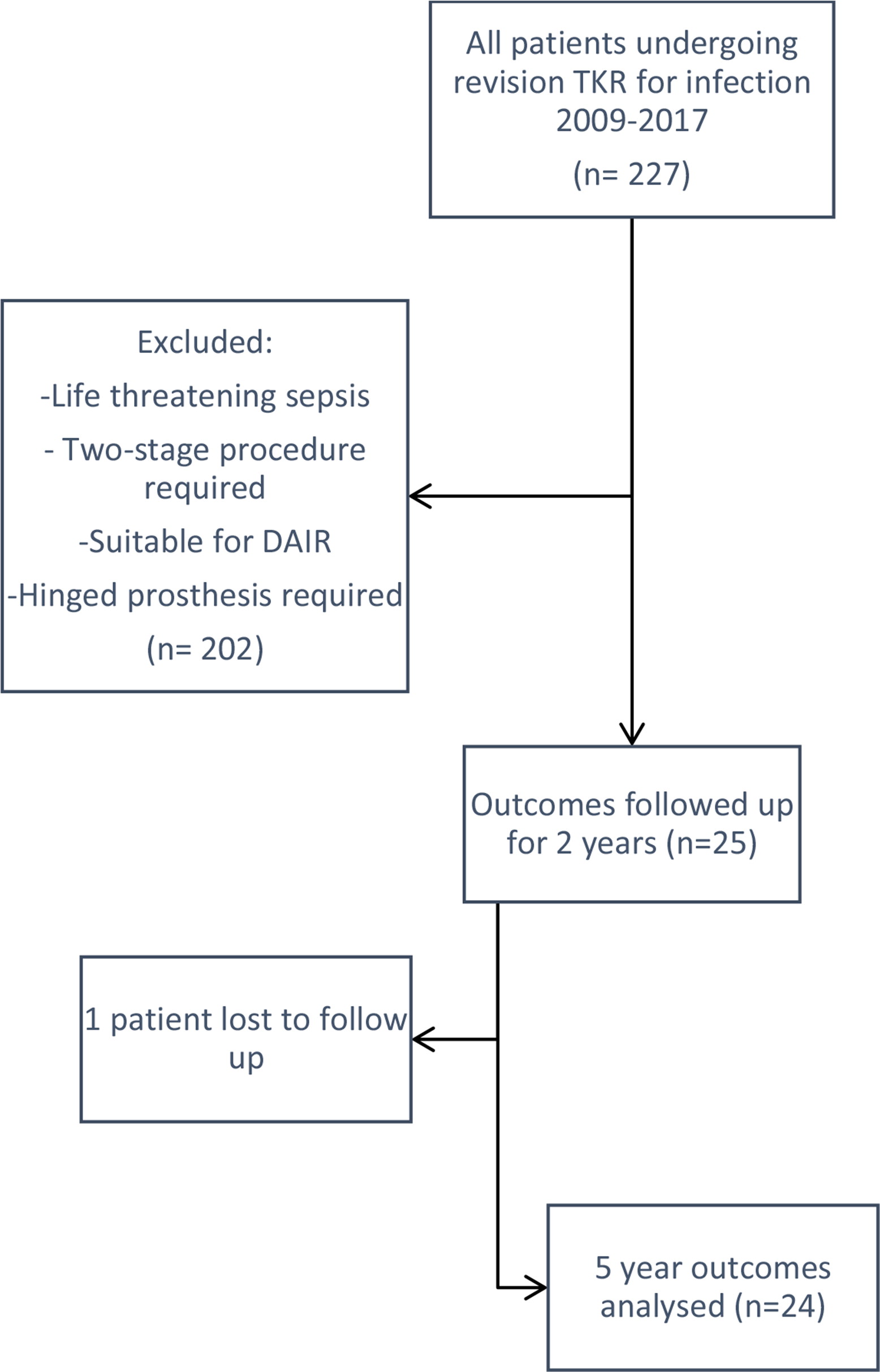
Fig. 1
Flowchart illustrating all patients initially meeting entry criteria to patients included in the final analysis. DAIR, debridement, antibiotics, and implant retention; TKR, total knee replacement.
This study group was composed of 12 males and 12 females (16 right knees and eight left knees revised), with a mean age of 72.7 years (standard deviation (SD) 7.6). Mean BMI was 33.3 kg/m2 (SD 5.7) and median ASA physical status grade was 2 (interquartile range 2 to 4). All primary arthroplasty procedures were performed between 1993 and 2016, and were all cemented TKAs. The mean time between primary surgery and revision was 3.0 years (10 months to 8.3 years). Six patients had actively discharging sinuses at the time of surgery. Five patients had failed previous revision procedures (two two-stage revisions and three DAIRs). Organisms were grown from deep tissue samples or joint aspirates in 20 patients. The mean duration of surgery was 143 minutes (94 to 286), and mean inpatient stay was 20 days (8 to 48). Stems were employed on either the femur or the tibia if the integrity of zone 2 was compromised by bone loss (Table I). Stems were used in 15 cases on the tibial side and eight on the femoral side.
Table I.
Preoperative Anderson Orthopaedic Research Institute grade of bone loss in femur and tibia.
| AORI Grade | Tibia | Femur |
|---|---|---|
| I | 0 | 2 |
| II | 18 | 17 |
| III | 6 | 5 |
-
AORI, Anderson Orthopaedic Research Institute.
Outcomes
There were two cases of recurrent infection. The first was treated with long-term antibiotic suppression therapy and remained systemically well at follow-up seven years after surgery. The second underwent successful DAIR procedure, and currently remains systemically well and off antibiotics at five-year follow-up. In the remaining cases, serum CRP returned to normal at a mean of 7.4 weeks (3 to 18). Overall reoperation rate was 5/24 (20.8%), with one secondary patella resurfacing, two superficial wound washouts, and one arthrotomy washout of an aseptic haematoma, in addition to the DAIR procedure above. Nine patients died, all from unrelated causes, and after completing five-year follow-up.
All patients recorded AKSS preoperatively, two years postoperatively, and five years postoperatively (Table II). Significant improvements (p < 0.001) in AKSS were seen, which remained at five-year follow-up (Table III).
Table II.
American Knee Society scores.
| American Knee Society Score | Mean (SD; SE) |
|---|---|
| Preoperative | 27.1 (10.2; 2.1) |
| Two-yr postoperative | 80.3 (14.8; 3) |
| Five-yr postoperative | 74.1 (19.8; 4) |
-
SD, standard deviation; SE, standard error of the mean.
Table III.
American Knee Society Score comparison.
| AKSS comparison | T | df | p-value* |
|---|---|---|---|
| Preoperative vs 2 yrs | -15.3 | 23 | < 0.001 |
| Preoperative vs 5 yrs | -10 | 23 | < 0.001 |
-
*
Paired t-test.
-
AKSS, American Knee Society Score.
OKS was recorded in all patients postoperatively at two and five years. Scores were organized into groups as described by Kalairajah et al,24 and are outlined in Table IV. Most patients fell into the “good” and “fair” outcome groups at both two and five years (a total of 23 and 17 patients, respectively).
Table IV.
Postoperative Oxford Knee Scores.
| Kalairajah Oxford Knee Score Classification | Patients, n | |
|---|---|---|
| 2 yrs | 5 yrs | |
| Poor (≤ 27) | 1 | 5 |
| Fair (28 to 33) | 4 | 5 |
| Good (34 to 41) | 19 | 12 |
| Excellent (42 to 48) | 0 | 2 |
Latest radiographs at a mean of 4.8 years postoperatively (1.0 to 10.0 years) show only one case of radiolucent lines (in one of the two recurrent infection cases). Additionally, only one other case showed evidence of stress protection or periosteal reaction. There were no cases of aseptic loosening or implant failure in this cohort of metaphyseal sleeves, which is comparable to the rate of revision in the noninfected cohort in our unit over the same period (2/202; 0.9%).
Discussion
This five-year follow-up study demonstrates the effectiveness of a two-in-one single-stage revision technique for infected TKA, with low rates of recurrent infection or aseptic failure. The selection criteria described allows the identification of appropriate patients for this technique, which performs similarly to the existing standard of care (two-stage revision), but with the benefits of a single hospital admission and procedure.
Patients with an actively discharging sinus were included in this study provided it could be excised and debrided, and all patients remained free from recurrence at most recent follow-up. This relief of disease burden was reported as a significant benefit by these patients. Similarly, the significant improvements in pain reflected in preoperative patient-reported outcome scores, compared with two years and remaining at five years, emphasizes the benefits of this intervention. Patients reported significant levels of pain preoperatively, and the mean duration from diagnosis of infection to single-stage revision was 26 months, due in part to patients who encountered failure in the initial two-stage procedure (n = 2) or DAIR procedure (n = 3).
As in all revision surgery, but particularly following significant periods of infection with tissue destruction and subsequent need for extensive debridement, surgeons may be faced with large areas of bone loss. This can pose a particular challenge: the balance of achieving adequate stability and constraint of the knee in the setting of frequently compromised soft-tissue stabilizers, while also providing adequate fixation of the implant to avoid early aseptic loosening. The use of metaphyseal sleeves, initially reported to be successful in hinged knee prostheses,25 has recently proved to be useful in treating tibial bone loss during revision surgery. These partially porous coated sleeves allow stable, cementless metaphyseal fixation, bypassing epiphyseal zone 1 where there is often bone loss following removal of the primary implant.14 This allows functional loading in zone 2, stimulating new bone deposition and the potential for filling in defects. The excellent biological fixation achieved by metaphyseal sleeves allows the ability to compensate for significant tibial defects, and therefore allows adequate and often extensive in the setting of revision surgery for infection.
In our series, metaphyseal sleeves were used in all patients on the tibial side, and all but two on the femur. At mean radiological follow-up of five years, there was no evidence of subsidence or loosening in any patients.
Although the relative rates of infection following TKA are low, the burden of infection is rising, as the volume of primary procedures performed each year continues to rise to meet the demands of an expanding ageing population.26,27 The current gold standard for infection of two-stage revision is effective but resource-intensive, and thus the debate regarding the indications and alternatives is ongoing.28 There is a growing body of evidence that single-stage revision is an acceptable alternative, with comparable functional outcomes and lower morbidity, mortality, and healthcare costs.29
To date there are no randomized controlled trials comparing two-stage revision with single-stage revision. Systematic reviews by Masters et al30 in 2013 and Chew et al8 in 2015 concluded that there was not enough evidence to address the adequacy of single-stage revision. More recently however, in 2019, Thakrar et al31 concluded from 22 articles that single-stage revision is an acceptable surgical treatment for PJI in selected patients (immunocompetent, without significant soft-tissue or bony compromise, or acute sepsis) with recurrence of infection ranging from 0% to 18% at a minimum of two years’ follow-up. This was echoed by Yaghmour et al,7 also in 2019, who reported good functional outcomes and low reinfection rates in their systematic review of 3,645 singe stage revisions.
Most evidence on this topic currently comprises case series and comparative studies. A propensity score-matched cohort study by Klemt et al32 in 2021 compared 44 patients undergoing single-stage revision TKA with 88 matched patients undergoing two-stage revision. Patients in the single-stage group reported improved PROMs, with similar rates of reinfection (25% single-stage to 27.2%) and 90-day readmission rates.
Selection criteria for single-stage revision remain controversial, with some advocating the need for well-identified causative pathogens.9,33,34 The European Bone and Joint Infection Society have recently proposed criteria for the definition of PJI, based on a combination of clinical findings, blood and synovial markers, microbiology, histology, and nuclear imaging. This allows stratification of patients into three groups (infection likely, unlikely, or confirmed) to guide treatment and facilitate research based upon a unified definition.35 Van den Kieboom et al36 recently compared the results of single-stage revision with two-stage revision in chronic culture-negative PJI. Their comparison of 105 patients (30 single-stage, 75 two-stage) at minimum one-year follow-up revealed similar outcomes in both groups in terms of reinfection, re-revision, and readmission.
Our results show comparable outcomes in terms of patient satisfaction, recurrence of infection, and reintervention rate, compared to the existing literature, demonstrating the safety and efficacy of this two-in-one single-stage technique.17,37 Strengths of the study include prospective collection of data with PROMs and radiological follow-up to five years. The conclusions of this study are limited by the small sample size of 24 patients, dictated by the number of cases in our department over the period of study, and the lack of control group undergoing two-stage revision for comparison.
In summary, this study demonstrates that the use of a single-stage approach for revision of infected TKA, with metaphyseal sleeves to address any bone loss, provides good fixation and implant survivorship at medium-term follow-up. The patient-reported outcomes show a significant and sustained improvement from the preoperative scores. The results of the study are comparable to those reported in the literature and demonstrate the efficacy of using a two-in-one single-stage revision TKA in the context of infection.
References
1. Blom AW , Brown J , Taylor AH , Pattison G , Whitehouse S , Bannister GC . Infection after total knee arthroplasty . J Bone Joint Surg Br . 2004 ; 86-B ( 5 ): 688 – 691 . Google Scholar
2. Kallala RF , Vanhegan IS , Ibrahim MS , Sarmah S , Haddad FS . Financial analysis of revision knee surgery based on NHS tariffs and hospital costs: does it pay to provide a revision service? Bone Joint J . 2015 ; 97-B ( 2 ): 197 – 201 . Crossref PubMed Google Scholar
3. No authors listed . Knees - All Procedures - Activity . National Joint Registry . 2021 . https://reports.njrcentre.org.uk/knees-all-procedures-activity ( date last accessed 12 January 2022 ). Google Scholar
4. No authors listed . Scottish Arthroplasty Project Annual Report 2020 . The Scottish Arthroplasty Project . 2021 . https://www.arthro.scot.nhs.uk/Reports/Main.html ( date last accessed 12 January 2022 ). Google Scholar
5. Postler A , Lützner C , Beyer F , Tille E , Lützner J . Analysis of total knee arthroplasty revision causes . BMC Musculoskelet Disord . 2018 ; 19 ( 1 ): 55 . Crossref PubMed Google Scholar
6. Insall JN , Thompson FM , Brause BD . Two-stage reimplantation for the salvage of infected total knee arthroplasty . J Bone Joint Surg Am . 1983 ; 65 ( 8 ): 1087 – 1098 . Crossref PubMed Google Scholar
7. Yaghmour KM , Chisari E , Khan WS . Single-stage revision surgery in infected total knee arthroplasty: a PRISMA systematic review . J Clin Med . 2019 ; 8 ( 2 ): E174 . Crossref PubMed Google Scholar
8. Chew E , Khan WS , Agarwal S , Morgan-Jones R . Single stage knee arthroplasty revision surgery: a systematic review of the literature . Open Orthop J . 2015 ; 9 : 504 – 510 . Crossref PubMed Google Scholar
9. Pangaud C , Ollivier M , Argenson JN . Outcome of single-stage versus two-stage exchange for revision knee arthroplasty for chronic periprosthetic infection . EFORT Open Rev . 2019 ; 4 ( 8 ): 495 – 502 . Crossref PubMed Google Scholar
10. Holland G , Brown G , Goudie S , Brenkel I , Walmsley PJ . Results of using a “2-in-1” single-stage revision total knee arthroplasty for infection with associated bone loss: prospective two-year follow-up . J Knee Surg . 2021 ; 34 ( 5 ): 526 – 532 . Google Scholar
11. Engh GA , Ammen DJ . Bone loss with revision total knee arthroplasty: defect classification and alternatives for reconstruction . Instr Course Lect . 1995 ; 48 : 167 – 175 . PubMed Google Scholar
12. Engh GA , Ammeen DJ . Classification and preoperative radiographic evaluation: knee . Orthop Clin North Am . 1998 ; 29 ( 2 ): 205 – 217 . Crossref PubMed Google Scholar
13. Panegrossi G , Ceretti M , Papalia M , Casella F , Favetti F , Falez F . Bone loss management in total knee revision surgery . Int Orthop . 2014 ; 38 ( 2 ): 419 – 427 . Crossref PubMed Google Scholar
14. Morgan-Jones R , Oussedik SIS , Graichen H , Haddad FS . Zonal fixation in revision total knee arthroplasty . Bone Joint J . 2015 ; 97-B ( 2 ): 147 – 149 . Crossref PubMed Google Scholar
15. Agarwal S , Azam A , Morgan-Jones R . Metal metaphyseal sleeves in revision total knee replacement . Bone Joint J . 2013 ; 95-B ( 12 ): 1640 – 1644 . Crossref PubMed Google Scholar
16. Dalury DF , Barrett WP . The use of metaphyseal sleeves in revision total knee arthroplasty . Knee . 2016 ; 23 ( 3 ): 545 – 548 . Google Scholar
17. Klim SM , Amerstorfer F , Bernhardt GA , et al. Septic revision total knee arthroplasty: treatment of metaphyseal bone defects using metaphyseal sleeves . J Arthroplasty . 2018 ; 33 ( 12 ): 3734 – 3738 . Crossref PubMed Google Scholar
18. Bonanzinga T , Akkawi I , Zahar A , Gehrke T , Haasper C , Marcacci M . Are metaphyseal sleeves a viable option to treat bone defect during revision total knee arthroplasty? A systematic review . Joints . 2019 ; 7 ( 1 ): 19 – 24 . Crossref PubMed Google Scholar
19. Matar HE , Bloch BV , James PJ . Role of metaphyseal sleeves in revision total knee arthroplasty: Rationale, indications and long-term outcomes . J Orthop . 2021 ; 23 : 107 – 112 . Crossref PubMed Google Scholar
20. Insall JN , Dorr LD , Scott RD , Scott WN . Rationale of the Knee Society clinical rating system . Clin Orthop Relat Res . 1989 ; 248 : 13 – 14 . PubMed Google Scholar
21. Dawson J , Fitzpatrick R , Murray D , Carr A . Questionnaire on the perceptions of patients about total knee replacement . J Bone Joint Surg Br . 1998 ; 80-B ( 1 ): 63 – 69 . Crossref PubMed Google Scholar
22. Murray DW , Fitzpatrick R , Rogers K , et al. The use of the Oxford hip and knee scores . J Bone Joint Surg Br . 2007 ; 89-B ( 8 ): 1010 – 1014 . Google Scholar
23. Saklad M . Grading of patients for surgical procedures . Anesthesiol . 1941 ; 2 ( 3 ): 281 – 284 . Google Scholar
24. Kalairajah Y , Azurza K , Hulme C , Molloy S , Drabu KJ . Health outcome measures in the evaluation of total hip arthroplasties--a comparison between the Harris hip score and the Oxford hip score . J Arthroplasty . 2005 ; 20 ( 8 ): 1037 – 1041 . Crossref PubMed Google Scholar
25. Jones RE , Barrack RL , Skedros J . Modular, mobile-bearing hinge total knee arthroplasty . Clin Orthop Relat Res . 2001 ; 392 ( 392 ): 306 – 314 . Crossref PubMed Google Scholar
26. Kurtz S , Ong K , Lau E , Mowat F , Halpern M . Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030 . J Bone Joint Surg Am . 2007 ; 89-A ( 4 ): 780 – 785 . Crossref PubMed Google Scholar
27. Springer BD , Cahue S , Etkin CD , Lewallen DG , McGrory BJ . Infection burden in total hip and knee arthroplasties: an international registry-based perspective . Arthroplast Today . 2017 ; 3 ( 2 ): 137 – 140 . Crossref PubMed Google Scholar
28. George DA , Konan S , Haddad FS . Single-stage hip and knee exchange for periprosthetic joint infection . J Arthroplasty . 2015 ; 30 ( 12 ): 2264 – 2270 . Crossref PubMed Google Scholar
29. Negus JJ , Gifford PB , Haddad FS . Single-stage revision arthroplasty for infection-an underutilized treatment strategy . J Arthroplasty . 2017 ; 32 ( 7 ): 2051 – 2055 . Crossref PubMed Google Scholar
30. Masters JPM , Smith NA , Foguet P , Reed M , Parsons H , Sprowson AP . A systematic review of the evidence for single stage and two stage revision of infected knee replacement . BMC Musculoskelet Disord . 2013 ; 14 ( 1 ): 222 . Crossref PubMed Google Scholar
31. Thakrar RR , Horriat S , Kayani B , Haddad FS . Indications for a single-stage exchange arthroplasty for chronic prosthetic joint infection . Bone Joint J . 2019 ; 101-B ( 1_Supple_A ): 19 – 24 . Crossref PubMed Google Scholar
32. Klemt C , Tirumala V , Oganesyan R , Xiong L , van den Kieboom J , Kwon Y-M . Single-Stage Revision of the Infected Total Knee Arthroplasty Is Associated With Improved Functional Outcomes: A Propensity Score-Matched Cohort Study . J Arthroplasty . 2021 ; 36 ( 1 ): 298 – 304 . Crossref PubMed Google Scholar
33. Vanhegan IS , Morgan-Jones R , Barrett DS , Haddad FS . Developing a strategy to treat established infection in total knee replacement: a review of the latest evidence and clinical practice . J Bone Joint Surg Br . 2012 ; 94-B ( 7 ): 875 – 881 . Crossref PubMed Google Scholar
34. Kalore NV , Gioe TJ , Singh JA . Diagnosis and management of infected total knee arthroplasty . Open Orthop J . 2011 ; 5 : 86 – 91 . Crossref PubMed Google Scholar
35. McNally M , Sousa R , Wouthuyzen-Bakker M , et al. The EBJIS definition of periprosthetic joint infection . Bone Joint J . 2021 ; 103-B ( 1 ): 18 – 25 . Crossref PubMed Google Scholar
36. van den Kieboom J , Tirumala V , Box H , Oganesyan R , Klemt C , Kwon Y-M . One-stage revision is as effective as two-stage revision for chronic culture-negative periprosthetic joint infection after total hip and knee arthroplasty . Bone Joint J . 2021 ; 103-B ( 3 ): 515 – 521 . Crossref PubMed Google Scholar
37. Parkinson RW , Kay PR , Rawal A . A case for one-stage revision in infected total knee arthroplasty? Knee . 2011 ; 18 ( 1 ): 1 – 4 . Crossref PubMed Google Scholar
Author contributions
A. C. C. Brunt: Formal analysis, Writing – original draft, Writing – review & editing.
M. Gillespie: Formal analysis, Writing – original draft, Writing – review & editing.
G. Holland: Formal analysis, Writing – review & editing.
I. Brenkel: Conceptualization, Data curation, Validation, Writing – review & editing.
P. Walmsley: Supervision, Project administration, Conceptualization, Data curation, Validation, Writing – review & editing.
Funding statement
The author(s) received no financial or material support for the research, authorship, and/or publication of this article
Acknowledgements
We would like to thank our team of four arthroplasty nurse practitioners who asssit with the data collection from patients both pre and post-operatively. Also, we are grateful for the multi-disciplinary support from the microbiology team led by Dr Keith Morris and Dr David Griffiths.
Ethical review statement
This study protocol was reviewed and approved by the local regional ethics committee.
Open access funding
The publishing costs were funded by support from St Andrews University Open Access Fund.
Follow G. Holland @GeorgeDBHolland
Follow P. Walmsley @PhilWalmsley4
© 2022 Author(s) et al. This is an open-access article distributed under the terms of the Creative Commons Attribution Non-Commercial No Derivatives (CC BY-NC-ND 4.0) licence, which permits the copying and redistribution of the work only, and provided the original author and source are credited. See https://creativecommons.org/licenses/by-nc-nd/4.0/.









