Abstract
Aims
When the present study was initiated, we changed the treatment for late-detected developmental dislocation of the hip (DDH) from several weeks of skin traction to markedly shorter traction time. The aim of this prospective study was to evaluate this change, with special emphasis on the rate of stable closed reduction according to patient age, the development of the acetabulum, and the outcome at skeletal maturity.
Methods
From 1996 to 2005, 49 children (52 hips) were treated for late-detected DDH. Their mean age was 13.3 months (3 to 33) at reduction. Prereduction skin traction was used for a mean of 11 days (0 to 27). Gentle closed reduction under general anaesthesia was attempted in all the hips. Concurrent pelvic osteotomy was not performed. The hips were evaluated at one, three and five years after reduction, at age eight to ten years, and at skeletal maturity. Mean age at the last follow-up was 15.7 years (13 to 21).
Results
Stable closed reduction was obtained in 36 hips (69%). Open reduction was more often necessary in patients ≥ 18 months of age at reduction (50%) compared with those under 18 months (24%). Residual hip dysplasia/subluxation occurred in 12 hips and was significantly associated with avascular necrosis (AVN) and with high acetabular index and low femoral head coverage the first years after reduction. Further surgery, mostly pelvic and femoral osteotomies to correct subluxation, was performed in eight hips (15%). The radiological outcome at skeletal maturity was satisfactory (Severin grades 1 or 2) in 43 hips (83%).
Conclusions
Gentle closed reduction can be attempted in children up to three years of age, but is likely to be less successful in children aged over 18 months. There is a marked trend to spontaneous improvement of the acetabulum after reduction, even in patients aged over 18 months and therefore simultaneous pelvic osteotomy is not always necessary.
Introduction
There is general agreement regarding the goals of treatment in late-detected developmental dislocation of the hip (DDH): to obtain and maintain concentric hip reduction, to avoid complications, and to use as few operative interventions as possible. However, in spite of numerous studies over the last decades, there is no consensus concerning the optimal method to reach these goals. The most debated questions include the use of prereduction traction, whether to use open or closed reduction, and whether or not pelvic osteotomy should be performed at the same time as hip reduction.
Preliminary skin traction of relatively short duration (two to three weeks), with the intentions to enable easier closed reduction and to reduce the rate of avascular necrosis (AVN) has been recommended by some authors,1,2 whereas others have reported no effect of preliminary traction.3,4 According to a questionnaire among POSNA members two decades ago, 82% of the responders used traction for 12-month-old children.5 A recent survey showed that 76% of POSNA members never used traction, indicating decreased use of traction during the last decades.6
Generally, closed reduction has been the preferred treatment method for late-detected DDH in the past.7,8 Open reduction has been reserved for patients in whom gentle closed reduction was not achieved. Although open reduction is more often needed in older patients, there are little objective data on the success of closed reduction according to patient age.9-11
If the development of the acetabulum is unsatisfactory, subsequent surgery such as pelvic osteotomy and/or femoral osteotomy can be used to correct residual dysplasia/subluxation, but the indications and frequency of such operations differ considerably.8,12,13 The rate of residual dysplasia can be reduced by simultaneous pelvic osteotomy at the time of primary reduction. This was initially used in patients older than 18 months.14-16 In recent years, however, concurrent pelvic osteotomy or acetabuloplasty has also been used in younger patients down to six months of age.17,18 This policy is controversial because the acetabulum has a considerable ability to spontaneous improvement.8,19
Some decades ago, the treatment of late-detected DDH in our department consisted of a relatively long period of longitudinal skin traction to obtain gradual closed reduction.8 For various reasons, our treatment has changed to shorter traction time followed by an attempt at closed reduction. The aim of this prospective study was to evaluate this change of treatment policy, with special emphasis on the rate of stable closed reduction according to patient age, the development of the acetabulum, and the radiological outcome at skeletal maturity.
Methods
Patients were included if they met the following criteria: age over three months and under three years at diagnosis, no associated anomaly, no neuromuscular disorder, and no previous closed or open reduction in other hospitals. Patients with acetabular dysplasia only or slight subluxation were not included. The study was approved by the hospital's privacy and data protection officer (ref: 2014/14357).
In all, 50 patients met these requirements and were consecutively treated with attempted closed reduction during 1996 to 2005, but one patient was excluded because the follow-up routines had not been followed. Thus, the study included 49 patients (52 hips). They were 47 girls (96%) and two boys with a mean age of 13.3 months (3 to 33) at the time of hip reduction. Three patients had bilateral DDH. Total dislocation occurred in 45 hips (87%) and severe subluxation (femoral head coverage under 50%) in seven hips.
All the patients except two had preliminary bilateral skin traction with slight flexion, neutral rotation, and about 30° abduction of each hip. The aim was not to obtain reduction of the dislocated hip, but rather to stretch the muscles and other soft tissues in the hope that this would facilitate reduction. The mean time in skin traction was 11.4 days (0 to 27). An attempt at gentle closed reduction under general anaesthesia was performed in all the patients. The stability of the reduction was tested manually assisted by intraoperative fluoroscopy. If closed reduction was not achieved, open reduction through an anterolateral approach was performed under the same anaesthesia. During open reduction, ligamentum teres and ligamentum transversum were resected, the iliopsoas tendon was cut, and the hypertrophic soft tissue in the acetabulum was removed to make the reduction more concentric. The joint capsule was closed using capsulorrhaphy to enhance the stability. A CT scan was taken the next day to check that the reduction was satisfactory. The mean immobilization time in hip spica after closed reduction was 5.9 months (3 to 9). Thereafter, an abduction orthosis was used for a few months.
Radiographic evaluation
Anteroposterior radiographs of the pelvis were taken with the child in the supine position and with the legs parallel. For assessment of radiological development, these radiographs were used: the primary one and those taken one, three and five years after reduction, at age eight to ten years, and at skeletal maturity. The radiological measurements were performed prospectively by one of the authors (TT) who has a very long experience with radiological evaluations of hip joints in children.
The acetabular index (AI) was measured according to Kleinberg and Lieberman.20 The migration percentage (MP) was measured according to Reimers.21 When migration is 33% to 89% the hip is subluxated and 90% or more means complete dislocation. The centre-edge (CE) angle of Wiberg22 was included from three years after reduction. Assessment of avascular necrosis (AVN) of the femoral head was performed according to Kalamchi and MacEwen,23 but only groups II-IV were regarded as true AVN.
The radiological outcome at skeletal maturity was assessed with a modification of the classification of Severin.24 We used the same limit for CE angle in children under 14 years of age as in older patients. Severin grades 1 and 2 hips have CE angles of 20° or above. Severin grade 3 is acetabular dysplasia with CE angle under 20°. Severin grade 4 is subluxation, with CE angle less than 10° and MP above 33%, plus a broken Shenton line. Hips with CE angle 20° or higher (Severin grades 1/2) had satisfactory radiological outcome and those with CE angle less than 20° (Severin grades 3/4) were termed unsatisfactory.
Statistics
SPSS software, version 25 (IBM, Armonk, New York, USA) was used for the statistical analysis. Categorical data were analyzed with Pearson's chi-squared test and continuous variables with Student's t-test for independent samples. The correlation between continuous variables was expressed as Pearson's correlation coefficient (r). All tests were two-sided. Differences were considered significant if the p-value was < 0.05.
Results
Initially, closed reduction was achieved in 42 hips and primary open reduction under the same anaesthesia was necessary in the remaining ten hips (Figure 1). Early redislocation after closed reduction occurred in six patients (six hips) and was diagnosed by CT on the first postoperative day in five patients and after one month in one patient, and was treated with open reduction as soon as possible. Thus, the permanent treatment was closed reduction in 36 hips (69%) and open reduction in 16 hips (31%). Permanent closed reduction was obtained more often in patients under 12 months of age (22 of 26 hips, 85%) than in children at age 12 to 23 months (12 of 20 hips, 60%) and age 24 to 33 months (two of six hips, 33%) (p = 0.026). The mean traction time was 10.5 days in hips treated with closed reduction and 13.2 days in those with open reduction; the difference was not statistically significant (p = 0.077). Redislocation after open reduction occurred in one hip and was treated with closed reduction on the first postoperative day.
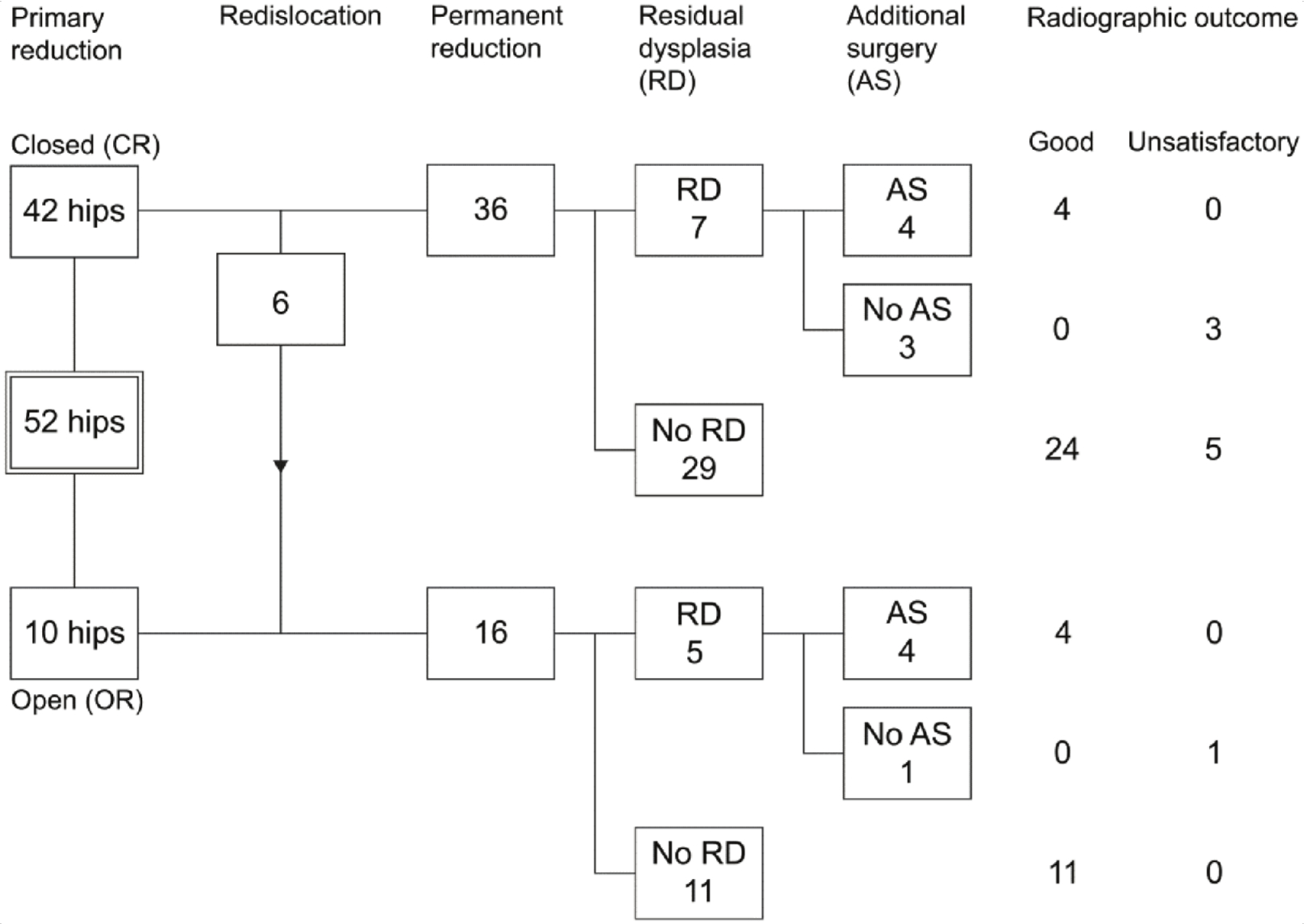
Figure 1
Flowchart of 52 hips with late-detected DDH, showing primary reduction, redislocation, permanent reduction, residual dysplasia, additional surgery, and radiological outcome at skeletal maturity.
AVN of the femoral head occurred in seven hips (13%). The distribution of AVN was group II in four hips and group III/IV in three hips. There was no significant association between the occurrence of AVN and closed reduction (three of 36 hips, 8%) or primary open reduction (one of ten hips, 10%). The highest occurrence of AVN (three out of six hips) was in the subgroup with primary closed reduction, early redislocation and subsequent open reduction. There were no significant associations between AVN and age groups at reduction or duration of preliminary traction.
Residual hip dysplasia (CE angle less than 15°) with or without subluxation during the follow-up period occurred in 12 hips (23%), five dysplasias and seven subluxations (Figure 1). Table I shows the association between residual dysplasia and potential prognostic variables. There were significant associations between residual dysplasia/subluxation and the following variables: occurrence of AVN, increased AI one and three years after reduction, and reduced femoral head coverage (reduced CE angle and increased MP) one and three years after reduction. No significant associations between residual dysplasia and traction time (more or less than one week), treatment groups or age groups at reduction were found. The rate of residual dysplasia was 18% in patients under 18 months of age at reduction and 36% in older patients (p = 0.189).
Table I.
Association between residual hip dysplasia/subluxation and clinical and radiological variables.
| Variables | Residual hip dysplasia/subluxation | ||
|---|---|---|---|
| No dysplasia | Dysplasia | p-value | |
| Age group at reduction | |||
| < 18 months | 31 (82%) | 7 (18%) | 0.189 |
| ≥ 18 months | 9 (64%) | 5 (36%) | |
| Traction time | |||
| 0 to 7 days | 13 (81%) | 3 (19%) | 0.622 |
| 8 to 27 days | 27 (75%) | 9 (25%) | |
| Treatment group | |||
| Closed reduction | 29 (81%) | 7 (19%) | 0.351 |
| Open reduction | 11 (69%) | 5 (31%) | |
| Avascular necrosis | |||
| No AVN | 37 (82%) | 8 (18%) | 0.021 |
| AVN | 3 (43%) | 4 (57%) | |
| AI at diagnosis (°) | 36.8 (5.4) | 39.3 (3.6) | 0.130 |
| AI 1 year f-up (°) | 23.7 (3.8) | 26.8 (5.0) | 0.026 |
| AI 3 years f-up (°) | 21.2 (3.8) | 24.8 (4.6) | 0.014 |
| MP at diagnosis (%) | 88.7 (26.8) | 100 (0) | 0.091 |
| MP 1 year f-up (%) | 11.9 (11.3) | 20.5 (14.9) | 0.045 |
| MP 3 years f-up (%) | 17.8 (8.2) | 29.9 (13.2) | 0.001 |
| CE 3 years f-up (°) | 18.5 4.9 | 11.1 (7.5) | 0.001 |
-
AVN, avascular necrosis; AI, acetabular index; f-up, follow-up time; MP, migration percentage; CE, centre-edge angle; categorical variables: number of hips (percentage); continuous variables: mean (SD).
Additional surgery for residual dysplasia/subluxation has been performed in eight hips (15%) at a mean patient age of 7.1 years (3.3 to 14.1). The surgical procedures were combined pelvic and femoral osteotomies in five hips (Figure 2), shelf operation and femoral osteotomy in two hips, and femoral osteotomy alone (varus and derotation) in one hip. The pelvic osteotomies were done with the Dega technique.25 The mean preoperative CE angle in the seven hips with combined pelvic and femoral operations was 8° (2 to 14). The mean CE angle one year postoperatively was 31° (23 to 45); thus, a mean correction of 23° (12 to 43) was obtained. Only one hip was operated on a second time (periacetabular osteotomy at patient age 14 years). Of the four hips that have not undergone surgical correction, two hips had acetabular dysplasia only and two also had subluxation. The patients with subluxation (CE angles 8° and 2°, respectively) have been recommended operative correction, but have so far refused surgery because they have no complaints from their hips.

Figure 2
a) Primary radiograph of a girl with dislocation of her left hip, with acetabular index 23° of the right hip and 40° of the left. Closed reduction was performed at an age of 19 months. b) Radiograph at an age of six years, showing residual dysplasia with subluxation of the left hip (CE angle 9°). Dega type pelvic osteotomy and femoral varus osteotomy with shortening were performed. c) Radiograph six weeks postoperatively showing good correction of the left hip. d) Radiograph at the last follow-up at an age of 17 years, showing adequate femoral head coverage (CE angle of left hip 21°).
The mean patient age at the last follow-up was 15.7 years (13 to 21). All the patients except one had closed epiphyseal lines of the acetabulum and proximal femur. Satisfactory radiological results (Severin grade 1 or 2) were obtained in 43 of the 52 hips (83%) (Figure 1). Lack of surgical correction of residual dysplasia was a risk factor for unsatisfactory outcome. All the eight hips with additional surgery had a good outcome whereas none of the four hips without additional surgery had a good outcome (p = 0.002). Age groups at reduction, duration of traction (more or less than one week), AVN, and closed vs. open reduction were not statistically associated with prognosis. In patients ≥ 18 months at reduction, the outcome was good in all the seven hips after open reduction and in six of seven after closed reduction.
Table II shows the radiological measurements from the time of diagnosis to skeletal maturity according to age groups at reduction. Only the measurements taken in the period before the subsequent operations were included for the eight hips with additional surgery. The mean acetabular index (AI) for all hips was 37.4° at the time of diagnosis and children less than 18 months had lower AI (36.3°) than older children (40.1°). There was a pronounced reduction in AI (mean 12.7°) during the first year after reduction, with no significant difference between age at reduction <18 months and ≥18 months (12.4° vs 13.4°; p = 0.536). AI continued to decrease in both age groups up to the last measurement at age 8 to 10 years (Figure 3), but to a lesser degree than the first year. At eight to ten years, AI was significantly higher in children ≥ 18 months of age at reduction compared with younger children.
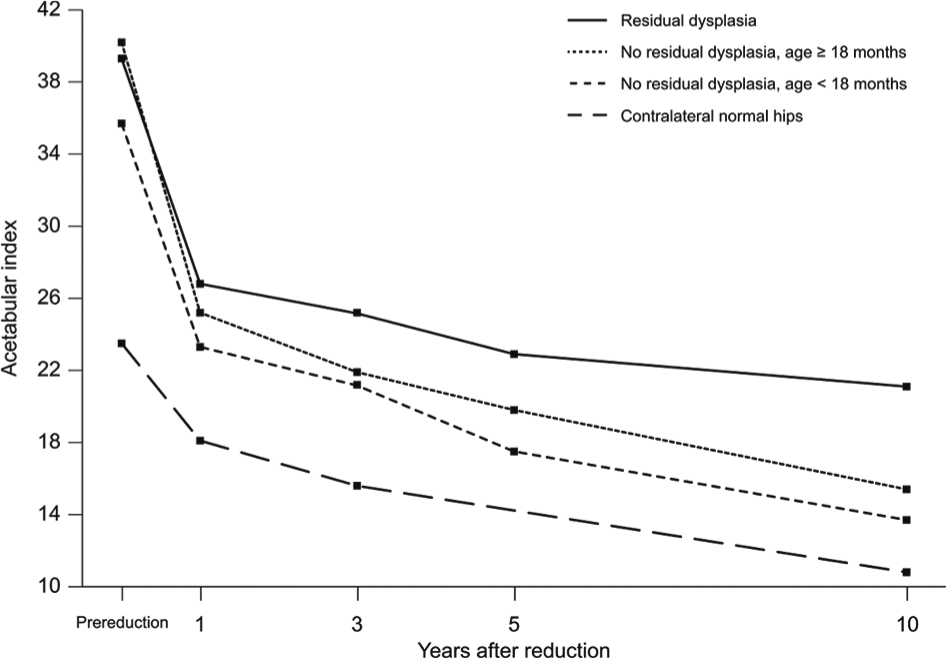
Figure 3
Development of the acetabular index from the prereduction radiograph to the radiograph at the age of ten years in four groups of hips: hips with residual dysplasia, hips without residual dysplasia (divided according to age under 18 months and ≥ 18 months at hip reduction), and contralateral normal hips.
Table II.
Radiological measurements at diagnosis and during follow-up according to age at hip reduction.*
| Age at reduction | ||||
|---|---|---|---|---|
| Parameters | All hips | < 18 months | ≥ 18 months | p-value |
| At diagnosis | ||||
| AI (°) | 37.4 (5.1) | 36.3 | 40.2 | 0.013 |
| MP (%) | 92.4 (22.4) | 91.5 | 93.4 | 0.831 |
| One year follow-up | ||||
| AI (°) | 24.5 (4.2) | 23.6 | 26.7 | 0.019 |
| Reduction in AI (°) | 12.7 (4.8) | 12.4 | 13.4 | 0.536 |
| MP (%) | 13.8 (12.5) | 14.3 | 12.6 | 0.670 |
| Three years follow-up | ||||
| AI (°) | 22.0 (4.2) | 21.6 | 23.8 | 0.067 |
| MP (%) | 20.1 (10.3) | 20.3 | 19.8 | 0.886 |
| CE angle (°) | 17.1 (6.1) | 17.2 | 16.9 | 0.902 |
| Age 8 to 10 years | ||||
| AI (°) | 15.2 (5.8) | 14.2 | 18.4 | 0.037 |
| MP (%) | 18.8 (8.0) | 19.4 | 17.1 | 0.419 |
| CE angle (°) | 22.3 (7.1) | 22.6 | 21.6 | 0.678 |
| Skeletal maturity | ||||
| MP (%) | 22.2 (8.2) | 23.7 | 17.3 | 0.029 |
| CE angle (°) | 24.5 (8.7) | 23.2 | 29.4 | 0.056 |
-
Results: mean (SD); AI, acetabular index; MP, migration percentage; CE angle, centre-edge angle; *only the follow-up examinations before surgery were included for the eight hips with late, additional operations.
MP decreased from 92% at diagnosis to 14% one year later. Thereafter, MP showed a moderate increase to a mean of 22% at skeletal maturity. The mean CE angle was 17° at the three-year follow-up and increased to 25° at skeletal maturity, and no statistically significant differences between the age groups occurred (Table II). There was a very good correlation between the parameters for measurement of femoral head coverage (MP and CE angle) at the follow-up examinations from three years after reduction to skeletal maturity, with correlation coefficients in the range of -0.83 to -0.95.
Discussion
Failure to maintain an initially acceptable closed reduction occurred in six of 42 hips (14%). This rate is rather high but is in accordance with the 13% to 15% failure rates reported by others.9,26 What could be the reasons for the failures? First, because the risk of AVN is increased by excessive hip abduction in the cast, the degree of abduction in these cases might have been insufficient to maintain stability. Secondly, we could have misjudged the position of the reduced hip at fluoroscopy and accepted a position that was not sufficiently concentric for maintenance of stability. This indicates that the strategy should be changed to open reduction in cases of doubt regarding the quality of closed reduction.
The rate of stable closed reduction was 69% (36 of 52 hips). This is in accordance with previous studies, where a range of 51% to 75% closed reduction was found after short-term or no preliminary traction.9,12,27,28 The rate of stable closed reduction decreases with increasing patient age. In children under 18 months of age, closed reduction was obtained in 76% of the present hips and in 83% of the hips reported by Sankar et al.11 In children aged 18 to 36 months, the rate of closed reduction was 50% of the present hips and 61% in a previous study.10 Another study confirms this trend,28 although the rates of closed reduction were somewhat lower (58% under 12 months and 36% at age 12 to 36 months). Although the individual rates differ, it seems that stable closed reduction after no or short-term traction is achieved in about two thirds of the hips in children under 18 months of age and in about half the hips at age 18 to 36 months.
The use of traction is controversial, partly because of different traction concepts. The aim of traction is important. Studies on long-lasting skin traction (four to eight weeks) in order to obtain gradual closed reduction, have reported less than 10% failures of reduction and good outcome in 83% to 96% of the hips at skeletal maturity.15,29,30 Before the present study started, a rather long period of skin traction (mean five weeks) to obtain gradual closed reduction, was the main method for late-detected DDH in our department.8 However, the disadvantages with long traction time are obvious. It is expensive, time-consuming, and inconvenient for the children and their families. Moreover, it requires competent and experienced nursing staff to ensure that the treatment is effective and to avoid skin complications. These were the reasons for the change to shorter traction periods of one to two weeks when we started this study. Then, the aim was not to obtain reduction, but to stretch the soft tissues in order to ease the subsequent reduction. A traction time of one week is unlikely to involve any positive effects and we found no significant associations between traction time of more or less than seven days and the rate of successful closed reduction or residual dysplasia. Therefore, preliminary traction, as it was used in the present study, probably has little or no efficacy. This is in accordance with the experience of two recent retrospective studies where a mean traction time of two to three weeks had no effect on the success rate of closed reduction.3,4 Since these studies were retrospective, this question should be further analyzed in a prospective randomized study including a sufficient number of patients.
An argument for using traction is reduced risk of AVN.1,2 However, others found no influence of preliminary traction on the rate of AVN.3,4 According to a review including seven studies of children under two years of age, the overall rate of AVN was 10%,31 which is in keeping with our rate of 13%.
The potential for osseous development of the acetabulum is maximal at birth and gradually declines thereafter. There is, however, no consensus regarding the rate of acetabular development according to age at reduction, a question that is relevant for the debate on residual acetabular dysplasia and the indications and timing of pelvic osteotomy. Salter14 maintained that normal development of the acetabulum after about 18 months of age is no longer assured even with the reduced hip in a stable position. This view is not supported by the present study, which showed a considerable potential for acetabular growth several years after reduction (Figure 4). AI was reduced by a mean of 12° to 13° during the first year and there was no significant difference between children less than 18 months and older children. A further mean decrease of 8° to 9° up to age eight to ten years was seen. This long-lasting improvement of the acetabulum is similar to that of previous studies, with a mean decrease in AI of 9° to 11° the first year and a further reduction for at least five years.19,32
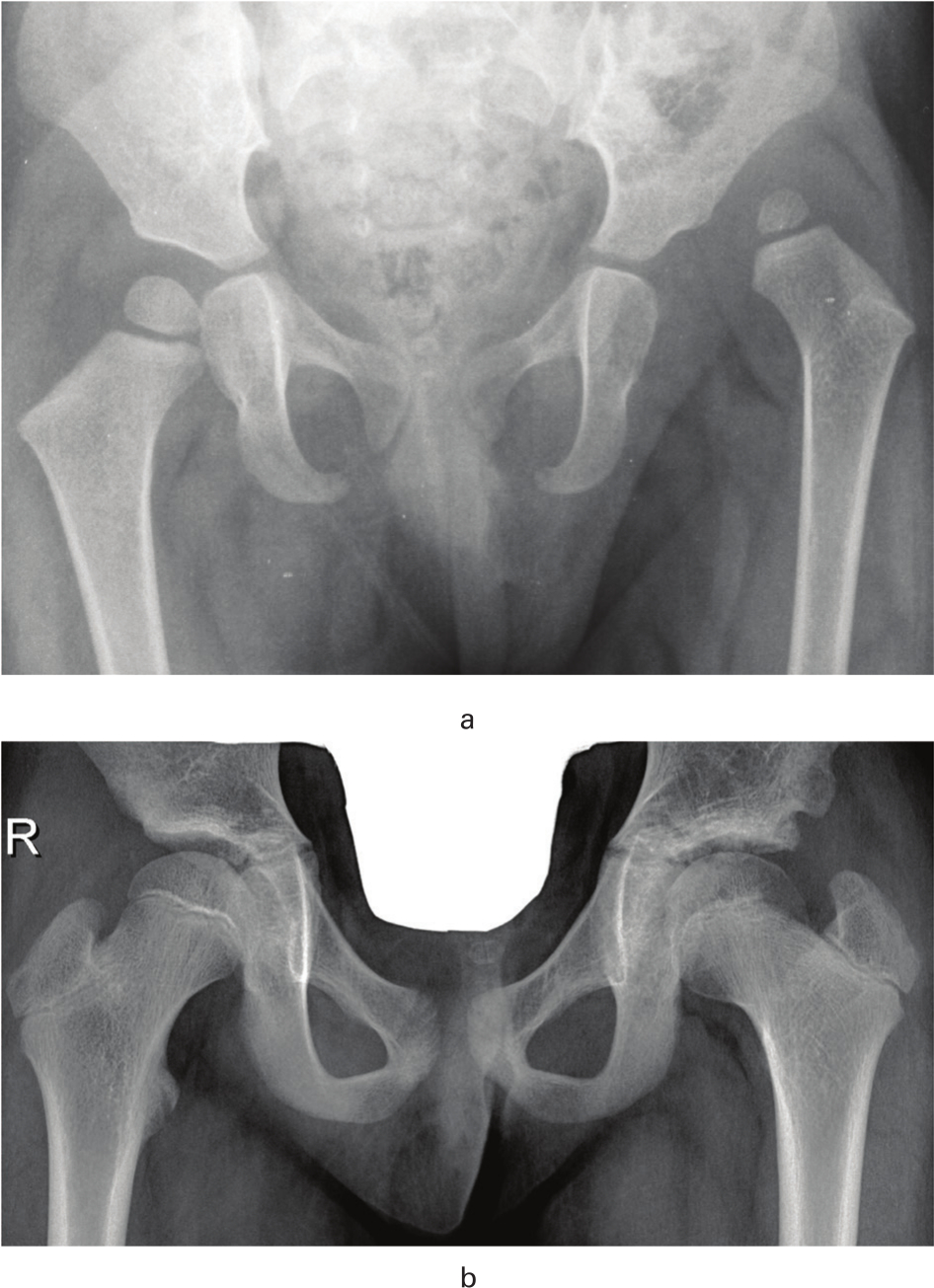
Figure 4
a) Primary radiograph of a girl with dislocation of her left hip, with acetabular index 23° of the right hip and 33° of the left. Redislocation occurred after closed reduction, and open reduction was performed at an age of 21 months. b) Radiograph at patient age ten years, showing marked improvement of the acetabulum (acetabular index 8°) and good femoral head coverage.
Although the acetabulum has a good ability to spontaneous improvement, residual dysplasia with or without subluxation sometimes occur. Different predictors for residual dysplasia have been reported. A high AI and reduced femoral head coverage the first years after reduction were predictors in the present study, supporting the findings of previous studies.12,32-35 High age at reduction was a predictor in some studies,12,32 but was not a significant risk factor in the present study or in other studies.35,36
The natural history of residual dysplasia was studied by Fu et al,35 showing that 87% of subluxated hips at age four to five years developed unsatisfactorily and became Severin 3/4 hips at skeletal maturity. Akagi et al33 studied acetabular development after open reduction and found that hips with residual dysplasia/subluxation at skeletal maturity had never been normal during the whole period of follow-up. A study with 45 years follow-up showed that the long-term prognosis of residual subluxation is poor, ending in osteoarthritis in almost every case, whereas the prognosis in dysplasia alone is considerably better.37 Thus, patients with residual subluxation that does not improve during the first years after reduction, should be recommended corrective surgery. In patients with dysplasia only, further follow-up is warranted, but surgery is indicated if deterioration to subluxation occurs or the patient experiences hip symptoms.
In the present study, further surgical correction with pelvic and femoral osteotomies has been performed in eight hips. In addition, surgical correction was indicated in two patients with subluxation, but since they so far have no complaints, surgery has been postponed. Thus ten out of 52 hips (19%) needed additional surgery. The frequency was higher in children aged ≥ 18 months at reduction (36%) than in children aged under 18 months (13%). Table III shows the rate of additional surgery in various studies. Since deterioration can occur in late childhood, studies with shorter than ten to 12 years follow-up should be taken with some caution. In children under two years of age at reduction, the rate of further surgery after preliminary traction under four weeks and closed reduction was 10% to 19%.9,13,26,38 The rate increased to 52% in children aged ≥ 18 months10 and 65% at age one to three years.12 Similar rates of additional operations have been found after open reduction: 22% in children under two years of age at reduction34 and 25% in the present study. Since the aim of Akagi et al33 was to evaluate the natural history of acetabular development after open reduction, no additional operations were performed during childhood, but five of 22 hips (23%) had residual subluxation at skeletal maturity. In conclusion, Table III indicates a trend to less frequent need of additional surgery in younger children.
Table III.
Late, additional surgery and final radiological results in various previous studies and in the present study.
| Authors | n, patients (hips) | Age (months) | Concurrent PO (% of hips) | Additional surgery (% of hips) | Follow-up (years) | Unsatisfactory outcome (% of hips) |
|---|---|---|---|---|---|---|
| Closed reduction | ||||||
| Race and Herring, 1983 | 48 (59) | 10 (0.2 to 24) | No | 17 | 7 (2 to 16) | 34 |
| Danielsson, 2000 | 71 (75) | 10 (2 to 64) | PO in 7% | 19 | 11 (6 to 18) | 1.5 |
| Cooke et al, 2010 | 42 (48) | 10 (2 to 20) | No | 13 | 11 (5 to 19) | 0 |
| Tennant et al, 2016 | 106 (113) | 9 (4 to 24) | No | 10 | ≥5 | 1 |
| Present study, 2019 | 35 (36) | 11.4 (3.5 to 33) | No | 17 | 14 (11 to 18) | 22 |
| Zionts et al, 1986 | (38) | 20 (13 to 36) | No | 65 | 12 (5 to 22) | 11 |
| Schoenecker et al, 1995 | 32 (38) | 23 (18 to 35) | No | 52 | 8.7 | 4 |
| Open reduction | ||||||
| Szepezi et al, 2013 | 45 (49) | 15 (6 to 24) | No | 22 | Skeletal maturity | 4 |
| Akagi et al, 1998 | 20 (22) | 14 (5 to 26) | No | 0 | 14 (12 to 19) | 36 |
| Present study, 2019 | 15 (16) | 17.4 (3 to 33) | No | 25 | 14 (11 to 21) | 6 |
| Ruszkowski and Pucher, 2005 | 26 (33) | 15 (6 to 24) | PO (Dega) | 0 | 9.4 (5 to 14.5) | 21 |
| Carsi et al, 2014 | 48 (55) | 15 (7 to 31) | Acetabuloplasty | 4 | 4 (2 to 8) | Short follow-up |
| Chang et al, 2015 | 63 (63) | 22 (18 to 33) | PO (Salter) | 5 | 10.8 | 14 |
| Gholve et al, 2012 | 42 (49) | 31 (15 to 92) | PO in 67% | 49 | 9.7 (5 to 17) | 8% |
| " | (15) | PO | 73 | |||
| " | (12) | No | 67 | |||
-
PO, pelvic osteotomy; unsatisfactory outcome, Severin grades 3/4.
We found a good effect of combined pelvic and femoral osteotomies on further hip development. This is in accordance with the experience of Gholve et al,36 who had a very high rate of additional pelvic and/or femoral osteotomies (49%), but only 8% of the hips had unsatisfactory outcome at ten-years follow-up.
For patients above the age of 18 months, concurrent pelvic osteotomy at the time of open or closed reduction has become common practice in many hospitals.14-16,36 This policy involved decreased use of additional surgery.16,39 Surprisingly, in a study of somewhat older patients (mean age 31 months at reduction), Gholwe et al36 found no significant difference in further surgery between hips with open reduction alone and hips with open reduction and concurrent pelvic osteotomy. Some studies have recommended concurrent pelvic osteotomy even in younger patients, down to six months of age.17,18 However, the problem of residual subluxation was not solved, since Ruszkowski and Pucher17 had 25% subluxations at the last follow-up in children under 12 months of age at reduction. Based on the marked spontaneous improvement of the acetabulum, we do not recommend concurrent pelvic osteotomy. It would have implied unnecessary pelvic surgery in the majority of the hips, since 40 out of 52 hips did not develop residual dysplasia/subluxation. Moreover, pelvic osteotomy in children less than one year would seem to be technically rather difficult.
Satisfactory radiological results (Severin grades 1/2) at skeletal maturity were obtained in 83% of the present hips, and there was no statistically significant difference between hips with open and closed reduction. Previous studies in children aged one to three years have shown unsatisfactory results (Severin 3/4) in 0% to 34% after closed reduction and in 4% to 36% after open reduction without concurrent pelvic osteotomy (Table III). This indicates quite good long-term prognosis when residual dysplasia/subluxation is corrected by late, additional osteotomies.
Limitations of the present study are that there was no control group without traction and that the number of patients is rather small, which might make the statistics, especially of the subgroups, less reliable. The main strength of the study is that it represents a consecutive series of patients that were followed prospectively, with only one patient lost to follow-up.
What are the clinical consequences of this study? A short period of skin traction had hardly any positive effects, but we shall not reintroduce our previous practice of long traction period for the reasons given. Thus, we recommend no preliminary traction. Gentle closed reduction can be attempted in children up to three years of age but is likely to be less successful in children over 18 months of age. If reduction fails, open reduction under the same anaesthesia can be performed. There is a marked trend to spontaneous improvement of the acetabulum after reduction, even in patients over 18 months of age and therefore simultaneous pelvic osteotomy is not always necessary. Residual subluxation should be treated with pelvic osteotomy if spontaneous normalization does not take place during the first years after reduction.
References
1. Salter RB , Kostuik J , Dallas S . Avascular necrosis of the femoral head as a complication of treatment for congenital dislocation of the hip in young children: a clinical and experimental investigation . Can J Surg . 1969 ; 12 : 44 - 61 . PubMed Google Scholar
2. Sibiński M , Murnaghan C , Synder M . The value of preliminary overhead traction in the closed management of DDH . Internat Orthop (SICOT) . 2006 ; 30 : 268 - 271 . Crossref PubMed Google Scholar
3. Li Y-Q , Li M , Guo Y-M , et al. Traction does not decrease failure of reduction and femoral head avascular necrosis in patients aged 6-24 months with developmental dysplasia of the hip treated by closed reduction: a review of 385 patients and meta-analysis . J Pediatr Orthop B . 2019 ; 28 : 436 - 441 . Google Scholar
4. Sucato DJ , De La Rocha A , Lau K , Ramo BA . Overhead Bryant's traction does not improve the success of closed reduction or limit AVN in developmental dysplasia of the hip . J Pediatr Orthop . 2017 ; 37 : e108 - e113 . Crossref PubMed Google Scholar
5. Fish DN , Herzenberg JE , Hensinger RN . Current practice in use of prereduction traction for congenital dislocation of the hip . J Pediatr Orthop . 1991 ; 11 : 149 - 153 . Crossref PubMed Google Scholar
6. Alves C , Truong WH , Thompson MV , et al. Diagnostic and treatment preferences for developmental dysplasia of the hip: a survey of EPOS and POSNA members . J Child Orthop . 2018 ; 12 : 236 - 244 . Crossref PubMed Google Scholar
7. Malvitz TA , Weinstein SL . Closed reduction for congenital dysplasia of the hip. Functional and radiographic results after an average of thirty years . J Bone Joint Surg [Am] . 1994 ; 76-A : 1777 - 1792 . Crossref PubMed Google Scholar
8. Terjesen T , Halvorsen V . Long-term results after closed reduction of late-detected hip dislocation: 60 patients followed up to skeletal maturity . Acta Orthop Scand . 2007 ; 78 : 236 - 246 . Google Scholar
9. Race C , Herring JA . Congenital dislocation of the hip: an evaluation of closed reduction . J Pediatr Orthop . 1983 ; 3 : 166 - 172 . Crossref PubMed Google Scholar
10. Schoenecker PL , Dollard PA , Sheridan JJ , Strecker WB . Closed reduction of developmental dislocation of the hip in children older than 18 months . J Pediatr Orthop . 1995 ; 15 : 763 - 767 . Crossref PubMed Google Scholar
11. Sankar WN , Gornitzky AL , Clarke NMP , et al. Closed reduction for developmental dysplasia of the hip: early-term results from a prospective, multicentre cohort . J Pediatr Orthop . 2019 ; 39 : 111 - 118 . Google Scholar
12. Zionts LE , MacEwen GD . Treatment of congenital dislocation of the hip in children between the ages of one and three years . J Bone Joint Surg [Am] . 1986 ; 68-A : 829 - 846 . PubMed Google Scholar
13. Cooke SJ , Rees R , Edwards DL , Kiely NT , Evans GA . Ossification of the femoral head at closed reduction for developmental dysplasia of the hip and its influence on the long-term outcome . J Pediatr Orthop B . 2010 ; 19 : 22 - 26 . Crossref PubMed Google Scholar
14. Salter RB . Innominate osteotomy in the treatment of congenital dislocation and subluxation of the hip . J Bone Joint Surg [Br] . 1961 ; 43-B : 518 - 539 . Google Scholar
15. Morin CM , Bisogno J , Kulkarni S , Morel G . Treatment of late-presenting Developmental dislocation of the hip by progressive orthopaedic reduction and innominate osteotomy. Our results with more than 30 years of follow up . J Child Orthop . 2011 ; 5 : 251 - 260 . Google Scholar
16. Chang CH , Yang WE , Kao HK , et al. Prognostic radiographic factors in developmental dysplasia of the hip following Salter osteotomy . J Pediatr Orthop B . 2015 ; 24 : 31 - 34 . Crossref PubMed Google Scholar
17. Ruszkowski K , Pucher A . Simultaneous open reduction and Dega transiliac osteotomy for developmental dislocation of the hip in children under 24 months of age . J Pediatr Orthop . 2005 ; 25 : 695 - 701 . Crossref PubMed Google Scholar
18. Carsi B , Al-Hallao S , Wahed K , Page J , Clarke NMP . Incomplete periacetabular Acetabuloplasty: a one-stop procedure for developmental dysplasia of the hip . Acta Orthop . 2014 ; 85 : 66 - 70 . Google Scholar
19. Lindstrom JR , Ponseti IV , Wenger DR . Acetabular development after reduction in congenital dislocation of the hip . J Bone Joint Surg [Am] . 1979 ; 61-A : 112 - 117 . PubMed Google Scholar
20. Kleinberg S , Lieberman HS . The acetabular index in infants in relation to congenital dislocation of the hip . Arch Surg . 1936 ; 32 : 1049 - 1054 . Google Scholar
21. Reimers J . The stability of the hip in children . Acta Orthop Scand . 1980 (Suppl 184); 51 : 4 - 91 . Crossref PubMed Google Scholar
22. Wiberg G . Studies on dysplastic acetabula and congenital subluxation of the hip joint . Acta Chir Scand . 1939 ( Suppl 58 ); 83 : 7 - 135 . Google Scholar
23. Kalamchi A , MacEwen GD . Avascular necrosis following treatment of congenital dislocation of the hip . J Bone Joint Surg [Am] . 1980 ; 62-A : 876 - 888 . PubMed Google Scholar
24. Severin E . Contribution to the knowledge of congenital dislocation of the hip joint . Acta Chir Scand . 1941 ( Suppl 63 ); 84 : 1 - 142 . Google Scholar
25. Karlen JW , Skaggs DL , Ramachandran M , Kay RM . The Dega osteotomy: a versatile osteotomy in the treatment of developmental and neuromuscular hip pathology . J Pediatr Orthop . 2009 ; 29 : 676 - 682 . Crossref PubMed Google Scholar
26. Tennant SJ , Eastwood DM , Calder P , Hashemi-Nejad A , Catterall A . A protocol for the use of closed reduction in children with developmental dysplasia of the hip incorporating open psoas and adductor releases and a short-leg cast . J Bone Joint Surg [Br] . 2016 ; 98-B : 1548 - 1553 . Crossref PubMed Google Scholar
27. Alassaf N . Prediction of the requirement of open reduction for developmental dysplasia of the hip . J Internat Med Res . 2018 ; 46 : 54 - 61 . Crossref PubMed Google Scholar
28. Kahle WK , Anderson MB , Alpert J , Stevens PM , Coleman SS . The value of Preliminary traction in the treatment of congenital dislocation of the hip . J Bone Joint Surg [Am] . 1990 ; 72-A : 1043 - 1047 . PubMed Google Scholar
29. Kaneko H , Kitoh H , Mishima K , Matsushita M , Ishiguro N . Long-term outcome of gradual reduction using overhead traction for developmental dysplasia of the hip over 6 months of age . J Pediatr Orthop . 2013 ; 33 : 628 - 634 . Crossref PubMed Google Scholar
30. Rampal V , Sabourin M , Erdeneshoo E , et al. Closed reduction with traction for developmental dysplasia of the hip in children aged between one and five years . J Bone Joint Surg [Br] . 2008 ; 90-B : 858 - 863 . Crossref PubMed Google Scholar
31. Bradley CS , Perry DC , Wedge JH , Murnaghan ML , Kelley SP . Avascular necrosis following closed reduction for treatment of developmental dysplasia of the hip: a systematic review . J Child Orthop . 2016 ; 10 : 627 - 632 . Crossref PubMed Google Scholar
32. Albinana J , Dolan LA , Spratt KF , et al. Acetabular dysplasia after treatment for developmental dysplasia of the hip . J Bone Joint Surg [Br] . 2004 ; 86-B : 876 - 886 . Crossref PubMed Google Scholar
33. Akagi S , Tanabe T , Ogawa R . Acetabular development after open reduction for developmental dislocation of the hip . Acta Orthop Scand . 1998 ; 69 : 17 - 20 . Crossref PubMed Google Scholar
34. Szepesi K , Scücs G , Szeverenyi C , Csernatony Z . Long-term follow-up of DDH patients who underwent open reduction without a postoperative cast . J Pediatr Orthop B . 2013 ; 22 : 85 - 90 . Crossref PubMed Google Scholar
35. Fu Z , Yang JP , Zeng P , Zhang ZL . Surgical implications for residual subluxation after closed reduction for developmental dislocation of the hip: a long-term follow-up . Orthop Surg . 2014 ; 6 : 210 - 216 . Crossref PubMed Google Scholar
36. Gholve PA , Flynn JM , Garner MR , Millis MB , Kim YJ . Predictors for secondary procedures in walking DDH . J Pediatr Orthop . 2012 ; 32 : 282 - 289 . Crossref PubMed Google Scholar
37. Terjesen T . Residual hip dysplasia as a risk factor for osteoarthritis in 45 years follow-up of late-detected hip dislocation . J Child Orthop . 2011 ; 5 : 425 - 431 . Google Scholar
38. Danielsson L . Late-diagnosed DDH: a prospective 11-year follow-up of 71 consecutive patients (75 hips) . Acta Orthop Scand . 2000 ; 71 : 232 - 242 . Crossref PubMed Google Scholar
39. Kothari A , Grammatopoulos G , Hopewell S , Theologis T . How does bony surgery affect results of anterior open reduction in walking-age children with developmental hip dysplasia? Clin Orthop Relat Res . 2016 ; 474 : 1199 - 1208 . Crossref PubMed Google Scholar
Author contributions
T. Terjesen: Planned and executed the study, Wrote the manuscript.
J. Horn: Participated in the follow-up of the patients, Revised the manuscript.
©2020 Author(s) et al. This is an open-access article distributed under the terms of the Creative Commons Attributions licence (CC-BY-NC-ND), which permits unrestricted use, distribution, and reproduction in any medium, but not for commercial gain, provided the original author and source are credited.









