Abstract
The COVID-19 pandemic has disrupted all segments of daily life, with the healthcare sector being at the forefront of this upheaval. Unprecedented efforts have been taken worldwide to curb this ongoing global catastrophe that has already resulted in many fatalities. One of the areas that has received little attention amid this turmoil is the disruption to trainee education, particularly in specialties that involve acquisition of procedural skills. Hand surgery in Singapore is a standalone combined programme that relies heavily on dedicated cross-hospital rotations, an extensive didactic curriculum and supervised hands-on training of increasing complexity. All aspects of this training programme have been affected because of the cancellation of elective surgical procedures, suspension of cross-hospital rotations, redeployment of residents, and an unsustainable duty roster. There is a real concern that trainees will not be able to meet their training requirements and suffer serious issues like burnout and depression. The long-term impact of suspending training indefinitely is a severe disruption of essential medical services. This article examines the impact of a global pandemic on trainee education in a demanding surgical speciality. We have outlined strategies to maintain trainee competencies based on the following considerations: 1) the safety and wellbeing of trainees is paramount; 2) resource utilization must be thoroughly rationalized; 3) technology and innovative learning methods must supplant traditional teaching methods; and 4) the changes implemented must be sustainable. We hope that these lessons will be valuable to other training programs struggling to deliver quality education to their trainees, even as we work together to battle this global catastrophe.
Introduction
The COVID-19 pandemic has disrupted all segments of daily life, devastating the social, economic and political fabric of countries across the world.1,2 Singapore was one of the earliest countries outside China to be hit by this outbreak, and most of our resources have been channelled to fight and suppress this pandemic.3 The ensuing control measures included: segregating healthcare workers (HCWs) to minimize cross-contamination, mandatory leave of absence for all staff with recent travel to shortlisted countries, deploying HCW to frontline duties, cancelling elective procedures, suspension of all travel leave, and rigorous personal protective measures. One of the areas that has received little attention amid this turmoil is the disruption to resident education, particularly in specialties that involve acquisition of procedural skills.
Hand surgery in Singapore is a combined six-year residency programme that includes elements of orthopaedic, plastic, and vascular surgery. The already-tight training timeline has been severely affected because of cancellation of elective surgical procedures, suspension of cross-hospital rotations, redeployment of residents, and an unsustainable duty roster. There is a real concern that trainees will not be able to meet their training requirements as well as suffer serious issues like burnout and depression. The current pandemic appears more protracted than the SARS outbreak in 2003 and there is no certainty about how long this situation will last.4 Suspending training activity indefinitely is not practical. This will not only extend training for the in-flight trainees, but it will also severely affect the “manpower pipeline” in the years to follow, resulting in disruption of essential medical services. At the same time, any measures implemented to maintain trainee knowledge and competence in this current climate must be simple and practical, within the scope of resources that are available and most importantly, the changes must still allow physicians and trainees to focus on their primary mission – taking care of the acutely unwell.
This article was prepared by the Joint Coordinating Committee (JCC) for the National Hand Surgery Residency Programme to outline a few of the key initiatives it has introduced to address the disruptions to resident education and maintain competency training. The authors have incorporated lessons learned from the current pandemic and the SARS outbreak. We hope that these lessons will be valuable to other training programs struggling to deliver quality education to their trainees, even as we work together to battle this global catastrophe.
Unique residency model
Singapore is one of few countries in the world where hand surgery is a standalone speciality with its own training programme. This system has been in place since the early 1990 s and the current structure is a six-year, nationwide residency programme that begins after internship. The resident is trained to be proficient in all aspects of hand surgery, including fracture fixation, nerve and tendon repair, arthroscopy, microvascular surgery and soft tissue coverage. It is truly a “regional” speciality. For example, a year five (R5) resident is expected to independently perform a digital replantation and a final year resident would be proficient at raising a free flap and performing the microvascular anastomoses under attending supervision. The learning curve is steep and the four key elements of training are: 1) highly structured rotations across specialties and institutions; 2) an extensive didactic curriculum; 3) progressive skills training in the operating room; and 4) dedicated laboratory training sessions using validated models.
Residents are currently rotated on a three- or six-monthly basis to one of three sponsoring institutions (SIs). Each SI comprises one to two academic hand surgery units with faculty affiliated to a medical school. These units provide tertiary level hand and reconstructive microsurgery services across the country. However, there are differences in the clinical case mix, and each institution may have a particular area of expertise e.g. congenital hand conditions; brachial plexus and peripheral nerve injuries; oncology; and reconstructive microsurgery. In addition, residents undergo cross-speciality rotations in orthopaedic surgery, plastic surgery, vascular surgery, dermatology, neurology and rehabilitation medicine to acquire a broad and holistic appreciation of the ailments affecting the hand and upper limb. During their training, residents are given increasing responsibilities during elective surgery. Regular 24-hour emergency calls provide the rigorous yet essential training that is necessary to ensure proficiency in this short period of time. Every aspect of this structured training programme has been adversely affected by the ongoing pandemic because of the suspension of cross-hospital rotations and teaching programs, cancellation of elective surgery, drastically reduced outpatient clinics and redeployment of trainees to frontline duties.
Key initiatives to maintain core competencies
1. Restructure duty and work-rest cycles
Resident safety and wellbeing are paramount when faced with the prospect of a long-drawn global pandemic. Every resident must be given clear guidelines on hygiene practices, use of personal protective equipment (PPE) and measures to take in the event of ill health. Trainees should only be engaged in essential clinical services. Despite the cancellation of elective surgery, the emergency hand surgery workload comprising trauma and infections has not changed significantly. The current segregation of each hand surgery department into two self-reliant teams comprising consultants and residents means that each resident takes a one-in-four (or more frequent) emergency call schedule. We have engaged senior management to make several changes to delivery of clinical services to reduce the burden on residents. First, the team that is “post-call” will have minimal outpatient clinic sessions so that the entire team can manage cases admitted the night before. This will allow the post-call resident to have a full rest day. Second, all non-critical procedures (e.g. open fractures, tendon and nerve injuries) have been deferred to the next available operating list. Third, consultant surgeons have rostered themselves to take several direct emergency calls (without a resident), so that their residents are not unnecessarily taxed.
2. Use technology and innovative learning methods to maintain training hours
Technology becomes a key asset in a situation where physical meetings and training sessions have been severely reduced. We made pre-recorded didactic lectures available to all residents in the past two months when there was significant uncertainty about the rapidly evolving situation. Moving forward, we have developed a weekly didactic teaching series hosted by each of the training institutions on a rotating basis. Each session comprises a 45-minute talk prepared by a resident, mentored by a supervisor, and will be delivered via teleconferencing software. The advantages of such technology on remote learning are well-known.5-7 Pre-reading material and structured pre-lecture questions will allow the participants to prepare beforehand and stimulate greater interaction. Virtual e-learning platforms have also enabled us to share resources. For instance, consultants who are relatively free of clinical duties (because of home quarantine or decreased elective surgeries) can contribute remotely to these educational efforts.
The cancellation of cross-hospital rotations means that many residents no longer get exposure to certain subspeciality areas e.g. peripheral nerve injuries and congenital hand problems. A useful method that we have introduced for discussing uncommon cases is an email-based worksheet (Figure 1). Each worksheet presents an uncommon clinical problem and a short vignette and is followed by five to six questions covering a broad range of learning points, including pathophysiology, clinical assessment, technical considerations and current best practices. The resident is permitted to consult textbooks, the literature and colleagues to prepare the answers. The supervisor will then discuss the answers through a teleconferencing session with all residents and/or individually via email.
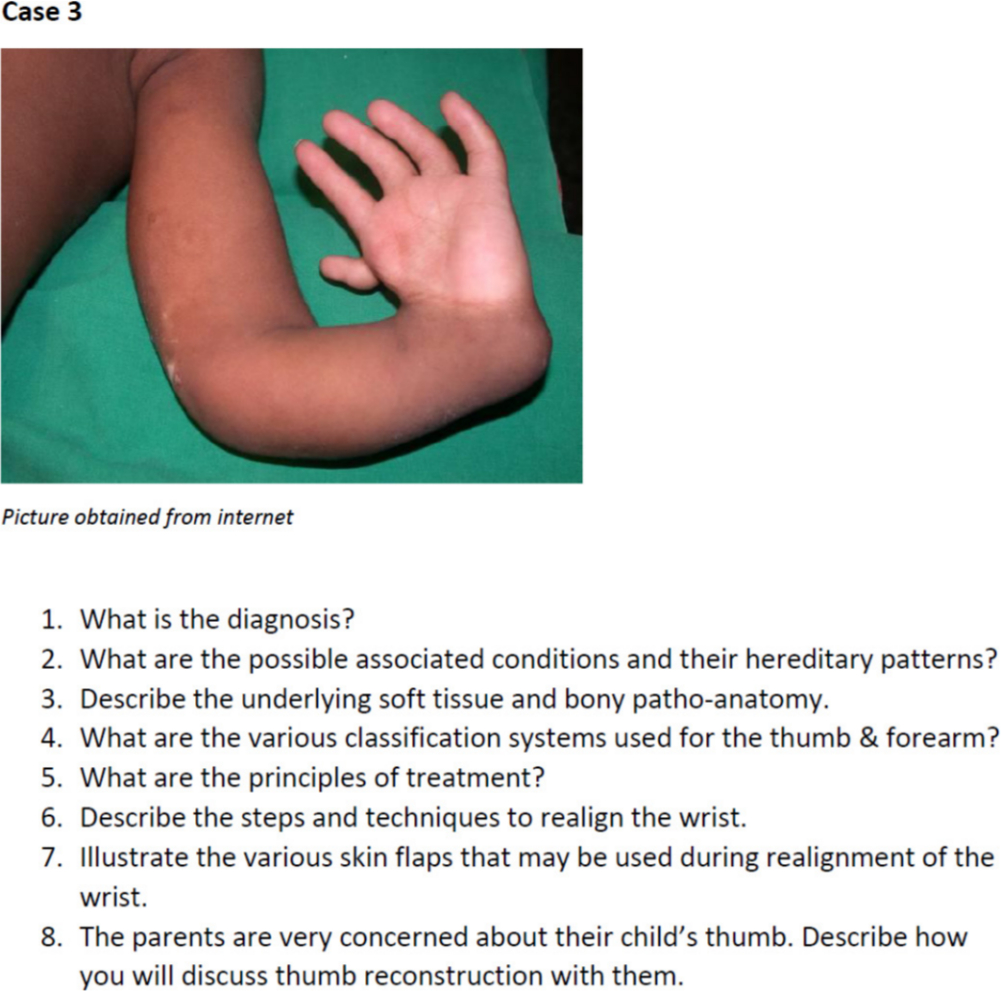
Fig. 1
Example of a case worksheet used to stimulate thinking and self-directed learning around uncommon clinical cases. These worksheets are sent out via email and can be completed remotely. Feedback is provided by email or through a teleconferencing session. The worksheets are designed to cover a wide range of issues, and an “open book” format is encouraged.
3. Enhance skills training with alternative approaches
The learning curve in hand surgery is steep because it requires expertise with multiple tissues. Many of the skills required in hand surgery can be simulated in the laboratory using validated training models. We have developed several models to train skin closure (banana peel model), tendon repairs (pig/sheep tendons), fracture pinning, microvascular anastomosis and color-coded cut-out sheets to illustrate Z-plasty and syndactyly-release flaps (Figure 2). Residents are now routinely assigned a two- to three-hour “skills slot” every week where they will not be required to perform any clinical duties. Their work is assessed by a dedicated supervisor (e.g. an attending surgeon or microsurgery technician). We have also successfully used dedicated software to make these assessments more precise and efficient.8 In addition, there is a vast repository of surgical videos on several platforms such as Hand-e (developed by the American Society for Surgery of the Hand) and VuMedi.9,10 These have been made available to the residents so that they can review them at their own pace.

Fig. 2
The fracture pinning model on the left comprises a semi-hard block with a soft resin behind it. This simulator trains and assesses a resident’s perception of 3-dimensional temporospatial relationships. E.g. they may be instructed to drill a specific design into the resin by orientating the K-wire at specified angles. The office-based microsurgery simulator shown on the right is easy to set up in a small room and requires a fixed-mounted microscope, microsurgical instruments and fine 9-0 and 10-0 sutures. Residents can complete increasingly complex suturing exercises on latex sheets, silicone strips and finally, small tubes. The Micro Trainer (Digital Surgicals, Singapore) is a simple jig onto which a silicone strip or tube can be mounted via soft clamps. The clamps can be rotated to simulate different vessel orientations. The model also allows residents to practice more advanced microvascular techniques, such as the “back-wall first” method and end-to-side anastomosis, without the need for animal models. The resident’s technique (e.g. size of bites, suture spacing, quality of knots) can be assessed by the accompanying software and immediate feedback can be provided by the microsurgery technician.
Despite the drastic reduction in the elective surgical caseload, there are some advantages to a more relaxed operating theatre schedule. The cases that are frequently relegated to a resident in a busy clinical service (e.g. fingertip injuries, infections) are now performed under the direct supervision of the consultant. This enables supervisors to impart valuable decision-making and technical skills and promotes a setting for immediate feedback in a more relaxed environment.
4. Maintain examination preparedness
In-training assessments and examination preparations have been affected globally, including postponement of national examinations.11 We have implemented several measures to ensure that the residents maintain their level of preparedness. At a local level, each supervising attending has been requested to conduct case-based tutorials and viva (oral) examination sessions, focusing on clinical and basic sciences as well as examination technique. Some attendings have even decided to use these sessions as a formal, formative assessment tool. At a national level, we are exploring methods to administer the multiple-choice questions (MCQ) and viva (oral) components of the national board examination virtually. In addition, standardized patients (actors) may be recruited for the clinical component. Although these measures are not ideal, they ensure that the examination itself can be standardized and decentralized across the country so that candidates and examiners are not required to congregate.
5. Actively develop professional skills
Every cloud has a silver lining, and every apocalyptic virus pandemic – no matter how devastating – teaches us something. The unprecedented events of the past two months have taught each of us about the importance of clear communication with patients and peers, decision-making with limited resources, being resilient and demonstrating empathy towards patients. Residents also quickly appreciate their role in the bigger organizational structure and the importance of strong leadership. These skills should be instilled indirectly by attendings who must strive to embody these traits, as well as formally through online workshops and webinars. These skills are more critical now than ever before and actively reinforcing them make our residents better doctors and not just technically proficient surgeons.
Future directions
COVID-19 has taught us several important lessons. First, resident education cannot take a backseat even as the world grapples with an escalating number of cases and fatalities. Second, we have taken the technological advances around us for granted and insisted on traditional teaching methods simply because we could. The ongoing pandemic has forced us to relook at the way we deliver teaching. For instance, videoconferencing and e-learning should become mainstream teaching tools. Besides allowing multiple people at different sites to participate in an interactive manner, it also makes didactic education much more efficient. Residents now no longer must travel across institutions to attend these lectures and this significantly frees up time for them to participate in other useful activities. Third, we have also recognized that regular simulation-based exercises are a crucial component of surgical training. Very often, these training tools are used to augment a skill set that is demonstrated in the operating room. However, we think it is beneficial to roster residents to such activities on a regular basis because it provides greater consistency in the training programme and enables residents to maintain currency with specific skill sets irrespective of clinical service requirements. Finally, there are many benefits to the traditional model of apprenticeship where the resident spends a substantial length of time with a single mentor. This is the true apprenticeship model that we have gradually lost because of the requirement for residents to rotate frequently and the pressure on attendings to generate clinical volume.
Our article outlines the principles and strategies implemented to deliver sustainable and resource-efficient surgical education during an unprecedented public health crisis. Many have argued that training is not a priority when there are other important issues to worry about. However, this is a short-sighted view and one that will come back to bite us in the future. This COVID-19 pandemic is not the first, and certainly will not be the last, global catastrophe that we will have to deal with. Resident education cannot be a casualty every time something like this happens.
References
1. McCloskey B , Zumla A , Ippolito G , et al. Mass gathering events and reducing further global spread of COVID-19: a political and public health dilemma . Lancet (London, England) . 2020 ; 395 ( 10230 ): 1096. Crossref PubMed Google Scholar
2. Fauci AS , Lane HC , Redfield RR . Covid-19 - Navigating the Uncharted . N Engl J Med . 2020 ; 382 ( 13 ): 1268 – 1269 . Crossref PubMed Google Scholar
3. Ng Y , Li Z , Chua YX , et al. Evaluation of the Effectiveness of Surveillance and Containment Measures for the First 100 Patients with COVID-19 in Singapore - January 2-February 29, 2020 . MMWR Morb Mortal Wkly Rep . 2020 ; 69 ( 11 ): 307. Crossref PubMed Google Scholar
4. Kuiken T , Fouchier RAM , Schutten M , et al. Newly discovered coronavirus as the primary cause of severe acute respiratory syndrome . Lancet (London, England) . 2003 ; 362 ( 9380 ): 263 – 270 . Crossref PubMed Google Scholar
5. Lamba P , Pankaj L . Teleconferencing in medical education: A useful tool . Australas Med J . 2011 ; 4 ( 8 ): 442 – 447 . Crossref PubMed Google Scholar
6. Augestad KM , Lindsetmo RO . Overcoming distance: video-conferencing as a clinical and educational tool among surgeons . World J Surg . 2009 ; 33 ( 7 ): 1356 – 1365 . Crossref PubMed Google Scholar
7. Chick RC , Clifton GT , Peace KM , et al. Using technology to maintain the education of residents during the COVID-19 pandemic . J Surg Educ . 2020 . Crossref PubMed Google Scholar
8. Lahiri A , Sebastin SJ , Yusoff SK , Sze Chong AK . Computer aided assessment in microsurgical training . J Hand Surg Asian-Pac Vol . 2016 ; 21 ( 2 ): 212 – 221 . Crossref PubMed Google Scholar
9. Hand.e . Free Video Database for Hand Surgeons | Hand.e . https://www.assh.org/hande/s/ (date last accessed March 29, 2020 ). Google Scholar
10. VuMedi. https://www.vumedi.com/ (date last accessed March 29, 2020). Google Scholar
11. Webinars | RCSEd. https://www.rcsed.ac.uk/professional-support-development-resources/learning-resources/webinars (date last accessed April 10, 2020). Google Scholar
Author contributions
S. Das De: Conceptualization, Primary draft of the manuscript, Edited the manuscript.
M. E. Puhaindran: Conceptualization, Primary draft of the manuscript, Edited the manuscript.
S. Sechachalam: Primary draft of the manuscript, Edited the manuscript.
K. J. H. Wong: Primary draft of the manuscript, Edited the manuscript.
C. W. Chong: Primary draft of the manuscript, Edited the manuscript.
A. Y. H. Chin: Primary draft of the manuscript, Edited the manuscript.
Funding statement
This report received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
ICMJE COI statement
The authors have no conflicts of interest to declare.
Acknowledgements
The authors would like to recognize the invaluable contributions of all attending staff and faculty from the Hand & Reconstructive Microsurgery departments of all the postgraduate training institutions in Singapore.
© 2020 Author(s) et al. This is an open-access article distributed under the terms of the Creative Commons Attributions licence (CC-BY-NC-ND), which permits unrestricted use, distribution, and reproduction in any medium, but not for commercial gain, provided the original author and source are credited. Standard









