Abstract
The use of robotics in arthroplasty surgery is expanding rapidly as improvements in the technology evolve. This article examines current evidence to justify the usage of robotics, as well as the future potential in this emerging field.
Robots and robotic technology are a source of human fascination. Aristotle (322BC) dreamt of robots, and Leonardo da Vinci (1495AD) designed one.1 Currently, there are numerous commercially available and developmental robotic devices for all types of hip and knee arthroplasty. These devices have varying levels of evidence to support their usage; perhaps the most pertinent question is, have robots reached the stage where they are relevant to orthopaedics today?
Responsible introduction of new technology is now considered essential following various implant failures in the recent past. Malchau proposed a now widely accepted stepwise algorithm for this purpose.2 This involves:
1. Initial preclinical testing
2. Small randomised trials with sensitive outcome measures (e.g. RSA)
3. Larger clinical studies
Once these stages have been completed, multicentre trials followed by Registry studies should be undertaken.
This review will examine how robotic technology has been introduced to the competitive orthopaedic market, and what the evidence is to support its use.
Background
A robot is a machine capable of carrying out a complex series of actions automatically, especially one programmable by a computer. Robots of many kinds have become commonplace since the first industrial robot was installed in 1961 to unload parts from a die casting operation.
More recently there has been a surge of interest in robotic surgery, led by the da Vinci robot (Intuitive Surgical, Sunnyvale, CA, USA). This allows a surgeon to remotely control laparoscopic instruments with increased precision and dexterity.3-5 The usage of this robot has increased from around 200 000 procedures per annum in 2009 to over 550 000 procedures worldwide in 2014.6 This still represents only a very small percentage of the total number of similar procedures performed using traditional methods, but the growth in the usage of this technology is forecast to continue at a rapid rate.
The use of robotics in joint arthroplasty has developed immensely over the past 30 years and differs in concept from the da Vinci robotic surgery. The relative rigidity of bone allows pre-operative imaging and pre-planning of bony cuts, essentially enabling the robot to perform large sections of the surgery in an automated manner. Intra-operative adjustment of the plan according to the patient’s soft tissues can generally be made, and it is this precision and accuracy of adherence to the surgeon’s plan by the robotic cutting tools that is the major proposed benefit of robotic-assisted joint arthroplasty surgery.
History
The first robot designed for orthopaedics, and total hip arthroplasty (THA) in particular, was the ROBODOC (Think Surgical, Fremont CA., USA) system. This was a collaboration between the IBM Watson Center and UC Davis in 1986. The system underwent dry bone and cadaveric validation over the next six years, until the first patient had a THA with the femoral canal milled by an autonomous robot in 1992.7 During this time, the team at University of Washington had demonstrated the concept of cutting a distal femur for total knee arthroplasty (TKA), utilising an industrial robot on bone models in a theatre environment.8 ROBODOC was later modified for use in TKA.9 The CASPAR (OrthoMaquet, Rastatt, Germany) system followed hot on ROBODOC’s heels in 199910, and this was also designed for femoral preparation in THA. This system was then developed again to be used for bony cuts of TKA.11
In 2001, the first paper was published describing surgery with robotic assistance in unicompartmental knee arthroplasty (UKA) utilising the Acrobot (Imperial College, London, UK).12 A simple system consisting of a robotic surgical arm with a burr as the end effector, it required the rigid fixation of limb to a frame, a significant drawback in the operating theatre.

Fig. 1a
Fig. 1a. Stryker Mako robot with hip reamer attachment.

Fig. 1b
Fig. 1b. Mako hip planning screen.
(Images courtesy of Stryker).
In 2006, Mako Surgical (Fort Lauderdale, FL, USA) first implanted UKA and then patellofemoral arthroplasties with its RIO robotic arm device,13,14 and since then the use of robotic technology in arthroplasty has continued to expand with over 80 000 procedures now performed worldwide.15,16
Classification
Robotic systems in arthroplasty have previously been classified into three broad types: fully automated, semi-automated and passive.17
Fully automated systems require registration and complete soft-tissue exposure to be performed by the surgeon. The robot then completes the bony resections autonomously. The only commercially available system of this type is ROBODOC. This device requires the patient’s limb to be rigidly fixed to the robot. Pre-operative planning is performed on the workstation (ORTHODOC), and requires previously acquired CT images. The planned bone resection is then performed autonomously by the robotic burr. The surgeon can stop the cutting process, but the control of the cuts is determined exclusively by the surgical plan. Attempts have been made to produce smaller automated cutting robots that attach to the bone (MBARS and HyBARS,18,19 but they are not yet available for clinical use.
Semi-automated robotic technology consists of robotic arm-assisted devices and handheld navigated cutting tools. The Mako robotic arm-assisted surgical system, like the ROBODOC, also requires the use of a pre-operative CT image (see Figs 1a, 1b). From this, a basic surgical plan is made, but this is then adjusted intra-operatively, by the surgeon, allowing for fine adjustments to the patient’s soft-tissue balance and intra-operative findings. The cutting tool is attached to the end of the robotic arm which then guides the surgeon into a determined surgical field and haptically prevents the surgeon from moving the cutting tool outside the planned field of surgical resection. The cutting tool is controlled by the surgeon within robotically applied limits. Although these machines could be programmed to act autonomously, they remain surgeon-controlled to allow better protection of soft tissues without extensive exposure.
The Navio PFS (Blue Belt Technologies, Plymouth, MN, USA) is the most widely available handheld semi-automated robotic device, although, by strict definition, not truly a robot, as the cutting tool is moved entirely by the surgeon. The computer will only allow the cutting tool to operate when it is within a planned resection zone. This technology is currently image-free using anatomic registration, in much the same way as image-free computer navigation systems.
Passive robotic systems involve an automated form of computer-assisted planning of surgical cuts. Following this planning, the robotic device is attached to the bone and the device then moves a cutting block to the planned position, allowing the surgeon to make the planned resection through the cutting block using a standard surgical oscillating saw. The Praxim (OMNIlife Science, Inc, East Taunton, MA, USA) is the most common example of this type of robotic application (see Figs 2a, 2b, 2c).
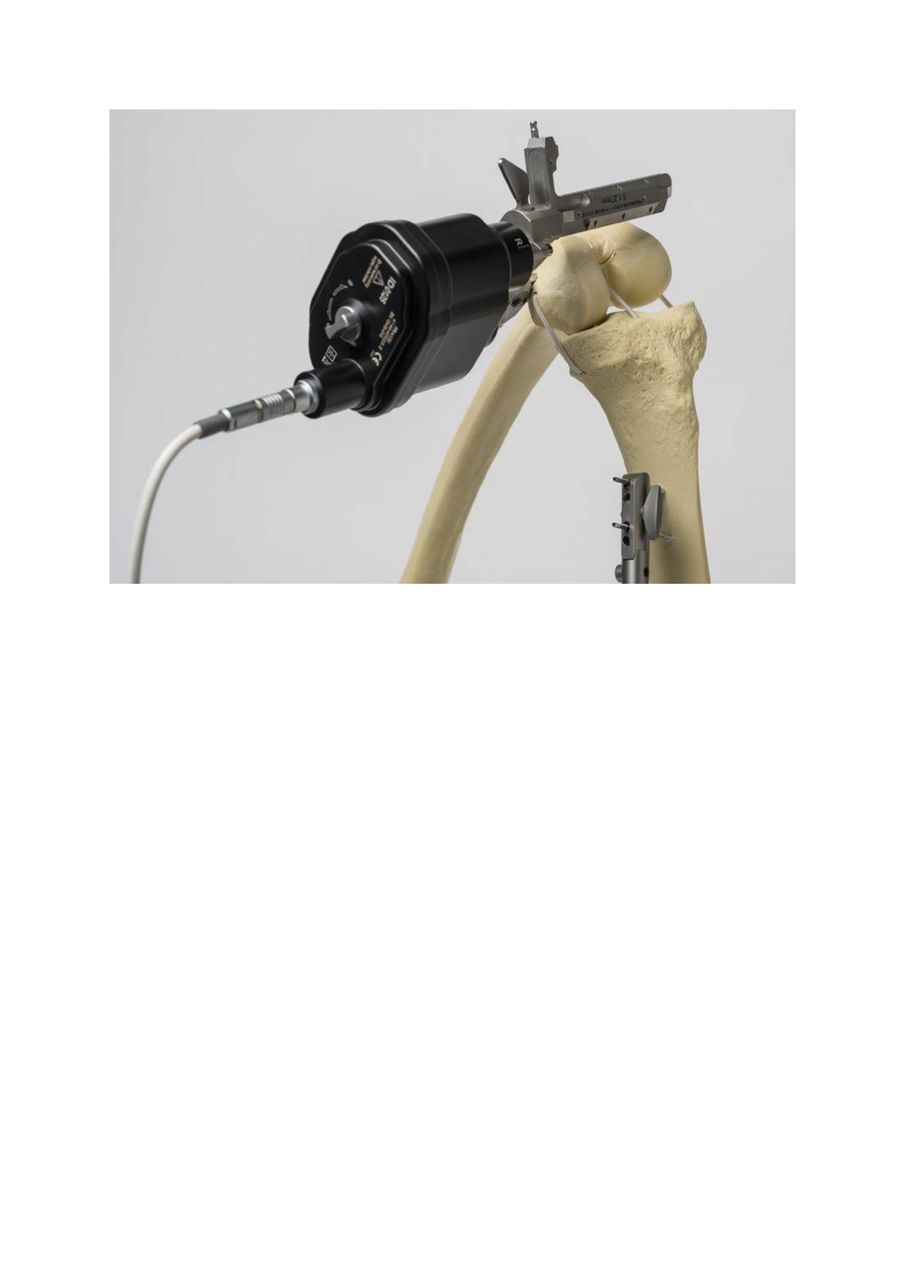
Fig. 2a
Fig. 2a. OmniNav station with computer and camera sensor to drive Praxim.

Fig. 2b
Fig. 2b. Praxim femoral planning screen.

Fig. 2c
Fig. 2c. Praxim Robot with placement on bone model.
(Images courtesy of Omnis).
The system is imageless, relying on anatomic registration. The surgeon determines the angle of cuts to be made, and the Praxim system moves the cutting block to the desired position autonomously. However, this system will only make the femoral cuts for a TKA.
Robotics in total hip arthroplasty
At present, THA can be performed utilising either the ROBODOC or Mako systems. The ROBODOC system is able to plan the acetabular and femoral component positions and the robot can then mill the femoral canal, while the surgeon manually reams the acetabulum. The Mako system does the reverse. It also plans the placement of both components, but then the robot only controls reaming of the acetabulum and placement of the cup. The surgeon is then able to identify the position of the planned surgical neck cut. This is performed manually, as is the femoral canal broaching and femoral prosthesis insertion.
ROBODOC has demonstrated precision in the milling of the femoral canal, achieving accurate femoral component position,20 and a reduction of intra-operative embolic events.21 Perhaps most interestingly, and likely due to the accuracy of femoral canal preparation, the system has been demonstrated to result in less post-operative stress shielding and bone loss in the proximal femur.22 There is however a flipside, with a documented increase in operative time and blood loss.20 Earlier versions of this robot were found to have high complication rates including femoral fracture, although these have been ironed out and are not reported in more recent series with newer generation machines.
Surgeons utilising the RIO system have been able to implant 100% of acetabular cups within 10° of intended position, both in anteversion and inclination.23 Biter et alalso demonstrated equivalence in leg length restoration with this system when compared with standard techniques.24 As yet, however, there are no published studies showing improved clinical or other outcomes with this technology over standard procedures.
Robotics in THA has only just passed the initial step in the responsible introduction of technology. Preclinical tests of accuracy and early case series are available. No long-term clinical outcomes or RCTs have been produced, and robotic applications in THA remain niche with no widespread release of this technology into a country with a robust national joint registry.
Robotics in total knee arthroplasty
Currently only RoboDoc and Praxim are commercially available for use in TKA, however, neither system has been widely utilised for this application.
ROBODOC pre-operatively plans the bony cuts on its workstation from CT imaging. The femur and tibia are then rigidly fixed directly to the robot and the knee distracted with an external fixator to allow adequate exposure for the robot to work. In a similar manner to a commercial lathe or router, this plan is then executed by the robotic end effector burr.
Most of the data published on robotic-assisted TKA relate to these autonomous robots. Both the CASPAR and ROBODOC robots have been shown to increase precision and accuracy significantly compared with conventional manual techniques, reducing the number of patients that are considered outliers in terms of accuracy of implantation (+/- 3° from mechanical axis).25-27 Song et al published a randomised controlled trial reporting a significant improvement in soft-tissue balance with 94% versus 80% having balanced rectangular flexion/extension gaps.28 However, clinical outcome studies thus far have reported no difference when comparing robotic TKA with conventional techniques.25,29 Things are not always rosy, however; earlier reports of the autonomous robotic TKA clinical series noted unacceptably high incidences of soft-tissue damage and requirement to abort the robotic procedures (3%-33%).30
The designers of the Praxim system reported initial cadaveric studies demonstrating small improvements in accuracy of bone cuts with this automated cutting block, when compared with standard computer-assisted techniques. A retrospective clinical case series comparing standard techniques with TKA utilising the Praxim system demonstrated a 0.5° smaller error of alignment when compared with computer-assisted TKA.31 All published studies report decreased time required to make femoral cuts with this system compared with standard computer navigation techniques.32 Overall tourniquet time is not decreased, presumably due to the time to insert the device into the distal femur.
This story is very similar to THA with a range of preclinical studies on surgical accuracy and selected early case series available for robotic use in TKA. There are no long-term clinical outcome studies or RCTs available, and this technology is not present within any of the substantial joint registries, worrying considering the 80 000 procedures now performed for all joint replacement types and counting!
Robotics in partial knee arthroplasty
Robotics has been most widely deployed in partial knee replacements. The relative simplicity of achieving soft tissue balance by tensioning the collateral ligament and the small amount of bone resection required made UKA particularly suited to robotic applications. Difficulties of access and accuracy of traditional methods of implantation combined with the nature of semiconstrained systems which lend themselves to unicompartmental knee replacements. Both of the commercially available semi-autonomous systems are marketed for this purpose. There is a slight difference in that the Mako system is a closed system that can utilise only the implants from the parent company, whereas the Navio PFS is a semi-open system with partnership agreements allowing a number of different companies’ implants to be inserted using the robotic assistance (see Figs 3a, 3b, 3c). The Mako system revolves around pre-operative CT images to allow intra-operative simulated implantation and adjustment to operative plans to achieve soft-tissue balance. The Navio PFS uses landmark registration and balances the knee in a similar manner to standard conventional techniques of gap balancing. Both systems use a burr as the end effector to make the femoral and tibial bone resections. Prostheses are inserted manually after preparation of the femoral and tibial surfaces by the robotic cutting device.
The Mako system has also given surgeons the ability to perform a patellofemoral arthroplasty in conjunction with a UKA without an excessive increase in operative time.33 This process can be planned simultaneously and is a relatively easy addition to the surgery. This utilises non-linked implants allowing the individual compartments to be aligned independently – certainly a controversial and thought-provoking technique.
Improved accuracy and alignment have been demonstrated in multiple studies of the RIO robotic system.34,35 Karia et al demonstrated a diminished learning curve and more accurate implantation of UKA on dry bones with the RIO system compared with conventional techniques in the hands of inexperienced surgeons.36 Coon et al retrospectively compared their first 36 UKA with the MAKO system with 45 previous manually instrumented UKAs.34 There was no clinical difference in outcome measured up to 12 weeks post-surgery. The Navio PFS for UKA has been validated for accuracy on bone models and cadaveric studies37,38 and these studies have been able to demonstrate improved precision and accuracy compared with conventional techniques.

Fig. 3a
Fig. 3a. Navio PFS handpiece.

Fig. 3b
Fig. 3b. Navio cart with computer and sensor.

Fig. 3c
Fig. 3c. Navio PFS femoral cutting guidance screen.
(Images courtesy of BlueBelt Technologies).
There are two studies, however, that do not support the theory of robotic UKA improving accuracy of implantation and alignment. Jaffray et al demonstrated on bone models that PSI was equivalent to robotic surgery (Sculptor) with respect to accuracy and alignment.39 This is yet to be replicated in a clinical setting. Hansen et al reported a retrospective single-surgeon series that did not demonstrate significant differences between robotic UKA (Mako) and manually instrumented UKR utilising extramedullary guides.40
The use of robotic technology for UKA is currently supported by preclinical data and case series with short-term follow-up. There are currently no long-term randomised controlled trials comparing robotic technology with conventional techniques, and long-term data have sadly not been published on any case series. This technology has only recently been utilised in Australia and it will be at least three years before any meaningful data could be extracted from the Australian National Joint Replacement registry. As with other indications, there remains a significant evidence gap for utilisation of this technology.
Research and development
It would be impossible to mount an evidence-based argument on the cost-effectiveness and the clinical benefit of robotic hip and knee arthroplasty currently. The evidence regarding clinical outcomes is only short-term, and not clearly in favour of robotics. However, there is a compelling argument for the use of robotic technology in the research and development of hip and knee arthroplasty.
Computer navigation is the most accurate technology widely available for hip and knee arthroplasty. This still has small cumulative errors that occur at every step from registration through to implantation. The purity of being able to accurately implant prostheses at the planned position and alignment would enable surgeons to minimise the ‘white noise’ due to inaccuracy that occurs when studying differences in alignment philosophies.
For 30 years, TKAs have been inserted perpendicular to the mechanical axis due to the concern regarding mechanical failure of implants that were outliers due to inaccurate implantation. Patient-specific instrumentation for kinematic axis has been abandoned at least in part due to inaccuracy of the cutting guides rather than evidence against the alignment theory. This technology would be perfectly suited to the evaluation of different alignment methods in TKA.
As surgeons, we are all aware of individual differences in pelvic and lumbar spine anatomy and mobility. Yet 40 years after THA became part of clinical practice we are still not able to individualise the placement of hip replacement components with any degree of certainty or accuracy. This is another area in which the accuracy of implantation afforded by robotic technology would benefit further research and may offer particular benefit in patients with abnormal geometry.
In addition to simply making more accurate cuts, robotic technology has the ability to make different types of cuts. The ability to burr three-dimensional shapes allows manufacturers and designers greater freedom of design. This may initially be more applicable to custom designs in revision situations with bone loss. In the future, with improvements to manufacturing techniques, such as 3D printing, the possibility of more bone-sparing individualised custom designs may become a reality – the very shape of a knee or hip replacement is determined as much by the instrumentation to implant as the biology they are trying to replicate. A mature robotic surgical technology would potentially remove the constraints of a flat saw blade and round reamer.
Health economic cost implications
There is a significant capital cost associated with using robotic technology for joint arthroplasty. This cost is currently funded by the hospital, or academic institution involved. This may be recouped through donations to research funds, but more commonly increased income or reduction by the hospital is required to justify the expense. Initially the costs were justified with decreased length of stays,41 however, these are now a standard element of care, and hospitals are requiring increased patient numbers to offset the cost.
There is a public perception that advanced technologies such as robotics produce better results.42 This is both a strength and weakness of the use of robotics in arthroplasty. Patient support and interest is likely to be easily achieved. Australia is an example of this phenomenon with much higher rates of uptake of computer navigation than elsewhere in the world. Currently 24% of TKAs in Australia are performed with computer assistance.43 If this public perception leads to hospitals needing to purchase the technology to maintain market share, it could lead to an escalation of overall costs, which would eventually fall back on our patients either through increased taxes or insurance premiums.
It is this public perception that will be very difficult to influence. Surgeons need to ensure that they continue to utilise the technology only on suitable patients (particularly with respect to UKA). This technology has the potential to be aggressively marketed to our patients, as various implants and techniques have been in the past. The marketing of this technology needs to be carefully monitored by the national orthopaedic associations and regulatory bodies.
Conclusion
The available evidence strongly suggests that robotic-assisted arthroplasty achieves more accurately implanted hip and knee prostheses. The potential associated benefits of improved function and longevity are, however, yet to be proven.
It is apparent that this technology currently results in increased cost and operating time. This will only be acceptable to surgeons, hospitals, governments, and insurers if robotic-assisted surgery results in improved patient outcomes. Only through responsible introduction of this technology, as outlined by Malchau, can the use of robotics be justified. This requires randomised controlled trials, followed by multicentre trials and eventually registry results.
Robotics in joint arthroplasty has vast potential. It is our responsibility as surgeons to ensure that we assess this potential for the benefit of our patients. The onus remains on early adopters of robotic technology to demonstrate the presence and extent of any improved clinical outcomes. With advances in technology and diminishing costs in the future, it is difficult to believe robotics will not be part of future arthroplasty surgery.
1 Yates DR, Vaessen C, Roupret M. From Leonardo to da Vinci: the history of robot-assisted surgery in urology. BJU Int 2011;108:1708-1713; discussion 1714. Google Scholar
2 Malchau H. On the importance of stepwise introduction of new hip implant technology: assessment of total hip replacement using clinical evaluation, radiostereometry, digitised radiography and a national hip registry. [PhD thesis]. Goteborg: Goteborg University; 1995. Google Scholar
3 Tewari A , SooriakumaranP, BlochDA, et al.Positive surgical margin and perioperative complication rates of primary surgical treatments for prostate cancer: a systematic review and meta-analysis comparing retropubic, laparoscopic, and robotic prostatectomy. Eur Urol2012;62:1–15.CrossrefPubMed Google Scholar
4 Weerakoon M , SenguptaS, SethiK, IschiaJ, WebbDR. Predictors of positive surgical margins at open and robot-assisted laparoscopic radical prostatectomy: a single surgeon series. J Robot Surg2012;6:311–316.CrossrefPubMed Google Scholar
5 Coronato EE , HarmonJD, GinsbergPC, et al.A multiinstitutional comparison of radical retropubic prostatectomy, radical perineal prostatectomy, and robot-assisted laparoscopic prostatectomy for treatment of localized prostate cancer. J Robot Surg2009;3:175–178. Google Scholar
6 No authors listed. da Vinci Surgery Intuitive Surgical Inc., Sunnyvale, 2015. http://www.davincisurgery.com/da-vinci-urology/da-vinci-surgery/frequently-asked-questions.php (date last accessed 19 August 2015). Google Scholar
7 Paul HA , BargarWL, MittlestadtB, et al.Development of a surgical robot for cementless total hip arthroplasty. Clin Orthop Relat Res1992;285:57–66.PubMed Google Scholar
8 Matsen FA III , GarbiniJL, SidlesJA, et al.Robotic assistance in orthopaedic surgery. A proof of principle using distal femoral arthroplasty. Clin Orthop Relat Res1993;296:178–186.PubMed Google Scholar
9 Börner, M, Wiesel U, Ditzen W. Clinical experiences with Robodoc and the Duracon total knee. In: Stiehl JB, et al, editors. Navigation and robotics in total joint and spine surgery. Springer-Verlag, 2004;362-366. Google Scholar
10 Paul HA . Surgical robot in endoprosthetics. How CASPAR assists on the hip. MMW Fortschr Med1999;141:18. Google Scholar
11 Siebert W , MaiS, KoberR, HeecktPF. Technique and first clinical results of robot-assisted total knee replacement. Knee2002;9:173–180.CrossrefPubMed Google Scholar
12 Jakopec M , HarrisSJ, Rodriguez y BaenaF, et al.The first clinical application of a "hands-on" robotic knee surgery system. Comput Aided Surg2001;6:329–339.CrossrefPubMed Google Scholar
13 Roche M , O’LoughlinPF, KendoffD, MusahlV, PearleAD. Robotic arm-assisted unicompartmental knee arthroplasty: preoperative planning and surgical technique. Am J Orthop (Belle Mead NJ)2009;38(Suppl):10–15.PubMed Google Scholar
14 Conditt MA , RocheMW. Minimally invasive robotic-arm-guided unicompartmental knee arthroplasty. J Bone Joint Surg [Am]2009;91-A(Suppl 1):63–68.CrossrefPubMed Google Scholar
15 No authors listed. THINK Surgical: Company History, 2014. http://thinksurgical.com/history (date last accessed 19 August 2015). Google Scholar
16 No authors listed. Stryker: Stryker NJ USA, 2015. http://www.stryker.com/en-us/index.htm (date last accessed 19 August 2015). Google Scholar
17 Picard F, Moody J, DiGioia AM III, Jaramaz B. Clinical classifications of CAOS systems. In: DiGioia AM III, Jaramaz B, Picard F, Nolte LP, eds. Computer and robotic assisted hip and knee surgery. New York, NY: Oxford University Press, 2004:43-48. Google Scholar
18 Wolf A , JaramazB, LisienB, DiGioiaAM. MBARS: mini bone-attached robotic system for joint arthroplasty. Int J Med Robot2005;1:101–121.CrossrefPubMed Google Scholar
19 Song S , MorA, JaramazB. HyBAR: hybrid bone-attached robot for joint arthroplasty. Int J Med Robot2009;5:223–231.CrossrefPubMed Google Scholar
20 Nishihara S , SuganoN, NishiiT, et al.Comparison between hand rasping and robotic milling for stem implantation in cementless total hip arthroplasty. J Arthroplasty2006;21:957–966.CrossrefPubMed Google Scholar
21 Hagio K , SuganoN, TakashinaM, et al.Effectiveness of the ROBODOC system in preventing intraoperative pulmonary embolism. Acta Orthop Scand2003;74:264–269.CrossrefPubMed Google Scholar
22 Hananouchi T , SuganoN, NishiiT, et al.Effect of robotic milling on periprosthetic bone remodeling. J Orthop Res2007;25:1062–1069.CrossrefPubMed Google Scholar
23 Domb BG , El BitarYF, SadikAY, StakeCE, BotserIB. Comparison of robotic-assisted and conventional acetabular cup placement in THA: a matched-pair controlled study. Clin Orthop Relat Res2014;472:329–336.CrossrefPubMed Google Scholar
24 El Bitar YF , JacksonTJ, LindnerD, et al.Predictive value of robotic-assisted total hip arthroplasty. Orthopedics2015;38:31–37.CrossrefPubMed Google Scholar
25 Liow MH , XiaZ, WongMK, et al.Robot-assisted total knee arthroplasty accurately restores the joint line and mechanical axis. A prospective randomised study. J Arthroplasty2014;29:2373–2377.CrossrefPubMed Google Scholar
26 Kim SM , ParkYS, HaCW, LimSJ, MoonYW. Robot-assisted implantation improves the precision of component position in minimally invasive TKA. Orthopedics2012;35:1334–1339.CrossrefPubMed Google Scholar
27 Bellemans J , VandenneuckerH, VanlauweJ. Robot-assisted total knee arthroplasty. Clin Orthop Relat Res2007;464:111–116.CrossrefPubMed Google Scholar
28 Song EK , SeonJK, ParkSJ, et al.Simultaneous bilateral total knee arthroplasty with robotic and conventional techniques: a prospective, randomized study. Knee Surg Sports Traumatol Arthrosc2011;19:1069–1076.CrossrefPubMed Google Scholar
29 Park SE , LeeCT. Comparison of robotic-assisted and conventional manual implantation of a primary total knee arthroplasty. J Arthroplasty2007;22:1054–1059.CrossrefPubMed Google Scholar
30 Chun YS , KimKI, ChoYJ, et al.Causes and patterns of aborting a robot-assisted arthroplasty. J Arthroplasty2011;26:621–625.CrossrefPubMed Google Scholar
31 Clark TC , SchmidtFH. Robot-assisted navigation versus computer-assisted navigation in primary total knee arthroplasty: efficiency and accuracy. ISRN Orthop2013;2013:794827.CrossrefPubMed Google Scholar
32 Kamath AF , LevackA, JohnT, ThomasBS, LonnerJH. Minimum two-year outcomes of modular bicompartmental knee arthroplasty. J Arthroplasty2014;29:75–79.CrossrefPubMed Google Scholar
33 Koulalis D , O’LoughlinPF, PlaskosC, et al.Sequential versus automated cutting guides in computer-assisted total knee arthroplasty. Knee2011;18:436–442.CrossrefPubMed Google Scholar
34 Coon TM , DriscollMD, CondittMA. Robotically assisted UKA is more accurate than manually instrumented UKA. J Bone Joint Surg [Br]2010;92-B(Suppl I):157. Google Scholar
35 Dunbar NJ , RocheMW, ParkBH, et al.Accuracy of dynamic tactile-guided unicompartmental knee arthroplasty. J Arthroplasty2012;27:803–808.CrossrefPubMed Google Scholar
36 Karia M , MasjediM, AndrewsB, JaffryZ, CobbJ. Robotic assistance enables inexperienced surgeons to perform unicompartmental knee arthroplasties on dry bone models with accuracy superior to conventional methods. Adv Orthop2013;2013:481039.CrossrefPubMed Google Scholar
37 Smith JR , RichesPE, RowePJ. Accuracy of a freehand sculpting tool for unicondylar knee replacement. Int J Med Robot2014;10:162–169.CrossrefPubMed Google Scholar
38 Lonner JH , SmithJR, PicardF, et al.High degree of accuracy of a novel image-free handheld robot for unicondylar knee arthroplasty in a cadaveric study. Clin Orthop Relat Res2015;473:206–212.CrossrefPubMed Google Scholar
39 Jaffry Z , MasjediM, ClarkeS, et al.Unicompartmental knee arthroplasties: robot vs. patient specific instrumentation. Knee2014;21:428–434.CrossrefPubMed Google Scholar
40 Hansen DC , KusumaSK, PalmerRM, HarrisKB. Robotic guidance does not improve component position or short-term outcome in medial unicompartmental knee arthroplasty. J Arthroplasty2014;29:1784–1789. Google Scholar
41 Swank ML , AlkireM, CondittM, LonnerJH. Technology and cost-effectiveness in knee arthroplasty: computer navigation and robotics. Am J Orthop (Belle Mead NJ)2009;38(Suppl):32–36.PubMed Google Scholar
42 Jassim SS , Benjamin-LaingH, DouglasSL, HaddadFS. Robotic and navigation systems in orthopaedic surgery: how much do our patients understand?Clin Orthop Surg2014;4:462–467.CrossrefPubMed Google Scholar
43 No authors listed. Australian Orthopaedic Association National Joint Replacement Registry 2014 annual report. https://aoanjrr.dmac.adelaide.edu.au/documents/10180/172286/Annual%20Report%202014 (date last accessed 01 September 2015). Google Scholar









