Abstract
Ankle replacements have improved significantly since the first reported attempt at resurfacing of the talar dome in 1962. We are now at a stage where ankle replacement offers a viable option in the treatment of end-stage ankle arthritis. As the procedure becomes more successful, it is important to reflect and review the current surgical outcomes. This allows us to guide our patients in the treatment of end-stage ankle arthritis. What is the better surgical treatment – arthrodesis or replacement?
Why replace ankles?
The impact of severe ankle arthritis on an individual’s quality of life is significant, both physically and emotionally, and its effects are reported to be as severe as those caused by end-stage hip arthritis.1 Ankle arthritis is most commonly post-traumatic, either as a result of a fracture or repeated ligamentous injury.2 Thus, unusually for arthritis, it typically presents in young patients with high functional demands. Ankle arthrodesis has long been considered the ‘gold standard’ for treatment of end-stage ankle arthritis. A solid well-aligned fusion offers good pain control and improved mobility without the need for future revision surgery. It has therefore traditionally been seen as the ideal ‘one-off’ procedure. However, fusion does have its limitations. Loss of ankle movement permanently disturbs normal gait which affects the kinematics of the subtalar, knee and midfoot joints. Coester et al3 has shown that at a mean of 22 years post-fusion, the majority of ankle fusion patients had functionally limiting arthritic changes in the ipsilateral foot. The early pain control provided by arthrodesis may not always be the solution to a long-term pain-free foot, as is often thought. This limitation, coupled with the success of arthroplasty in other weight-bearing joints, makes ankle replacement an attractive alternative.
Development of ankle replacements
Themistocles Gluck attempted the first hip replacement in 1891 using an ivory femoral head replacement for tuberculosis. Ankle joint replacements were developed much later; a case report in 2002 of the 40-year follow-up of a talar replacement indicates that attempts to replace the ankle were being made as early as 1962.4 Nevertheless, it was not until the 1970s that interest in ankle replacement gained momentum. Lord and Marotte are credited with the first series of total ankle replacements. Their replacement consisted of the femoral stem from a hip arthroplasty implanted in the tibia and an acetabular cup cemented into the calcaneum, following a talectomy.
A number of early implants were developed including the St George, Imperial College Hospital London, Irvine, Mayo, New Jersey and Richard Smith prostheses. In general they were variations of a two-component design, predominantly with a polyethylene tibial component and a metal talar component. All were cemented. It became apparent that there were high complication and failure rates limiting these early designs.5-7 Almost 50% of Lord and Marotte’s implants failed by ten years; a similar rate was seen in other early designs.8 Failure was mainly due to loosening, massive osteolysis, subsidence and pain. The reliance on cement fixation required significant tibial resection. This meant that the tibial component was seated in less supportive metaphyseal cancellous bone, which was prone to failure and subsidence under compressive loads. The limitation of the constrained two-component designs results in transmission of large forces to the cement prosthesis interface, leading to early loosening. Revision of these failed arthroplasties to fusion was made more difficult by the loss of bone stock resulting from the primary procedure. The high failure rates associated with salvaging the failed ankle replacement led to the stalling of interest in ankle replacements, and the first generation implants were abandoned. In 1985 Bolton-Maggs stated, “[T]he overall results and the long-term outlook of ankle arthroplasty is so poor as to warrant offering only ankle arthrodesis as the surgical treatment of disabling ankle arthritis”.9
With the subsequent development of uncemented fixation for hip and knee arthroplasties, several groups utilised the new surface technologies associated with uncemented hips to develop uncemented ankle replacement through the 1980s. By the 1990s there was a resurgence of interest, with the availability of second-generation models: the Buechel-Pappas, Scandinavian Total Ankle Replacement (STAR) and Agility ankle replacements.
The Agility was the first second-generation replacement to be developed by Frank Alvine in 1984. It is a semi-constrained design consisting of a cobalt chrome talus and a titanium tibial component with a fixed polyethylene bearing. As well as sagittal movements, some axial rotation and medial to lateral translation can occur as the talus is smaller than the tibial cup-shaped articulation. The Agility requires fusion of the tibiofibular syndesmosis (Fig. 1). It is still in use today, mainly in the USA where up until 2006 it was the only FDA- (Food and Drug Association) approved ankle prosthesis.
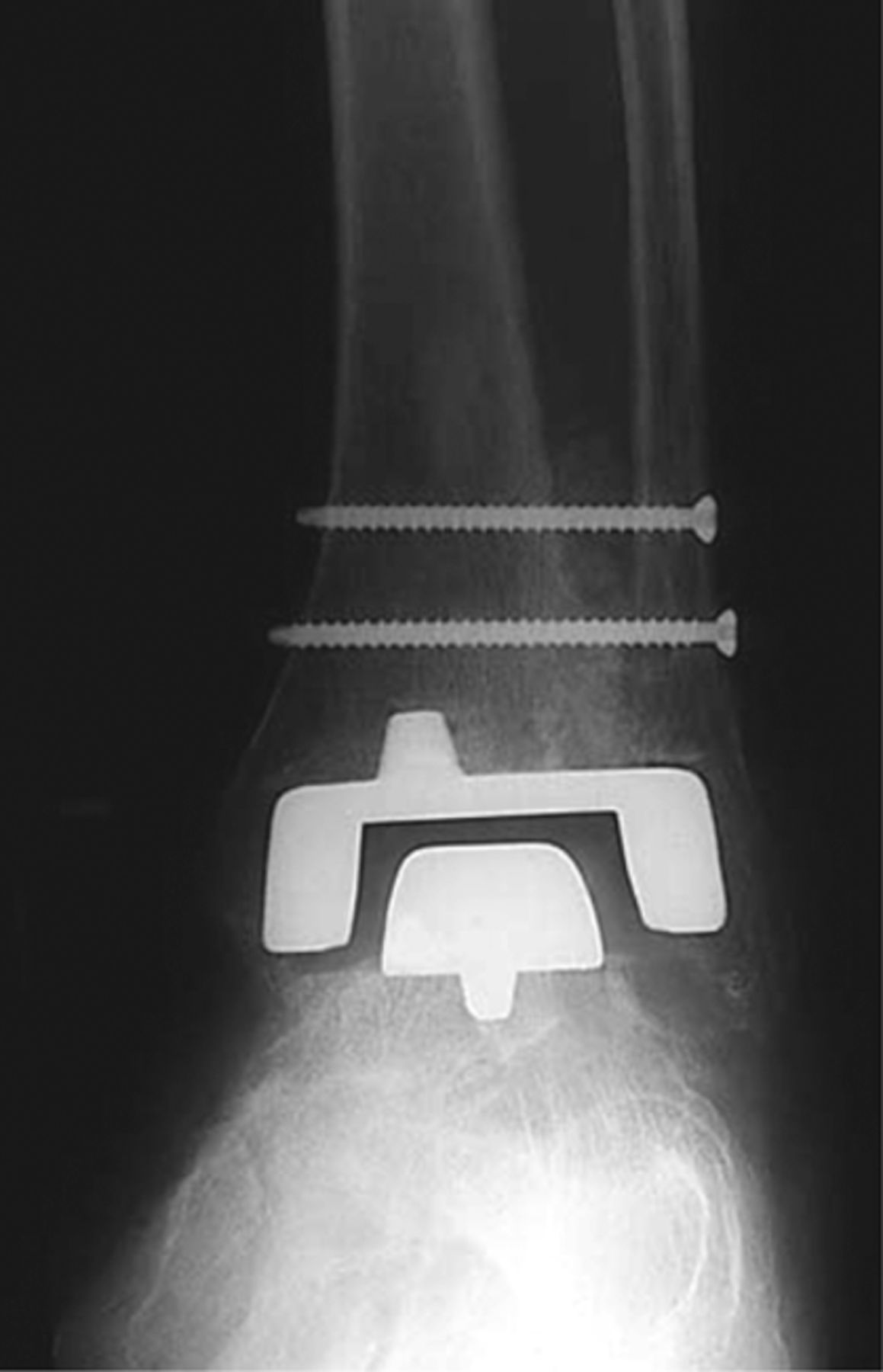
Fig. 1
Agility ankle replacement. A fixed bearing design with fusion of the distal fibula and tibia. Picture courtesy of DePuy Orthopaedics, Inc. (West Chester, Pennsylvania, USA).
The Buechel-Pappas was an evolution of the LCS total knee replacement. It had ceramic-coated titanium tibial and talar components and a mobile polyethylene bearing. The polyethylene meniscus was first introduced in 1978 to the knee replacement, and the idea was then adapted to the ankle. The ultra-high molecular-weight polyethylene meniscal bearing articulated with a flat tibial surface and the deep sulcus of the talar component (Fig. 2). This allows rotation between the tibial component and the meniscus, and flexion/extension between the meniscus and talus. Despite widespread use, it has not been in production since 2008. Newer implants with a similar design are, however, available.

Fig. 2
Components of the Buechel Pappas replacement from anterior and medial views, showing stemmed tibial component. Picture courtesy of Wood PR, Sutton C, Mishra V, Suneja R.10
The STAR prosthesis was originally developed by Hakon Kofoed in 1978 as a cemented, two-component implant. In the 1980s it was modified to its current cementless, mobile-bearing design (Figs 3 and 4). It has been widely used across Europe.
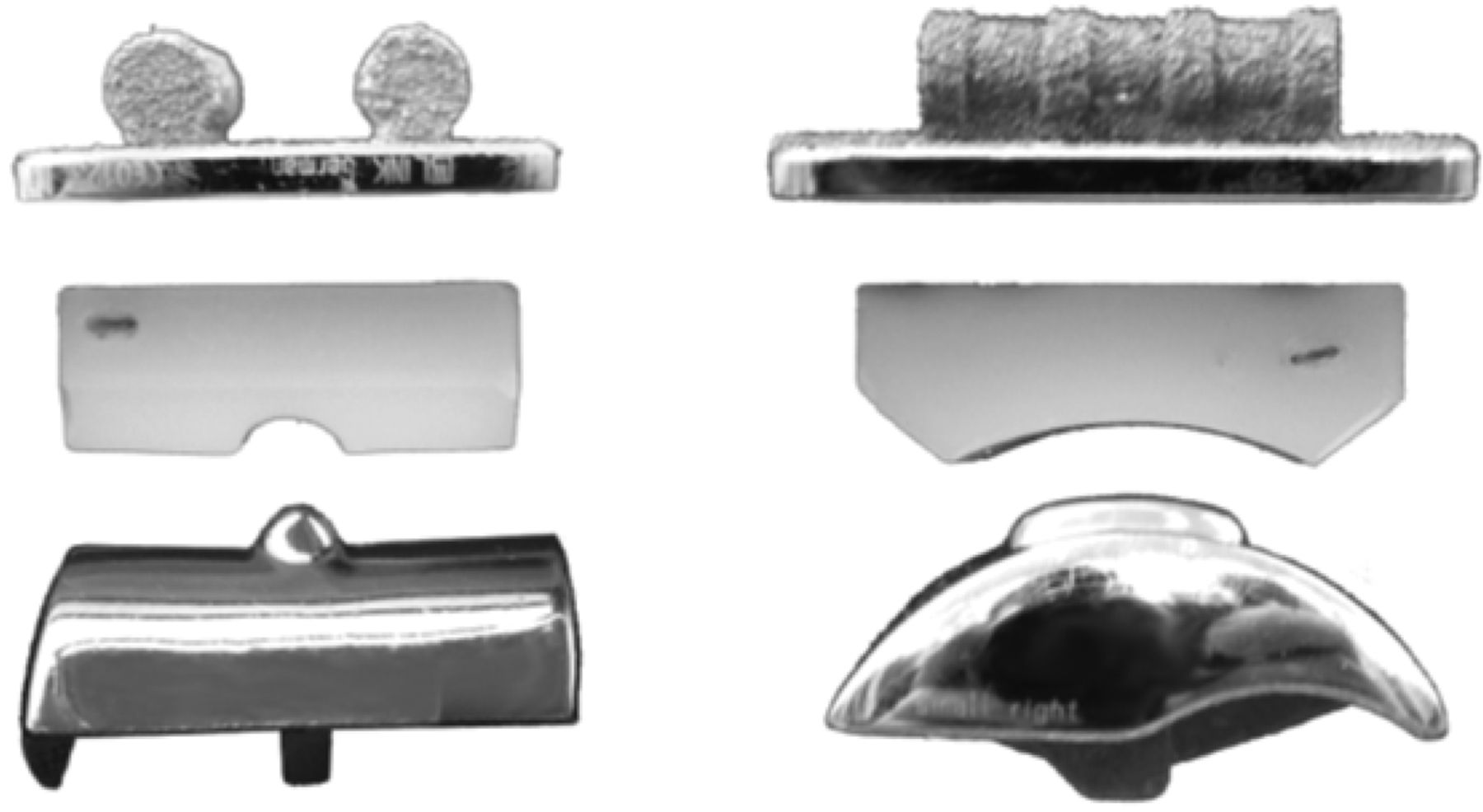
Fig. 3
Components of the STAR replacement from anterior and medial views. Picture courtesy of Wood PR, Sutton C, Mishra V, Suneja R.10

Fig. 4
STAR total ankle replacement. A mobile bearing design with parallel dowel fixation in the tibia.
Short- and mid-term results of the second-generation designs showed improvement on first-generation models, and enthusiasm for ankle replacement returned. Better understanding of the complex biomechanics of hindfoot joints and the importance of bony and soft-tissue alignment, along with further design modifications, has resulted in the modern third-generation implants.
At present, multiple total ankle replacement systems are available. Many small variations exist between the different designs, but, in general, current replacements consist of three components: tibial, talar and a polyethylene articulation. Some have the polyethylene secured to the tibial component creating a fixed-bearing prosthesis. The majority are mobile bearing (Table I), theoretically reducing constraint and hence force transmission and possible loosening of the prosthesis by allowing rotation. However, there is no consensus in clinical evidence to support superiority of either fixed- or mobile-bearing current designs. Mobile-bearing designs have been widely adopted across Europe whereas fixed-bearing designs are more commonly used in the USA as a result of the design restrictions enforced by the FDA. The mobile-bearing STAR has recently been approved following a non-inferiority study.11
Table I. Fixedversus mobile bearing ankle replacements
| Fixed bearing | Mobile bearing |
|---|---|
| Agility | AES* |
| Eclipse | Box |
| ESKA | Buechel Pappas* |
| IN BONE | German Ankle System |
| SALTO Talaris | HINTEGRA |
| Mobility* | |
| SALTO | |
| STAR | |
| Zenith |
-
*Indicates replacements no longer available
Aside from the major difference of fixed- versus mobile-bearing ankle replacements, there is variability in many other design features. Different fixation methods, coatings, instrumentation and bony resection strategies exist. The overall number of ankle replacements implanted is small and there is not enough evidence to ascertain which specific design features improve performance.
At present all designs use a polyethylene-on-cobalt chrome bearing except for a Japanese implant, the TNK, which is ceramic-on-metal. Some designs (Zenith, Salto) use a stemmed tibial prosthesis in keeping with the original Buechel-Pappas design. Insertion of this style of prosthesis requires intra-operative windowing of the anterior tibial cortex to seat the tibial component. This potentially creates a source of weakness in the anterior tibia and an entry route for wear particles. Other tibial fixation methods include fins, pegs, keels and parallel dowels. The Hintegra is essentially flat and can be supplemented by screw fixation in the distal tibia.
The amount of talus resected also varies, with most aiming to simply resurface with minimal resection of bone stock. The need to resurface the sides of the talus is controversial, with some reasoning that the sides of the talus provide substantial support for the talar component and reduce gutter pain; others that the increased bone resection leads to weakness and subsidence. Evidence is once again lacking.
Indications
As with all joint arthroplasty, a successful outcome is not solely dependent on implant design but relies also on surgical technique and patient selection.
The ideal patient for ankle arthroplasty is typically older, with low functional demands (in terms of both work and recreational activities). The ideal patient should have a normal BMI, little coronal deformity and be neurovascularly intact, with good soft tissues and bone stock. Patients with rheumatoid arthritis and those with degenerative change or who have had fusions of adjacent foot joints are also good candidates. The ideal patient is rare. Many surgeons are developing techniques to broaden the classic indications. Indeed, the 2012 UK National Joint Registry data show that 18% of prostheses were implanted into ankles with deformity greater than 150, despite Wood and Deakin showing that those with greater deformity had a worse outcome.12 The absolute contraindications are active infection, a neuropathic joint, peripheral vascular disease, ulceration and neuromuscular disorders with paralysis or significant weakness around ankle.
Ankle arthroplasty can maintain movement, but does not tend to restore movement. Traditionally, ankles that are stiff pre-operatively are considered less likely to reap the benefits of preserved motion, although from personal experience these patients can in fact function well with replacement.
Current UK practice
The UK National Joint Registry has included ankle replacements since April 2010. A total of 2004 total ankle replacements have been recorded to date, and 505 primary ankle replacements were recorded for 2013, with eight different prostheses being used. The Mobility was the most commonly used (35.6%), followed by Zenith (24.6%) and Hintegra (12.3%). Box, Salto, STAR, Rebalance and Inbone were also implanted. Registry data show that there are 165 consultants, performing an average of just three ankle arthroplasties per annum in the UK.
The annual rate of ankle joint arthroplasty in the UK is about 1.2 per 100 000 of the population, which is similar to the rates in Sweden, Norway and Denmark (1 per 100 000). In Finland the rate is double, and in New Zealand triple this rate.13
In comparison with hip and knee arthroplasty, substantially fewer ankle replacements are performed in the NHS in England and Wales. The 2012 data show that 540 primary ankle arthroplasties were performed, in comparison with 76 448 primary THAs and 84 833 primary TKAs for the same period. A total of 76% of units perform fewer than five ankle replacements a year, with 3% of units doing over 25 procedures annually. Annual rates of hip and knee arthroplasty are 218 and 235, respectively, per orthopaedic unit.
Where are we now? Performance and results
Overall, the results of second- and third- generation ankle replacements have been promising, with marked improvement in survival in comparison with the first-generation designs.14-18 However, the levels of success and survivorship still lag behind those of established hip and knee arthroplasties.
The literature on ankle replacements is still lacking. Long-term results are available with cohorts of patients from centres and the results from national registry data. Unsurprisingly, there is a tendency for higher survivorship in reports from the design centres, where the surgeons are more familiar with the design rationale of the implant and instrumentation.19,20The joint registry data are dependent upon compliance rates but do include a wide range of surgeons with varying experience and are more likely to reflect outcomes for the ‘typical’ surgeon. Disturbingly, there is recent evidence from the New Zealand registry that the number of reported revisions may reflect only half of the actual rate.
A systematic review in 2013 collated the evidence for ankle replacements currently available on the market.20 The data showed an overall ten-year survival rate of 73% if registry data are included and 89% if registry data were excluded. Complication rates of 8% intra-operatively and 13.5% post-operatively were seen, with the most common intra-operative event being a malleolar fracture. Overall, ankle replacements in this systematic review were shown to give good improvement in function and pain scores. The data highlight the presence of radiological lucencies, visible in 22.4% of cases at four years. These occurred more commonly on the tibial (21%) than the talar side (1.4%). The AES ankle replacement, a third-generation mobile-bearing design based on the Buechel-Pappas replacement, was withdrawn from the market in 2008 due to concern about significant osteolysis, mainly around the tibial component.21-23Long-term follow-up of radiological lucencies is required to determine their natural progression, whether they affect long-term outcomes and whether early grafting is curative. CT scanning is more accurate in the detection of periprosthetic osteolysis, and may have a role in osteolysis detection and surveillance.
Evidence synthesis from the same systematic review suggests that ankle replacements maintain or improve ankle movement by approximately 10° on average. Despite this preserved motion, progression of subtalar arthritis occurred in 19% to 59% of subjects in four studies by seven years.20 The long-term incidence and morbidity from progressive arthritis in adjacent foot joints following ankle replacement is not currently known and whether arthroplasty offers better future protection against surrounding arthritis than arthrodesis is not established.
To replace or fuse?
The question as to which is better remains unanswered. There is a lack of randomised controlled trials comparing ankle arthroplasty with ankle fusion at present. The high degree of variability between the design of individual studies looking at each of the procedures means that current data are insufficient to draw reliable conclusions. In 2007, Haddad et al24 attempted to perform a systematic review of the literature and reported that the long-term outcomes of second-generation replacements and arthrodesis were comparable. Unfortunately, the review did not include any studies that directly compared arthroplasty with arthrodesis; it consisted of ten arthroplasty studies and 39 arthrodesis studies. Given that there is likely to be a significant selection bias in those chosen for each procedure, the conclusions must be viewed with caution. More recently a prospective non-inferiority study comparing the STAR prosthesis and ankle fusion has shown that at 24 months’ follow-up there was better function and equivalent pain control in those with arthroplasty, but the complication and re-operation rate was higher than in the arthrodesis group.11 Similarly, the Canadian Orthopaedic Foot and Ankle Society (COFAS) prospective study of total ankle replacement (involving Agility, STAR, Mobility, or Hintegra prostheses) and ankle arthrodesis with a mean follow-up of 5.5 ± 1.2 years has shown the clinical outcome of total ankle replacement and ankle arthrodesis to be comparable, but rates of re-operation and major complications were higher after ankle replacement.25 Seven (7%) of the arthrodeses and 48 (17%) of the ankle replacements underwent revision by final follow-up.
There are currently two RCTs in progress comparing the two procedures. In the US, an RCT sponsored by the Seattle Institute for Biomedical and Clinical Research has been recruiting since 2012. It is designed to give a 24-month follow-up, with initial results expected in 2016. Unfortunately, the arthroplasty arm will be limited to include only ankle arthroplasties with FDA approval. A large UK multicentre randomised controlled trial of total ankle replacement versus ankle arthrodesis (TARVA) is due to commence shortly. This will provide comparison of modern third-generation mobile-bearing replacements with fusion. This trial is not expected to report until 2018.
The arthroplasty learning curve
Ankle arthroplasty is a technically demanding procedure with a substantial learning curve. Better outcomes are achieved with increasing experience, volume and familiarity with the technique. A review of the results of the first and last 50 cases of STARs performed by a single surgeon in a consecutive series showed a decrease in surgery time and peri-operative fractures, and improvement in component orientation amongst the latter cases.26
The UK National Joint Registry data show that 505 ankle replacements were performed by 165 surgeons in the last recorded year - a mean of three per surgeon.27 This raises the question as to whether there should be centralisation with regional ankle arthroplasty units, as in Sweden where six units now carry out all ankle replacements nationally. Rethinking how we provide arthroplasty services is topical following the recent withdrawal of the Mobility replacement from the market by DePuy earlier this year. A large number of surgeons in the UK and worldwide have now been forced to reconsider their choice of implant and face a new learning curve with a different prosthesis and unfamiliar instrumentation. If ankle arthroplasty units are established it may be more sensible to concentrate on the number of arthritic ankles treated, as opposed to the number of arthroplasties, to avoid pressuring surgeons into stretching the indications for replacement.
Failed arthroplasty
This review would not be complete without considering the effects of failed arthroplasty procedures. In some cases it is possible to revise the replacement, however, in others the lack of bone stock, amongst other factors, dictates that fusion, either of the ankle alone, or in combination with the subtalar joint, may be the only option. Although many studies report good rates of union in arthrodesis following failed arthroplasty, it must be remembered that salvage surgery is challenging. The functional outcomes are not widely reported and their comparison with a primary arthrodesis is an important metric.
Amputation rates of up to 19% in salvage arthrodeses from failed arthroplasties where large cancellous allografts were required to tackle bone loss have recently been reported by Myerson et al28and act as a reminder of the difficulties faced in the challenge to improve function for those with end-stage ankle degeneration. An alternative to massive grafting is to undertake an arthrodesis with a small amount of shortening. Revision ankle replacement is sometimes an option but is not without risk in light of one study finding a 4% amputation rate with revision arthroplasty.29
Conclusion
Ankle replacement offers much for patients with debilitating end-stage ankle arthritis, but there is still a long way to go before the level of success is equivalent to that of hip and knee arthroplasty. Better data collection through multicentre randomised studies and the continuing input into national joint registries will help to determine the long-term benefits. Improved understanding of ankle and hindfoot biomechanics will advance implant design further.
Interest in joint preserving surgeries such as osteotomies is also increasing. Success here may delay the need for either replacement or fusion. No single procedure is going to be the panacea; the key will be developing sound evidence to determine which procedure is best in each individual case, but there is no doubt some patients achieve excellent function following ankle replacement.
1 Glazebrook M , DanielsT, YoungerA, et al.Comparison of health-related quality of life between patients with end-stage ankle and hip arthrosis. J Bone Joint Surg [Am]2008;90-A:499–505.CrossrefPubMed Google Scholar
2 Saltzman CL , SalamonML, BlanchardGM, et al.Epidemiology of ankle arthritis: report of a consecutive series of 639 patients from a tertiary orthopaedic center. Iowa Orthop J2005;25:44–46.PubMed Google Scholar
3 Coester LM , SaltzmanCL, LeupoldJ, PontarelliW. Long-term results following ankle arthrodesis for post-traumatic arthritis. J Bone Joint Surg [Am]2001;83-A:219–228.CrossrefPubMed Google Scholar
4 Muir DC , AmendolaA, SaltzmanCL. Forty-year outcome of ankle “cup” arthroplasty for post-traumatic arthritis. Iowa Orthop J2002;22:99–102. Google Scholar
5 Kirkup J . Richard Smith ankle arthroplasty. J R Soc Med1985;78:301–304.CrossrefPubMed Google Scholar
6 Newton SE III . Total ankle arthroplasty. Clinical study of fifty cases. J Bone Joint Surg [Am]1982;64-A:104–111.PubMed Google Scholar
7 Kitaoka HB , PatzerGL. Clinical results of the Mayo total ankle arthroplasty. J Bone Joint Surg [Am]1996;78-A:1658–1664.CrossrefPubMed Google Scholar
8 Lord G , MarotteJH. Total ankle replacement (trans.). Rev Chir Orthop Repar Appar Mot1980;66:527–530. Google Scholar
9 Bolton-Maggs BG , SudlowRA, FreemanMA. Total ankle arthroplasty. A long-term review of the London Hospital experience. J Bone Joint Surg [Br]1985;67-B:785–790.CrossrefPubMed Google Scholar
10 Wood PR , SuttonC, MishraV, SunejaR. A randomised, controlled trial of two mobile bearing total ankle replacements. J Bone Joint Surg [Br]2009;91-B:69–74. Google Scholar
11 Saltzman CL , MannRA, AhrensJE, et al.Prospective controlled trial of STAR total ankle replacement versus ankle fusion: initial results. Foot Ankle Int2009;30:579–596.CrossrefPubMed Google Scholar
12 Wood PL , DeakinS. Total ankle replacement. The results in 200 ankles. J Bone Joint Surg [Br]2003;85-B:334–341.CrossrefPubMed Google Scholar
13 Henricson A , Nilsson J-A, CarlssonA. 10-year survival of total ankle arthroplasties: a report on 780 cases from the Swedish Ankle Register. Acta Orthop2011;82:655–659.CrossrefPubMed Google Scholar
14 Pyevich MT , SaltzmanCL, CallaghanJJ, AlvineFG. Total ankle arthroplasty: a unique design. Two to twelve-year follow-up. J Bone Joint Surg [Am]1998;80-A:410–420.PubMed Google Scholar
15 Buechel FF , BuechelFF, PappasMJ. Twenty-year evaluation of cementless mobile-bearing total ankle replacements. Clin Orthop Relat Res2004;424:19–26.CrossrefPubMed Google Scholar
16 Wood PL , PremH, SuttonC. Total ankle replacement: medium-term results in 200 Scandinavian total ankle replacements. J Bone Joint Surg [Br]2008;90-B:605–609.CrossrefPubMed Google Scholar
17 Wood PL , KarskiMT, WatmoughP. Total ankle replacement: the results of 100 mobility total ankle replacements. J Bone Joint Surg [Br]2010;92-B:958–962.CrossrefPubMed Google Scholar
18 Bonnin M , GaudotF, LaurentJR, et al.The Salto total ankle arthroplasty: survivorshipand analysis of failures at 7 to 11 years. Clin Orthop Relat Res2011;469:225–236. Google Scholar
19 Gougoulias N , KhannaA, MaffulliN. How successful are current ankle replacements?: a systematic review of the literature. Clin Orthop Relat Res2010;468:199–208.CrossrefPubMed Google Scholar
20 Zaidi R , CroS, GurusamyK, et al.The outcome of total ankle replacement: a systematic review and meta-analysis. Bone Joint J2013;95-B:1500–1507.CrossrefPubMed Google Scholar
21 Besse JL , BritoN, LienhartC. Clinical evaluation and radiographic assessment of bone lysis of the AES total ankle replacement. Foot Ankle Int2009;30:964–975.CrossrefPubMed Google Scholar
22 Rodriguez D , BevernageBD, MaldagueP, et al.Medium term follow-up of the AES ankle prosthesis: High rate of asymptomatic osteolysis. Foot Ankle Surg2010;16:54–60.CrossrefPubMed Google Scholar
23 Kokkonen A , IkävalkoM, TiihonenR, et al.High rate of osteolytic lesions in medium-term followup after the AES total ankle replacement. Foot Ankle Int . 2011;32:168–175.CrossrefPubMed Google Scholar
24 Haddad SL , CoetzeeJC, EstokR, et al.Intermediate and long-term outcomes of total ankle arthroplasty and ankle arthrodesis. A systematic review of the literature. J Bone Joint Surg [Am]2007;89-A:1899–1905.CrossrefPubMed Google Scholar
25 Daniels TR , YoungerAS, PennerM, et al.Intermediate-term results of total ankle replacement and ankle arthrodesis: a COFAS multicenter study. J Bone Joint Surg [Am]2014;96-A:135–142.CrossrefPubMed Google Scholar
26 Schimmel JJ , WalschotLH, LouwerensJW. Comparison of the short-term results of the first and last 50 Scandinavian total ankle replacements: assessment of the learning curve in a consecutive series. Foot Ankle Int2014;35:326–333.CrossrefPubMed Google Scholar
27 No authors listed. National Joint Registry: National Joint Registry for England, Wales and Northern Ireland, 11th Annual report 2014. http://www.njrcentre.org.uk/njrcentre/Portals/0/Documents/England/Reports/11th_annual_report/NJR%2011th%20Annual%20Report%202014.pdf (date last accessed 09 February 2015). Google Scholar
28 Jeng CL , CampbellJT, TangEY. Tibiotalocalcaneal arthrodesis with bulk femoral head allograft for salvage of large defects in the ankle. Foot Ankle Int2013;34:1256–1266.CrossrefPubMed Google Scholar
29 Ellington JK , GuptaS, MyersonMS. Management of failures of total ankle replacement with the agility total ankle arthroplasty. J Bone Joint Surg [Am]2013;95-A:2112–2118.CrossrefPubMed Google Scholar









