Abstract
Aims
An algorithm to determine the constitutional alignment of the lower limb once arthritic deformity has occurred would be of value when undertaking kinematically aligned total knee arthroplasty (TKA). The purpose of this study was to determine if the arithmetic hip-knee-ankle angle (aHKA) algorithm could estimate the constitutional alignment of the lower limb following development of significant arthritis.
Methods
A matched-pairs radiological study was undertaken comparing the aHKA of an osteoarthritic knee (aHKA-OA) with the mechanical HKA of the contralateral normal knee (mHKA-N). Patients with Grade 3 or 4 Kellgren-Lawrence tibiofemoral osteoarthritis in an arthritic knee undergoing TKA and Grade 0 or 1 osteoarthritis in the contralateral normal knee were included. The aHKA algorithm subtracts the lateral distal femoral angle (LDFA) from the medial proximal tibial angle (MPTA) measured on standing long leg radiographs. The primary outcome was the mean of the paired differences in the aHKA-OA and mHKA-N. Secondary outcomes included comparison of sex-based differences and capacity of the aHKA to determine the constitutional alignment based on degree of deformity.
Results
A total of 51 radiographs met the inclusion criteria. There was no significant difference between aHKA-OA and mHKA-N, with a mean angular difference of −0.4° (95% SE −0.8° to 0.1°; p = 0.16). There was no significant sex-based difference when comparing aHKA-OA and mHKA-N (mean difference 0.8°; p = 0.11). Knees with deformities of more than 8° had a greater mean difference between aHKA-OA and mHKA-N (1.3°) than those with lesser deformities (-0.1°; p = 0.009).
Conclusion
This study supports the arithmetic HKA algorithm for prediction of the constitutional alignment once arthritis has developed. The algorithm has similar accuracy between sexes and greater accuracy with lesser degrees of deformity.
Cite this article: Bone Joint Open 2020;1-7:339–345.
Clinical Relevance
-
With increased adoption of alignment strategies in TKA that aim to restore constitutional alignment, a method to predict this is required.
-
The arithmetic HKA algorithm provides an accurate method to determine constitutional alignment of the limb once arthritis and secondary deformity have occurred.
Introduction
Attempts to recreate the constitutional alignment of the lower limb have recently gained popularity in total knee arthroplasty (TKA) surgery. The technique, termed kinematic alignment, aims to restore constitutional knee alignment and soft tissue tension by preserving three-dimensional knee kinematics and maintaining collateral ligament balance through a range of movement. One component of this goal is achieved by restoring the hip-knee-ankle (HKA) angle and joint line obliquity by reconstruction of the native distal femoral and proximal tibial articular surface joint lines.1-3 There are conflicting results in the literature on whether this technique improves clinical outcomes.4-8 In addition, there is no consensus on ideal alignment boundaries among studies.2,4-9
It is now recognized that there is significant variability in constitutional lower limb alignment in healthy subjects.10 However, determination of constitutional alignment once arthritis has developed has proven to be more elusive. Various kinematic TKA techniques have been described that aim to achieve constitutional alignment using surrogate measures to reach this target. These include intraoperative estimation of pre-arthritic cartilage-bone composite thickness;2,9 use of preoperative radiological distal femoral and proximal tibial landmarks to guide resections via patient-specific templates or navigated techniques;3-7,11-13 intraoperative analysis of soft tissue laxities to guide navigated resection angles;13 or use of a combination of these methods. To date, no single method has been validated to accurately predict the constitutional lower limb alignment once arthritis has developed.
The purpose of this study was to determine if a newly described “arithmetic HKA” (aHKA) algorithm14 could predict the constitutional alignment of the lower limb following development of significant arthritis using the opposite, radiologically normal, limb as the comparator. The primary hypothesis was that the arithmetic HKA in the arthritic knee would be equivalent to the mechanical HKA in the opposite normal (non-arthritic) limb. If the aHKA could estimate the lower limb constitutional alignment prior to the onset of arthritis, this would support its clinical use by those surgeons wishing to perform kinematic alignment techniques in TKA.
Methods
Study design
We undertook a matched-pairs study using long leg alignment radiographs to compare the arithmetic HKA of an arthritic knee with the mechanical HKA of the contralateral normal knee serving as the control.
Study group
All radiographs were evaluated from an imaging database of patients who had undergone either unilateral unicompartmental or unilateral total knee arthroplasty for end-stage degenerative osteoarthritis between January 2016 and January 2018. Two orthopaedic surgeons (SJM, DBC) performed the surgeries at one private hospital in Sydney, Australia.
Inclusion criteria were knees with preoperative Grade 3 or 4 Kellgren-Lawrence tibiofemoral osteoarthritis, indicative of moderate or severe joint space loss. In addition, Grade 0 or I Kellgren-Lawrence changes, nil, or doubtful joint space loss had to have been present in the contralateral knee to serve as the normal comparator.15 Patients were excluded if they had a prior contralateral total or unicompartmental knee arthroplasty; if there were any extra-articular deformities of the femur or tibia; if the patient had undergone a prior femoral or tibial osteotomy; or if there were prior intra- or extra-articular fractures of the femur or tibia.
The inclusion of radiographs into the study was undertaken through a two-step process. An orthopaedic fellow performed the initial screening of all radiographs from the study period and included those that may be considered suitable. This set of radiographs was then reassessed, and agreement had to be reached between two observers in order for the radiograph to be included in the analysis.
Radiographic technique
Standing long leg radiographs that included the pelvis were taken in one radiology unit using the technique described by Paley16 (Figure 1a). Positioning was in the “stand-at-attention” position with both patellae facing forward. Three 430 mm cassettes were used to undertake the examination, and digital stitching was undertaken using the Philips Digital Diagnostics Software (Philips Healthcare, North Ryde, Australia). The tube-to-knee distance was approximately 250 cm. Kilovoltage settings varied between 70kV and 85kV per cassette.
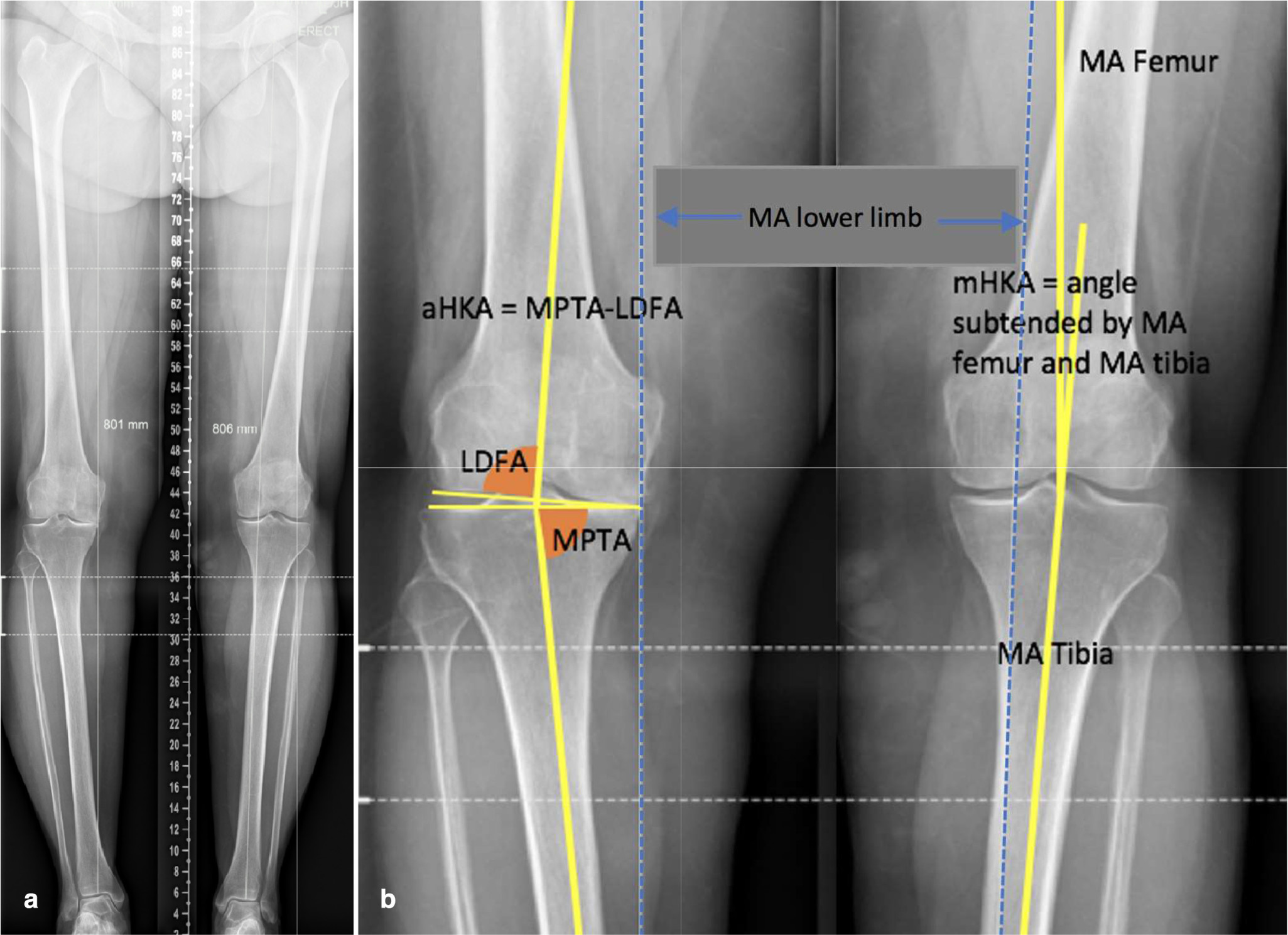
Fig. 1
a) Full preoperative long leg standing radiograph. Grade 4 Kellgren-Lawrence tibiofemoral osteoarthritis of right knee. Grade 1 tibiofemoral osteoarthritis left knee, serving as matched control. b) Same long leg radiograph with digital radiological reference lines. Right knee demonstrates calculation of constitutional alignment in the arthritic knee using aHKA algorithm. Left normal knee shows calculation of mHKA. aHKA, arithmetic hip-knee-ankle angle algorithm; LDFA, lateral distal femoral angle; MPTA, medial proximal tibial angle; mHKA, mechanical hip-knee-ankle angle; MA, mechanical axis.
All radiographs deemed suitable for inclusion were then evaluated for image quality. Appropriate rotational positioning was defined by the patella being positioned symmetrically facing forward; the lesser trochanters having a similar shape; and the proximal tibiofibular joints having similar overlap. In addition, significant fixed flexion deformity of the arthritic limb was assessed by noting asymmetry of the intercondylar outline. Radiographs were excluded if they were deemed to be poor quality due to patient positioning.
Radiographic analysis
The mechanical axis (MA) of the femur was defined as a line from the centre of the femoral head to the centre of the distal femur at the knee joint. The MA of the tibia was defined as a line at the midpoint of the tibia at the level of the knee joint to the centre of the tibial plafond at the ankle. The lateral distal femoral angle (LDFA) was defined as the lateral angle subtended by the MA of the femur and a line drawn across the articular surface of the distal femur at the most distal points of the lateral and medial femoral condyles. Similarly, the medial proximal tibial angle (MPTA) was defined as the angle subtended medially by the MA of the tibia and a line drawn between the most distal articular contours of the mid-points of the lateral and medial plateaus. The mechanical hip-knee-ankle angle (mHKA) was defined as the angular difference between the MA of the femur and MA of the tibia, with varus represented as a negative value and valgus as a positive value. Figure 1b demonstrates radiological landmarks for each knee. All measurements were performed by an orthopaedic fellow . A second observer (DBC) undertook a subgroup analysis of 15 patients, repeated at one-week intervals to assess for inter- and intra-observer agreement.
The arithmetic HKA algorithm
The arithmetic HKA was calculated by subtracting the LDFA from the MPTA14 (Figure 2). It ignores the joint line convergence angle (JLCA), which shows a slight convergence to the medial side of the knee of 0.51.10 For simplicity, as well as the fact that its value is considered to be within the margins of both measurement error and surgical resection error, it was ignored in the aHKA algorithm. Furthermore, it has been shown in a previous study not to be a significant contributing factor to overall lower limb alignment.10
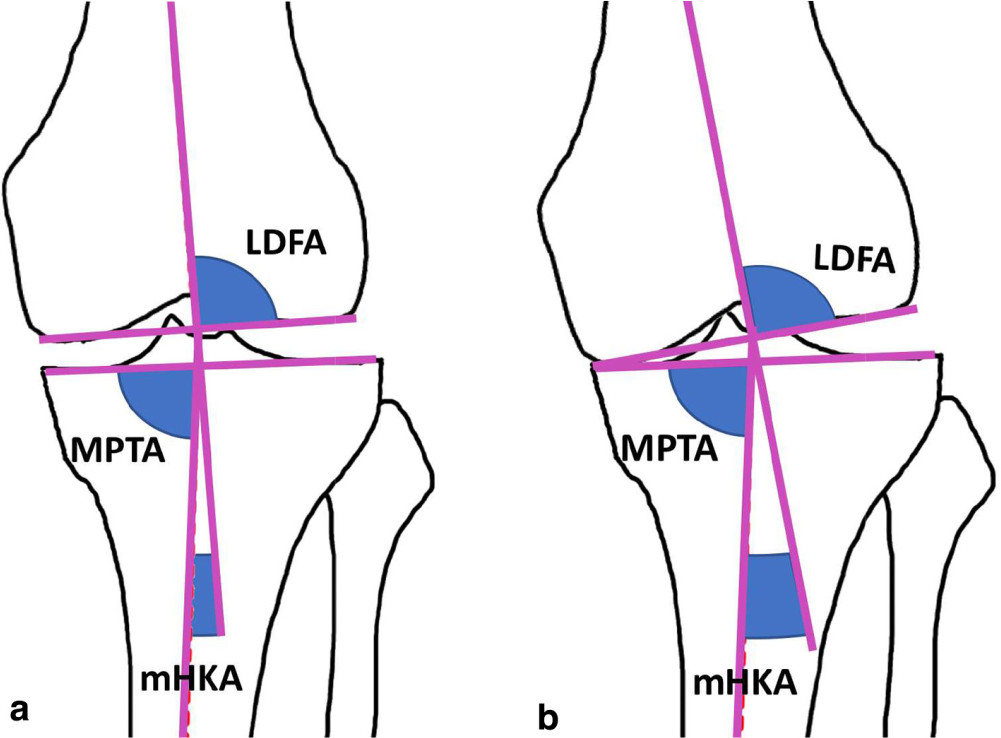
Fig. 2
Radiological changes that occur with joint space loss and deformity. a) LDFA, MPTA and mHKA in a knee with preserved joint space and mild constitutional varus alignment. b) The same knee following degenerative loss of medial joint space, showing a change in mHKA and no change to LDFA and MPTA (and therefore, no change to aHKA). mHKA, mechanical hip-knee-ankle angle; LDFA, lateral distal femoral angle; MPTA, medial proximal tibial angle.
Outcomes
The primary outcome was the mean of the paired differences between the arithmetic HKA of the arthritic knee (aHKA-OA) and the mechanical HKA of the normal knee (mHKA-N). The aHKA-OA was hypothesized to be predictive of the constitutional alignment of the lower limb, based on the mHKA of the non-affected side. Secondary outcomes included comparison of aHKA, mHKA, LDFA and MPTA between sexes. In addition, aHKA accuracy to determine the constitutional alignment with coronal deformities of greater than versus less than or equal to 8° from neutral alignment was assessed.
Sample size calculation
Our prior research found that the aHKA in the normal population (aHKA-N) is −0.9o of varus with a standard deviation (SD) of 2.5. It was felt that a mean difference of 1.5o or less between sides would be indicative of equivalence between mHKA-N and aHKA-OA on clinical grounds, as well as within the margin of error for radiological measures of knee alignment. Based on a maximum difference between groups of 1.5°, a power of 80%, and statistical significance of 5%, we required a minimum of 47 paired radiographs to determine if a true difference in alignment existed between sides.
Statistical analysis
Descriptive statistics were used for calculation of means, SD, and 95% confidence intervals. Paired t-tests were used for comparison of means between all other radiological alignment parameters assuming normality of distribution on Shapiro-Wilk’s test and Q-Q plots. Pearson’s r (r) and the coefficient of determination (R2) were calculated comparing mHKA-N and aHKA-OA. Independent two-tailed t-tests were used for analysis of mean differences in deformities greater and less than 8°, as well as differences between sexes. Intraclass correlation coefficients were used to assess inter-observer and intra-observer agreement using a two-way mixed-effects model with absolute agreement. Significance was set with a p-value < 0.05.
Results
Radiographs of 587 patients undergoing knee arthroplasty surgery in the study period were screened. Overall, 65 patients had radiographs that met the initial inclusion criteria based on arthritic disease in one knee and a normal contralateral knee. In all, 14 radiographs were excluded: nine due to rotational asymmetry; two due to the presence of prior femoral or tibial fractures resulting in extra-articular angular deformities; two due to the presence of significant asymmetrical lateral distal femoral valgus (most likely from juvenile physeal growth arrest), and one due to asymmetric anteroposterior radiological projectional differences because of a flexion contracture in the arthritic knee. Final analysis included 51 radiographs. Table I presents the demographics of the study group.
Table I.
Demographics of study group.
| Variable | Value |
|---|---|
| Mean age, (range) years | 69 (43 to 87) |
| Sex ratio (male:female) | 28:23 |
| Laterality of arthritic knee (left:right) | 28:23 |
| Mean height, cm | 170.3 |
| Mean weight, kg | 86.0 |
| Mean BMI | 29.6 |
-
cm = centimetres; kg = kilograms; BMI = body mass index
The mean mechanical HKA of the normal knee was −1.2° (SD 2.9°; range −8.2 to 5.9°) and the mean mechanical HKA of the arthritic knee was −4.6° (SD 5.2°; range −11.9 to 11.4°). There was a significant difference between male and female normal knees, with male knees having greater constitutional varus (mean −2.2°; SD 2.7°) than female knees (mean 0.0°; SD 2.8°). In addition, in both normal and arthritic limbs, female knees had greater valgus alignment than males with respect to LFDA. Females also had greater valgus alignment in normal limbs with respect to aHKA and mHKA (Table II). The aHKA of the normal limb was in slight valgus compared to the mechanical HKA of the normal limb, with some of this difference most likely caused by the JLCA, which may contribute approximately 0.5° more valgus to the aHKA.10
Table II.
Radiological parameters – all knees and differences between sexes.
| Variable (°) | All knees (n = 51), mean ± SD |
Male knees (n = 27), mean ± SD |
Female knees (n = 24), mean ± SD |
p-value between sexes |
|---|---|---|---|---|
| aHKA-OA (°) | −1.3 ± 3.2 | −2.2 ± 3.1 | −0.8 ± 3.3 | 0.11 |
| mHKA-OA (°) | −4.6 ± 5.2 | −5.5 ± 4.2 | −3.7 ± 6.1 | 0.21 |
| LDFA-OA (°) | 88.2 ± 2.6 | 89.0 ± 2.4 | 87.4 ± 2.7 | 0.02* |
| MPTA-OA (°) | 86.8 ± 2.6 | 86.9 ± 2.8 | 86.6 ± 2.4 | 0.75 |
| aHKA-N (°) | −0.5 ± 3.1 | −1.4 ± 3.1 | 0.6 ± 2.7 | 0.01* |
| mHKA-N (°) | −1.2 ± 2.9 | −2.2 ± 2.7 | 0.0 ± 2.8 | 0.005* |
| LDFA-N (°) | 87.5 ± 2.2 | 88.3 ± 2.0 | 86.6 ± 2.1 | 0.006* |
| MPTA-N (°) | 87.0 ± 2.2 | 86.9 ± 2.7 | 87.2 ± 1.5 | 0.60 |
-
*
significant p-values; minus values indicate varus.
-
OA = arthritic limb; N = normal limb; aHKA = arithmetic hip-knee-ankle angle; mHKA = mechanical hip-knee-ankle angle; LDFA = lateral distal femoral angle; MPTA = medial proximal tibial angle; SD= standard deviation
Primary outcome: aHKA-OA versus mHKA-N
Results showed no significant difference between aHKA-OA and mHKA-N, with a mean angular difference of −0.4° (95% SE −0.8 to 0.1°; paired t-test). In addition, aHKA-OA and mHKA-N were strongly positively correlated (r = 0.84, p < 0.001; R2 = 0.71 (Figure 3).
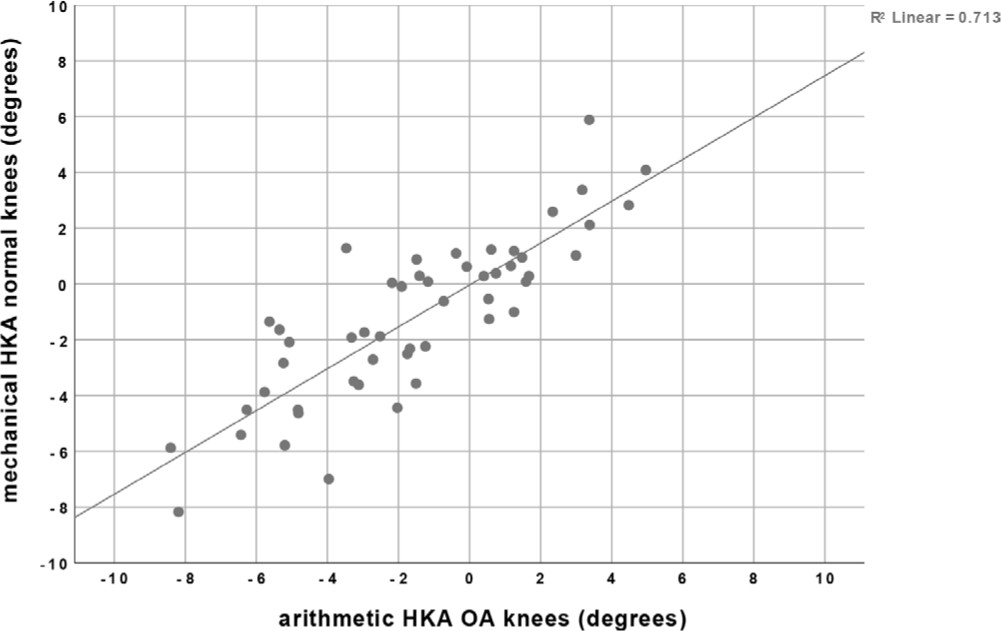
Fig. 3
Comparison of aHKA in the arthritic group versus mHKA in the normal group. HKA, hip-knee-ankle angle; mHKA, mechanical hip-knee-ankle angle; aHKA, arithmetic hip-knee-ankle angle; R2, coefficient of determination.
Differences between sexes
There was a trend for the aHKA to be in more valgus than the mHKA-N in females. However, the differences between sexes were small and not statistically significant (mean difference 0.8°, p = 0.11; independent samples t-test) (Table III).
Table III.
Primary outcome differences between aHKA-OA and mHKA-N.
| Variable (°) | Mean ± SD (°) | Range (°) | 95% CI (°) | p-value |
|---|---|---|---|---|
| aHKA-OA | −1.5 ± 3.3 | −8.4 to 5.0 | −2.5 to −0.6 | 0.16 (paired t-test) |
| mHKA-N | −1.2 ± 2.9 | −8.2 to 5.9 | −2.0 to −0.4 | |
| Mean difference overall | −0.4 ± 0.4 | N/A | −0.8 to 0.1 | N/A |
| Mean difference males |
0.0 ± 1.8 | −3.0 to 4.3 | −0.2 to 1.8 | 0.11 (independent samples t-test) |
| Mean difference females | 0.8 ± 1.7 | −1.7 to 4.8 |
-
aHKA-OA = arithmetic hip-knee-ankle angle of arthritic knees; mHKA-N = mechanical hip-knee-ankle angle of normal knees; SD = standard deviation; CI=confidence interval; N/A = not applicable
Relationship between severity of deformity and aHKA-OA prediction of mHKA-N
Knees with deformities greater than 8° (n = 15) had a greater mean difference between aHKA-OA and mHKA-N than those with deformities less than or equal to 8° (1.3° versus −0.1°; p = 0.009; 95% CI 0.4 to 2.4) (Table IV). There was no significant difference in variance between the two groups (Fisher’s F test; p = 0.375, 95% CI −0.5 to 5.5).
Table IV.
Analysis of difference between aHKA-OA and mHKA-N based on severity of deformity.
| Mean difference in aHKA-OA and mHKA-N± SD (°) | Range (°) | 95% CI (°) | p-value | |
|---|---|---|---|---|
| Deformity > 8° (n = 15) | 1.3 ± 1.9 | −3.0 to 4.8 | 0.3 to 2.4 | N/A |
| Deformity < 8° (n = 36) | −0.1 ± 1.6 | −2.4 to 4.3 | −0.6 to 0.5 | |
| Difference in means between groups | 1.4 | N/A | 0.4 to 2.4 | 0.009* |
-
aHKA-OA= arithmetic hip-knee-ankle angle of arthritic knees; mHKA-N = mechanical hip-knee-ankle angle of normal knees; SD= standard deviation; CI = SE interval; *= significant p-value; N/A = not applicable
Intra-observer and inter-observer agreement
Intra-observer agreement between measures one week apart was high, with an intraclass correlation coefficient of 0.95 (p < 0.0001) for Observer One and 0.97 (p < 0.0001) for Observer Two. Similarly, inter-observer agreement both at weeks one and two was high, with an intraclass correlation coefficient of 0.97 (p < 0.0001) and 0.95 (p < 0.0001) respectively.
Discussion
The purpose of this study was to validate the aHKA as an algorithm to predict the constitutional (pre-arthritic) alignment once significant arthritis has occurred. The study found that the aHKA in the arthritic knee was able to estimate the mechanical alignment in the contralateral normal knee within 0.4 of a degree. This result was within our pre-defined boundary of 1.5°, which was within the radiological measurement error range as well as within the surgical resection accuracy of TKA. Even in knees with preoperative arthritic deformity exceeding 8°, the predicted constitutional alignment still remained well within the accepted boundaries.
As surgical techniques in the field of knee arthroplasty evolve, it is increasingly recognized that attempting to restore the constitutional alignment may reduce the requirement for significant ligament balancing, and potentially return the soft tissue envelope to a more physiological state.1-3,8,13,17-19 Having a planning tool to determine the constitutional alignment prior to performing surgical resections of the distal femur and proximal tibia is valuable to surgeons aiming to restore the knee to its pre-arthritic alignment.
Cooke et al20 described a calculation of the mechanical alignment in normal knees using a combination of distal femoral, proximal tibial and condylar plateau angles. They did not apply their calculation to arthritic knees, nor use it to predict constitutional knee alignment. Several recent papers on kinematic alignment planning have used distal femoral and proximal tibial angles as a way to restore the native limb alignment.12,13 To date, however, we are unaware of a clearly defined and validated algorithm that can estimate the constitutional alignment once arthritis has intervened.
The aHKA algorithm had similar accuracy between males and females, although we noted a trend for the aHKA to be in slightly more valgus in females when compared to males, in whom the aHKA-OA and mHKA-N were more closely aligned. It is likely that this difference relates to the finding that female knees have a statistically smaller LDFA angle (greater distal femoral valgus) than males, when comparing this angle in both normal and arthritic knees between sexes. This finding was different to the results noted in the 2012 paper on normal knee alignment, where the MPTA was significantly different between sexes, but the LDFA was not.10
When looking at its capacity to determine the constitutional alignment in more advanced deformities, we found a greater mean difference between the aHKA of the arthritic knee compared to the mHKA-N of the normal knee. It is probable that the capacity of the arithmetic HKA to determine the constitutional alignment in more advanced states is slightly less. This makes intuitive sense, because when arthritis progresses, bone erosion may alter the landmarks for determination of the LFDA and MPTA, both of which are required for calculation of the aHKA. In addition, there is increased likelihood of joint flexion contractures, which may subtly alter the extension surface articular topography for landmark referencing, which will contribute to measurement error. The other consideration is that this difference may have been related to a sampling error, as there were only 15 patients who had deformities greater than 8°.
It is important to outline special considerations and limitations of the arithmetic HKA. Firstly, the calculation requires high-quality long leg radiographs with accurate stitching of cassettes. The benefit of this imaging modality is that it is less costly, has lower radiation dosing and is more readily available than calculated tomography. It also allows for weight-bearing assessment of limb deformity, as the algorithm references bony landmarks and is not affected by changes in joint space with weight-bearing. The arithmetic HKA has not been validated with biplanar lower limb radiography, computed tomography or magnetic resonance imaging, although it is possible that these more advanced imaging methods may offer increased accuracy by controlling for rotational and sagittal limb positioning issues that may increase measurement error. Secondly, the calculations in this study were performed using digital imaging, which has been found to be more accurate than manual templating on plain radiographs.21 Third, all patients with poor-quality imaging were excluded, and this needs to be considered when interpreting the results of the study and clinical applicability. It is critical that the clinician individually scrutinizes the quality of the imaging, and if this cannot be guaranteed, it should not be relied upon for calculation of the constitutional alignment. Fourth, variability between limbs has been reported in a CT-based analysis of individuals without skeletal abnormalities.22 Hence, using the opposite, non-arthritic side as an exemplar target for constitutional alignment restoration may not represent a perfect control in every case. Lastly, we arbitrarily set the boundary for deformity severity at 8°. This was done to ensure a sufficient number of patients for analysis in this range to allow some statistical inferences to occur. However, we do not know the accuracy at this stage with greater levels of deformity or with significant bone loss; hence, caution should be used when estimating the constitutional alignment with severe arthritic deformities or when bone loss is present.
The results of this study strongly support the use of the arithmetic HKA for prediction of the constitutional alignment in the arthritic knee. It has clinical applicability for those surgeons aiming to restore the constitutional lower limb alignment during TKA. The algorithm has similar accuracy between sexes and potentially greater accuracy with lesser degrees of deformity.
References
1. Howell SM , Howell SJ , Kuznik KT , Cohen J , Hull ML . Does a kinematically aligned total knee arthroplasty restore function without failure regardless of alignment category? Clin Orthop Relat Res . 2013 ; 471 ( 3 ): 1000 – 1007 . Crossref PubMed Google Scholar
2. Howell SM , Papadopoulos S , Kuznik KT , Hull ML . Accurate alignment and high function after kinematically aligned TKA performed with generic instruments . Knee Surg Sports Traumatol Arthrosc . 2013 ; 21 ( 10 ): 2271 – 2280 . Crossref PubMed Google Scholar
3. Hutt JR , LeBlanc MA , Masse V , Lavigne M , Vendittoli PA . Kinematic TKA using navigation: Surgical technique and initial results . Orthop Traumatol Surg Research . 2016 ; 102 ( 1 ): 99 – 104 . Crossref PubMed Google Scholar
4. Calliess T , Bauer K , Stukenborg-Colsman C , et al. PSI kinematic versus non-PSI mechanical alignment in total knee arthroplasty: a prospective, randomized study . Knee Surg Sports Traumatol Arthrosc . 2017 ; 25 ( 6 ): 1743 – 1748 . Crossref PubMed Google Scholar
5. Dossett HG , Swartz GJ , Estrada NA , LeFevre GW , Kwasman BG . Kinematically versus mechanically aligned total knee arthroplasty . Orthopedics . 2012 ; 35 ( 2 ): e160 – 169 . Crossref PubMed Google Scholar
6. Waterson HB , Clement ND , Eyres KS , Mandalia VI , Toms AD . The early outcome of kinematic versus mechanical alignment in total knee arthroplasty: A prospective randomised control trial . Bone Joint J . 2016 ; 98-B ( 10 ): 1360 – 1368 . Crossref PubMed Google Scholar
7. Young SW , Walker ML , Bayan A , et al. The Chitranjan S. Ranawat Award : No difference in 2-year functional outcomes using kinematic versus mechanical alignment in TKA: A randomized controlled clinical trial . Clin Orthop Relat Res . 2017 ; 475 ( 1 ): 9 – 20 . Crossref PubMed Google Scholar
8. McEwen P , Dlaska C , Jovanovic I , Doma K , Brandon B . Computer-assisted kinematic and mechanical axis total knee arthroplasty: A prospective randomized controlled trial of bilateral simultaneous surgery . J Arthroplasty . 2019 ; 35 ( 2 ): 443-450 . Crossref PubMed Google Scholar
9. Lee YS , Howell SM , Won YY , et al. Kinematic alignment is a possible alternative to mechanical alignment in total knee arthroplasty . Knee Surg Sports Traumatol Arthrosc . 2017 ; 25 ( 11 ): 3467 – 3479 . Crossref PubMed Google Scholar
10. Bellemans J , Colyn W , Vandenneucker H , Victor J . The Chitranjan Ranawat award: Is neutral mechanical alignment normal for all patients? The concept of constitutional varus . Clin Orthop Relat Res . 2012 ; 470 ( 1 ): 45 – 53 . Crossref PubMed Google Scholar
11. Hutt J , Masse V , Lavigne M , Vendittoli PA . Functional joint line obliquity after kinematic total knee arthroplasty . Int Orthop . 2016 ; 40 ( 1 ): 29 – 34 . Crossref PubMed Google Scholar
12. Almaawi AM , Hutt JRB , Masse V , Lavigne M , Vendittoli PA . The impact of mechanical and restricted kinematic alignment on knee anatomy in total knee arthroplasty . J Arthroplasty . 2017 ; 32 ( 7 ): 2133 – 2140 . Crossref PubMed Google Scholar
13. McEwen P , Balendra G , Doma K . Medial and lateral gap laxity differential in computer-assisted kinematic total knee arthroplasty . Bone Joint J . 2019 ; 101-B ( 3 ): 331 – 339 . Crossref PubMed Google Scholar
14. Griffiths-Jones WH , Chen DB , Han S , et al. Arithmetic HKA (aHKA): a novel algorithm for estimating constitutional lower limb alignment in the arthritic patient population . Submitted for publication to Bone Joint J . 2020 . Google Scholar
15. Kellgren JH , Lawrence JS . Radiological assessment of osteo-arthrosis . Ann Rheum Dis . 1957 ; 16 ( 4 ): 494 – 502 . Crossref PubMed Google Scholar
16. Paley D . Principles of deformity correction . Heidelberg, Germany : Springer-Verlag , 2003 . Google Scholar
17. Ji H-M , Han J , Jin DS , Seo H , Won Y-Y . Kinematically aligned TKA can align knee joint line to horizontal . Knee Surg Sports Traumatol Arthrosc . 2016 ; 24 ( 8 ): 2436 – 2441 . Crossref PubMed Google Scholar
18. Delport H , Labey L , Innocenti B , et al. Restoration of constitutional alignment in TKA leads to more physiological strains in the collateral ligaments . Knee Surg Sports Traumatol Arthrosc . 2015 ; 23 ( 8 ): 2159 – 2169 . Crossref PubMed Google Scholar
19. MacDessi SJ , Griffiths-Jones W , Chen DB , et al. Restoring the constitutional alignment with a restrictive kinematic protocol improves quantitative soft-tissue balance in total knee arthroplasty: A randomized controlled trial . Bone Joint J . 2020 ; 102-B ( 1 ): 117 – 124 . Crossref PubMed Google Scholar
20. Cooke TDV , Sled EA , Scudamore RA . Frontal plane knee alignment: a call for standardized measurement . J Rheumatol . 2007 ; 34 ( 9 ): 1796 – 1801 . PubMed Google Scholar
21. Goker B , Block JA . Improved precision in quantifying knee alignment angle . Clin Orthop Relat Res . 2007 ; 458 : 145 – 149 . Crossref PubMed Google Scholar
22. Eckhoff DG , Jacofsky DJ , Springer BD , et al. Bilateral Symmetrical Comparison of Femoral and Tibial Anatomic Features . J Arthroplasty . 2016 ; 31 ( 5 ): 1083 – 1090 . Crossref PubMed Google Scholar
Author contributions
S. J. MacDessi: Conceived and designed the study, Produced the manuscript, Analyzed the data, Gave final approval.
W. Griffiths-Jones: Designed the study, Produced the manuscript, Gave final approval.
I. A. Harris: Interpreted the data, Produced the manuscript, Gave final approval.
J. Bellemans: Produced the manuscript, Gave final approval.
D. B. Chen: Designed the study, Produced the manuscript, Gave final approval.
Funding statement
The author or one or more of the authors have received or will receive benefits for personal or professional use from a commercial party related directly or indirectly to the subject of this article. In addition, benefits have been or will be directed to a research fund, foundation, educational institution, or other non- profit organization with which one or more of the authors are associated.
ICMJE COI statement
J. Bellemans reports a patent application and IP pertaining to this study acquired by Stryker, which was obtained after the research was completed. D. Chen reports fellowship funding from Smith & Nephew and Zimmer Biomet, consulting fees from Amplitude, and a patent application and IP pertaining to this study acquired by Stryker, which was obtained after the research was completed. W. Griffiths-Jones also reports a patent application and IP pertaining to this study acquired by Stryker, which was obtained after the research was completed. S. E. MacDessi reports fellowship funding from Smith & Nephew and Zimmer Biomet, consulting fees from Amplitude, and a patent application and IP pertaining to this study acquired by Stryker, which was obtained after the research was completed.
Acknowledgements
We wish to acknowledge Dr Davide Salvo, Research Fellow, Sydney Knee Specialists, for performing radiographic measurements in this study. We are also sincerely appreciative of the efforts of Ms Jil Wood, MSN, Clinical Research Manager, Sydney Knee Specialists, for her role in editing and submission.
Ethical review statement
Ethics approval was obtained to conduct this study (Hunter New England Local Health District, Approval Number: EX201905-01).
© 2020 Author(s) et al. This is an open-access article distributed under the terms of the Creative Commons Attributions licence (CC-BY-NC-ND), which permits unrestricted use, distribution, and reproduction in any medium, but not for commercial gain, provided the original author and source are credited.









