Abstract
Aims
Although the short stem concept in hip arthroplasty procedure shows acceptable clinical performance, we sometimes get unexplainable radiological findings. The aim of this retrospective study was to evaluate changes of radiological findings up to three years postoperatively, and to assess any potential contributing factors on such radiological change in a Japanese population.
Methods
This is a retrospective radiological study conducted in Japan. Radiological assessment was done in accordance with predetermined radiological review protocol. A total of 241 hips were included in the study and 118 hips (49.0%) revealed radiological change from immediately after surgery to one year postoperatively; these 118 hips were eligible for further analyses. Each investigator screened whether either radiolucent lines (RLLs), cortical hypertrophy (CH), or atrophy (AT) appeared or not on the one-year radiograph. Further, three-year radiographs of eligible cases were reviewed to determine changes such as, disappeared (D), improved (I), stable (S), and progression (P). Additionally, bone condensation (BC) was assessed on the three-year radiograph.
Results
CH was observed in 49 hips (21.1%), AT was observed in 63 hips (27.2%), and RLLs were observed in 34 hips (14.7%) at one year postoperatively. Among 34 hips with RLLs, 70.6% showed change of either D or I on the three-year radiograph. BC was observed in younger patients more frequently.
Conclusion
The Fitmore stem works well in a Japanese population with favourable radiological change on hips with RLLs. Longer-term follow-up is required to determine clinical relevance.
Cite this article: Bone Jt Open 2022;3(1):20–28.
Take home message
Most of our cohort showed favourable radiological change of femur.
Even if there are radiological changes in the early postoperative period, improvement or stable appearance can also be seen over time, based on our three-year experience.
The short curved stem used in this study works differently from conventional (longer, straight) stems. Longer follow-up research is necessary to assess long-term performance.
Introduction
Implants, surgical technique, and surgical assistance have evolved over time. The short stem concept is to retain intact or untouched medullary canal while maintaining biological and mechanical fixation with the most proximal part of femur. Although short stems are clinically successful, the variety of bone reactions, such as cortical hypertrophy (CT), radiolucency, and atrophy (AT), after short stem hip arthroplasty surgery, is not fully understood.1-8 We frequently observed radiological changes beyond one year on the patient who received the Fitmore (Zimmer Biomet, USA) short stem hip arthroplasty without significant clinical signs or symptoms.
Rectangular cross-section of Fitmore stem was derived from that of the Zweymüller type femoral stem, which has a long-term clinical outcome.9-12 According to Pepke et al,13 rotational stability is higher compared to stems with a conically flat cross-section. We could actually feel rotational stability at the time of rasping during intraoperative femoral canal preparation. Further, Bieger et al14 reported that longitudinal initial stability is achieved by triple taper shape. In addition, shorter stem length with less lateral flare design allows the surgeon to insert the Fitmore stem along with curvature of medial calcar while preserving attachments of Piriformis and conjoint tendon, especially via the anterior approach.
The aim of this retrospective study was to evaluate changes of radiological findings up to three years postoperatively and to assess potential contributing factors on such radiological change.
Methods
Ethical approval was obtained before study implementation (approval number: 29-043(8659)). We offered to all eligible patients the opportunity to opt-out from the study at any time. Retrospective review of medical records, as well as radiographs, was conducted by investigators at our institution. Radiological assessment was attempted twice; initial assessment was conducted by multiple assessors other than the senior orthopaedic surgeon (HF), and the second assessment was done solely by the senior orthopaedic surgeon; agreement between first and second assessment was confirmed. A total of 241 hips in patients who received total hip arthroplasty (THA) using the Fitmore stem between Jan 2014 and Jun 2016 at the hospital were eligible for screening. Table I shows the demographic data and surgical parameters of two groups: 110 hips with radiological findings, and 122 hips without radiological findings, at one year.
Surgery and postoperative management
The Fitmore hip stems were implanted by a single surgical team, which was led by one of the authors (HF), as standard implant in all consecutive cases. Cases with an extremely narrow medullary canal at the subtrochanteric area or cases with extreme anteversion of the femoral neck (> 40°) were contraindicated. The approach was anterolateral supine minimally invasive (ALS) in 237 hips (98%) and posterolateral (PL) in four hips (2%). Figure 1 shows stem size distribution in our cohort with identification of radiological findings. A trabecular metal modular cup (Zimmer Biomet) was used in 241 hips (100%) and a ceramic head in 234 hips (97%). All patients started full weightbearing activities with a crutch gait immediately after the operation.

Fig. 1
Stem size distribution for entire cohort (n = 232). Black bar represents number of patients with radiological findings at one year postoperatively, and white bar represents number of patients without radiological finding at one year postoperatively.
Radiological assessment
Radiographs were taken in accordance with a well-established protocol as Engh suggested,15 and the same radiology team was responsible throughout the course of the patient journey.
Image assessment was conducted in accordance with the image assessment protocol, which had been developed before the study initiation. The protocol defines that CH was diagnosed when > 2 mm radiological appearance was observed extracortically, AT was qualitatively diagnosed when cortical absorption induced by stress-shielding was observed, and radiolucent lines (RLLs) were qualitatively diagnosed when they were observed between the inner ridge of cortex and inserted stem implant. Additionally, all image assessing investigators rated the testing image radiographs to confirm consistency of radiograph assessment, and we confirmed that interobserver reliability was 0.952 of interclass correlation coefficient (ICC) in 30 cases. When any disagreement on radiographical assessment was noted, a discussion was held to finalize the assessment result. The investigators screened postoperative anteroposterior (AP) radiographs at the one-year visit to confirm whether the patient showed a) CH, b) AT, or c) RLLs. Further image assessments at two years and three years were conducted to confirm changes over time. Changes were recorded according to the following four categories: disappeared (D), improved (I), stable (S), and progressed (P) for patients with any radiological findings at one year postoperatively. CH was diagnosed when > 2 mm radiological appearance was observed and in the case that > 2 mm of reduction was observed, then the CH was recognized as “I”, and both AT and RLLs were qualitatively assessed for changes. In addition, the existence of bone condensation (BC) was assessed on the three-year radiograph. The definition of radiological findings is shown in Figure 2. As a result of initial screening, 118 hips (49.0%) revealed any radiological findings and 123 hips (51.0%) did not have any radiological findings at one year postoperatively. Among 118 hips, radiographs at three years postoperatively were missed on eight hips, and of the 123 hips without radiological findings, one hip was missed at three years postoperatively. Therefore, overall 110 hips with radiological findings and 122 without radiological findings were subject to final analysis. The incidence ratio of each radiological finding was calculated by dividing the number of hips with findings by 232 hips. The ratio of improvement was calculated by dividing the number of hips with either “improved” or “disappeared” on the three-year radiograph by the number of hips with a particular finding on the one-year radiograph. A radiological finding was recorded at each Gruen zone (1 to 7).16
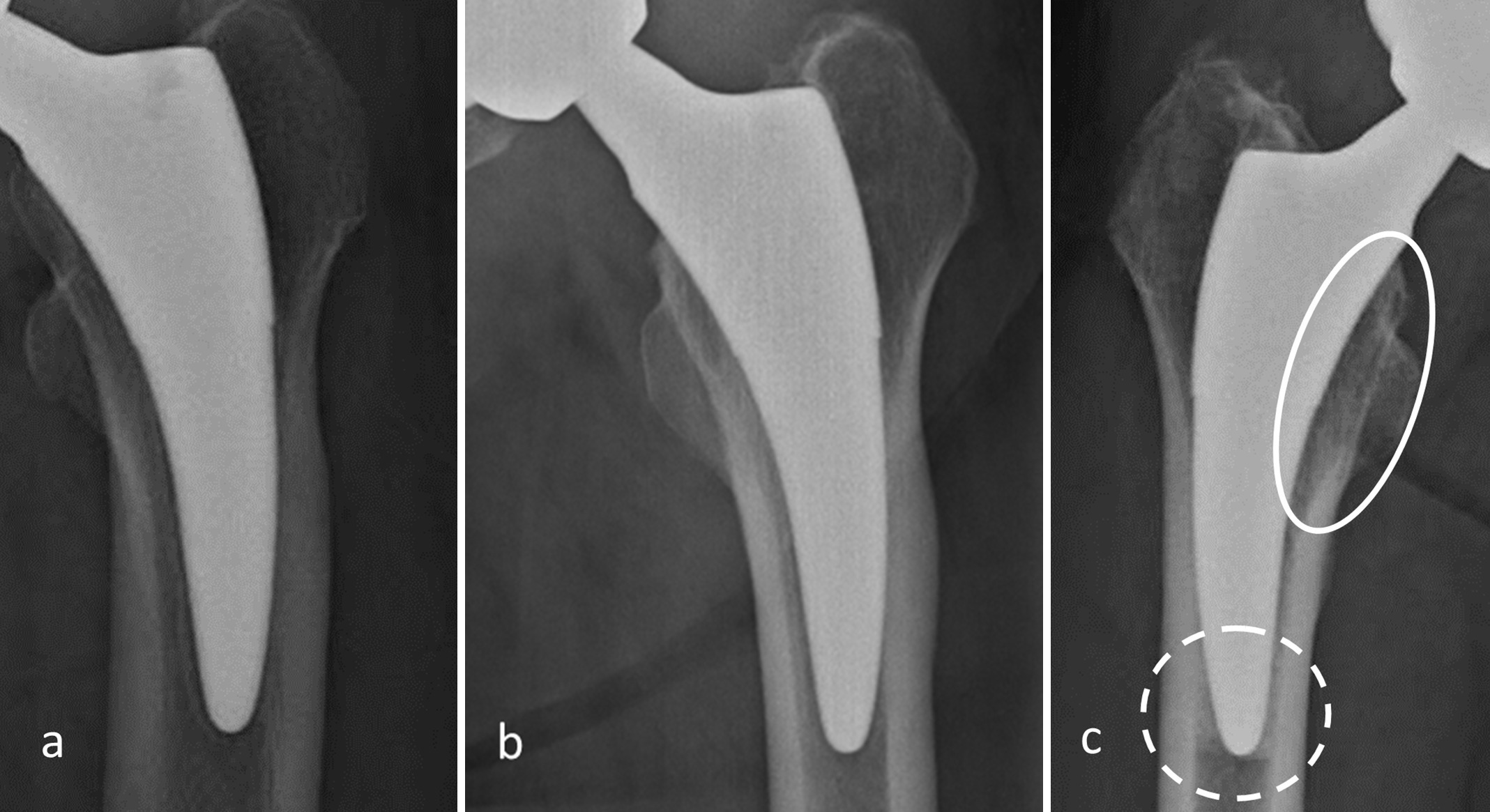
Fig. 2
Definition of each radiological finding: a) radiolucency on a 78-year-old female, b) cortical hypertrophy on a 72-year-old female, c) atrophy (circle with solid line), and bone condensation (circle with dotted line) on 64 years old female. All images were frontal view and taken at one year postoperatively.
Clinical evaluation
Japanese Orthopaedic Association Hip Disease Evaluation Questionnaire (JHEQ)17 scores were taken for all hips in accordance with standard practice. JHEQ score is a patient-reported outcome measure (PROM), with a highest possible score of 84 and a lowest possible score of 0, where a higher score indicates a better hip joint condition. The JHEQ score can be further assessed by individual domains: pain domain, movement domain, and mental domain are each assessed from 0 to 28 points.
Statistical analysis
Results were reported as the number of observations with percentage for categorical data, and comparisons were conducted using chi-squared test. Data values are expressed as means with ranges, and comparisons were done by independent-samples t-test. All statistical analyses were performed with Microsoft Excel 2016 (Microsoft, USA). A p-value < 0.05 was considered significant.
Results
Sex, weight, BMI, operating time, and intraoperative blood loss were significantly different between groups, but no JHEQ scores, including preoperative score as well as scores at three-year follow-up visit, were significantly different (Table II). Among 232 hips, 110 (47.4%) revealed at least one type of radiological finding (AT, RLL, or CH) at one year postoperatively. The most frequent findings were AT at Zone 1 and CH at Zone 3 on 35 hips. The proportion of CH among 232 hips was 21.0% (49 hips) and CH tended to appear at distal portion of stem (Zone 3/5). AT (27.0%, 63 hips) showed up at the proximal portion of stem (Zone 1/7) and RLLs (14.6%, 34 hips) tended to appear at Zone 1 or 4; most of these were marked as D or I at three years (Table III). Figure 3 captures typical RLL changes over time and Figure 4 shows RLL changes at each Gruen zone. Overall, radiological findings were stable throughout the course of study; only a few hips showed progression of radiological finding. Among 122 hips without radiological findings at one year postoperatively, one hip went on to show CH, and four hips show AT, at two years postoperatively. Four hips with AT did not disappear at three years postoperatively, while CH had disappeared by this time. No newly developed radiological findings at three years postoperatively were observed.

Fig. 3
Representative radiolucent line (RLL) case. a) Immediate postoperative radiograph. b) RLL is observed at Zone 1 and 5 at one year postoperatively. c) No RLL is observed at three years postoperatively. All images show frontal view of a 51-year-old female.
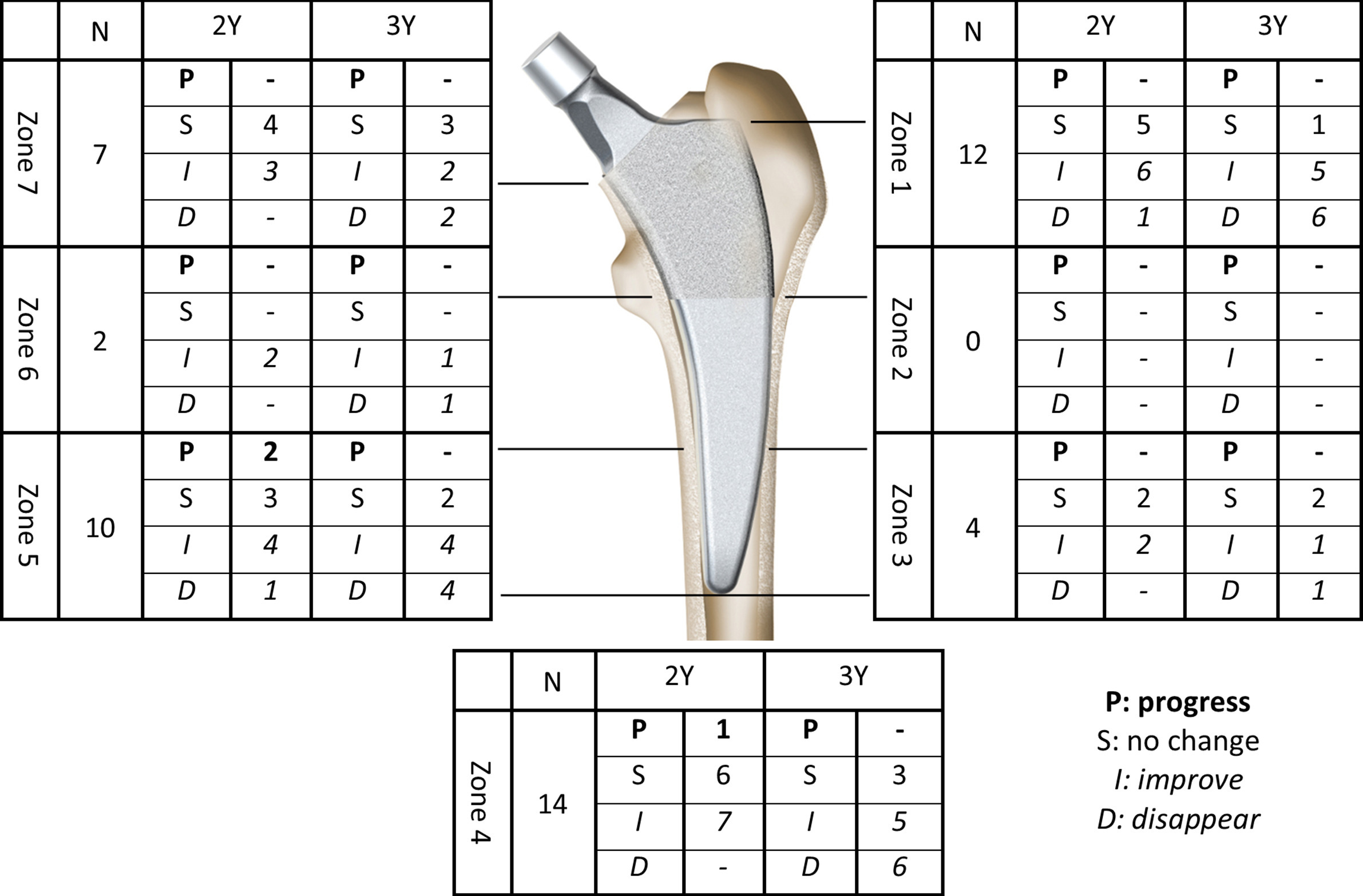
Fig. 4
Changes of radiolucent lines at each Gruen zone when compared to one-year postoperative radiograph. This figure has been provided courtesy of Zimmer Biomet.
Table I.
Demographic data of patients at one year postoperatively.
| Characteristic | With radiological findings (n = 110) | Without radiological findings (n = 122) | p-value |
|---|---|---|---|
| Sex, F:M | 95:15 | 87:35 | 0.005* |
| Side, R:L | 55:55 | 67:55 | 0.454* |
| Mean age at operation, yrs (range) | 65.6 (30 to 93) | 64.5 (23 to 87) | 0.470† |
| Mean height, cm (range) | 156.1 (142 to 182) | 157.2 (136 to 176) | 0.318† |
| Mean weight, kg (range) | 56.0 (39 to 89.6) | 60.1 (37 to 100) | 0.011† |
| Mean BMI, kg/m2 (range) | 22.9 (16.0 to 33.7) | 24.2 (17.4 to 32.9) | 0.008† |
| Mean operating time, mins (range) | 104.8 (43 to 203) | 119.6 (51 to 216) | < 0.001† |
| Mean blood loss, cc (range) | 302.4 (15 to 1495) | 375.8 (60 to 1590) | 0.043† |
| Approach, n | > 0.999* | ||
| ALS | 108 | 120 | |
| PL | 2 | 2 | |
| Dorr type, A:B:C | 8:95:7 | 17:103:2 | 0.057* |
-
*
Chi-squared test.
-
†
Independent-samples t-test.
-
ALS, anterolateral supine; PL, posterolateral.
Table II.
Clinical score comparison between patients with one-year postoperative radiological findings (n = 110) and those without (n = 122).
| Mean score (range) | Preoperative | Three yrs postoperative | ||||
|---|---|---|---|---|---|---|
| With findings | No findings | p-value* | With findings | No findings | p-value* | |
| JHEQ-VAS | 84.4 (35 to 100) | 86.8 (35 to 100) | 0.187 | 4.1 (0 to 30) | 6.0 (0 to 60) | 0.078 |
| JHEQ-Index | 22.0 (1 to 47) | 22.0 (1 to 53) | 0.971 | 74.6 (46 to 84) | 73.5 (31 to 84) | 0.346 |
| Pain | 8.6 (0 to 17) | 7.9 (0 to 24) | 0.268 | 27.0 (20 to 28) | 26.6 (9 to 28) | 0.217 |
| Activity | 5.1 (0 to 16) | 5.3 (0 to 16) | 0.684 | 22.7 (5 to 28) | 22.4 (2 to 28) | 0.682 |
| Mental | 8.4 (0 to 25) | 8.8 (0 to 26) | 0.624 | 25.0 (13 to 28) | 24.6 (13 to 28) | 0.373 |
-
*
Independent-samples t-test.
-
JHEQ, Japanese Orthopaedic Association Hip Disease Evaluation Questionnaire; VAS, visual analogue scale.
Table III.
Incidence ratio and improvement of each radiological finding (232 hips).
| Variable, n (%) | Hypertrophy | Improved/disappeared at 3 yrs, % | Atrophy | Improved/disappeared at 3 yrs, % | RLL | Improved/disappeared at 3 yrs, % |
|---|---|---|---|---|---|---|
| Number of cases | 49 (21.1) | 63 (27.2) | 34 (14.7) | |||
| Zone 1 | 0 | 35 (15.0) | 2.9 | 12 (5.2) | 91.7 | |
| Zone 2 | 1 (0.4) | 0 | 4 (1.7) | 0 | 0 | |
| Zone 3 | 35 (15.0) | 28.6 | 0 | 4 (1.7) | 50.0 | |
| Zone 4 | 3 (1.3) | 0 | 0 | 14 (6.0) | 78.6 | |
| Zone 5 | 17 (7.3) | 35.3 | 0 | 10 (4.3) | 80.0 | |
| Zone 6 | 1 (0.4) | 0 | 1 (0.4) | 100 | 2 (0.9) | 100 |
| Zone 7 | 1 (0.4) | 0 | 31 (13.3) | 6.5 | 7 (3.0) | 57.1 |
-
RLL, radiolucent line.
Table IV shows comparative data on 49 CH cases. Among 49 hips, CH was improved or disappeared on 13 hips (26.5% (Figure 5)). Significantly younger cases showed improvement of CH at three years.

Fig. 5
Representative cortical hypertrophy (CH) case, frontal view of a 59-year-old male. a) More than 2 mm of radiological change is recognized as CH at one year postoperatively. b) Reduction of > 2 mm is classified as improvement at three years postoperatively.
Table IV.
Patient demographics of 49 hips with cortical hypertrophy.
| Characteristic | Stable/progressed (n = 36) | Improved (n = 13) | p-value |
|---|---|---|---|
| Sex, F:M | 29:7 | 11:2 | 0.746* |
| Side, R:L | 15:21 | 12:1 | 0.002* |
| Mean age at operation, yrs (range) | 66.3 (30 to 81) | 57.8 (34 to 68) | 0.012† |
| Mean height, cm (range) | 157.6 (142 to 178) | 159.1 (152 to 182) | 0.595† |
| Mean weight, kg (range) | 59.7 (39 to 82) | 60.5 (43 to 84) | 0.844† |
| Mean BMI, kg/m2 (range) | 23.9 (17.8 to 33.7) | 23.8 (18.1 to 32.0) | 0.888† |
| Mean operating time, mins (range) | 121.7 (77 to 203) | 100.8 (81 to 125) | 0.003† |
| Mean blood loss, cc (range) | 371.4 (15 to 1,495) | 340.0 (50 to 1,015) | 0.722† |
| Approach, n | |||
| ALS | 36 | 13 | N/A |
| Dorr type, A:B:C | 1:33:2 | 0:12:1 | 0.805* |
-
*
Chi-squared test.
-
†
Independent-samples t-test.
-
ALS, anterolateral supine; N/A, not applicable.
Table V shows comparative data between hips with BC and no BC. A significantly younger population (p = 0.005, independent-samples t-test) showed BC, and more developmental dysplasia of the hip (DDH) cases were included in the BC group. Preoperative JHEQ pain domain was significantly better in the BC group (p = 0.040, independent-samples t-test), as were JHEQ VAS and mental domain (Table VI).
Table V.
Comparison of patient demographics between bone condensation and no bone condensation groups.
| Characteristic | BC (n = 95) | No BC (n = 136) | p-value |
|---|---|---|---|
| Sex, F:M | 73:22 | 108:28 | 0.641* |
| Side, R:L | 45:50 | 76:60 | 0.202* |
| Mean age at operation, yrs (range) | 62.5 (30 to 81) | 66.7 (23 to 93) | 0.005† |
| Mean height, cm (range) | 157.3 (142 to 182) | 155.8 (136 to 178) | 0.048† |
| Mean weight, kg (range) | 58.4 (39 to 89.6) | 57.0 (37 to 100) | 0.072† |
| Mean BMI, kg/m2 (range) | 23.4 (16.6 to 32.0) | 24.3 (16.0 to 33.7) | 0.275† |
| Diagnosis, n | 0.023* | ||
| OA | 31 | 52 | |
| DDH | 59 | 60 | |
| AVN | 4 | 15 | |
| RA | 0 | 3 | |
| RDC | 1 | 6 | |
| Mean operating time, mins (range) | 109.4 (45.5 to 191) | 112.3 (34 to 216) | 0.788† |
| Mean blood loss, cc (range) | 335.5 (15 to 1,495) | 340.3 (50 to 1,590) | 0.883† |
| Approach, n | > 0.999* | ||
| ALS | 93 | 134 | |
| PL | 2 | 2 | |
| Dorr type, A:B:C | 9:82:4 | 16:115:5 | 0.847* |
| With radiograph finding, Y:N | 55:40 | 55:81 | 0.009* |
-
*
Chi-squared test.
-
†
Independent-samples t-test.
-
ALS, anterolateral supine; AVN, avascular necrosis; BC, bone condensation; DDH, developmental dysplasia of the hip; OA, osteoarthritis; RA, rheumatoid arthritis; RDC, rapidly distructive coxarthropathy.
Table VI.
Comparison of clinical score between bone condensation and no bone condensation groups.
| Mean score (range) | Preoperatively | 3 yrs postoperatively | ||||
|---|---|---|---|---|---|---|
| w/ BC (n = 95) |
w/o BC (n = 136) |
p-value* | w/ BC (n = 95) |
w/o BC (n = 136) |
p-value* | |
| JHEQ-VAS | 84.1 (35 to 100) | 85.9 (50 to 100) | 0.703 | 4.0 (0 to 22) | 5.9 (0 to 60) | 0.048 |
| JHEQ-Index | 23.5 (1 to 53) | 21.0 (1 to 47) | 0.114 | 75.3 (46 to 84) | 73.4 (31 to 81) | 0.112 |
| Pain | 9.1 (0 to 24) | 7.7 (0 to 17) | 0.040 | 26.9 (20 to 28) | 26.7 (9 to 28) | 0.541 |
| Activity | 5.2 (0 to 16) | 5.3 (0 to 16) | 0.668 | 23.2 (9 to 28) | 22.4 (5 to 28) | 0.418 |
| Mental | 9.2 (0 to 26) | 8.0 (0 to 25) | 0.076 | 25.3 (13 to 28) | 24.4 (13 to 28) | 0.043 |
-
*
Independent-samples t-test.
-
BC, bone condensation; JHEQ, Japanese Orthopaedic Association Hip Disease Evaluation Questionnaire; VAS, visual analogue scale.
Complications
Approximately 2 mm of stem subsidence was reported in two cases at one year postoperatively, but none of subsided cases showed progression of subsidence at three years postoperatively.
During and after the operation, complications such as infection, fracture and dislocation, and loosening of stem were not observed. Good excursion and reacquisition of walking ability were achieved in all patients. Overall our cohort showed significant improvement from preoperative period to one-year visit, and then stable until three years’ follow-up visit. There is no revision reported in either group.
Discussion
This is, to our knowledge, the first longitudinal study to assess radiological changes of the Fitmore stem in an Asian population. In a typical Japanese population, half of them showed either CH, AT, or RLLs at one year postoperatively. Radiological appearance(s) seemed to be related to sex, where females tend to show radiological appearance at one year postoperatively. Relatively weaker bone quality is seen on the female patients than males within the same generation. Aro et al18 reported that low BMD affected initial stability and delayed osseointegration of cementless stems in women. Also, operating time was significantly shorter with significantly less intraoperative blood loss in the patient cohort with radiological findings at one year postoperatively. We believe those differences were not directly related to postoperative radiological appearances. Longer operating time with more blood loss is due to learning curve of Fitmore short stem usage in our institution. Mean operating time of the initial 50 cases was 117.3 minutes and from 51 cases onwards was 111.3 minutes. In fact, from the initial 50 cases, 35 patients were diagnosed without radiological findings at one year, and 15 patients were diagnosed with radiological finding at one year. This also affected blood loss, since a weak positive correlation coefficient (0.4) was found between operating time and blood loss.
Although RLLs are thought to be an initial sign of loosening, we found that improvement or even disappearance of RLLs was observed in 73.5% of hips (25/34). This phenomenon can be considered as an initial bone reaction until the Fitmore stem finds the appropriate position in the medullary canal without apparent subsidence. Our guess is that stress distribution pattern is not stable or consistent before coming to the “Final” position, which takes approximately one year. Further, once the stem comes to the “Final” position, the stress distribution pattern becomes stable/consistent, which can lead to bone remodelling by adjusted stress distribution pattern,19-26 which is specific to each patient. Gustke27 reported that cortical hypertrophy was observed in 29% of the cohort, which was clinically uneventful. Our results, especially the 21.0% incidence of CH (49 out of 232 hips), were quite different from previous report by Thalmann et al,28 who reported that CH was observed in 69% of patients at one year postoperatively and 71% at five years. Our cohort includes a typical Japanese patient group as assessed by ratio of Dorr type (A: 25 hips/10.8%, B: 198 hips/85.3%, C: 9 hips/3.9%), whereas the cohort in Thalmann et al’s28 study consists of 82% of Dorr type A and 18% of Dorr type B. There is no specific relationship between Dorr type and radiological finding (Table I, p = 0.057, chi-squared test). This suggests that bone type does not impact on radiological findings as long as an appropriate level of Fitmore stem fixation to the medullary canal is obtained. What is novel in our study is that CH in 13 hips (26.5%) either disappeared or improved in three years. To the authors’ knowledge, no such cases were reported previously. The actual mechanism is not known, but this may suggest that stress distribution at a particular portion does not necessarily continue postoperatively. Some sort of gradual change via biological and/or mechanical stabilization of the stem may contribute to the change of stress distribution pattern.29-33 CH patients with improved/disappeared radiological findings at three years were significantly younger than those with no change. We suggest that this phenomenon is similar to the bone remodelling process, which is more favourable to a younger population than an older population, perhaps due to higher degree of systemic digestion.
Since BC was observed significantly more often in the younger population, BC can be interpreted as a sign of bone fixation or remodelling. Gustke27 reported short-term results on 500 cases of primary THA using the Fitmore stem. Stem subsidence occurred in 34% of the initial 100 cases, but no subsidence in any of the later cases was identified and they pointed out the surgical technique-related issue. In our current cohort, we also experienced two subsided cases in the early phase. We believe that the cause of subsidence is the same as that reported by Cinotti et al,34 who believe that at least in a few cases, short stems may need initial settling in the host bone to gain mechanical stability and subsequent metaphyseal osseointegration of the implant. Nieuwenhuijse et al35 evaluated another short femoral stem, the Global Tissue-Sparing (GTS) stem, by using Roentgen stereophotogrammetric analysis. The GTS stem showed initial migration up to three months and then stabilized without significant stem migration until two years postoperatively. This may suggest that initial instability or stability can affect radiological findings at a certain postoperative timepoint. Since stress intensity to bone and implant surface of the shorter stem was quite high in comparison to the standard length stem as Kwak et al36 suggested by finite element model; it was thought that radiological change becomes more visible when using a short stem.
As for 122 hips without radiological findings at one year postoperatively, radiological change was not observed in 96% of the cohort (117 of 122). Although no apparent tendencies were found, minor differences were found in terms of JHEQ subscale on five hips showing CH or AT at two years postoperatively. Mean preoperative JHEQ Activity domain and Mental domain of 117 cases were 5.4 and 9.0, respectively, and those of five cases were 2.2 and 4.2, respectively. As far as the entire cohort is concerned, only 2.2% (five hips) of population show radiological findings beyond one year postoperatively, and none of the patients show radiological findings beyond two years postoperatively. Since we used one-year postoperative radiographs for screening, we could detect most of the radiological changes of our entire cohort.
Our study has limitations. The first is that the radiological assessment was not done by independent reviewers. We developed an image assessment protocol, and trial assessment was done until a certain degree of consistency was seen among assessors. Although unblinded multiple investigators assessed radiographs, assessment results should be consistent. Two different surgeons assessed all radiographs and agreement between two assessors was confirmed. The second limitation is that the study is retrospective. However, drop-out or lost-to-follow-up ratio is quite small: 4% (9 out of 241 hips).
A strength of our study is that all patients were operated on by a single surgical team. Therefore, operating parameters, such as sizing of the stem, insertion level as well as alignment, and postoperative management were quite consistent. This makes our data less variable.
In conclusion, the Fitmore stem works well in a Japanese population. Approximately half of the cases did not show radiological change at one year. Patient-reported outcome measures did not differ between patients with and without radiological changes. Moreover, even if RLLs are present around the Fitmore stem, 71% may have an opportunity to improve or diminish by three years postoperatively. Longer-term follow-up is needed to determine the clinical success of this implant.
References
1. Pipino F , Calderale PM . Biodynamic total hip prosthesis . Ital J Orthop Traumatol . 1987 ; 13 ( 3 ): 289 – 297 . PubMed Google Scholar
2. Morrey BF . Short-stemmed uncemented femoral component for primary hip arthroplasty . Clin Orthop Relat Res . 1989 ; 249 : 169 – 175 . PubMed Google Scholar
3. Dietrich M , Kabelitz M , Dora C , Zingg PO . Perioperative fractures in cementless total hip arthroplasty using the direct anterior minimally invasive approach: Reduced risk with short stems . J Arthroplasty . 2018 ; 33 ( 2 ): 548 – 554 : S0883-5403(17)30799-4 . Crossref PubMed Google Scholar
4. Oldenrijk JV , Molleman J , Klaver M , et al. Revision rate after short-stem total hip arthroplasty a systematic review of 49 clinical studies . Acta Orthop . 2014 ; 85 ( 3 ): 250 . Google Scholar
5. Falez F , Casella F , Panegrossi G , Favetti F , Barresi C . Perspectives on metaphyseal conservative stems . J Orthop Traumatol . 2008 ; 9 ( 1 ): 49 – 54 . Crossref PubMed Google Scholar
6. Molli RG , Lombardi AJ , Berend KR , Adams JB , Sneller MA . A short tapered stem reduces intraoperative complications in primary total hip arthroplasty . Clin Orthop Relat Res . 2012 ; 470 ( 2 ): 450 – 461 . Crossref PubMed Google Scholar
7. Kutzner KP , Pfeil D , Kovacevic MP , et al. Radiographic alteration in short-stem total hip arthroplasty: a 2-year followup study of 216 cases . Hip Int . 2016 ; 26 ( 3 ): 278 – 283 . Google Scholar
8. Hauer G , Vielguy I , Amerstorfer F . Survival Rate of Short-Stem Hip Prostheses- A Comparative Analysis of Clinical Studies and National Arthroplasty Registers . J Arthroplasty . 2018 ; 33 ( 6 ): 1800 – 1805 : S0883-5403(18)30054-8 . Google Scholar
9. Suckel A , Geiger F , Kinzl L . Long-term results for the uncemented Zweymüller/Alloclassic hip endoprosthesis. A 15-year minimum follow-up of 320 hip operations . J Arthroplasty . 2009 ; 24 ( 6 ): 846 – 853 . Google Scholar
10. Vervest TM , Anderson PG , van Hout F . Ten to twelve-year results with the Zweymüller cementless total hip prosthesis . J Arthroplasty . 2005 ; 20 ( 3 ): 362 – 368 . Crossref PubMed Google Scholar
11. Paleochorlidis IS , Badras LS , Skretas EF , Georgaklis VA , Karachalios TS , Malizos KN . Clinical outcome study and radiological findings of Zweymuller metal on metal total hip arthroplasty. a follow-up of 6 to 15 years . Hip Int . 2009 ; 19 ( 4 ): 301 – 308 . Crossref PubMed Google Scholar
12. Wick M , Lester DK . Radiological changes in second- and third-generation Zweymüller stems . J Bone Joint Surg Br . 2004 ; 86-B ( 8 ): 1108 – 1114 . Crossref PubMed Google Scholar
13. Pepke W , Nadorf J , Ewerbeck V , Streit MR , Klinkel S , Gotterbarm T . Primary stability of the Fitmore stem: biomechanical comparison . Int Orthop . 2014 ; 38 ( 3 ): 483 – 487 . Crossref PubMed Google Scholar
14. Bieger R , Ignatius A , Decking R , Claes L , Reichel H , Dürselen L . Primary stability and strain distribution of cementless hip stems as a function of implant design . Clinical Biomechanics . 2012 ; 27 ( 2 ): 158 – 164 . Crossref PubMed Google Scholar
15. Engh CA . Recent advances in cementless total hip arthroplasty using the AML prosthesis . Techniques in Orthopaedics . 1991 ; 6 ( 3 ): 59 – 72 . Google Scholar
16. Gruen TA , McNeice GM , Amstutz HC . “Modes of failure” of cemented stem- type femoral components: a radiographic analysis of loosening . Clin Orthop . 1979 ; 141 : 17 – 27 . Google Scholar
17. Matsumoto T , Kaneuji A , Hiejima Y , et al. Japanese Orthopaedic Association Hip-Disease Evaluation Questionnaire (JHEQ): a patient-based evaluation tool for hip-joint disease. The Subcommittee on Hip Disease Evaluation of the Clinical Outcome Committee of the Japanese Orthopaedic Association . J Orthop Sci . 2012 ; 17 ( 1 ): 25 – 38 . Google Scholar
18. Aro TH , Alm JJ , Moritz N , Mäkinen TJ , Lankinen P . Low BMD affects initial stability and delays stem osseointegration in cementless total hip arthroplasty in women: a 2-year RSA study of 39 patients . Acta Orthop . 2012 ; 83 ( 2 ): 107 – 114 . Crossref PubMed Google Scholar
19. Sumner DR , Turner TM , Urban RM , Galante JO . Experimental studies of bone remodeling in total hip arthroplasty . Clin Orthop Relat Res . 1992 ; 276 : 83 – 90 . PubMed Google Scholar
20. Sychterz CJ , Engh CA . The influence of clinical factors on periprosthetic bone remodeling . Clin Orthop Relat Res . 1996 ; 332 ( 322 ): 285 – 292 . PubMed Google Scholar
21. Pitto RP , Schramm M , Hohmann D , Schmidt R . Clinical outcome and quantitative evaluation of periprosthetic bone-remodeling of an uncemented femoral component with taper design. A prospective study . Chir Organi Mov . 2001 ; 86 ( 2 ): 87 – 97 . PubMed Google Scholar
22. Freitag T , Hein MA , Wernerus D , Reichel H , Bieger R . Bone remodelling after femoral short stem implantation in total hip arthroplasty: 1-year results from a randomized DEXA study . Arch Orthop Trauma Surg . 2016 ; 136 ( 1 ): 125 – 130 . Crossref PubMed Google Scholar
23. Yan SG , Weber P , Steibruck A . Periprosthetic bone remodelling of short-stem total hip arthroplasty: a systematic review . Int Orthop . 2018 ; 42 : 2077 – 2086 . Crossref PubMed Google Scholar
24. Acklin YP , Jenni R , Bereiter H . Prospective clinical and radiostereometric analysis of the Fitmore short-stem total hip arthroplasty . Arch Orthop Trauma Surg . 2016 ; 136 ( 2 ): 277 – 284 . Crossref PubMed Google Scholar
25. Speirs AD , Heller MO , Taylor WR , Duda GN , Perka C . Influence of changes in stem positioning on femoral loading after Thr using a short-stemmed hip implant . Clin Biomech . 2007 ; 22 ( 4 ): 431 – 439 . Crossref PubMed Google Scholar
26. Patel RM , Lo WM , Cayo MA , Dolan MM , Stulberg SD . Stable, dependable fixation of short-stem femoral implants at 5 years . Orthopedics . 2013 ; 36 ( 3 ): 301 – 307 . Crossref PubMed Google Scholar
27. Gustke K . Short stems for total hip arthroplasty. initial experience with the Fitmore stem . J Bone Joint Surg Br . 2012 ; 94-B ( Suppl A ): 47 – 51 . Google Scholar
28. Thalmann C , Kempter P , Stoffel K , Ziswiler T , Frigg A . Prospective 5-year study with 96 short curved Fitmore™ hip stems shows a high incidence of cortical hypertrophy with no clinical relevance . J Orthop Surg Res . 2019 ; 14 ( 1 ): 156 – 165 . Crossref PubMed Google Scholar
29. Innmann M , Weishorn J , Bruckner T . Fifty-six percent of proximal femoral cortical hypertrophies 6 to 10 years after Total hip arthroplasty with a short Cementless curved hip stem -a cause for concern . BMC Musculoskelet Disord . 2019 ; 20 ( 1 ): 261 . Google Scholar
30. Maier MW , Streit MR , Innmann MM , et al. Cortical hypertrophy with a short, curved uncemented hip stem does not have any clinical impact during early follow-up . BMC Musculoskelet Disord . 2015 ; 16 ( 1 ): 1 – 9 . Google Scholar
31. Ritter MA , Fechtmann RW . Distal CH following total hip arthroplasty . J Arthroplasty . 1988 ; 3 ( 2 ): 117 – 121 . Google Scholar
32. Cho YJ , Chun YS , Rhyu KH , Baek JH , Liang H . Distal Femoral Cortical Hypertrophy after Hip Arthroplasty Using a Cementless Double-Tapered Femoral Stem . J Orthop Surg (Hong Kong) . 2016 ; 24 ( 3 ): 317 – 322 . Google Scholar
33. Katsimihas M , Katsimihas G , Lee MB , Learmonth ID . Distal femoral cortical hypertrophy: predisposing factors and their effect on clinical outcome . Hip Int . 2006 ; 16 ( 1 ): 18 – 22 . Crossref PubMed Google Scholar
34. Cinotti G , Della Rocca A , Sessa P , Ripani FR , Giannicola G . Thigh pain, subsidence and survival using a short cementless femoral stem with pure metaphyseal fixation at minimum 9-year follow-up . Orthop Traumatol Surg Res . 2013 ; 99 ( 1 ): 30 – 36 : S1877-0568(12)00278-2 . Crossref PubMed Google Scholar
35. Nieuwenhuijse MJ , Vehmeijer SBW , Mathijsen NMC , Keizer SB . Fixation of the short global tissue-sparing hip stem . Bone Joint J . 2020 ; 102-B ( 6 ): 699 – 708 . Crossref PubMed Google Scholar
36. Kwak D , Bang S , Lee S , Park J , Yoo J . Effect of stem position and length on bone-stem constructs after cementless hip arthroplasty . Bone Joint Res . 2021 ; 10 ( 4 ): 250 – 258 . Crossref PubMed Google Scholar
Author contributions
H. Fujii: Conceptualization, Formal analysis, Writing – original draft.
T. Hayama: Data curation, Formal analysis, Investigation.
T. Abe: Investigation.
M. Takahashi: Investigation.
A. Amagami: Investigation.
Y. Matsushita: Investigation, Writing – review & editing.
T. Otani: Writing – review & editing.
M. Saito: Supervision.
Funding statement
No external funding source was used for this study. No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
ICMJE COI statement
Informed consent was obtained from each patient. The authors declare that they have no competing interests.
Data sharing
This study was carried out in the Hospital of the Jikei University School of Medicine (3–25-8 Nishi-Shinbashi Minato-ku, Tokyo, Japan). The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Acknowledgements
The techniques used in this research, especially regarding the surgical operation, were supported by the Department of Orthopaedic Surgery at the Jikei University School of Medicine.
Ethical review statement
This study was conducted in accordance with the World Medical Association Declaration of Helsinki and was approved by the institutional review board of The Jikei University (Approval number: 29-043(8659)).
Open access funding
The authors confirm that the open access fee for this study was self-funded.
© 2022 Author(s) et al. This is an open-access article distributed under the terms of the Creative Commons Attribution Non-Commercial No Derivatives (CC BY-NC-ND 4.0) licence, which permits the copying and redistribution of the work only, and provided the original author and source are credited. See https://creativecommons.org/licenses/by-nc-nd/4.0/.









