Abstract
Aims
Simultaneous bilateral total knee arthroplasty (TKA) has been used due to its financial advantages, overall resource usage, and convenience for the patient. The training model where a trainee performs the first TKA, followed by the trainer surgeon performing the second TKA, is a unique model to our institution. This study aims to analyze the functional and clinical outcomes of bilateral simultaneous TKA when performed by a trainee or a supervising surgeon, and also to assess these outcomes based on which side was done by the trainee or by the surgeon.
Methods
This was a retrospective cohort study of all simultaneous bilateral TKAs performed by a single surgeon in an academic institution between May 2003 and November 2017. Exclusion criteria were the use of partial knee arthroplasty procedures, staged bilateral procedures, and procedures not performed by the senior author on one side and the trainee on another. Primary clinical outcomes of interest included revision and re-revision. Primary functional outcomes included the Oxford Knee Score (OKS) and patient satisfaction scores.
Results
In total, 315 patients (630 knees) were included for analysis. Of these, functional scores were available for 189 patients (378 knees). There was a 1.9% (n = 12) all-cause revision rate for all knees. Overall, 12 knees in ten patients were revised, and both right and left knees were revised in two patients. The OKS and patient satisfaction scores were comparable for trainees and supervising surgeons. A majority of patients (88%, n = 166) were either highly likely (67%, n = 127) or likely (21%, n = 39) to recommend bilateral TKAs to a friend.
Conclusion
Simultaneous bilateral TKA can be used as an effective teaching model for trainees without any significant impact on patient clinical or functional outcomes. Excellent functional and clinical outcomes in both knees, regardless of whether the performing surgeon is a trainee or supervising surgeon, can be achieved with simultaneous bilateral TKA.
Cite this article: Bone Jt Open 2022;3(1):29–34.
Take home message
Simultaneous bilateral total knee arthroplasty (TKA) can be used as an effective teaching model for trainees without any significant impact on patient clinical or functional outcomes.
Excellent functional and clinical outcomes in both knees, regardless of whether the performing surgeon is a trainee or supervising surgeon, can be achieved with simultaneous bilateral TKA.
Introduction
Simultaneous bilateral total knee arthroplasty (TKA) has been widely used due to financial advantages and overall resource usage in terms of time spent in the operating room.1 The benefits of undergoing a single period of rehabilitation for both knees, as opposed to staged procedures requiring two periods of rehabilitation, are significant for the patient while also reducing absence from work, recreation, and social functions. Bilateral simultaneous TKA is known to induce a greater physiological insult when compared to staged procedures in the acute setting; Liu et al2 demonstrated, in their meta-analysis of 73,617 simultaneous bilateral TKA, that there is a significantly higher risk of mortality, pulmonary embolism (PE), and all complications when compared to staged procedures, although the differences were small.
Historically, the risk of death secondary to cardiac events has been the main concern for simultaneous procedures and these findings have highlighted the importance of appropriate patient selection when considering simultaneous bilateral TKA.3,4 The question of whether staged or simultaneous procedures are more appropriate became an area of controversy for some time.5 However, more recently, there is emerging evidence to indicate that significantly higher rates of cardiac, respiratory, urinary, PE, and deep vein thrombosis (DVT) complications occur after the second staged TKA has been performed when compared to after the first single TKA.6 This supports a move back to simultaneous bilateral TKA. In a study by Tsay et al,7 the absolute clinical difference in complication rates between staged and simultaneous bilateral TKA was shown to be minimal (< 1%) when analyzing over 70,000 knees that were operated on bilaterally (either staged or simultaneous).
In keeping with current trends, our institution supports the use of simultaneous bilateral TKA as an enduring practice, with the senior surgeon (BAM) having performed simultaneous bilateral knee arthroplasties for the past 26 years. The training model where a trainee performs the first TKA followed by the trainer surgeon performing the second TKA is unique to our institution, and allows the trainee to be exposed to a TKA from skin incision to skin closure. Supervision by the senior surgeon is available until skin closure, and while the trainee is closing the first side, the surgeon completes the second sidee. The purpose of this method is to maximize operating room efficiency. This unique training model allows us to assess whether there are any differences in the clinical or functional outcomes of TKAs performed by trainees and their supervising surgeons.
The purpose of this study is to analyze the functional and clinical outcomes of bilateral simultaneous TKA when performed by a trainee or supervising surgeon. The main research hypothesis is that that there is no difference in outcome regardless of whether the knee arthroplasty is done by the surgeon or the trainee, while using the bilateral knee arthroplasty model as a means to control for all patient-related variables that are otherwise difficult to control for in a single-sided TKA model.
Methods
This was a retrospective cohort study of all simultaneous bilateral TKAs performed by a single surgeon in an academic institution between May 2003 and November 2017. All patients received the NexGen LPS-Flex (Zimmer, USA) total knee prosthesis. Inclusion criteria were all bilateral TKAs performed for osteoarthritis (OA) between May 2003 and November 2017 with a minimum of four years’ follow-up. Exclusion criteria were the use of partial knee arthroplasty procedures, staged bilateral procedures, and procedures where both sides were operated on by the same person (for example, both by a trainee or by the surgeon). Institutional Review Board approval was granted prior to commencing this study.
Surgical technique
Patients underwent bilateral procedures through the medial parapatellar approach with the use of a tourniquet, unless there was a contraindication to the use of a tourniquet such as peripheral vascular disease. All implants were inserted using a gap-balancing technique to achieve a neutral mechanical alignment. Initially, once the distal femoral cut and proximal tibial cut were made, the extension gap was assessed using a block of equal thickness to the polyethylene liner to be inserted. Any coronal imbalance was corrected using careful sequential soft-tissue release depending on whether the gap was tighter on the medial or lateral side. The flexion gap was also assessed once the posterior femoral condylar resections were performed. Again, any imbalance was corrected for using careful soft-tissue release. The training model in this institution is such that a trainee would typically perform the first TKA on the right knee under the supervision of the senior author. This would then be followed by the left TKA, performed by the senior author. In a small number of cases (n = 19), the right TKA was performed by the senior author and the left knee by the trainee. This occurred early in the development of the training model before the senior author decided on the final training design as described, although the first side was always done by the trainee regardless of which right side was done first. The side that was done by the trainee was recorded for all cases.
Data collection
Demographic-dependent variables recorded included age, sex, diagnosis, BMI, and American Society of Anesthesiologists (ASA) score. Other variables recorded included surgeon grade (trainee or attending) and tourniquet time (minutes).
Outcomes
Primary clinical outcomes of interest included all secondary procedures, including revision, re-revision, and the indication for all revision procedures were recorded. This also included the need for manipulation under anaesthesia in all cases.
Primary functional outcomes included the Oxford Knee Score (OKS)8,9 at most recent clinical review.10 In order to differentiate between the functional outcomes of both knees in the same patient, we asked each patient to complete a separate OKS for each knee. Patient satisfaction scores were recorded under the headings of function, pain, recreation, and results.11 A custom patient questionnaire was distributed to all patients asking two questions. The first question read ‘Which knee do you prefer?’ with possible answers including ‘left’, ‘right’, or ‘no preference’. We adjusted the analysis of these answers to determine whether the patient preferred the surgeon or the trainee knee. The second question read, ‘How likely are you to recommend that both knee arthroplasties be done at the same time as opposed to one at a time to a friend?’ with possible answers including ‘highly likely’, ‘likely’, ‘neutral’, ‘unlikely’, or ‘highly unlikely’.
Demographic data
In total, 315 patients (613 knees) with bilateral simultaneous TKAs performed between May 2003 and November 2017 were included for analysis. Of these, functional scores were available for 189 patients (378 knees). All functional scores were current (reported in 2020) with a minimum of two years’ follow-up for each knee. Mean age of the cohort was 63.7 years (standard deviation (SD) 9.2, 40 to 84). There was a preponderance of females at 53% (n = 167) compared to 47% males (n = 148). The mean BMI was 31.7 kg/m2 (SD 5.8, 17.6 to 55.2) and the ASA distribution was 9.5% grade 1 (n = 30), 71.7% grade 2 (n = 226), 18.1% grade 3 (n = 57), and 0.6% grade 4 (n = 2). At the time of review, 23 patients were deceased, but none within the first year after surgery. All procedures were performed for the indication of OA. The tourniquet time was comparable between the supervising surgeon (mean 31.1 minutes( SD 9.4; 95% confidence interval (CI) 30.0 to 32.3)) and the trainee (mean 31.4 minutes (SD 9.5; 95% CI 30.2 to 32.6)) (p = 0.736, two-samples Mann-Whitney U test).
Statistical analysis
Descriptive statistics were used to capture demographic data, with interval variables being expressed as mean values with standard deviations (SDs) and ranges or 95% CIs. The OKS was expressed using median values with interquartile ranges (IQRs), consistent with box plot representation. Percentages were used to represent categorical demographic variables.
The relationship between two categorical variables was analyzed using the chi-squared test provided there were more than five subjects in each group. Otherwise, Fisher’s exact test was used for these analyses. Interval functional outcomes were not normally distributed based on the Shapiro-Wilk test for normal data distribution (p < 0.05). To determine the impact of categorical independent variables on interval dependent variables, the two-sample Mann-Whitney U test was used. A p-value of 0.05 was taken to be statistically significant, and the statistical software used was Stata/IC 13.1 for Mac (64-bit Intel; StataCorp, USA).
Box plots were used to illustrate differences in functional scores between groups. The midline in the box plot represents the median value with the box height representing 25% to 75% of the dataset (second and third quartiles). The whiskers extended out to the upper and lower extremes of the datasets. If there were any outliers in the datasets, these were illustrated as single dots/data points. Mean values for function, pain, recreation, and results scores were illustrated using histograms.
Results
Revision
There was a 1.9% (n = 12) all-cause revision rate for all knees. In total, 12 knees in ten patients were recorded, and both right and left knees were revised in two patients. The indications for revision surgery are summarized in Table I. The mean time to revision was 1,179 days (σ 1,039; 13 to 2,878). There were six revisions of left knees and six revisions of right knees (p = 1.000, chi-squared test) and six revisions of knees were performed by the trainee and six were performed by the trainer (p = 1.000, chi-squared test). Listed in the indications for revision were two broken tibial posts related to the use of highly cross-linked polyethylene, which had been previously published.12
Table I.
Indications for revision.
| # | Side | Surgeon grade | Indication and details | Time to revision, days |
|---|---|---|---|---|
| 1 | Left | Trainer | Deep infection – underwent DAIR procedure | 13 |
| 2 | Left | Trainee | Broken tibial baseplate – revised components | 1,133 |
| 3 | Left | Trainer | Patellar instability in a patient with Parkinson’s disease – revised to a hinged prosthesis | 1,047 |
| 4* | Left | Trainer | Aseptic loosening of tibial component – revised components | 862 |
| 5 | Left | Trainer | Aseptic loosening of tibial component – revised components | 2,471 |
| 6* | Left | Trainer | Broken tibial post – revised liner | 2,878 |
| 7 | Right | Trainer | Deep infection – underwent DAIR procedure | 32 |
| 8 | Right | Trainee | Deep infection – underwent DAIR procedure | 44 |
| 9 | Right | Trainee | Aseptic loosening of tibial component – revised components | 1,210 |
| 10* | Right | Trainee | Broken tibial post – revised liner | 2,211 |
| 11* | Right | Trainee | Aseptic loosening of tibial component – revised components | 862 |
| 12† | Right | Trainee | Deep infection – underwent DAIR procedure | 39 |
-
*
Bilateral knees revised.
-
†
Required re-revision.
-
DAIR, debridement, antibiotics, and implant retention (with polyethylene liner exchange).
Re-revision
Re-revision for infection was performed for one knee only. This patient underwent a single-stage revision consisting of debridement, antibiotics, and implant retention (DAIR) at 39 days after the index procedure. Infection was not eradicated after the DAIR procedure in this case so a subsequent two-stage re-revision was performed at 59 days post index procedure. At recent review, four years after the index procedure, infection was completely eradicated in this patient.
Manipulation under anaesthesia
In total, 12 knees were manipulated under anaesthesia due to stiffness secondary to arthrofibrosis. Seven were originally performed by trainees compared to five trainer knees requiring MUA (p = 0.560, chi-squared test).
Functional scores
The median normalized OKS in the trainee knees was 93.75% (IQR 81.2% to 97.9%) compared to 90.6% (IQR 79.1% to 97.9%) in the trainer knees (p = 0.860) (Figure 1). We normalized the OKS out of 100, due to the change in scoring from a maximum of 60 to a maximum of 48 during the data collection for the study.
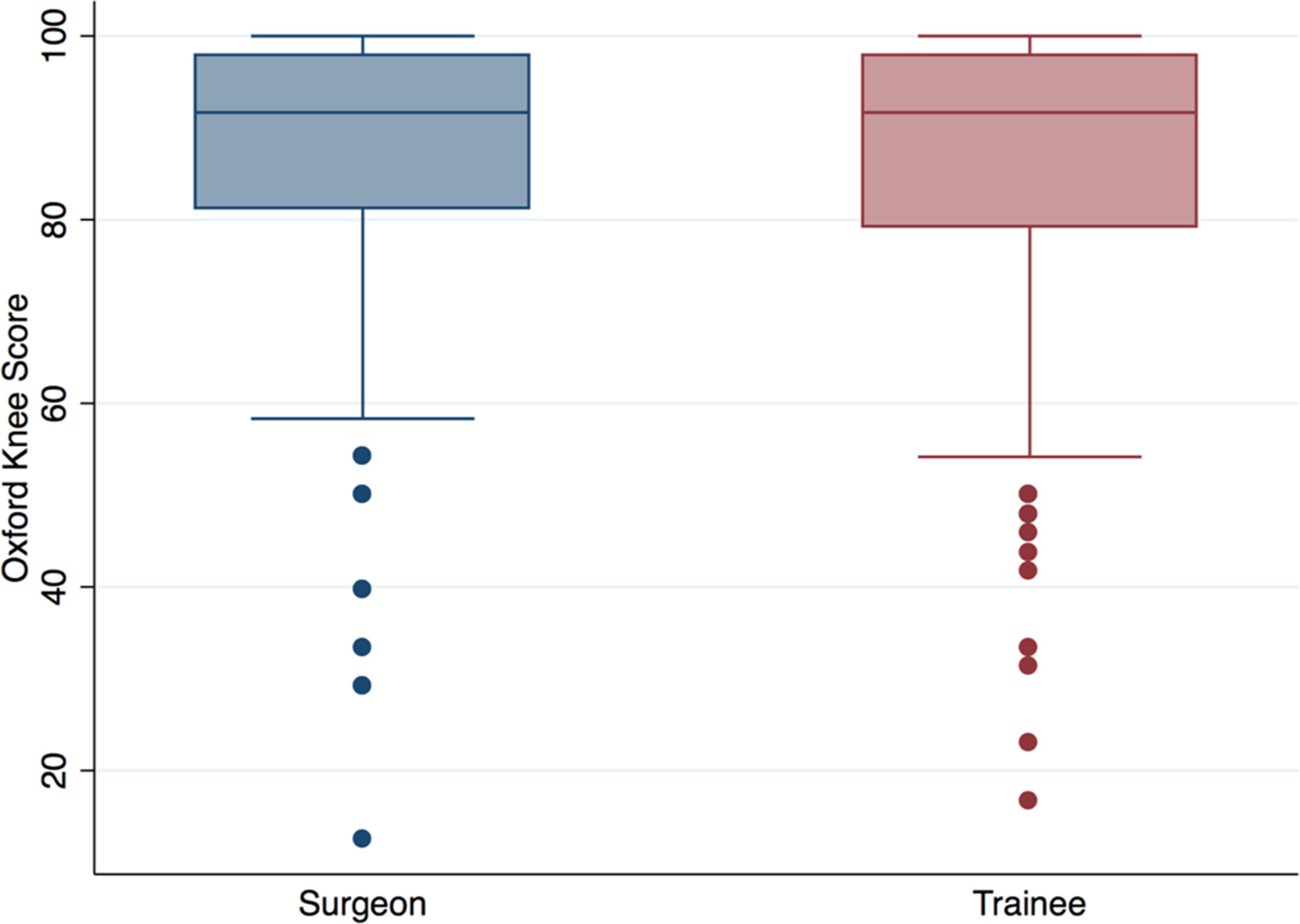
Fig. 1
Oxford Knee Scores for trainer and trainees.
The mean values comparing trainer and trainee knees for the patient satisfaction score under the headings of Function (p = 0.309), Pain (p = 0.746), Recreation (p = 0.740), and Results (p = 0.937, all two-samples Mann-Whitney U test) are illustrated in the histogram shown in Figure 2.
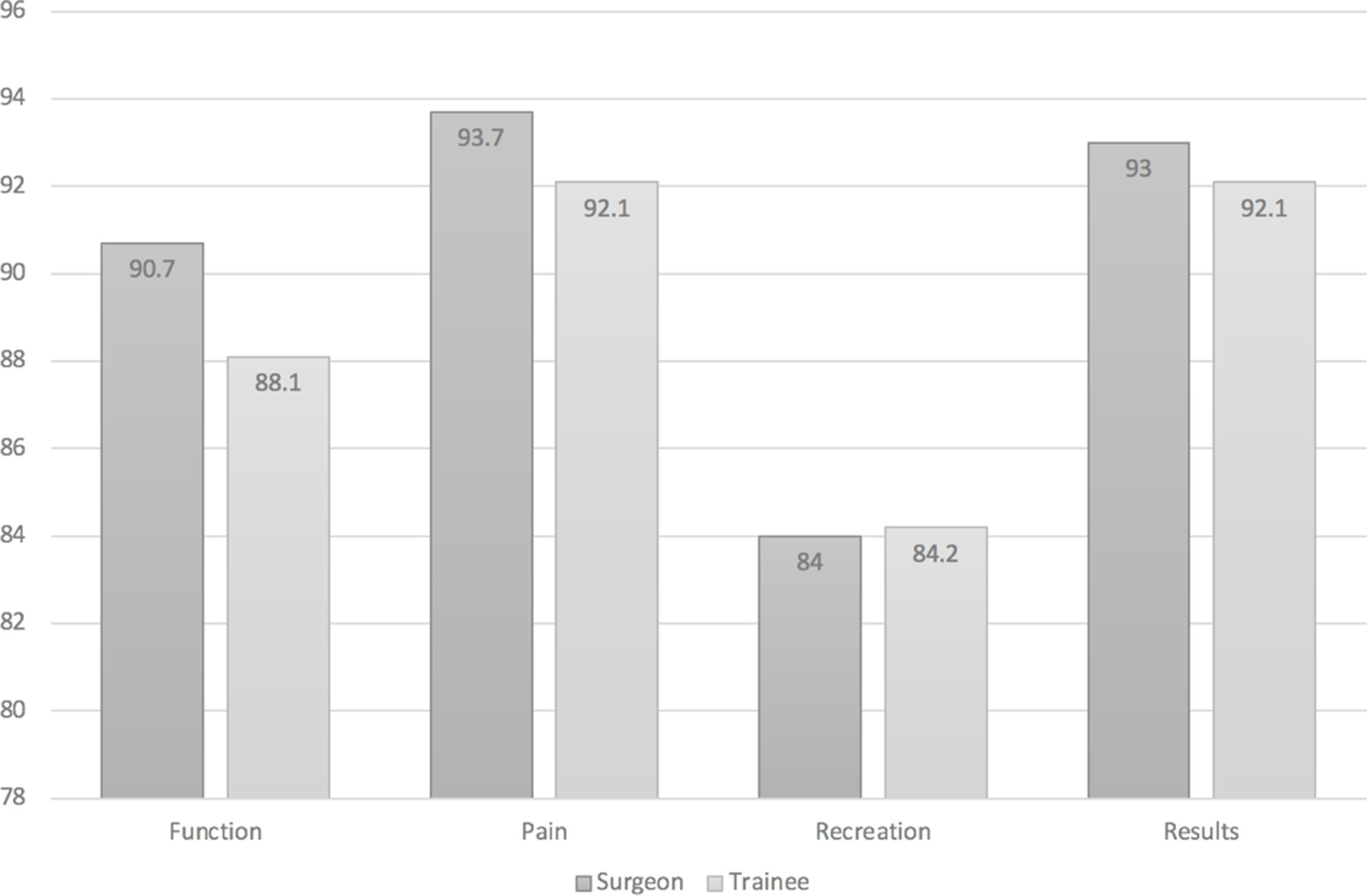
Fig. 2
Patient satisfaction scores comparing trainer and trainees.
Patient questionnaires
Our results showed that 23 (11%) patients preferred the side done by the surgeon, whereas 33 (15%) patients preferred the side done by the trainee (p = 0.152, chi-squared test). The remainder of patients (n = 161, 74%) reported no preference between the two sides.
When asked, ‘How likely are you to recommend that both knee arthroplasties be done at the same time as opposed to one at a time to a friend?’, it was reported that 88% of patients (n = 166) were either highly likely (67%, n = 127) or likely (21%, n = 40) to recommend bilateral TKAs to a friend. The answers were ‘neutral’ in 6% (n = 11), ‘unlikely’ in 2% (n = 4) and ‘highly unlikely’ in 4% (n = 8) of patients.
Discussion
The impact of trainees performing procedures such as unilateral TKA has been investigated widely, with the general consensus confirming that trainees can achieve similar outcomes to trainer surgeons. Similar long-term clinical outcomes at ten years between trainee and trainer TKAs have been reported by Faulkner et al.13 A recent study investigating the impact of surgeon volume and training status on TKA alignment also showed that trainees can perform similarly to their supervising trainer counterparts.14 However, it is possible that easier cases were delegated to trainees while more difficult cases were done by the surgeon, as these were unilateral cases. Our study attempts to remove the potential patient-related variables that may affect the difficulty of surgery, by using a bilateral knee arthroplasty model where many of these variables are not applicable as it is the same patient.
Very little information is known, however, about the impact that surgeon grade can have on the clinical and functional outcomes of two knees undergoing simultaneous bilateral TKAs. Goto et al15 analyzed 38 knees and confirmed similar outcomes for trainees and their supervisors where one side was performed by the trainee and the other performed by the supervisor, but in comparison to our study, the numbers are small; this motivated this current study, with much higher numbers, leading to a more robust analysis. We therefore report a sample size of 630 knees that far exceeds that study and so contributes significant weight to the debate.
In our study, we report no difference between trainee and trainer TKAs for clinical outcomes including all-cause revision (p = 1.000) or the need for MUA (p = 0.56), with patient-related variables being controlled for by virtue of the fact that the trainee and trainer operated on different knees in the same patient, at the same time.
The Knee Society Score was comparable for both knees in the study reported by Goto et al.15 We report similar findings for the Oxford Knee Score with no significant difference in the mean OKS when comparing trainee to trainer performed knees (p = 0.86). Huang et al16 demonstrated a higher rate of satisfaction with the second knee (left side) performed in a simultaneous sitting for bilateral TKA. They analyzed 46 patients, compared to 315 patients in this current study, where we demonstrated no difference between either knee.
In our study, we are unable to comment on the difference based on laterality or sequence done because the first knee was almost always the right knee, which was done by the trainee. Therefore, the only independent variable in our study is whether the surgery was done by the trainee or by the trainer. Depsite this, there was still no difference between right and left knees in terms or failure rate, clinical outcome, or satisfaction. Other variables recorded in the current study included tourniquet times which were similar for both trainer (mean 29 minutes) and trainee (mean 30 minutes) TKAs (p = 0.736). This is important to note because under appropriate supervision, allowing the trainee to perform a TKA does not slow down the pace of surgery. This mirrors an analysis of over 6,000 TKAs reported by Khanuja et al,17 which demonstrated similar findings with no difference between operating times based on the surgeons’ level of experience, but in a unilateral TKA model.
The second part of the study was to test our belief that patients are better served by simultaneous bilateral TKA instead of staged bilateral TKA. It is noteworthy that there was no mortality within the first year of surgery in our group. The patient questionnaire results were supportive of the continued use of simultaneous bilateral TKA, as 89% (n = 168) of patients felt they were either ‘highly likely’ or ‘likely’ to recommend the procedure to a friend. Only 6% (n = 11) of patients were either ‘unlikely’ or ‘highly unlikely’ to recommend the procedure to a friend. Patient satisfaction scores were also noted to be comparable across all headings including function, pain, recreation and results.
In summary, while the outcomes reported in this study have been reported in other unilateral TKA models, one cannot be certain that those cases performed by trainees were not cherry-picked for simplicity, with the surgeon performing the more complex cases. The strength of the current study is that the patient has been eliminated as a variable, which confirms that the previously reported similarity in functional and clinical outcomes between trainers and trainees still applies when a bilateral TKA model is applied. Furthermore, another strength of this study is that it demonstrates that patients are happy with their choice of bilateral simultaneous surgery, which has not been demonstrated in previous studies, and supports our hypothesis that patients are not being disadvantanged, at least from their point of view, with the recommendation of simultaneous bilateral surgery.
This was a retrospective study with all the associated limitations of such a design. Clinical follow-up ranged from four to 17 years, and so further revision cases may present themselves in the future. A minimum of two years for functional outcomes is appropriate and likely to accurately reflect the true new baseline functional outcome of this cohort of patients. Functional outcome scores were only available for 189 patients, as not all returned the questionnaire to our institution; we did not perform a radiological analysis, and 23 patients were deceased at the time of review.
In conclusion, simultaneous bilateral TKA can be used as an effective teaching model for trainees without any significant impact on patient clinical or functional outcomes. Excellent functional and clinical outcomes in both knees, regardless of whether the performing surgeon is a trainee or supervising surgeon, can be achieved with simultaneous bilateral TKA.
References
1. Alghadir AH , Iqbal ZA , Anwer S , Anwar D . Comparison of simultaneous bilateral versus unilateral total knee replacement on pain levels and functional recovery . BMC Musculoskelet Disord . 2020 ; 21 ( 1 ): 246 . Crossref PubMed Google Scholar
2. Liu L , Liu H , Zhang H , Song J , Zhang L . Bilateral total knee arthroplasty: Simultaneous or staged? A systematic review and meta-analysis . Medicine (Baltimore) . 2019 ; 98 ( 22 ): e15931 . Google Scholar
3. Oakes DA , Hanssen AD . Bilateral total knee replacement using the same anesthetic is not justified by assessment of the risks . Clin Orthop Relat Res . 2004 ; 428 : 87 – 91 . Google Scholar
4. Gurunathan U . Perioperative considerations of bilateral total knee replacement: a review . J Clin Anesth . 2013 ; 25 ( 3 ): 232 – 239 . Crossref PubMed Google Scholar
5. Noble J , Goodall JR , Noble DJ . Simultaneous bilateral total knee replacement: a persistent controversy . Knee . 2009 ; 16 ( 6 ): 420 – 426 . Crossref PubMed Google Scholar
6. Grace TR , Tsay EL , Roberts HJ , Vail TP , Ward DT . Staged bilateral total knee arthroplasty: increased risk of recurring complications . J Bone Joint Surg Am . 2020 ; 102-A ( 4 ): 292 – 297 . Crossref PubMed Google Scholar
7. Tsay EL , Grace TR , Vail T , Ward D . Bilateral simultaneous vs staged total knee arthroplasty: minimal difference in perioperative risks . J Arthroplasty . 2019 ; 34 ( 12 ): 2944 – 2949 . Crossref PubMed Google Scholar
8. Dawson J , Fitzpatrick R , Murray D , Carr A . Questionnaire on the perceptions of patients about total knee replacement . J Bone Joint Surg Br . 1998 ; 1 : 63 – 69 . Crossref PubMed Google Scholar
9. Murray DW , Fitzpatrick R , Rogers K , et al. The use of the Oxford hip and knee scores . J Bone Joint Surg Br . 2007 ; 8 : 1010 – 1014 . Google Scholar
10. Levy Y , Azar M , Raffaelli A , et al. One-session bilateral total knee replacement: late complications and survivorship . Orthop Traumatol Surg Res . 2020 ; 106 ( 5 ): 903 – 906 . Crossref PubMed Google Scholar
11. Solomon DH , Bates DW , Horsky J , Burdick E , Schaffer JL , Katz JN . Development and validation of a patient satisfaction scale for musculoskeletal care . Arthritis Care Res . 1999 ; 12 ( 2 ): 96 – 100 . Crossref PubMed Google Scholar
12. Diamond OJ , Howard L , Masri B . Five cases of tibial post fracture in posterior stabilized total knee arthroplasty using Prolong highly cross-linked polyethylene . Knee . 2018 ; 25 ( 4 ): 657 – 662 . Crossref PubMed Google Scholar
13. Faulkner A , Reidy MJ , Davies PSE , et al. Balancing training and outcomes in total knee replacement: A ten-year review . Surgeon . 2018 ; 16 ( 4 ): 227 – 231 . Crossref PubMed Google Scholar
14. Kazarian GS , Lawrie CM , Barrack TN , et al. The impact of surgeon volume and training status on implant alignment in total knee arthroplasty . J Bone Joint Surg Am . 2019 ; 101-A ( 19 ): 1713 – 1723 . Crossref PubMed Google Scholar
15. Goto K , Katsuragawa Y , Miyamoto Y . Outcomes and component-positioning in total knee arthroplasty may be comparable between supervised trained surgeons and their supervisor . Knee Surg Relat Res . 2020 ; 32 ( 1 ): 3 . Crossref PubMed Google Scholar
16. Huang S , Li X , Tang Y , et al. Different patient satisfaction levels between the first and second knee in the early stage after simultaneous bilateral total knee arthroplasty (TKA): a comparison between subjective and objective outcome assessments . J Orthop Surg Res . 2017 ; 12 ( 1 ): 121 . Crossref PubMed Google Scholar
17. Khanuja HS , Solano MA , Sterling RS , Oni JK , Chaudhry YP , Jones LC . Surgeon mean operative times in total knee arthroplasty in a variety of settings in a health system . J Arthroplasty . 2019 ; 34 ( 11 ): 2569 – 2572 . Crossref PubMed Google Scholar
Author contributions
G. A. Sheridan: Investigation, Formal analysis, Writing – original draft.
R. Moshkovitz: Investigation, Writing – review & editing.
B. A. Masri: Conceptualization, Investigation, Writing – review & editing.
Funding statement
The author(s) received no financial or material support for the research, authorship, and/or publication of this article.
Ethical review statement
Institutional Review Board approval was granted prior to commencing this study.
Open access funding
The authors confirm that the open access fee for this study was self-funded.
© 2022 Author(s) et al. This is an open-access article distributed under the terms of the Creative Commons Attribution Non-Commercial No Derivatives (CC BY-NC-ND 4.0) licence, which permits the copying and redistribution of the work only, and provided the original author and source are credited. See https://creativecommons.org/licenses/by-nc-nd/4.0/.









