Abstract
Aims
Single-shot adductor canal block (ACB) after total knee arthroplasty (TKA) for postoperative analgesia is a common modality. Patients can experience breakthrough pain when the effect of ACB wears off. Local anaesthetic infusion through an intra-articular catheter (IAC) can help manage breakthrough pain after TKA. We hypothesized that combined ACB with ropivacaine infusion through IAC is associated with better pain relief compared to ACB used alone.
Methods
This study was a prospective double-blinded placebo-controlled randomized controlled trial to compare the efficacy of combined ACB+ IAC-ropivacaine infusion (study group, n = 68) versus single-shot ACB+ intra-articular normal saline placebo (control group, n = 66) after primary TKA. The primary outcome was assessment of pain, using the visual analogue scale (VAS) recorded at 6, 12, 24, and 48 hours after surgery. Secondary outcomes included active knee ROM 48 hours after surgery and additional requirement of analgesia for breakthrough pain.
Results
The study group (mean visual analogue scale (VAS) pain score of 5.5 (SD 0.889)) experienced significant reduction in pain 12 hours after surgery compared to the control group (mean VAS 6.62 (SD 1.356); mean difference = 1.12, 95% confidence interval (CI) -1.46 to 0.67; p < 0.001), and pain scores on postoperative day (POD) 1 and POD-2 were lower in the study group compared to the control group (mean difference in VAS pain = 1.04 (-1.39 to -0.68, 95% CI, p < 0.001). Fewer patients in the study group (0 vs 3 in the control group) required additional analgesia for breakthrough pain, but this was not statistically significant. The study group had significantly increased active knee flexion (mean flexion 86.4° (SD 7.22°)), compared to the control group (mean 73.86° (SD 7.88°), mean difference = 12.54, 95% CI 9.97 to 15.1; p < 0.014).
Conclusion
Combined ACB+ ropivacaine infusion via IAC is a safe, reproducible analgesic modality after primary TKA, with superior analgesia compared to ACB alone. Further large volume trials are warranted to generate evidence on clinical significance on analgesia after TKA.
Cite this article: Bone Jt Open 2021;2(12):1082–1088.
Take home message
Breakthrough pain after total knee arthroplasty remains a impediment to recovery and rehabilitation. Adductor canal block (ACB) is effective in managing breakthrough pain after the effect of spinal anaesthesia wears off.
Since the ACB analgesic effect is short-lived, we propose the use of intra-articular local anaesthetic infusion for breakthrough pain after surgery.
In our study, patients benefited from local anaesthetic infusion with reduced pain and improved knee range of motion. Further large volume trials will help establish a clinical practice guideline for the use of intra-articular local anaesthetic infusions for postoperative pain management after primary total knee arthroplasty.
Introduction
Total knee arthroplasty (TKA) is one of the most commonly performed orthopaedic procedures. Postoperative pain following TKA is a challenge and can interfere with patient rehabilitation. Inadequate pain control may reduce patient participation in physical therapy, resulting in longer length of stay (LOS) and poorer outcomes. Pain management strategies have evolved from systemic opioids to epidural anaesthesia to peripheral nerve blockade, trending towards a more local approach which has shown promising results.1-3 Multimodal analgesia has been shown to be superior to monotherapy, subsequently reducing opiate use after surgery.
Peripheral nerve blocks and local anaesthetic agents have several advantages when compared to regional or systemic methods. These include less toxicity and early mobilization.2,3 Problems with epidural anaesthesia are mainly related to delayed rehabilitation, and bladder and bowel problems.4 There have been reports of quadriceps weakness with femoral nerve block, leading to delayed mobilization.5 Patient-controlled analgesia often leads to under-dosage or over-dosage of the drug, requiring frequent monitoring and dose adjustment for adequate pain relief, to minimize opioid-related side effects.6
Adductor canal block (ACB) is a peripheral nerve blockade technique which provides pain relief without compromising quadriceps strength and allows early rehabilitation.1,7 However, the majority of patients experience block resolution and breakthrough pain on the day of surgery. Andersen et al8 reported a mean duration of only 10.5 hours of pain relief with adductor canal block. We hypothesize that local anaesthetic infusion through a catheter can help manage breakthrough pain and provide prolonged analgesia. Intra-articular catheter (IAC) with infusion of a local anaesthetic (ropivacaine) has also been reported to provide adequate analgesia following surgery without any systemic effects.9 Dannana et al10 studied the efficacy of ACB+ multimodal periarticular infiltration (MPI) with and without local anaesthetic infusion via IAC, reporting increased pain relief in the group with additional local anaesthetic infusion. However, this was a non-randomized prospective study. To our knowledge, there are no placebo-controlled double-blind randomized controlled trials (RCTs) which studied the efficacy of local anaesthetic infusion via IAC in combination with single-shot ACB.
The aim of this study was to compare the postoperative analgesic efficacy of single-shot adductor canal blockade (ACB) in isolation (in combination with placebo normal saline infusion through IAC) versus single-shot ACB in combination with intra-articular ropivacaine infusion after primary TKA. Secondary objectives were to compare active knee range of motion (ROM) and analgesia-related complications between the two groups.
Methods
This study was a placebo-controlled double-blinded RCT conducted at a single centre. The trial was approved by the Institutional Ethics Committee (SS/2018/IEC 296) and prospectively registered with the Clinical Trials Registry of India (CTRI/2018/08/015386). The trial was to compare the postoperative analgesic efficacy of single-shot ACB alone (control group) versus single-shot ACB combined with intra-articular ropivacaine infusion via IAC (study group), in patients undergoing primary total knee arthroplasty. The trial was conducted after obtained written informed consent of trial participants and according to the Declaration of Helsinki guidelines.11
Patients undergoing unilateral TKA for primary osteoarthritis (OA) of the knee were eligible for participation. Inclusion criteria comprised patients of either sex, aged 20 years and older, with primary OA of the knee joint, who consented to undergo unilateral primary TKA. Exclusion criteria were patients undergoing bilateral simultaneous or staggered TKA, inflammatory arthropathy, post-traumatic arthritis, history of previous surgeries on the knee, gross deformities (varus or valgus more than 20° or fixed-flexion deformity more than 15°), and patients who could not comprehend the visual analogue pain scale (VAS).
All patients participating in this study were operated under spinal anaesthesia, and received 2.5 ml of 0.5% hyperbaric bupivacaine intrathecal. All surgeries were performed by a single surgeon (AVGR), using a standard medial-parapatellar approach and a posterior-stabilized prosthesis design (P.F.C. Sigma Posterior-Stabilized Knee, DePuy Synthes, USA). In all cases, an IAC was used. The participants of the study group were randomized to receive ultrasound-guided ACB in combination with a local anaesthetic infusion (20 ml, 0.2% ropivacaine, administered every six hours for the first 24 hours after surgery) via IAC. The control group received ACB in combination with equal-volume placebo (20 ml normal saline, administered every six hours for the first 24 hours after surgery) via IAC. ACB was administered in both groups immediately after the surgery in the operating room, with 20 ml of 0.2% ropivacaine. A bolus of 20 ml of 0.2% ropivacaine equates to 40 mg of the local anaesthetic. Administration of intra-articular boluses every six hours adds up to a cumulative ropivacaine dose of 160 mg of ropivacaine, which is less than the daily maximum dose of the local anaesthetic (225 mg) in adults, as reported by Rosenberg.12
Patients in both study groups received oral celecoxib (200 mg) and gabapentin (300 mg) as pre-emptive analgesia 12 hours before surgery. A uniform postoperative analgesic protocol was implemented with intravenous (IV) paracetamol (1 g) every eight hours for the first 24 hours postoperatively, followed by a switch to oral celecoxib (200 mg) twice a day, oral paracetamol (1 g) three times a day and gabapentin (300 mg) once a day till discharge. Breakthrough pain in the recovery room (first 24 hours) was managed with IV fentanyl bolus given, based on body weight, by the anaesthesiologist. Breakthrough pain in the ward was managed with stat intravenous tramadol 50 mg. IACs were removed on postoperative day (POD) 2 in all cases and all patients were discharged on the second postoperative day.
Outcomes measured
The primary outcome (postoperative pain) was assessed using the VAS. The VAS score was scored out of 10 and was recorded with the patient at rest. VAS pain was recorded at six and 12 hours postoperatively on POD 0 (day of surgery), every eight hours on POD 1, and once on POD 2 before the patient is discharged. All patients were started on physical therapy with knee ROM and quadriceps exercises on POD 1.
The secondary outcomes (active knee ROM, additional analgesic requirements for breakthrough pain, and immediate postoperative complications) were recorded on POD 2. Side effects of ropivacaine toxicity (including blurred vision, chest pain, dizziness, syncope, peri-oral paraesthesias, acute onset delirium, and cardiac arrhythmias) were monitored and documented in the immediate postoperative period.
Randomization
A total of 150 patients were enrolled in the study and subsequently 140 patients were randomized into two groups. Randomization was performed with the help of a computer-generated, blocked random-allocation sequence with a 1:1 ratio. Patients enrolled in the study and the operating surgeon were blinded to modality of analgesia prior to surgery. Postoperative pain and functional assessment by an arthroplasty fellowship trainee (VC), who was also blinded to the randomization scheme. A sealed envelope was attached to the file of the patient on admission, with details of random allocation. Patients were randomized into two groups: the study group (combination of single-shot ACB and local anaesthetic infusion (bolus of 20 ml of 0.2% ropivacaine every six hours) via IAC), and the control group (combination of single-shot ACB and placebo (bolus 20 ml of normal saline every six hours) via IAC).
Statistical analysis
Assessment of whether the data were normally distributed was made using the Kolmogorov-Smirnov test. Continuous variables were analyzed using the independent-samples t-test. Parametric categorical variable data were analyzed using the chi-squared test and non-parametric data was analyzed with Fisher’s exact test. The SPSS 19.0 software (IBM, USA) was used for the statistical analysis. The nature of hypothesis testing was two-tailed and a p-value < 0.005 was considered statistically significant. As VAS pain score assessment was a repeated outcome measure, analysis of variance (ANOVA) was performed to compare the mean scores at different time intervals to analyze significance.
To show a difference of ‘one point’ on the VAS scale (scored 0 to 10), pre-study power analysis estimated a sample size of 50 participants in each group with 95% confidence intervals (CIs) and power of 0.8. Significance was defined as a p-value < 0.05. Based on published studies,13,14 we considered a one-point difference on the VAS pain scale to be a clinically significant change. Estimating a loss to follow-up of 15% to 20%, we set a target of 75 participants in each group.
Results
The flow diagram of the trial, based on Consolidated Standards of Reporting Trials (CONSORT) guidelines,15 is illustrated in Figure 1. A total of 140 study participants were randomized into two groups: the study group (n = 70, ACB+ ropivacaine infusion via IAC) and the control group (n = 70, ACB+ normal saline placebo via IAC). Six patients were excluded (two from the study group and four from the control group) due to IAC blockade requiring premature removal of the IAC. Overall, 134 trial participants (68 study group, 66 control group) were included in the final data analysis.
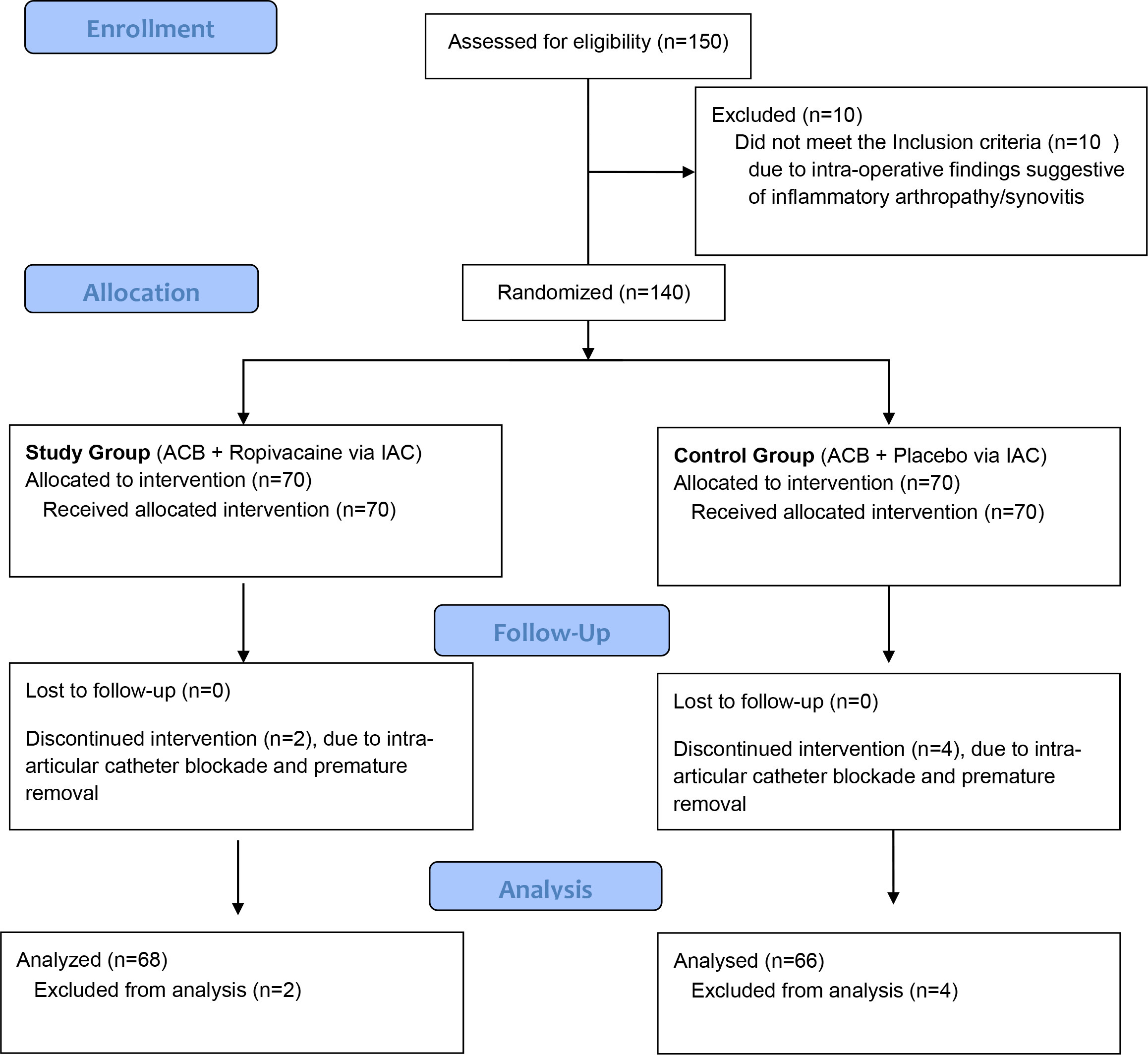
Fig. 1
Consolidated Standards of Reporting Trials flow diagram.
Baseline demographic and clinical characteristics of trial participants are summarized in Table I.
Table I.
Baseline information of study participants.
| Variable | Study group (n = 68) |
Control group (n = 66) |
|---|---|---|
| Mean age, yrs (SD) | 66.4 (9.4) | 66.6 (8.6) |
| Sex, n (%) | ||
| Male | 28 (41.1) | 31 (46.9) |
| Female | 40 (58.8) | 35 (53.03) |
| Mean height, cm (SD) | 157 (8.5) | 163 (7.4) |
| Mean weight, kg, (SD) | 68 (11.4) | 72 (9.6) |
| Mean BMI, kg/m2 (SD) | 27.5 (2.5) | 27.09 (1.8) |
| Mean CCI (SD) | 3 (1.15) | 3.17 (1.27) |
| ASA classification, n (%) | ||
| ASA 1 | 11 (16.2) | 13 (19.7) |
| ASA 2 | 57 (83.8) | 53 (80.3) |
| Mean duration of surgery, mins (SD) | 70 (8.5) | 68 (10.2) |
| Mean preoperative VAS (SD) | 6.29 (0.648) | 6.0 (0.765) |
| Mean preoperative knee flexion, ° (SD) | 100.5 (15.4) | 105 (9.8) |
-
ASA, American Society of Anesthesiologists; CCI, Charlson Comorbidity Index; SD, standard deviation; VAS, visual analogue scale.
Primary outcome assessment: postoperative pain and analgesic efficacy of intervention
The pain difference, as assessed by VAS pain scores, was not significantly different in the first six hours after surgery (study group mean VAS pain score 4.88 (standard deviation (SD) 0.744) vs control group 4.98 (SD 0.969); mean difference = 0.1 with 95% CI -0.39 to 0.19; p = 0.494, ANOVA). By the end of POD 0, study group (ACB+ ropivacaine) with mean VAS pain score of 5.5 (SD 0.889) experienced significant reduction in pain compared to the control group (mean VAS 6.62 (SD 1.356), mean difference = 1.12, 95% CI -1.46 to -0.67; p < 0.001, ANOVA for repeated measures). Similarly, VAS scores at rest on POD 1 and POD 2 were lower in the study group compared to the control group (Table II) and the difference was found to be statistically significant (mean difference in VAS pain = 0.97 with 95% CI -1.254 to -0.686; p < 0.001, ANOVA for repeated measures).
Table II.
Postoperative pain and range of motion assessment.
| Outcome measured | Study group (n = 68) | Control group (n = 66) | Mean difference (95% CI) | p-value* |
|---|---|---|---|---|
| Mean VAS pain 6 hrs postop (SD) | 4.88 (0.744) | 4.98 (0.969) | 0.1 (-0.39 to 0.19) | 0.494 |
| Mean VAS pain 12 hrs postop (SD) | 5.5 (0.889) | 6.62 (1.356) | 1.12 (-1.46 to -0.67) | < 0.001 |
| Mean VAS pain, 6 am, POD 1 (SD) | 5.49 (0.906) | 6.53 (1.427) | 1.04 (-1.486 to -0.67) | < 0.001 |
| Mean VAS pain, 12 pm, POD 1 (SD) | 4.96 (0.905) | 6 (1.129) | 1.04 (-1.39 to -0.68) | < 0.001 |
| Mean VAS pain, 6 pm, POD 1 (SD) | 5.5 (0.68) | 6.42 (0.929) | 0.92 (-1.25 to -0.68) | < 0.001 |
| Mean VAS pain, 6 am, POD 2 (SD) | 5.53 (0.922) | 6.52 (0.864) | 0.99 (-1.30 to -0.69) | < 0.001 |
| Mean active knee ROM on POD 2, ° (SD) | 86.40 (7.220) | 73.86 (7.884) | 13 (9.97 to 15.10) | < 0.001 |
-
*
Independent-samples t-test.
-
CI, confidence interval; POD, postoperative day; ROM, range of motion; SD, standard deviation; VAS, visual analogue scale.
Comparison of breakthrough pain and additional analgesic requirements
None of the study group participants required additional analgesics for breakthrough pain. Adequate analgesia (VAS pain score < 5/10), was achieved in all study group participants with intra-articular ropivacaine infusion along with intravenous paracetamol 1 g, every eight hours. Three of 66 (4.5%) control group participants received additional analgesia for breakthrough pain. All three subjects received a single dose of IV tramadol (50 mg/IV) on POD 1, and two patients required another single dose of IV tramadol (50 mg) on POD 2.
Secondary outcomes
Active ROM (knee flexion) was assessed by goniometer on the second postoperative day. Patients in the study group had increased active knee ROM (mean flexion 86.4° (SD 7.22)), and was found to be significantly better than the control group (mean flexion 73.86 (SD 7.88), mean difference = 12.54 with 95% CI 9.97 to 15.1; p = 0.017, independent-samples t-test).
Perioperative complications are summarized in Table III. In total, 19 patients in the study group (27.9%) and 12 patients in the control group (18.2%) experienced increased wound soakage requiring daily compression dressing. Overall, 19 (27.9%) patients in the study group and 17 (25.75%) patients in the control group experienced nausea requiring medication, however this was not statistically significant. No patient had any other wound-related complication or infection. No incidence of catheter breakage or becoming stuck in the knee joint was encountered. No patients in either group had complications associated with toxicity of the local anaesthetic (including blurred vision, chest pain, dizziness, syncope, peri-oral paraesthesias, acute onset confusion or delirium, and no documentation of cardiac arrhythmias).
Table III.
Immediate postoperative complications in study population.
| Complications, n (%) | Study group (n = 68) |
Control group (n = 66) |
p-value* |
|---|---|---|---|
| Nausea/vomiting | 19 (27.94) | 17 (25.75) | 0.343 |
| Breakthrough pain | 0 | 3 (4.5) | 0.451 |
| Opiate analgesia for breakthrough pain | Nil | Tramadol cumulative dose 2 patients - 100 mg 1 patient - 50 mg |
|
| Wound soakage | 19 (27.94) | 12 (18.18) | 0.301 |
-
*
Chi-squared test.
None of the trial participants, of either group, were documented to have surgical site infections (SSIs), periprosthetic joint infections (PJIs), complications related to treatment, or medical comorbidities in the first six months after surgery.
Discussion
This study demonstrated that combined single-shot ACB with intra-articular ropivacaine infusion was associated with a significant reduction in postoperative pain after primary TKA, in comparison to only single-shot ACB. Active knee ROM was significantly better in the study group.
Pain after TKA can cause dissatisfaction and negatively influence rehabilitation after surgery. Benefits of peripheral nerve blockade and its role in faster postoperative rehabilitation have been studied and widely reported. Multimodal analgesia is now the standard of care for analgesia after TKA. This includes pre-emptive analgesia, regional anaesthesia at the time of surgery followed by various options such as oral and IV analgesics, peripheral nerve blocks, and opiates.
Adductor canal blocks can be administered either as single-shot injections or by continuous adductor canal catheter infusions, and were introduced as ‘pure sensory’ nerve blocks without associated motor weakness. Single-shot adductor canal block has been established as an efficient source of pain control and improved rehabilitation.1,7 Compared to other available peripheral nerve blocks, such as the sciatic block or the femoral nerve block (FNB), ACB is associated with reduced motor deficits after surgery, thus aiding faster recovery and rehabilitation. Several reports support the use of ACB over FNB to avoid quadriceps weakness and reduce the time required to attain an independent ambulatory status.16-20 Toftdahl et al21 concluded that peri- and intra-articular analgesia following TKA has better analgesia and mobilization compared to continuous femoral nerve block.
Direct delivery of local anaesthetic agents into the joint after TKA is another established analgesic modality. Gomez-Cardero et al9 reported that use of ropivacaine infusion pumps was associated with improved postoperative pain scores and reduced opioid use. It also improved immediate functionality and patient comfort, resulting in reduced LOS without added complications. An earlier randomized, double-blinded, placebo-controlled study for IAC (using ropivacaine) versus epidural plus single-shot FNB by Reinhardt et al22 concluded that IAC is a safe and effective analgesic modality.
In their study, Andersen et al23 found that peri and intra-articular infusion of ropivacaine was associated with improved analgesia when compared to epidural infusions. Smith et al24 reported lower pain scores for patients receiving intra-articular bupivacaine infusion when compared to periarticular liposomal bupivacaine injection. Ikeuchi et al25 performed a double-blinded RCT to study the efficacy of local anaesthetic infusion (with steroid) after TKA, and reported significantly reduced pain in the group receiving local anaesthetic infusion via catheter. This study population received patient-controlled analgesia (PCA) as per institutional protocol, without use of peripheral nerve blockade after TKA.
In contrast, De-Weese et al26 found they had more use of breakthrough analgesia in group receiving continuous intra-articular bupivacaine compared with another group on epidural analgesia. Reeves and Skinner27 could not find any positive benefit of ropivacaine intra-articular infusion in their study.
A RCT by Beausang et al28 compared the independent use of ACB versus intra-articular local anaesthetic infusions, and showed the superiority of ACB in reducing pain and opiate consumption 24 hours after TKA. Dannana et al10 evaluated pain relief after TKA with ACB with periarticular infiltration of the knee, versus ACB combined with local infiltration and intra-articular ropivacaine boluses. They concluded that the additional use of intra-articular ropivacaine was associated with significant reduction in pain after surgery. Gurava Reddy et al29 performed a multicentre non-randomized study comparing continuous adductor-canal block by catheter versus local anaesthetic infusion by intra-articular catheter, with comparable pain relief with both analgesic methods.
Use of peripheral nerve blocks is not without complications. Feibel et al30 reported increased falls after surgery in patients receiving peripheral nerve blocks, especially continuous FNB. ACB has also been reported to result in motor weakness due to proximal spread of the local anaesthetic.30-33 However, this is a relatively rare complication. In this study, no patient experienced falls after surgery in the immediate postoperative period or during early follow-up.
The strengths of this study are its design (prospective, randomized, double-blinded, placebo-controlled), and the fact that the surgery performed by a single surgeon. The study was adequately powered to detect changes in the VAS pain scale, and there was a uniform analgesic protocol for management of postoperative pain.
The risk of introducing infection with IAC is minimal, and no study has reported any serious complications with IAC.8 The only disadvantage with IAC in our view is the additional cost and increased wound soakage.
A limitation of our study is that VAS pain scores were recorded with the patient at rest and not during active physical therapy. Further, there was a cumulative dose difference in local anaesthetic used between both the groups, however this was within the safe maximal-dose limits of ropivacaine. Further studies on optimal local anaesthetic drug dosage and duration of treatment are warranted.
In conclusion, combined single-shot ACB with intra-articular local anaesthetic infusion is effective in managing postoperative pain following TKA and promoting early rehabilitation of patients, without increasing the risk of complications. Further large volume trials are warranted to generate evidence on clinical significance on analgesia after TKA.
References
1. Sankineani SR , Reddy ARC , Eachempati KK , Jangale A , Gurava Reddy AV . Comparison of adductor Canal block and IPACK block (interspace between the popliteal artery and the capsule of the posterior knee) with adductor canal block alone after total knee arthroplasty: A prospective control trial on pain and knee function in immediate postoperative period . Eur J Orthop Surg Traumatol . 2018 ; 28 ( 7 ): 1391 – 1395 . Crossref PubMed Google Scholar
2. Gibbs DMR , Green TP , Esler CN . The local infiltration of analgesia following total knee replacement . J Bone Joint Surg Br . 2012 ; 94-B ( 9 ): 1154 – 1159 . Crossref PubMed Google Scholar
3. Cui Y , Yang T , Zeng C , et al. Intra-articular Bupivacaine after joint arthroplasty: A systematic review and meta-analysis of randomised placebo-controlled studies . BMJ Open . 2016 ; 6 ( 7 ): e011325 . Crossref PubMed Google Scholar
4. Kasture S , Saraf H . Epidural versus intra-articular infusion Analgesia following total knee replacement . J Orthop Surg (Hong Kong) . 2015 ; 23 ( 3 ): 287 – 289 . Crossref PubMed Google Scholar
5. Antoni M , Jenny JY , Noll E . Postoperative pain control by intra-articular local anesthesia versus femoral nerve block following total knee arthroplasty: Impact on discharge . Orthop Traumatol Surg Res . 2014 ; 100 ( 3 ): 313 – 316 . Crossref PubMed Google Scholar
6. Halawi MJ , Grant SA , Bolognesi MP . Multimodal analgesia for total joint arthroplasty . Orthopedics . 2015 ; 38 ( 7 ): e616 - 25 . Crossref PubMed Google Scholar
7. Beausang DH , Pozek J-P , Chen AF , et al. A randomized controlled trial comparing adductor canal catheter and intraarticular catheter after primary total knee arthroplasty . J Arthroplasty . 2016 ; 31 ( 9 Suppl ): 298 – 301 . Crossref PubMed Google Scholar
8. Andersen HL , Gyrn J , Møller L , Christensen B , Zaric D . Continuous saphenous nerve block as supplement to single-dose local infiltration analgesia for postoperative pain management after total knee arthroplasty . Reg Anesth Pain Med . 2013 ; 38 ( 2 ): 106 – 111 . Crossref PubMed Google Scholar
9. Gómez-Cardero P , Rodríguez-Merchán EC . Postoperative analgesia in TKA: ropivacaine continuous intraarticular infusion . Clin Orthop Relat Res . 2010 ; 468 ( 5 ): 1242 – 1247 . Crossref PubMed Google Scholar
10. Dannana CS , Apsingi S , Ponnala VK , Bollavaram VR , Boyapati G , Eachempati KK . Comparative study of the influence of adductor canal block plus multimodal periarticular infiltration versus combined adductor canal block, multimodal periarticular infiltration and intra-articular epidural catheter ropivacaine infiltration on pain relief after total knee arthroplasty: A prospective study . Musculoskelet Surg . 2020 ; 104 ( 2 ): 201 – 206 . Crossref PubMed Google Scholar
11. World Medical Association . World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects . JAMA . 2013 ; 310 ( 20 ): 2191 – 2194 . PubMed Google Scholar
12. Rosenberg PH , Veering BT , Urmey WF . Maximum Recommended doses of local anesthetics: A multifactorial concept . Reg Anesth Pain Med . 2004 ; 29 ( 6 ): 564 – 575 . Crossref PubMed Google Scholar
13. Myles PS , Myles DB , Galagher W , et al. Measuring acute postoperative pain using the visual analog scale: The minimal clinically important difference and patient acceptable symptom state . Br J Anaesth . 2017 ; 118 ( 3 ): 424 – 429 . Crossref PubMed Google Scholar
14. Kendrick DB , Strout TD . The minimum clinically significant difference in patient-assigned numeric scores for pain . Am J Emerg Med . 2005 ; 23 ( 7 ): 828 – 832 . Crossref PubMed Google Scholar
15. Schulz KF , Altman DG , Moher D , CONSORT Group . CONSORT 2010 statement: updated guidelines for reporting parallel group randomized trials . Ann Intern Med . 2010 ; 152 ( 11 ): 726 – 732 . Crossref PubMed Google Scholar
16. Jaeger P , Nielsen ZJK , Henningsen MH , Hilsted KL , Mathiesen O , Dahl JB . Adductor canal block versus femoral nerve block and quadriceps strength: A randomized, double-blind, placebo-controlled, crossover study in healthy volunteers . Anesthesiology . 2013 ; 118 ( 2 ): 409 – 415 . Crossref PubMed Google Scholar
17. Kwofie MK , Shastri UD , Gadsden JC , et al. The effects of ultrasound-guided adductor canal block versus femoral nerve block on quadriceps strength and fall risk: A blinded, randomized trial of volunteers . Reg Anesth Pain Med . 2013 ; 38 ( 4 ): 321 – 325 . Crossref PubMed Google Scholar
18. Kim DH , Lin Y , Goytizolo EA , et al. Adductor canal block versus femoral nerve block for total knee arthroplasty: A prospective, randomized, controlled trial . Anesthesiology . 2014 ; 120 ( 3 ): 540 – 550 . Crossref PubMed Google Scholar
19. Shah NA , Jain NP . Is continuous adductor canal block better than continuous femoral nerve block after total knee arthroplasty? Effect on ambulation ability, early functional recovery and pain control: A randomized controlled trial . J Arthroplasty . 2014 ; 29 ( 11 ): 2224 – 2229 . Crossref PubMed Google Scholar
20. Mudumbai SC , Kim TE , Howard SK , et al. Continuous adductor canal blocks are superior to continuous femoral nerve blocks in promoting early ambulation after TKA . Clin Orthop Relat Res . 2014 ; 472 ( 5 ): 1377 – 1383 . Crossref PubMed Google Scholar
21. Toftdahl K , Nikolajsen L , Haraldsted V , Madsen F , Tønnesen EK , Søballe K . Comparison of peri- and intraarticular analgesia with femoral nerve block after total knee arthroplasty: A randomized clinical trial . Acta Orthop . 2007 ; 78 ( 2 ): 172 – 179 . Crossref PubMed Google Scholar
22. Reinhardt KR , Duggal S , Umunna B-P , et al. Intraarticular analgesia versus epidural plus femoral nerve block after TKA: a randomized, double-blind trial . Clin Orthop Relat Res . 2014 ; 472 ( 5 ): 1400 – 1408 . Crossref PubMed Google Scholar
23. Andersen KV , Bak M , Christensen BV , Harazuk J , Pedersen NA , Søballe K . A randomized, controlled trial comparing local infiltration analgesia with epidural infusion for total knee arthroplasty . Acta Orthop . 2010 ; 81 ( 5 ): 606 – 610 . Crossref PubMed Google Scholar
24. Smith EB , Kazarian GS , Maltenfort MG , Lonner JH , Sharkey PF , Good RP . Periarticular Liposomal Bupivacaine Injection Versus Intra-Articular Bupivacaine Infusion Catheter for Analgesia After Total Knee Arthroplasty: A Double-Blinded, Randomized Controlled Trial . J Bone Joint Surg Am . 2017 ; 99-A ( 16 ): 1337 – 1344 . Crossref PubMed Google Scholar
25. Ikeuchi M , Kamimoto Y , Izumi M , et al. Local infusion analgesia using intra-articular double lumen catheter after total knee arthroplasty: A double blinded randomized control study . Knee Surg Sports Traumatol Arthrosc . 2013 ; 21 ( 12 ): 2680 – 2684 . Crossref PubMed Google Scholar
26. DeWeese FT , Akbari Z , Carline E . Pain control after knee arthroplasty: Intraarticular versus epidural anesthesia . Clin Orthop Relat Res . 2001 ; 392 : 226 – 231 . Crossref PubMed Google Scholar
27. Reeves M , Skinner MW . Continuous intra-articular infusion of ropivacaine after unilateral total knee arthroplasty . Anaesth Intensive Care . 2009 ; 37 ( 6 ): 918 – 922 . Crossref PubMed Google Scholar
28. Beausang DH , Pozek J-P , Chen AF , et al. A randomized controlled trial comparing adductor canal catheter and intraarticular catheter after primary total knee arthroplasty . J Arthroplasty . 2016 ; 31 ( 9 Suppl ): 298 – 301 . Crossref PubMed Google Scholar
29. Gurava Reddy AV , Manohar M , Shetty A , et al. A comparative study evaluating the role of adductor canal block catheter versus intraarticular analgesic infusion on knee pain and range of motion in the immediate postoperative period: A prospective multicenter trial . Musculoskelet Surg . 2020 ; 104 ( 3 ): 267 – 271 . Crossref PubMed Google Scholar
30. Feibel RJ , Dervin GF , Kim PR , Beaulé PE . Major complications associated with femoral nerve catheters for knee arthroplasty: A word of caution . J Arthroplasty . 2009 ; 24 ( 6 Suppl ): 132 – 137 . Crossref PubMed Google Scholar
31. Veal C , Auyong DB , Hanson NA , Allen CJ , Strodtbeck W . Delayed quadriceps weakness after continuous adductor canal block for total knee arthroplasty: A case report . Acta Anaesthesiol Scand . 2014 ; 58 ( 3 ): 362 – 364 . Crossref PubMed Google Scholar
32. Chen J , Lesser JB , Hadzic A , Reiss W , Resta-Flarer F . Adductor canal block can result in motor block of the quadriceps muscle . Reg Anesth Pain Med . 2014 ; 39 ( 2 ): 170 – 171 . Crossref PubMed Google Scholar
33. Gautier PE , Lecoq JP , Vandepitte C , Harstein G , Brichant JF . Impairment of sciatic nerve function during adductor canal block . Reg Anesth Pain Med . 2015 ; 40 ( 1 ): 85 – 89 . Crossref PubMed Google Scholar
Author contributions
K. Hippalgaonkar: Conceptualization, Investigation, Writing – review & editing.
V. Chandak: Investigation, Writing – original draft.
D. Daultani: Investigation, Writing – review & editing.
P. Mulpur: Writing – original draft, Writing – review & editing, Formal analysis.
K. K. Eachempati: Writing – review & editing.
A.V. Gurava Reddy: Writing – review & editing.
Funding statement
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
ICMJE COI statement
P. Mulpur reports an institutional grant from the Journal of Bone & Joint Surgery (Dr. Robert Bucholz Journal Club Grant 2020-2021), unrelated to this study.
Acknowledgements
We acknowledge the contribution of Dr. Khubchand Jhakotia (Consultant Anaesthesiologist).
Ethical review statement
This study was approved by the Institute Ethics Committee.
Open access funding
The authors confirm that the open access fee for this study was self-funded.
Follow P. Mulpur @PraharshaMulpur









