Abstract
Aims
Complex total hip arthroplasty (THA) with subtrochanteric shortening osteotomy is necessary in conditions other than developmental dysplasia of the hip (DDH) and septic arthritis sequelae with significant proximal femur migration. Our aim was to evaluate the hip centre restoration with THAs in these hips.
Methods
In all, 27 THAs in 25 patients requiring THA with femoral shortening between 2012 and 2019 were assessed. Bilateral shortening was required in two patients. Subtrochanteric shortening was required in 14 out of 27 hips (51.9%) with aetiology other than DDH or septic arthritis. Vertical centre of rotation (VCOR), horizontal centre of rotation, offset, and functional outcome was calculated. The mean followup was 24.4 months (5 to 92 months).
Results
The mean VCOR was 17.43 mm (9.5 to 27 mm) and horizontal centre of rotation (HCOR) was 24.79 mm (17.2 to 37.6 mm). Dislocation at three months following acetabulum reconstruction required femoral shortening for offset correction and hip centre restoration in one hip. Mean horizontal offset was 39.72 (32.7 to 48.2 mm) compared to 42.89 (26.7 to 50.6 mm) on the normal side. Mean Harris Hip Score (HHS) of 22.64 (14 to 35) improved to 79.43 (68 to 92). Mean pre-operative shortening was 3.95 cm (2 to 8 cm). Residual limb length discrepancy was 1.5 cm (0 to 2 cm). Sciatic neuropraxia in two patients recovered by six months, and femoral neuropraxia in one hip recovered by 12 months. Mean Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) was 13.92 (9 to 19). Mean 12-item short form survey (SF-12) physical scores of 50.6 and mental of 60.12 were obtained.
Conclusion
THA with subtrochanteric shortening is valuable in complex hips with high dislocation. The restoration of the hip centre of rotation and offset is important in these hips.
Level of evidence IV
-
Femoral shortening useful in conditions other than DDH and septic sequelae.
-
Restoration of hip centre combined with offset to be planned and ensured.
Introduction
Total hip arthroplasty (THA) with femoral shortening is essential in the adult hip with high dislocation developmental dysplasia of the hip (DDH) for long-term successful outcome.1-4 Septic arthritis sequelae in the adult hip is one of the etiological factors other than DDH with significant proximal migration of the hip centre requiring femoral shortening at THA.5-8 Long term results of sub trochanteric shortening with THA in management of childhood pyogenic arthritis with hip centre restoration have also been described.9,10 Pre-operative planning includes templating with assessment of the acetabulum and proximal femur prior to extensive soft tissue release combined with proximal femur shortening to restore the centre of rotation of the hip.2,3,11,12
Proximal femur migration at THA can also be associated with post-traumatic sequelae, long-standing inflammatory arthritis with protrusio among other causes. THA in these hips are challenging and would require extensive soft tissue release with subtrochanteric osteotomy for restoration of the hip centre to achieve a stable hip with good functional outcome. Femoral shortening performed at revision hip arthroplasty been reported.13
Adequate preoperative planning is essential for THA in complex hip arthroplasty. The extensive soft tissue release and identification of the true acetabulum is critical in placement of the acetabular component at the normal hip centre. The dysplastic acetabulum requires small acetabular components. The proximal femur changes require modular implants with provision for version adjustment. Femoral proximal migration with the lesser trochanter at or above the level of the tear drop would require a subtrochanteric shortening to restore the hip centre of rotation.
Subtrochanteric osteotomy at THA with hip centre restoration for causes other than DDH, septic arthritis sequelae, and revision arthroplasty have not been described. We realized that this is an effective procedure in complex THA to achieve stable reduction with hip centre restoration.
We collected data on our patients who underwent femoral shortening at THA. Our goal was to avoid a high hip centre in these complex hips. Informed consent was taken from all patients. Institutional review board approval was obtained for this study. The aim of this study was to analyze data regarding the restoration of hip centre of rotation in these patients.
Methods
In all, 27 hips in 25 patients had subtrochanteric femoral shortening with THA at our unit from 2012 to 2019. Bilateral femoral shortening was required in two patients. Data was collected from the medical records, last hospital visit and telephonic review. There were 15 females and ten males with age 16 years to 63 years (mean 33.4 years). Subtrochanteric shortening was required in 14 out of 27 hips (51.9%) with aetiology other than DDH and septic arthritis sequelae. The mean follow-up was 24.4 months (5 to 92 months). The complex hips requiring THAs in these series were due to delayed presentation in various hip disorders with associated bony and soft tissue changes. The distribution is given in Table I.
Table I.
Diagnosis at THA with femoral shortening 27 hips in 25 patients with proximal femur migration (high hip).
| Diagnosis | Number of hips |
|---|---|
| DDH | 7 (including 1 bilateral) |
| Septic arthritis sequelae > 10 yrs | 6 |
| Other | |
| Acetabulum defects Type 3a Post-traumatic - 2, revision -1 |
3 |
| Type 3 b RA -3(including bilateral -1), AS - 1 |
4 (including 1 bilateral) |
| Childhood arthritis | 3 |
| Revision THA | 2 |
| Excision arthroplasty > 20 yrs | 1 |
| Trauma neglected | 1 |
-
RA, rheumatoid arthritis; THA, total hip arthroplasty.
Pre-operative templating was done in all cases to evaluate the acetabulum and the proximal femur. Proximal migration of the femur with the level of the lesser trochanter at or above the level of the inter tear drop line would include planning for a sub trochanteric femoral shortening. The acetabular and femoral sizes were assessed along with the plan for the osteotomy level. CT scans with 3D reconstruction were analyzed to assess the anterior, posterior, and superior acetabular bone stock to enable planning for bone graft or acetabular augmentation as required. The CT and radiological findings regarding the proximal femur anatomy was also evaluated.
The extensile posterior approach with gluteus maximus release was used for all the hips. Femoral soft tissue release included release of the gluteus maximus, the contracted anterior and posterior capsular tissue sparing the iliopsoas. Circumferential release of the acetabular attachment of the anterior and posterior capsule was carried out. Acetabular implantation was done after defining the native hip margins and using the best fit component with maximum host bone preservation and contact.
Cementless modular femoral stems (SROM; Depuy Synthes, Warsaw, Indiana, USA) was used in all hips. The proximal and distal canal preparation was done prior to the osteotomy. Extensive femoral soft tissue release without compromising the abductors failed to achieve trial reduction in all the hips. Subtrochanteric osteotomy was carried out just distal to the inferior margin of the trial sleeve component to achieve good final rotational stability with the distal femoral component. The overlap of the fragments with traction was measured after achieving reduction with the trial implant in the proximal fragment before bony resection. Stable reduction was achieved after mean shortening of 1.48 cm (1 to 2.5 cm). The preparation of the proximal femur resulted in cortical thinning and occasional fractures at implantation of the proximal component. The reduced bone stock in the proximal femur in these hips was probably due to the offloading with longstanding hip abnormality. Four hips with such incomplete fractures in the proximal femur required wire fixation for additional stability.
The distal femur canal size was assessed at completion of osteotomy. This ensured optimal canal sizing, fit and good stability at the subtrochanteric osteotomy. Plate fixation was required in six hips for additional rotational stability at the osteotomy. Available cancellous bone and cortical chips were used at the site of osteotomy to aid union.14 The hip stability assessed intraoperatively and an adductor tenotomy performed in 15 hips. Protected weightbearing was advised for almost six to eight months. Follow-up radiograph assessment was done with advise on progressive weightbearing depending on clinical and radiological union.
The anteroposterior view of the hips were studied to assess the acetabular inclination, implant position, and union at site of osteotomy. The vertical centre of rotation (VCOR) was measured from the femoral head centre to the inter tear drop line. A perpendicular line depicting the horizontal distance of the head centre to the bottom of the tear drop was measured to depict the horizontal centre of rotation (HCOR).15,16 The horizontal offset, combined offset (measured from tear drop to femoral axis) and the vertical offset was also calculated. All measurements were done by a radiologist with the GE (General Electric) Picture Archiving and Communication System (PACS). The distribution of the values was done using Stata Version 11 software. All the measurements made were tabulated and the values obtained for this descriptive analysis. The functional outcome was obtained using the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) questionnaire, and the 12-item short form survey (SF-12) score with the physical and mental components. Pain, stiffness, and physical activity were scored separately as part of the WOMAC assessment.
Results
The mean vertical centre of rotation (VCOR) was 17.43 mm (9.5 to 27 mm). The VCOR on the contralateral normal 17 hips was 14.44 mm (9 to 25.9 mm). The distribution of the VCOR in the two groups is seen in Figure 1.
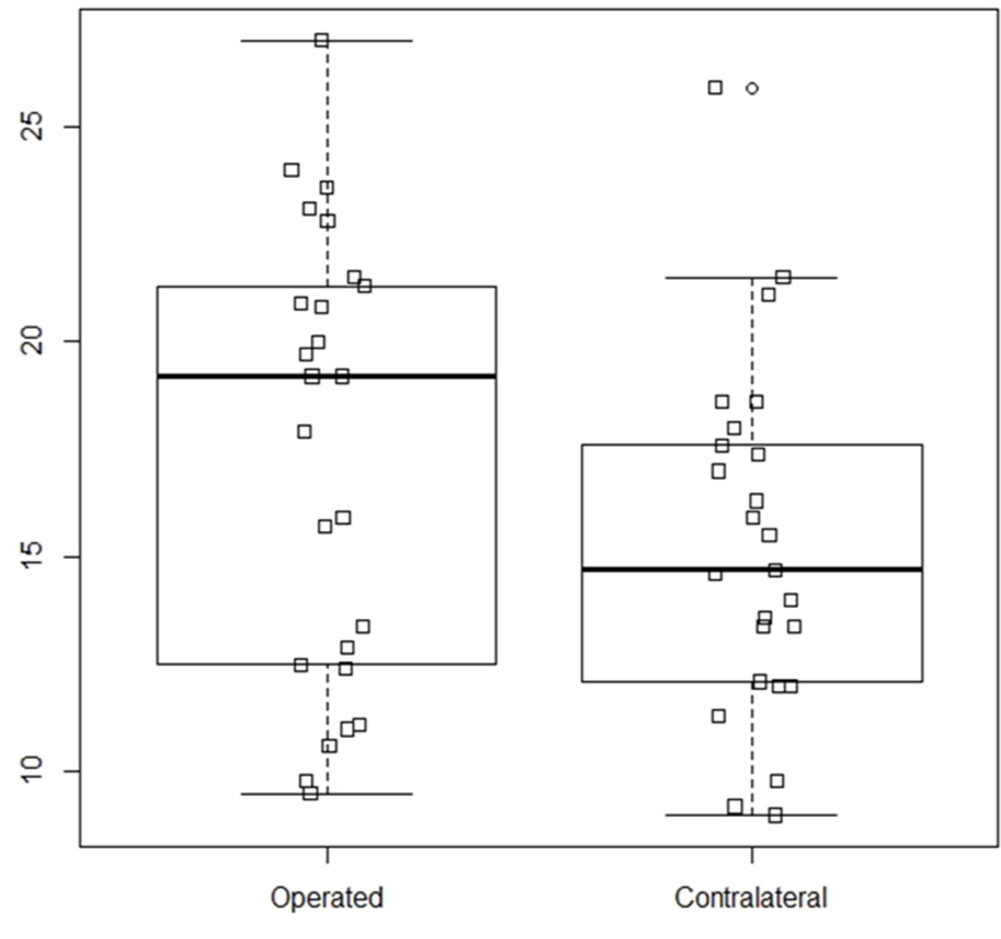
Fig. 1
Distribution of the vertical centre of rotation (VCOR) in the two groups; operated and contralateral (normal).
Overall, seven of 25 patients had bilateral THA. The hip centre in the 17 hips were considered for the normal group as 1 contralateral hip had femoral head deformity due to childhood arthritis. These 17 hips had no anatomical abnormality. The mean horizontal centre of rotation HCOR) for the THAs was 24.79 mm (7.2 to 37.6 mm) and the HCOR for the the 17 normal contralateral hips was 29.09 (25.2 to 35.5 mm). Two hips had undisplaced fracture of the thin medial acetabular wall with no compromise of the cementless component fixation. The HCOR was medialized under 10 mm in both these hips.
The vertical hip centre did not exceed 35 mm from the inter tear drop line in all our hips. The mean size of the acetabular component was 47 mm (38 to 58 mm). Acetabular component inclination was measured on the anteroposterior radiograph as described earlier.17 The mean acetabular inclination was 45.97° (40.6° to 53.8°). Screws were used to supplement acetabular component fixation in 13 hips, and two hips required no screws. Bone graft with additional screw fixation were required in nine hips; three hips with acetabular defects required acetabular augments (two posterosuperior buttress augment, and one medial augment). Acetabulum components were cemented in a 63-year-old female with bilateral Crowe 4 dysplasia. The right hip required acetabular augmentation with autogenous bone graft and screw fixation.
Furthermore, three patients with staged revision THA required femoral shortening. One patient presented 15 months after stage one revision with spacer for revision surgery with significant proximal migration of the femur. Revision THA with a cementless acetabulum component supported by a posterosuperior buttress augment for a type 3a defect. Stable reduction was achieved without femoral shortening after extensive soft tissue release. The hip dislocated three months later due to impingement resulting from reduced offset. Femoral shortening with restoration of the lateral offset was required to achieve a stable reduction. The femoral implant had to be changed to calcar arthroplasty (Calcar Neck + 21,SROM,Depuy,USA) in order to restore the corrected offset resulting in a good functional hip at 46 months (Figure 2 a-c). The horizontal offset improved from 10.5 mm to 32.7 mm and the vertical offset increased from 23.7 mm to 58.6 mm. We analyzed that shortening could have been carried out at acetabular reconstruction for similar proximal hip migration after extensive soft tissue release in long-standing hip disorders at THA. Inadequate offset and subsequent impingement could be missed in these complex procedures. The restoration of offset with potential impingement needs to be verified at trial reduction after acetabular reconstruction. Reduction of the hip, restoration of the offset, and stable ROM without impingement would be possible after extensive releases and femoral shortening osteotomy in these reconstructive procedures. The mean postop horizontal offset of 39.72 mm (32.7 to 48.2 mm) matched 42.89 mm (26.7 to 50.6 mm) for the 17 normal hips. Mean vertical offset of 51.74 mm (29.1 to 75.6 mm) compared to 51.9 mm (range 39 to 64.3 mm). The mean postoperative global offset was 65.15 mm (range 52 to 87.1 mm) equated with 77.89 mm (55.2 to 103 mm) in the normal. The hips with protrusio requiring bone grafting did not have significant lateralization in the horizontal offset (< 10 mm compared to the normal side).

Fig. 2
(a) 41-year-old male with septic loosening , one year and four months postoperatively stage 1 revision THA with proximal migration and type 3a acetabular deficiency. (b) Postoperative acetabular reconstruction for type 3a defect with posterosuperior buttress augment and acetabulumcomponent with SROM femur, reduction stable at final reduction with extensive soft tissue release, dislocation three months postoperatively due to reduced offset causing impingement (c) Postoperative femoral shortening with femoral component changed to calcar replacement CR SROM (DePuy, USA) with restoration of offset (horizontal offset correction 10.5 mm to 32.7 mm (vertical offset 23.7 mm to 58.6 mm); four-year postoperatively showing componentnand augment well fixed with femoral component and osteotomy union.
The mean Harris Hip Score (HHS) of 22.64 (14 to 35) improved to 79.43 (68 to 92). Three patients with bilateral hip disease were significantly incapacitated prior to surgery. The involvement of the other joints in RA, and contralateral hip involvement also contributed to outcome scores at review. All patients had associated back pain with limp prior to the THA. The patient with a malunited acetabular fracture underwent a staged THA due to infection also had a foot drop from the index trauma. He is awaiting a tendon transfer to improve his overall outcome. Two patients with rheumatoid arthritis (RA) and one male with ankylosing spondylitis (AS) are continuing their medical treatment. The RA patients have functional limitations due to involvement of the other joints as well.
Functional outcome at last review was done using WOMAC questionnaire and SF-12. The mean WOMAC score of 13.92 (9 to 19) was obtained. Individual components assessed revealed a mean pain score of 1.2 (0 to 2), mean stiffness score of 0.16 (0 to 1), and, mean Physical activity score of 12.56 (range 9 to 16). SF 12 survey instrument was used for functional outcome for both physical and mental components. The physical score (PS) was mean 50.6 (37 to 56) and the mental score (MS) was mean 60.12 (57 to 64).
All patients had moderate discomfort or pain at the site of femoral shortening for a few weeks which gradually subsided. The osteotomy had united in all cases with no lysis around the acetabulum or the femoral components on the xrays reviewed at last followup . The 63-year-old female with bilateral neglected DDH underwent left knee constrained TKA for fixed valgus OA and is currently using a walking aid for ambulation. 21/25 patients could walk and climb stairs comfortably with no pain or discomfort, while the remaining four had some discomfort on walking for long distances. The longstanding proximal migration with restoration of the hip centre at THA could result in considerable time taken for the abductor and hip muscle strength to be restored. This improvement in muscle strength occurs gradually to result in a long standing stable hip.2,3,11 The mild residual limp is probably due to the minimal abductor weakness seen at review. There was significant improvement in overall function as indicated by their functional scores.
The mean preoperative shortening was 3.95 cm (2 to 8 cm) in 21 patients as two individuals had bilateral hip involvement. The limb length discrepancy at postoperative assessment was 1.5 cm (0 to 2 cm). Sciatic nerve neuropraxia was seen in 2 patients which recovered by six months. In additon, one patient with femoral nerve neuropraxia manifested as quadriceps weakness ,which recovered by 12 months. There were no postoperative infections or dislocations after femoral shortening with THA in our series.
Discussion
Proximal femur migration with high hip centre are seen in conditions similar to septic arthritis sequelae and DDH. THA in these hips need restoration of the hip centre. The extensive soft tissue releases and subsequent femoral shortening to establish the hip centre is challenging in these high hips with delayed presentation. The changes with the DDH sequelae have been well described. These patients typically have shortening, limp and onset of back pain. Radiological findings include a significantly proximally migrated hip with a poorly developed anatomy of the proximal femur and acetabulum. THA restores the anatomical hip centre and provides a stable hip with good longterm survivorship.2,11 An extensive soft tissue release sparing the abductors is required to mobilize the proximal femur. Acetabular component placement at 35 mm or more from the inter-tear drop line is associated with altered joint reaction forces leading to complications and compromised outcome.15,18-22 Femoral subtrochanteric shortening osteotomy would be useful in avoiding a high hip centre and restoration of the anatomical centre of rotation.
RA and AS with protrusio (Figure 3, 4, 5) requires significant soft tissue release combined with femoral shortening at THA. Childhood dislocation with delayed presentation for definitive treatment is demanding (Figure 6). Delayed presentation after complex hip trauma and excision arthroplasty presenting for THA are complex procedures. Fibrosis with soft tissue scarring pose significant challenges especially in posttraumatic sequelae and infection (Figure 7). These difficult hips require extensive releases and shortening to restore the centre of rotation.

Fig. 3
21-year-old female with juvenile rheumatoid arthritis with bilateral type 3b acetabulum defect with 'for review only' protrusio, bilateral femoral shortening with plate for right femur for additional stability, and SS wiring for the proximal fragment for intraoperative split. Acetabulum impaction grafting with femoral head blocks, restored centre of rotation. 36-month follow-up with implant position well maintained and osteotomy site well united bilaterally. Acetabulum graft well incorporated. The combined offset measures 72.2 mm left and 72.8 mm right; the horizontal offset was 35.3 mm and 41.1 mm respectively without significant lateralization.
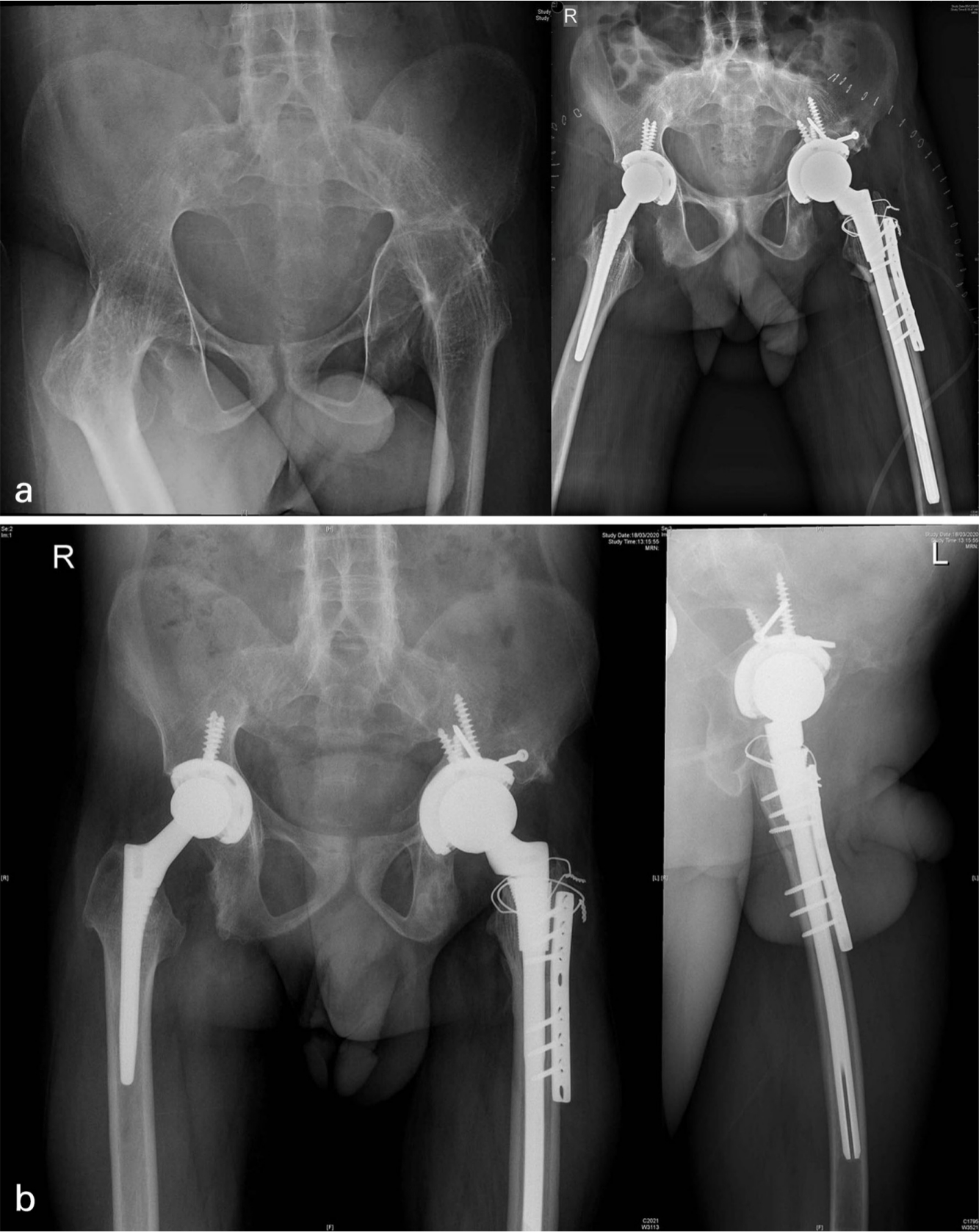
Fig. 4
(a) 31-year-old male with bilateral fused hips and ankylosing spondylitis. Proximal migration of the left hipwith femoral head and acetabular type 3b acetabular deficiency, bilateral THA with left hip femoral shortening. Acetabulum medial wall fracture, defect managed with bone graft and screws for superioraugmentation. SS wire for proximal femur incomplete split, femur plate for additional rotational stability. (b) 15-month follow-up with osteotomy site union, acetabulum graft well united. Lateral view confirming osteotomy site union and component femur position.

Fig. 5
36-year-old male with RA and Rt protrusio. Autografting acetabulum and component without significant lateralization and shortening with THA . Three months postoperative showing good union progress at osteotomy site.Right hip postop global offset 71 mm compared to 69.4 mm, horizontal offset 35.3 mm compared to 41.1 mm onthe contralateral side indicating hip not lateralized significantly. Pt is doing well at two years.

Fig. 6
49-year-old male with childhood arthritis sequelae with 5 cm shortening, eight months postoperative THA with extensive release, 42 mm acetabular component, femoral shortening signs of osteotomy site union.
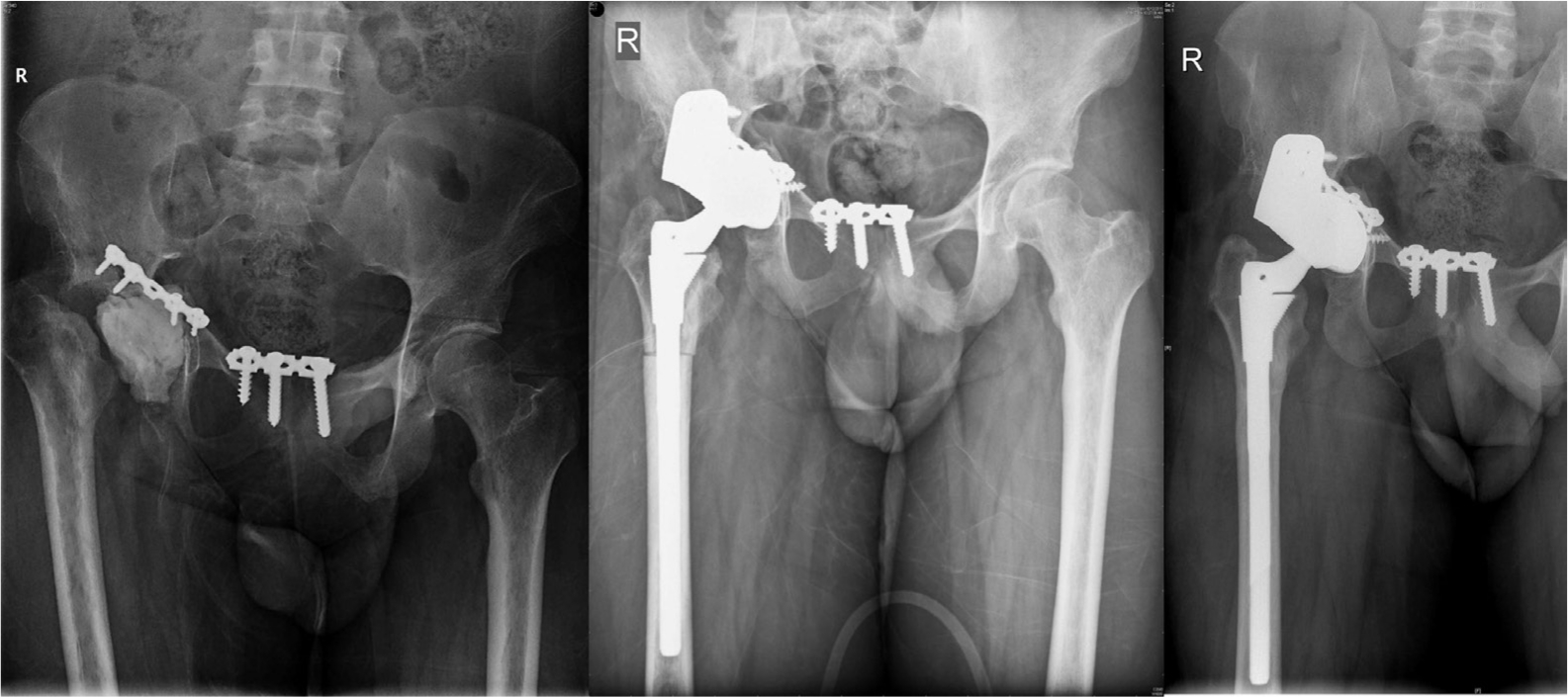
Fig. 7
19-year-old male with post-trauma surgery infection treated with spacer, augment for acetabular defect type 3 defect, femoral shortening with THA, two-year follow-up x-ray with osteotomy and acetabular fracture union, doing well at four years four months.
Delayed presentation of complex acetabular fractures with bone defects and prior infection is challenging as it requires hip centre restoration to provide a stable hip. Post-traumatic sequelae, long-standing protrusio, fused hips with proximal migration are few conditions requiring a sub trochanteric shortening osteotomy for restoring the centre of rotation. Delayed presentation of protrusio, ankylosed hips seen with rheumatoid arthritis and ankylosing spondylitis among the inflammatory polyarthritis and spondyloarthropathy disorders that require restoration of the hip centre with subtrochanteric osteotomy. Our series required femoral shortening in 14/27 hips (51.9%) with proximal femoral migration for causes other than DDH and septic arthritis. The revision THA that presented with dislocation two months after reconstruction underwent femoral shortening to correct the impingement due to reduced vertical and horizontal offset. Restoration of offset is an essential step in reconstruction during primary complex THA with significant proximal femur migration. Pre-operative planning includes templating and assessment of proximal femur migration. Radiological finding of the lesser trochanter seen at or above the level of the tear drop needs preparation for femoral shortening if the restoration of hip centre is not possible with extensive soft tissue release. The sequence of extensive soft tissue needs to be combined with femoral shortening to achieve a stable reduction, ROM, restoration of offset and avoidance of impingement. Data regarding shortening at THA for AS, RA and post-traumatic sequelae is limited. The technique is particularly useful in delayed presentation and sequelae related to such conditions. The restoration of the vertical centre of rotation and offset in these hips as shown in our series ensures near normal anatomy with a stable hip joint.
Reconstructive THA especially in high dislocations should ideally achieve restoration of the hip centre with offset. The establishment of normal joint and soft tissue anatomy ensures good ROM with stability. Femoral shortening with extensive soft tissue release is a useful technique in these challenging situations to achieve stable reduction with good functional outcome.
The mean follow-up in our series is 24 months (5 to 92 months). Mean HHS of 79.43 (68 to 92) at review is similar to the threshold values described.23 The functional outcome with WOMAC and SF 12 at last review indicates good overall mental and physical outcome in these complex hips. This is a significant limitation regarding the lack of uniform long term follow-up data in this series. Our series had 14 out of 27 hips (51.9%) with aetiology other than DDH and septic arthritis sequelae. We found this technique valuable in difficult complex THAs as described in our series. The number of hips in each group is small. Long-term follow-up with more numbers would add more value to future data analysis.
Conclusion
Femoral shortening after extensive soft tissue release could be required in complex primary THA with long standing high hip centre. This technique is useful in difficult complex hip arthroplasty with significant proximal migration of the femur to restore the hip centre of rotation. The restoration of the offset combined with hip centre restoration is essential in achieving a stable hip in these complex THAs with good functional outcome.
References
1. Rollo G , Solarino G , Vicenti G , et al. Subtrochanteric femoral shortening osteotomy combined with cementless total hip replacement for Crowe type IV developmental dysplasia: a retrospective study . J Orthop Traumatol . 2017 ; 18 ( 4 ): 407 – 413 . Crossref PubMed Google Scholar
2. Zeng W-N , Liu J-L , Wang F-Y , et al. Total hip arthroplasty for patients with Crowe type IV developmental dysplasia of the hip: ten years results . Int J Surg . 2017 ; 42 : 17 – 21 . Crossref PubMed Google Scholar
3. Yasgur DJ , Stuchin SA , Adler EM , DiCesare PE . Subtrochanteric femoral shortening osteotomy in total hip arthroplasty for high-riding developmental dislocation of the hip . J Arthroplasty . 1997 ; 12 ( 8 ): 880 – 888 . Crossref PubMed Google Scholar
4. Greber EM , Pelt CE , Gililland JM , et al. Challenges in total hip arthroplasty in the setting of developmental dysplasia of the hip . J Arthroplasty . 2017 ; 32 ( 9S ): S38 – S44 . Crossref PubMed Google Scholar
5. Zeng W-N , Liu J-L , Jia X-L , et al. Midterm results of total hip arthroplasty in patients with high hip dislocation after suppurative hip arthritis . J Arthroplasty . 2019 ; 34 ( 1 ): 102 – 107 . Crossref PubMed Google Scholar
6. Kim Y-H , Seo H-S , Kim J-S . Outcomes after THA in patients with high hip dislocation after childhood sepsis . Clin Orthop Relat Res . 2009 ; 467 ( 9 ): 2371 – 2378 . Crossref PubMed Google Scholar
7. Yang Y , Yu Qiu-Ping , Wang Shao-Lin , Yu Q-P , Wang S-L , et al. Outcomes after total hip arthroplasty using a Cementless S-ROM modular stem for patients with high hip dislocation secondary to hip pyogenic arthritis . Orthop Surg . 2019 ; 11 ( 3 ): 460 – 466 . Crossref PubMed Google Scholar
8. Gao X , He R-xin , Yan S-gui , He R , Yan S . Total hip arthroplasty for patients with osteoarthritis secondary to hip pyogenic infection . Chin Med J . 2010 ; 123 ( 2 ): 156 – 159 . PubMed Google Scholar
9. Wang D , Zeng W-N , Qin Y-Z , et al. Long-Term results of Cementless total hip arthroplasty for patients with high hip dislocation after childhood pyogenic infection . J Arthroplasty . 2019 ; 34 ( 10 ): 2420 – 2426 . Crossref PubMed Google Scholar
10. Park C-W , Lim S-J , Cha Y-T , Park Y-S . Total hip arthroplasty with subtrochanteric shortening osteotomy in patients with high hip dislocation secondary to childhood septic arthritis: a matched comparative study with Crowe IV developmental dysplasia . J Arthroplasty . 2020 ; 35 ( 1 ): 204 – 211 . Crossref PubMed Google Scholar
11. Rollo G , Solarino G , Vicenti G , et al. Subtrochanteric femoral shortening osteotomy combined with cementless total hip replacement for Crowe type IV developmental dysplasia: a retrospective study . J Orthop Traumatol . 2017 ; 18 ( 4 ): 407 – 413 . Crossref PubMed Google Scholar
12. Krych AJ , Howard JL , Trousdale RT , Cabanela ME , Berry DJ . Total hip arthroplasty with shortening subtrochanteric osteotomy in Crowe type-IV developmental dysplasia: surgical technique . J Bone Joint Surg Am . 2010 ; 92 Suppl 1 Pt 2 : 176. https://doi.org/10.2106/JBJS.J.00061 Crossref PubMed Google Scholar
13. Takeda Y , Fukunishi S , Nishio S , Fujihara Y , Yoshiya S . Subtrochanteric femoral shortening osteotomy concomitantly performed with revision total hip arthroplasty: a case report . Medicine . 2018 ; 97 ( 42 ): e12934 . Crossref PubMed Google Scholar
14. Yazar EA , Karakus O , Saygi B . The effect of graft positions on the stability of total hip arthroplasty with different types of subtrochanteric shortening . Rev Bras Ortop . 2019 ; 54 ( 4 ): 465 – 470 . Crossref PubMed Google Scholar
15. Kaneuji A , Sugimori T , Ichiseki T , et al. Minimum ten-year results of a porous acetabular component for Crowe I to III hip dysplasia using an elevated hip center . J Arthroplasty . 2009 ; 24 ( 2 ): 187 – 194 . Crossref PubMed Google Scholar
16. Nawabi DH , Meftah M , Nam D , Ranawat AS , Ranawat CS . Durable fixation achieved with medialized, high hip center cementless THAs for Crowe II and III dysplasia . Clin Orthop Relat Res . 2014 ; 472 ( 2 ): 630 – 636 . Crossref PubMed Google Scholar
17. Mu W , Yang D , Xu B , et al. Midterm outcome of Cementless total hip arthroplasty in Crowe IV-Hartofilakidis type III developmental dysplasia of the hip . J Arthroplasty . 2016 ; 31 ( 3 ): 668 – 675 . Crossref PubMed Google Scholar
18. Komiyama K , Fukushi J-I , Motomura G , et al. Does high hip centre affect dislocation after total hip arthroplasty for developmental dysplasia of the hip? Int Orthop . 2019 ; 43 ( 9 ): 2057 – 2063 . Crossref PubMed Google Scholar
19. Pagnano W , Hanssen AD , Lewallen DG , Shaughnessy WJ . The effect of superior placement of the acetabular component on the rate of loosening after total hip arthroplasty . J Bone Joint Surg Am . 1996 ; 78 ( 7 ): 1004 – 1014 . Crossref PubMed Google Scholar
20. Christodoulou NA , Dialetis KP , Christodoulou AN . High hip center technique using a biconical threaded Zweymüller cup in osteoarthritis secondary to congenital hip disease . Clin Orthop Relat Res . 2010 ; 468 ( 7 ): 1912 – 1919 . Crossref PubMed Google Scholar
21. Russotti GM , Harris WH . Proximal placement of the acetabular component in total hip arthroplasty. A long-term follow-up study . J Bone Joint Surg Am . 1991 ; 73 ( 4 ): 587 – 592 . PubMed Google Scholar
22. Chen M , Luo Z-L , Wu K-R , et al. Cementless total hip arthroplasty with a high hip center for Hartofilakidis type B developmental dysplasia of the hip: results of midterm follow-up . J Arthroplasty . 2016 ; 31 ( 5 ): 1027 – 1034 . Crossref PubMed Google Scholar
23. Galea VP , Florissi I , Rojanasopondist P , et al. The patient acceptable symptom state for the Harris hip score following total hip arthroplasty: validated thresholds at 3-month, 1-, 3-, 5-, and 7-year follow-up . J Arthroplasty . 2020 ; 35 ( 1 ): 145 – 152 . Crossref PubMed Google Scholar
Author contributions
Oommen A. T: Carried out surgery, Prepared the manuscript, Underlook a literature review.
V. J Chandy: Carried out data collection and literature review.
C. Jeyaraj: Carried out data collection.
T. D Hariharan: Carried out data collection and literature review.
A Arun Shankar: Carried out data collection.
Poonnoose P. M: Undertook surgery, manuscript preparation.
R. J Korula: Academic input, Mentor.
M. Kandagaddala: Carried out radiological assessment.
Funding statement
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
© 2020 Author(s) et al. This is an open-access article distributed under the terms of the Creative Commons Attributions licence (CC-BY-NC-ND), which permits unrestricted use, distribution, and reproduction in any medium, but not for commercial gain, provided the original author and source are credited.









