Abstract
Aims
Our retrospective analysis reports the outcome of patients operated for slipped capital femoral epiphysis using the modified Dunn procedure. Results, complications, and the need for revision surgery are compared with the recent literature.
Methods
We retrospectively evaluated 17 patients (18 hips) who underwent the modified Dunn procedure for the treatment of slipped capital femoral epiphysis. Outcome measurement included standardized scores. Clinical assessment included ambulation, leg length discrepancy, and hip mobility. Radiographically, the quality of epiphyseal reduction was evaluated using the Southwick and Alpha-angles. Avascular necrosis, heterotopic ossifications, and osteoarthritis were documented at follow-up.
Results
At a mean follow-up of more than nine years, the mean modified Harris Hip score was 88.7 points, the Hip Disability and Osteoarthritis Outcome Score (HOOS) 87.4 , the Merle d’Aubigné Score 16.5 points, and the UCLA Activity Score 8.4. One patient developed a partial avascular necrosis of the femoral head, and one patient already had an avascular necrosis at the time of delayed diagnosis. Two hips developed osteoarthritic signs at 14 and 16 years after the index operation. Six patients needed a total of nine revision surgeries. One operation was needed for postoperative hip subluxation, one for secondary displacement and implant failure, two for late femoroacetabular impingement, one for femoroacetabular impingement of the opposite hip, and four for implant removal.
Conclusion
Our series shows good results and is comparable to previous published studies. The modified Dunn procedure allows the anatomic repositioning of the slipped epiphysis. Long-term results with subjective and objective hip function are superior, avascular necrosis and development of osteoarthritis inferior to other reported treatment modalities. Nevertheless, the procedure is technically demanding and revision surgery for secondary femoroacetabular impingement and implant removal are frequent.
Cite this article: 2020;1-4:80–87.
Introduction
The slipped capital femoral epiphysis (SCFE) occurs with an incidence ranging from 0.33 to 24.58 of 100,000 children aged from eight to 15 years.1 Males are more affected than females.2 Three classification systems of SCFE are used. The chronological classification divides the SCFE into acute, acute on chronic, and chronic SCFE;3 the stability-based classification divides SCFE as stable or unstable, depending on the walking capacity of the patient;4 and the morphological classification is based on the displacement of the epiphysis as visualized on frog-leg radiographs according to Southwick.5 The slip is defined as mild when the angle of the affected and the contralateral side differs by less than 30°, moderate by 30° to 50°, and severe by more than 50°. Various surgical procedures have been described including in situ fixation,6,7 arthroscopic offset correction,8,9 compensatory osteotomies,10,11 and osteotomies with correction of the deformity at the head-neck junction.12-24 Nevertheless, there is no clear consensus on how best to treat SCFE. The modified Dunn procedure has become to be a standard treatment for SCFE allowing anatomic capital realignment without running a high risk of avascular necrosis (AVN) of the femoral head.25-27 Long-term outcome data remain sparse, but recent studies describe a low rate of osteoarthritis (OA) and AVN in patients treated with a modified Dunn procedure.24,28
The aim of this retrospective study is to report the long-term outcome of patients who underwent the modified Dunn osteotomy for the treatment of SCFE at our institution by a single surgeon. The clinical and radiographical results, complications, and revisions are compared with other series of surgical treatment of SCFE.
Methods
We retrospectively assessed the clinical and radiographic outcome of patients treated for SCFE using the modified Dunn procedure. Exclusion criteria were defined as patients with previous surgery, patients treated without surgical hip dislocation, and a follow-up below four years. Between 1998 and 2019, 19 patients were treated for SCFE in our institution. One patient was excluded being treated using an anterolateral approach and one for insufficient follow-up time (1.8 years). In all, 17 patients (18 hips) were available for clinical and radiographic assessment in our outpatient department. The mean age at operation was 12.9 years (6.8 to 17.0). There was a preponderance of male patients (15 males vs two females). The mean follow-up reached 9.4 years (4.2 to 20.8). 16 patients had unilateral and one patient had bilateral SFCE and was operated with 1.8 years interval on both sides. One patient (5.6%) had an acute SCFE following an adequate injury, three hips (16.7%) presented a chronic SCFE, and 14 (77.8%) an acute-on-chronic SCFE. Overall, 14 hips (77.8%) were classified as stable, and four (22.2%) as unstable. The Regional Ethical Committee for Medical and Health Research approved this study (No. 3,2006,144), and written informed consent was obtained from all the participants.
Modification of the surgical technique
Surgery is performed in full lateral position. The trochanteric slide osteotomy is performed without step to allow later free repositioning of the greater trochanter. The epiphysis is stabilized by means of a Kirschner wire (K-wire) and epiphyseal perfusion is checked before surgical hip dislocation.29 The extended retinacular flap is developed by trimming the stable part of the greater trochanter on its posterior and superior aspects down to the size of the femoral neck. Then the periosteum of the femoral neck is incised on the superior aspect towards the femoral head, and continues towards antero-inferior to reach the inferior retinaculum (Figure 1a).17 The neck is completely peeled from its periosteum, the postero-inferior callus removed, and the stump of the neck symmetrically rounded. Before reduction of the epiphysis, three drill holes of 2.5 mm diameter are drilled starting from the stump of the femoral neck in an antegrade manner towards the lateral femoral cortex allowing ideal positioning of the implants at the head neck junction (Figure 1b) . The femoral head is reduced manually and centered on the neck adjusting the anatomical offset proportions. Thereby the tension on the retinaculum as well as bleeding of the head has to be checked. The epiphysis is stabilized by a 2.5 mm K-wire introduced through the fovea and replaced before reduction of the hip by wo 2.5 mm K-wires introduced through the anterior aspect of the neck (Figure 1c). After hip relocation impingement free range of motion is evaluated clinically, and the offset controlled with fluoroscopy in two planes. Definitive stabilization is performed using the pre-drilled holes either with three fully threaded 3 mm K-wires or three 3.5 mm cortical screws. The greater trochanter is stabilized in a slight anterior and distal position to relatively lengthen the neck using two 3.5 mm cortical screws.
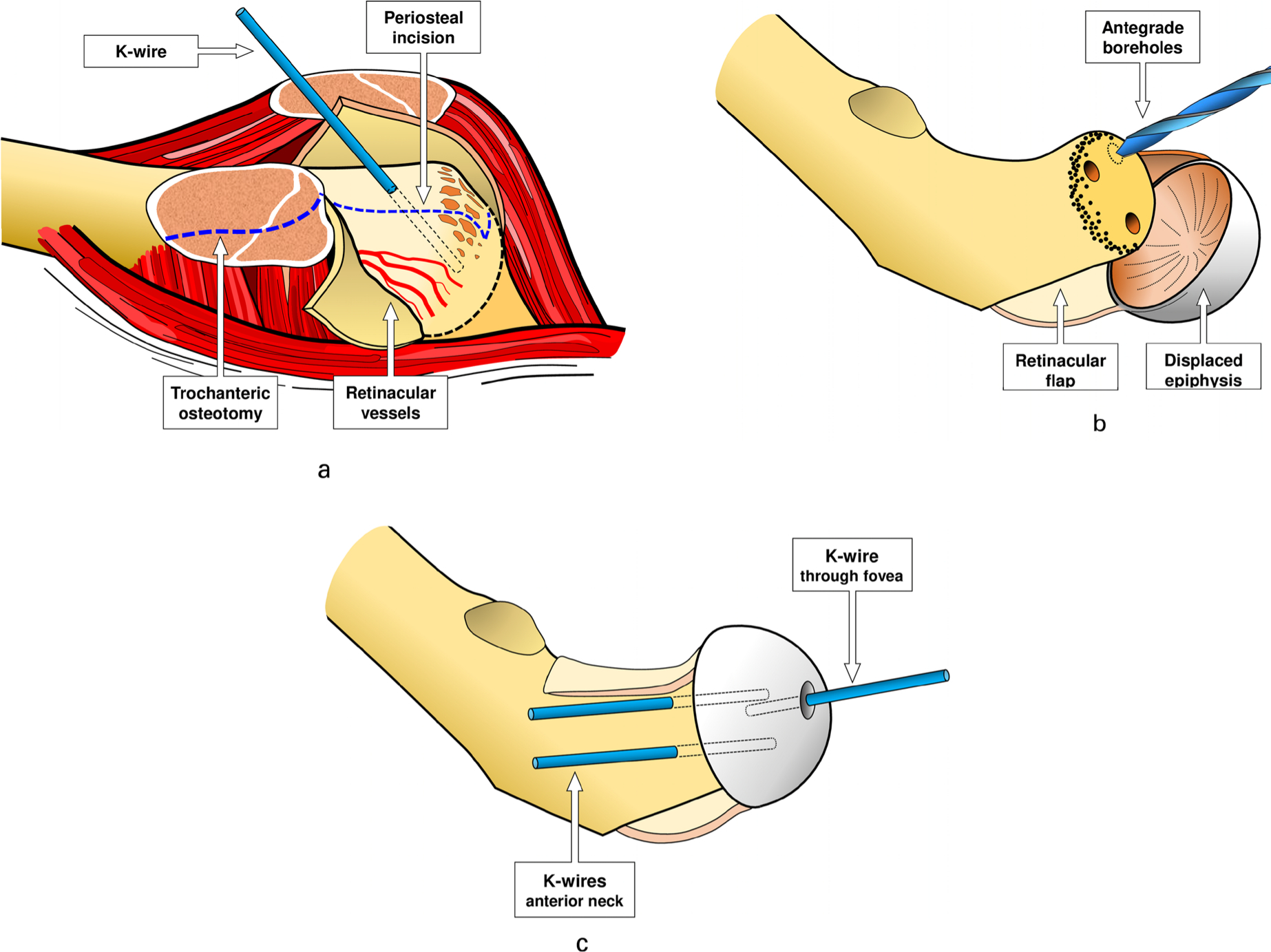
Fig. 1
a) Shows the surgical site after Z-shaped capsulotomy and trochanteric slide osteotomy of a left hip. The obliquely running apophyseal growth plate of the greater trochanter is visible. The slip zone with partially torn periosteal sheet at the head-neck junction and the femoral head in its posterior slip position are drawn. The blue dotted lines indicate the reduction osteotomy of the posterior and superior aspects of the neck and the L-shaped (superior towards anterior) incision of the periosteum for safe development of the extended periosteal flap leaving intact the terminal subsynovial branches of the deep branch of the medial femoral circumflex artery. The head is securely fixed with a K-wire. b) After removal of all the cartilage of the growth plate two distal and one proximal antegrade boreholes for later definitive stabilization of the epiphysis are made. This technical modification allows optimal positioning of the definitive implants at the level of head-neck junction. c) After manual reduction of the femoral head, a first provisional K-wire is introduced antegrade through the fovea of the head and the head offset is controlled visually and manually all around the neck. Then two retrograde K-wires are introduced from the anterior aspect of the neck, the first K-wire removed, the hip relocated and hip clearance checked. Correct bleeding out of a borehole of the head is assessed after reduction and provisional fixation.
Clinical evaluation included analysis of leg length discrepancy and muscle force of the hip abductors. Functional assessment was performed by measurement of the range of movement and evaluation of anterior femoro-acetabular impingement. Subjective outcome was assessed using questionnaires including the modified Harris Hip Score (mHHS),30 the Hip Disability and Osteoarthritis Outcome Score (HOOS),31,32 the Merle d’Aubigné Score (MdA),33 and the UCLA Activity Score. Radiological evaluation included an antero-posterior pelvis and cross-table axial or frog-leg view. The initial epiphyseal displacement was quantified by means of the epi-diaphyseal angle, the Alpha-angle and the Klein line34 on the antero-posterior projection, and the posterior slip and the Alpha-angle on the lateral views. Postoperative analysis included in addition the Beta-angle on the axial views.35 At last follow-up Alpha-angles in both planes and Beta-angles on the axial views were evaluated. Thereby, an Alpha-angle greater than 80° on the anteroposterior or greater than 60° on the lateral radiograph was defined as cam morphology due to a post-slip deformity.35-37 We noted signs of AVN, heterotopic ossification according to the classification of Brooker,38 and OA according to the grading of Tönnis.39
Statistical analysis was performed using the Winstat software (R. Fitch Software, Bad Krozingen, Germany). Level of significance was set to p < 0.05. Normal distribution of all continuous parameters was tested with the Kolmogorov-Smirnov test. Because most parameters were not normally distributed, we only used nonparametric tests, the Wilcoxon’s signed-rank test to compare dependent variables, and the Mann-Whitney U-test for independent variables.
Results
All 17 patients were available for a clinical and radiological assessment, and nobody was lost to follow-up. There were no complications during and after surgery such as deep or superficial infection, nerve or vascular injury, and thromboembolic problems. At follow-up, all hips were preserved and no total hip arthroplasty was performed. All patients walked without limping. Pelvic obliquity was seen in three patients due to a leg length discrepancy of between 0.5 cm and 2.0 cm. The force of the hip abductor muscles was found to be normal and the Trendelenburg sign was negative in all patients. The anterior impingement test was positive in five hips. The functional outcome scores showed little to no pain and a good subjective function. This is illustrated with a mean mHHS of 88.7, HOOS of 87.4, MdA of 16.5, and UCLA Activity Score of 8.4 points (Table I).
Table I.
Demographic data, classification, clinical results, and re-operations
| Hip | Sex | Age years | Side | Severity | Chronicity | Stability | FU years | Result | mHHS | HOOS | MdA | UCLA | Re-operations | Interval |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | M | 13.8 | left | severe | chronic | stable | 9.4 | AVN OA 3 |
95.00 | 97.5 | 16 | 10 | Re-ORIF ROH |
5 months, 9 months |
| 2 | M | 13.6 | left | severe | acute on chronic | stable | 9.6 | 100.00 | 98.8 | 18 | 9 | |||
| 3 | F | 11.5 | left | moderate | acute on chronic | unstable | 5.8 | 64.00 | 57.5 | 15 | 6 | ROH | 6.3 years | |
| 4 | M | 12.9 | right | moderate | acute on chronic | stable | 4.7 | 100.00 | 99.4 | 18 | 10 | |||
| 5 | F | 12.8 | left | moderate | acute on chronic | stable | 9.2 | 95.80 | 95.0 | 17 | 9 | |||
| 6 | M | 14.9 | left | moderate | acute on chronic | stable | 18.1 | 65.00 | 34.4 | 15 | 6 | Open offset correction ROH |
4.1 years 7.9 years |
|
| 7 | M | 15.2 | left | moderate | acute on chronic | unstable | 5.1 | 52.00 | 66.3 | 14 | 5 | Arthroscopic offset correction contralateral | 5.2 years | |
| 8 | M | 17.0 | left | moderate | acute on chronic | stable | 5.2 | 99.83 | 100.0 | 18 | 10 | |||
| 9 | M | 6.8 | right | moderate | acute | unstable | 20.8 | 81.00 | 87.5 | 16 | 9 | ROH Open offset correction |
4 months, 16.4 years |
|
| 10 | M | 13.7 | left | moderate | acute on chronic | unstable | 9.1 | 95.90 | 97.5 | 17 | 9 | |||
| 11 | M | 13.0 | left | mild | acute on chronic | stable | 4.2 | 100.00 | 98.8 | 18 | 9 | |||
| 12 | M | 11.5 | left | mild | acute on chronic | stable | 10.9 | 92.75 | 92.5 | 16 | 9 | |||
| 13 | M | 12.1 | left | mild | acute on chronic | stable | 7.3 | 97.00 | 97.9 | 18 | 10 | |||
| 14 | M | 13.0 | left | mild | acute on chronic | stable | 5.7 | AVN OA 2 |
94.00 | 97.5 | 16 | 9 | Re-ORIF | 3 months |
| 15 | M | 11.0 | left | mild | acute on chronic | stable | 8.2 | 99.80 | 100.0 | 18 | 10 | |||
| 16 | M | 12.5 | right | mild | acute on chronic | stable | 6.6 | 100.00 | 100.0 | 18 | 10 | |||
| 17 | M | 12.3 | right | mild | chronic | stable | 15.8 | OA 1 | 82.00 | 76.3 | 16 | 6 | ||
| 18 | M | 14.1 | left | mild | chronic | stable | 14.0 | OA 1 | 82.00 | 76.3 | 14 | 6 | ||
| mean | 12.9 | 9.4 | 88.7 | 87.4 | 16.5 | 8.4 | ||||||||
| min | 6.8 | 4.2 | 52 | 34.4 | 14 | 5 | ||||||||
| max | 17.0 | 20.8 | 100 | 100 | 18 | 10 |
-
mHHS modified Harris Hip Score
-
HOOS Hip Disability and Osteoarthritis Outcome Score
-
MdA Merle d’Aubigné Score
-
UCLA University of California at Los Angeles Activity Score
Radiographic analysis revealed eight hips presenting a mild, eight a moderate, and two a severe slip. The Klein line was positive in 15 hips. Preoperatively, the modified Alpha-angle on the AP view was 75° on the SCFE side and 52° on the contralateral side. On the axial views, the mean posterior slip angle was 31° and the Alpha-angle 92° on the SCFE, and 50° on the opposite side. The postoperative analysis reveals that the surgical reduction of the epiphyses was correct in all hips documented by the normalization of all the measured angles. The mean slip angle of 31° was corrected to minus 6°, which means more neutral positioning with respect to the present posterior slope of the contralateral side of 10°. At follow-up only the Alpha-angle on the AP view increased significantly from 49° to 61° (p = 0.0429), while the Alpha- and Beta-angles on the axial view remained unchanged (Table II).
Table II.
Radiographic results
| Parameter | Preoperative angles | Postoperative angles | Follow-up angles | p-value pre- versus postoperative | p-value preoperative versus FU | p-value postoperative versus FU | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| Antero-posterior slip angle | Difference SCFE-contralateral | 16.4 ± 13.2 | (1 - 45) | - 4.4 ± 11.8 | (-27 to 13) | 0.0004 | ||||
| Caudal inclination | SCFE | 49.5 ± 16.4 | (33 - 92) | 28.4 ± 11.8 | (11 - 45) | < 0.0001 | ||||
| Caudal inclination | Contralateral | 33.1 ± 5.2 | (27 - 49) | 32.8 ± 5.7 | (22 - 42) | 0.7583 | ||||
| Axial slip angle | Difference SCFE-contralateral | 30.8 ± 14.3 | (9 - 56) | - 5.9 ± 7.4 | (-18 to 8) | 0.0002 | ||||
| Posterior slip | SCFE | 42.1 ± 16.6 | (16 - 70) | 4.1 ± 5.9 | (-6 to 17) | < 0.0001 | ||||
| Posterior slope | Contralateral | 11.3 ± 4.8 | (2 - 20) | 9.9 ± 3.8 | (2 - 16) | 0.0281 | ||||
| α-angle (ap view) | SCFE | 74.5 ± 19.0 | (47 - 119) | 49.0 ± 9.5 | (33 - 73) | 60.8 ± 21.5 | (32 - 94) | 0.0018 | 0.0742 | 0.0429 |
| Contralateral | 52.2 ± 8.6 | (42 - 75) | 56.4 ± 6.5 | (46 - 74) | 58.7 ± 14.0 | (45 - 89) | 0.0674 | 0.2330 | 0.9382 | |
| α-angle (axial view) | SCFE | 92.3 ± 13.4 | (55 - 120) | 37.9 ± 7.7 | (30 - 56) | 41.7 ± 12.1 | (30 - 83) | < 0.0001 | 0.0002 | 0.3958 |
| Contralateral | 49.7 ± 8.5 | (35 - 66) | 45.6 ± 8.9 | (33 - 71) | 44.7 ± 9.1 | (33 - 64) | 0.0843 | 0.0609 | 0.3343 | |
| β-angle (axial view) | SCFE | 37.1 ± 7.7 | (26 - 51) | 40.9 ± 13.5 | (29 - 88) | 0.8961 | ||||
| Contralateral | 41.2 ± 6.4 | (31 - 51) | 40.1 ± 8.4 | (32 - 64) | 0.2585 |
-
Values are given as mean ± 1 SD (range minimum to maximum)
-
Level of significance p < 0.05
Among the 18 hips two hips presented AVN with concomitant OA grade 2 and 3. In one patient with a delay of diagnosis of 1.5 years, AVN was diagnosed during surgery; the second patient was revised at three months after the index procedure due to secondary displacement, implant fatigue failure and intra-articular protrusion of the K-wires (Figures 2a-e, 3a-c). At long-term follow-up both patients reported good subjective outcomes (mHHS 95, HOOS 97.5, MdA 16, UCLA 10, and 94, 97.5, 16, 9, respectively). Heterotopic ossifications stage 1 was seen in three hips. Development of slight signs of OA (grade 1) was observed in two hips at 14 and 16 years after the index operation.
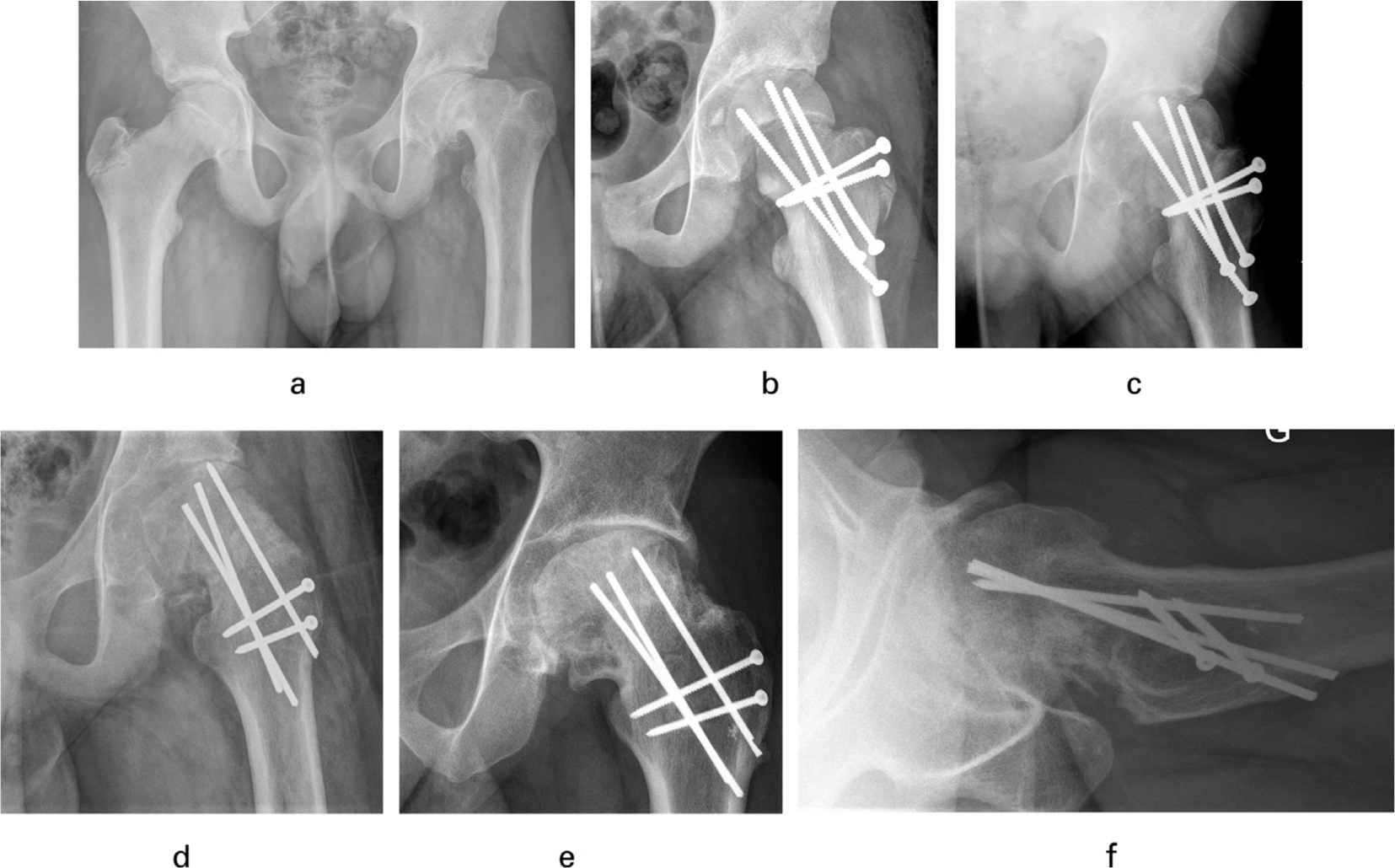
Fig. 2
a) 13.7 years old patient presenting with a 1.5-year history of left knee pain showing a severe chronic slip. b) Postoperative radiograph showing overcorrection with severe valgus position of the epiphysis and concomitant lateralization of the head. The head shows radiotransparency as sign of pre-existing AVN in its superior segment. c) Shows AVN with lateral femoral head subluxation at 12 weeks. d) Anteroposterior radiograph after the second hip dislocation with varisation of the epiphysis to re-center the hip and rotate the necrotic parts of the femoral head out of the weight-bearing area. e) Situation at 9.5 years. f) The femoral head is re-centered in both planes and the necrotic parts of the head at least partially remodeled. The subjective outcome is good (mHHS 95, HOOS 97.5, MdA 16, UCLA 10).
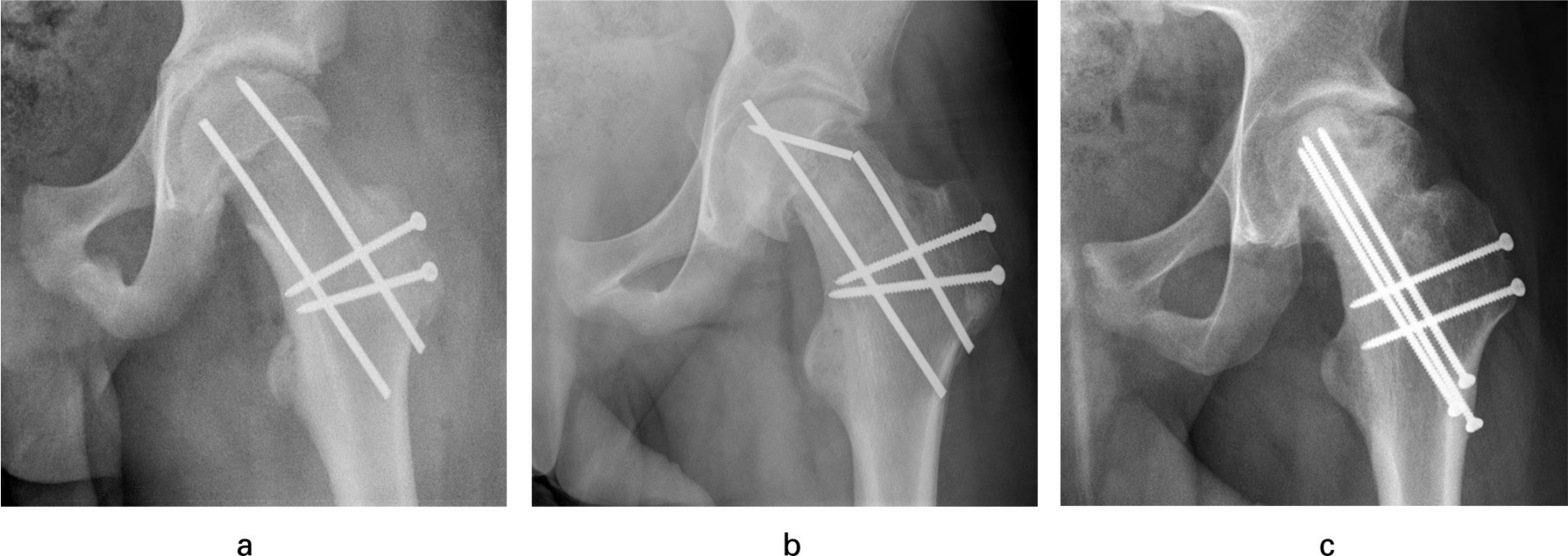
Fig. 3
a) Shows the postoperative result in a 13.3-year-old patient who presented with a mild SCFE. Stabilization was performed using only two threaded K-wires. b) At 12 weeks, secondary dislocation, implant fatigue failure and intra-articular protrusion of one K-wire occurred, needing revision surgery. c) Radiographic result at six years showing partial AVN and flattening of the lateral head segment. In addition, the adjacent acetabulum is sclerotic and flattened due to the remodeling process. Nevertheless, the outcome is good (mHHS 94, HOOS 97.5, MdA 16, UCLA 9).
Six patients needed a total of nine revision surgeries. One operation was performed for surgically induced lateral hip subluxation, one for secondary displacement and implant failure, two for late femoroacetabular impingement (FAI) at four and 16 years, one for FAI of the opposite hip at five years, and four for implant removal. A cam morphology was observed in a total of eight hips, four had a mild, four a severe deformity at the head-neck junction.
Discussion
This study is the third long-term report in the literature beside the published work of Ziebarth and Lerch.2,24 It shows at an average follow-up of more than nine years for good hip function, and a low rate of AVN and OA in patients with SCFE treated with the modified Dunn procedure. The rate of surgical complications was low, although six out of 17 patients needed further surgical interventions (Table I). The patient reported outcome was good to excellent in 14 patients (15 hips) based on the scores. Moderate slips showed a tendency towards lower scores and a higher re-operation rate, but differences were statistically not significant. Good to excellent results are also reported by other authors.18,20The radiologic outcome elucidates that with the open surgery the capital realignment could be achieved in all hips. But at nine years the modified Alpha-angle increased, creating a concomitant decrease of the offset at the superolateral head neck junction. This phenomenon could be explained by a radiologically visible bell-shaped morphology of the proximal femur due to remodeling and osteogenic activity of the resutured periosteal sheet. In our study, the rate of postoperative AVN reached 5.6% and is comparable with other recent studies.16,24 After the modified Dunn procedure, low2,17,18,20,22,40,41 and high rates up to 29%21,23,42-46 of AVN are reported. After in situ pinning, AVN is seen in 4% to 42%,21,43,47 and even after prophylactic fixation of the contralateral hip AVN can occur.48 These differences could be attributed to differences in the applied surgical technique, or different delay between diagnosis and surgery. The two patients in our series presenting AVN radiologically are only slightly symptomatic and have a good long-term clinical outcome. Asymptomatic OA grade 1 was seen in both hips of a patient suffering from bilateral SCFE. This low rate of OA is comparable with other studies using the same reduction technique.21,22,24 Higher rates are reported after in-situ pinning with long-term follow-up. Castañeda49 reports after 20 years OA grade 2 in 26.4% and OA grade 3 in 62% of patients.
In our series, five hips had a positive anterior impingement test, but only two of them had a pathological Alpha-angle on the axial view. Cam-type morphology50 and positive impingement tests are also reported in the literature being between 20% and 79.3%.7,49 But surgical revisions due to FAI are performed in only up to 16% of the SCFE hips.2,17,18,20,22,42 This corresponds to our study with a revision rate of two out of 18 SCFE hips, and one arthroscopic offset correction on the contralateral side. Nevertheless, early cartilage degeneration and OA seem to be related to persisting FAI in adulthood.49
Several advantages of the modified Dunn procedure have to be mentioned. First, it permits the complete removal of the postero-inferior callus and allows epiphyseal reduction without stretching or kinking of the retinacular vessels. Second, capital realignment and offset at the head-neck junction can be directly visualized. Third, impingement free movement of the hip can be tested intra-operatively. Fourth, the blood supply to the femoral head can be checked during surgery and measures for improvement during surgery are possible. And fifth, the correct extra-articular position of all implants can be assured without image intensifier, thus avoiding intra-articular implant penetration with subsequent chondrolysis.51 Our proposed modification of the fixation technique has the advantage of correct positioning of the implants at the most critical area of the head neck junction and allows assessment of hip clearance with the provisional fixation.
Our study has some limitations. First, we have no control group allowing comparison with another treatment. Second, all patients were treated with the same surgical technique, regardless of the severity, stability, or chronicity of the slip. Third, we did not include pre-operative movement of the hips, as correct measurement in a painful SCFE hip would not be reliable. This study presents some strength: first, all patients declared written consent for clinical and radiological examinations and no patient was lost for follow-up. Second, all the operations were performed by one surgeon. Third, all patients were personally examined by the authors in the outpatient department.
Conclusion
The modified Dunn procedure offers the technical possibility to achieve near anatomical realignment of the capital epiphysis in SCFE hips. Long-term outcome data show good to excellent scores, nearly normal hip function and low rates of AVN or progression of OA. In our opinion, all severity groups of SCFE should be treated the same way to restore normal hip morphology. But AVN remains a significant risk and later surgical hip revision due to cam-type morphology and symptomatic femoro-acetabular impingement may be needed.
References
1. Loder RT , Skopelja EN . The epidemiology and demographics of slipped femoral epiphysis . ISRN Orthopedics . 2011:486512. Google Scholar
2. Ziebarth K , Milosevic M , Lerch T , et al. High survivorship and little osteoarthritis at 10-years follow-up in SCFE patients treated with a modified Dunn procedure . Clin Orthop Relat Res . 2017 ; 475 ( 4 ): 1212 – 1228 . Google Scholar
3. Fahey JJ , O’Brien ET . Acute slipped capital femoral epiphysis: review of the literature and report of ten cases . J Bone Joint Surg . 1965 ; 47-A : 1105 – 1127 . PubMed Google Scholar
4. Loder RT , Richards BS , Shapiro PS , Reznick LR , Aronson DD . Acute slipped capital femoral epiphysis: the importance of physeal stability . J Bone Joint Surg . 1993 ; 75-A ( 8 ): 1134 – 1140 . Crossref PubMed Google Scholar
5. Southwick WO . Osteotomy through the lesser trochanter for slipped capital femoral epiphysis . J Bone Joint Surg . 1967 ; 49-A ( 5 ): 807 – 835 . PubMed Google Scholar
6. Johari AN , Pandey RA . Controversies in management of slipped capital femoral epiphysis . World J Orthop . 2016 ; 7 ( 2 ): 78 – 81 . Crossref PubMed Google Scholar
7. Ghijselings S , Touquet J , Himpe N , et al. Degenerative changes of the hip following in situ fixation for slipped capital femoral epiphysis: a minimum 18-year follow-up study . Hip Int . 2019 : 1120700019867248 . Crossref PubMed Google Scholar
8. Leunig M , Horowitz K , Manner H , Ganz R . In situ pinning with arthroscopic osteoplasty for mild SCFE: a preliminary technical report . Clin Orthop Relat Res . 2010 ; 468 ( 12 ): 3160 – 3167 . Crossref PubMed Google Scholar
9. Tscholl PM , Zingg PO , Dora C , et al. Arthroscopic osteochondroplasty in patients with mild slipped capital femoral epiphysis after in situ fixation . J Child Orthop . 2016 ; 10 ( 1 ): 25 – 30 . Crossref PubMed Google Scholar
10. Hiertonn T . Wedge osteotomy in advanced femoral epiphysiolysis . Acta Orthop Scand . 1955 ; 25 ( 1 ): 44 – 62 . PubMed Google Scholar
11. Imhäuser G . Die Imhäuser Osteotomie bei floridem Gleitprozess . Z Orthop . 1965 ; 100 : 312 – 320 . Google Scholar
12. Herndon CH , Heyman CH , Bell DM . Treatment of slipped capital femoral epiphysis by epiphyseodesis and osteoplasty of the femoral neck. A report of further experiences . J Bone Joint Surg . 1963 ; 45-A : 999 – 1012 . PubMed Google Scholar
13. Dunn DM . The treatment of adolescent slipping of the upper femoral epiphysis . J Bone Joint Surg . 1964 ; 46-B ( 4 ): 621 – 629 . PubMed Google Scholar
14. Broughton NS , Todd RC , Dunn DM , Angel JC . Open reduction of the severely slipped upper femoral epiphysis . J Bone Joint Surg . 1988 ; 70-B ( 3 ): 435 – 439 . Crossref PubMed Google Scholar
15. Fron D , Forgues D , Mayrargue E , Halimi P , Herbaux B . Followup study of severe slipped capital femoral epiphysis treated with Dunn’s osteotomy . J Pediatr Orthop . 2000 ; 20 ( 3 ): 320 – 325 . Google Scholar
16. Ziebarth K , Zilkens C , Spencer S , et al. Capital realignment for moderate and severe SCFE using a modified Dunn procedure . Clin Orthop Relat Res . 2009 ; 467 ( 3 ): 704 – 716 . Crossref PubMed Google Scholar
17. Slongo T , Kakaty D , Krause F , Ziebarth K . Treatment of slipped capital femoral epiphysis with a modified Dunn procedure . J Bone Joint Surg . 2010 ; 92-A : 2898 – 2908 . Crossref PubMed Google Scholar
18. Huber H , Dora C , Ramseier LE , Buck F , Dierauer S . Adolescent slipped capital femoral epiphysis treated by a modified Dunn osteotomy with surgical hip dislocation . J Bone Joint Surg . 2011 ; 93-B ( 6 ): 833 – 838 . Crossref PubMed Google Scholar
19. Masse A , Aprato A , Grappiolo G , et al. Surgical hip dislocation for anatomic reorientation of slipped capital femoral epiphysis: preliminary results . Hip Int . 2012 ; 22 ( 2 ): 137 – 144 . Crossref PubMed Google Scholar
20. Madan SS , Cooper AP , Davies AG , Fernandes JA . The treatment of severe slipped capital femoral epiphysis via the Ganz surgical dislocation and anatomical reduction: a prospective study . Bone Joint J . 2013 ; 95-B ( 3 ): 424 – 429 . Crossref PubMed Google Scholar
21. Sankar WN , Vanderhave KL , Matheney T , Herrera-Soto JA , Karlen JW . The modified Dunn procedure for unstable slipped capital femoral epiphysis: a multicenter perspective . J Bone Joint Surg . 2013 ; 95-A : 585 – 591 . Crossref PubMed Google Scholar
22. Novais EN , Hill MK , Carry PM , Heare TC , Sink EL . Modified Dunn procedure is superior to in situ pinning for short-term clinical and radiographic improvement in severe stable SCFE . Clin Orthop Relat Res . 2015 ; 473 ( 6 ): 2108 – 2117 . Crossref PubMed Google Scholar
23. Davis RL , Samora WP , Persinger F , Klingele KE . Treatment of unstable versus stable slipped capital femoral epiphysis using the modified Dunn procedure . J Pediatr Orthop . 2019 ; 39 ( 8 ): 411 – 415 . Crossref PubMed Google Scholar
24. Lerch TD , Vuilleumier S , Schmaranzer F , et al. Patients with severe slipped capital femoral epiphysis treated by the modified Dunn procedure have low rates of avascular necrosis, good outcomes, and little osteoarthritis at long-term follow-up . Bone Joint J . 2019 ; 101-B ( 4 ): 403 – 414 . Crossref PubMed Google Scholar
25. Gautier E , Ganz K , Krügel N , Gill T , Ganz R . Anatomy of the medial femoral circumflex artery and its surgical implications . J Bone Joint Surg . 2000 ; 82-B ( 5 ): 679 – 683 . PubMed Google Scholar
26. Ganz R , Gill TJ , Gautier E , et al. Surgical dislocation of the adult hip - a technique with full access to the femoral head and acetabulum without the risk of avascular necrosis . J Bone Joint Surg . 2001 ; 83-B : 1119 – 1124 . Google Scholar
27. Ganz R , Huff TW , Leunig M . Extended retinacular soft-tissue flap for intraarticular hip surgery: surgical technique, indications, and results of application . Instr Course Lect . 2009 ; 58 : 241 – 255 . Google Scholar
28. Tannast M , Jost LM , Lerch TD , et al. The modified Dunn procedure for slipped capital femoral epiphysis: the Bernese experience . J Child Orthop . 2017 ; 11 ( 2 ): 138 – 146 . Crossref PubMed Google Scholar
29. Gill TJ , Sledge JB , Ekkernkamp A , Ganz R . Intraoperative assessment of femoral head vascularity after femoral neck fracture . J Orthop Trauma . 1998 ; 12 ( 7 ): 474 – 478 . Crossref PubMed Google Scholar
30. Harris WH . Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation . J Bone Joint Surg . 1969 ; 51-A ( 4 ): 737 – 755 . PubMed Google Scholar
31. Klassbo M , Larsson E , Mannevik E . Hip disability and osteoarthritis outcome score. An extension of the Western Ontario and McMaster Universities Osteoarthritis Index . Scand J Rheumatol . 2003 ; 32 ( 1 ): 46 – 51 . Crossref PubMed Google Scholar
32. Nilsdotter AK , Lohmander LS , Klässbo M , Roos EM . Hip disability and osteoarthritis outcome score (HOOS) - validity and responsiveness in total hip replacement . BMC Musculoskelet Disord . 2003 ; 4 : 10 . Google Scholar
33. Merle d’Aubigné R , Postel M . Functional results of hip arthroplasty with acrylic prosthesis . J Bone Joint Surg . 1954 ; 35-A : 451 – 475 . PubMed Google Scholar
34. Klein A , Joplin RJ , Reidy JA , Hanelin J . Slipped capital femoral epiphysis; early diagnosis and treatment facilitated by normal roentgenograms . J Bone Joint Surg . 1952 ; 34-A ( 1 ): 233 – 239 . Google Scholar
35. Nötzli HP , Wyss TF , Stoecklin CH , et al. The contour of the femoral head-neck junction as a predictor for the risk of anterior impingement . J Bone Joint Surg . 2002 ; 84-B ( 4 ): 556 – 560 . Crossref PubMed Google Scholar
36. Gosvig KK , Jacobsen S , Palm H , Sonne-Holm S , Magnusson E . A new radiological index for assessing asphericity of the femoral head in cam impingement . J Bone Joint Surg . 2007 ; 89-B ( 10 ): 1309 – 1316 . Crossref PubMed Google Scholar
37. Agricola R , Waarsing JH , Thomas GE , et al. Cam impingement: defining the presence of a cam deformity by the alpha angle: data from the CHECK cohort and Chingford cohort . Osteoarthritis Cartilage . 2014 ; 22 ( 2 ): 218 – 225 . Crossref PubMed Google Scholar
38. Brooker AF , Bowerman JW , Robinson RA , Riley LH . Ectopic ossification following total hip replacement. Incidence and a method of classification . J Bone Joint Surg . 1973 ; 55-A : 1629 – 1632 . PubMed Google Scholar
39. Tönnis D , Heinecke A . Acetabular and femoral anteversion: relationship with osteoarthritis of the hip . J Bone Joint Surg . 1999 ; 81-A ( 12 ): 1747 – 1770 . Crossref PubMed Google Scholar
40. Elmarghany M , Abd El-Ghaffar TM , Seddik M , et al. Surgical hip dislocation in treatment of slipped capital femoral epiphysis . SICOT J . 2017 ; 3 : 10 . Crossref PubMed Google Scholar
41. Persinger F . Davis RL 2nd, Samora WP, Klingele KE. Treatment of unstable slipped capital epiphysis via the modified Dunn procedure . J Pediatr Orthop . 2018 ; 38 : 3 – 8 . Google Scholar
42. Upasani VV , Matheney TH , Spencer SA , et al. Complications after modified Dunn osteotomy for the treatment of adolescent slipped capital femoral epiphysis . J Pediatr Orthop . 2014 ; 34 ( 7 ): 661 – 667 . Crossref PubMed Google Scholar
43. Souder CD , Bomar JD , Wenger DR . The role of capital realignment versus in situ stabilization for the treatment of slipped capital femoral epiphysis . J Pediatr Orthop . 2014 ; 34 ( 8 ): 791 – 798 . Crossref PubMed Google Scholar
44. Sikora-Klak J , Bomar JD , Paik CN , Wenger DR , Upasani V . Comparison of surgical outcomes between a triplane proximal femoral osteotomy and the modified Dunn procedure for stable, moderate to severe slipped capital femoral epiphysis . J Pediatr Orthop . 2019 ; 39 ( 7 ): 339 – 346 . Crossref PubMed Google Scholar
45. Ebert N , Rupprecht M , Stuecker R , et al. Outcome of the modified Dunn procedure in severe chronic or acute on chronic slipped capital femoral epiphysis . J Orthop Surg Res . 2019 ; 14 ( 1 ): 349 . Crossref PubMed Google Scholar
46. Masquijo JJ , Allende V , D’Elia M , Miranda G , Fernández CA . Treatment of slipped capital femoral epiphysis with the modified Dunn procedure: a multicenter study . J Pediatr Orthop . 2019 ; 39 ( 2 ): 71 – 75 . Crossref PubMed Google Scholar
47. Rattey T , Piehl F , Wright JG . Acute slipped capital femoral epiphysis. Review of outcomes and rates of avascular necrosis . J Bone Joint Surg . 1996 ; 78-A ( 3 ): 398 – 402 . Crossref PubMed Google Scholar
48. Kroin E , Frank JM , Haughom B , Kogan M . Two cases of avascular necrosis after prophylactic pinning of the asymptomatic, contralateral femoral head for slipped capital femoral epiphysis: case report and review of the literature . J Pediatr Orthop . 2015 ; 35 ( 4 ): 363 – 366 . Crossref PubMed Google Scholar
49. Castañeda P , Ponce C , Villareal G , Vidal C . The natural history of osteoarthritis after a slipped capital femoral epiphysis/the pistol grip deformity . J Pediatr Orthop . 2013 ; 33 ( Suppl 1 ): S76 – 82 . Crossref PubMed Google Scholar
50. Fraitzl CR , Käfer W , Nelitz M , Reichel H . Radiological evidence of femoroacetabular impingement in mild slipped capital femoral epiphysis: a mean followup of 14.4 years after pinning in situ . J Bone Joint Surg . 2007 ; 89-B : 1592 – 1596 . Google Scholar
51. Walters R , Simon SR . Joint destruction: a sequel of unrecognized pin penetration in patients with slipped capital femoral epiphyses. In: The hip: proceedings of the eighth open scientific meeting of the hip Society . St. Louis : CV Mosby , 1980 : 145 – 164 . Google Scholar
Funding statement
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article
©2020 Author(s) et al. This is an open-access article distributed under the terms of the Creative Commons Attributions licence (CC-BY-NC-ND), which permits unrestricted use, distribution, and reproduction in any medium, but not for commercial gain, provided the original author and source are credited.









