Abstract
There are significant differences in the methods and styles of orthopaedic surgical training between continents, all with the aim to produce competent consultant surgeons, but the differences in training content and pathway are vast. We review and contrast the key differences between three continents.
A recently performed survey was undertaken of 69 orthopaedic trainees from Wessex and East Midlands regions in the UK, University of Denver, Colorado, USA and New Zealand trainees, with the complete results expected later in the year. This survey has highlighted many variations between the differing national training programmes. Sixty five percent of US trainees have joined a surgical training programme just one year following medical school qualification, whereas 52% of UK and 58% of New Zealand trainees took four years or more after qualification. Working hours differed substantially, with 3% of UK, 90% of New Zealand and 100% of US trainees reporting working over 60 hours per week.
The aim of this article is to summarise the training formats between these three developed continents and outline the differing aspects of orthopaedic surgical training given emphasis in each system. At a time when healthcare is pushed financially, efficient training is more important than ever.
Training in the UK
Medical training in the UK has undergone significant changes over the last few years, largely related to the introduction of the European Working Time Directive (EWTD) in August 2009. This Directive was designed to protect the health and safety of workers by restricting the number of hours any European worker (including doctors) can work and by imposing maximum working hours and minimum rest requirements for all workers.
Orthopaedic training structure within the UK is illustrated in Figure 1. Trauma and orthopaedic surgery recently has been delivered by two different training programmes: ‘uncoupled’ and ‘run-through’. ‘Uncoupled’ training commences with two years of core training (CT1/2), followed by a further competitive application system for higher training posts (ST3+) with progression to completion of training if all competency requirements are met. In contrast, ‘run-through’ training allowed automatic progression between training levels providing all competency requirements are met, however, recruitment is no longer widely conducted to these posts. The Trauma and Orthopaedic curriculum is governed by the Intercollegiate Surgical Curriculum Programme (ISCP), which helps to build orthopaedic experience from ST1/3 to the completion of training and is competency based.

Fig. 1
Schematic diagram detailing the UK orthopaedic training structure.
The intermediate years of training (from ST3 onwards) are structured around more focused orthopaedic training, concentrating on trauma management and the generality of elective practice. It is based around the core principles of the National Orthopaedic Curriculum. Trainees are required to demonstrate the attainment of competencies by continuous assessments between trainee and trainer using the Orthopaedic Competence Assessment Programme (OCAP) which in recent years has been integrated into the ISCP. The culmination of this phase of training will be in undertaking the Fellowship of the Royal College of Surgeons (Trauma and Orthopaedic) examination. This exam is designed to equip and assess candidates to the standard expected of a newly appointed consultant. Initially the candidate is assessed with a multiple choice exam (Part 1), which if successful is followed by a clinical and viva exam (Parts 2 and 3) several months later. The current pass rate for trainees taking the exam from an approved training programme (known as Type 1 trainees) exceeds 80%, but is much lower for those who have not completed an approved programme.
Subspecialist knowledge and surgical expertise are attained through a series of senior positions and fellowships in the UK and also abroad. This forms the basis of a development of practice after award of the Certificate of Completion of Training (CCT). The trainee is then eligible to apply to join the specialist register and apply for consultant posts.
With the reduction of hours brought about by the EWTD, concerns have been raised about training standards and achievement of proficiencies, particularly in craft specialities such as orthopaedics. There is an increasing economic drive to reduce the cost of training as well as to increase the number of consultants, which potentially risks a decrease in the standard of consultant care.
A reduction in the length of training is not compatible with the high standards of surgical training detailed in the current Trauma and Orthopaedic curriculum. Inevitably this will lead to erosion of surgical experience and proficiency of newly qualified surgeons. The introduction of EWTD and a change to full shift pattern working has already had a detrimental effect on training and any further reduction in training time would only exacerbate this problem. The EWTD has resulted in a 44% reduction in overall training time, from 32 000 hours to 18 000 hours across an eight year surgical training period (CST and HST), further compounded by the SiMAP and Jaeger rulings. Other implications of EWTD include a negative impact on patient care and training, under-reporting of hours worked, and a desire to opt-out of compliant rotas.
In 2012, the Association of Surgeons in Training published a document reiterating concerns regarding the impact of regulations on surgical training, going on to make recommendations for the future of surgical training and education. It was suggested that the EWTD for surgeons in training should be relaxed, giving flexibility where required to work more than an average of 48 hours per week up to a limit averaging 65 hours per week. The Association of Surgeons in Training performed a survey of the UK surgical trainee workforce in 2013 which included 1200 fully completed responses. Of those respondents who had worked on an EWTD compliant rota, 71% felt that it had negatively impacted on their training. Trainees are taking action in order to protect their training, with 72% attending to train on days off. The evidence suggests that projected benefits to work-life balance and patient safety have not been realised despite being implemented over four years ago. A relaxation in the regulations may permit an increase in dedicated training time and encourage honest reporting of working hours. Appropriate remuneration for actual working hours and consideration of alternative working patterns are paramount if this training programme is to deliver high quality surgeons.
Training in the USA
Orthopaedic training in the US differs greatly from the UK, right from the inception of training. A doctor embarks on a medical career in the US later than in the UK, starting around age 22 years following four years in College. This is offset by more rapid and organised career progression which lasts a total of just five years. Potential orthopaedic trainees are selected using medical school records (mainly USMLE scores), research experience, extracurricular activities and letters of recommendation. It is an extremely competitive programme, resulting in the appointment of highly motivated, proactive trainees. Initial training (the postgraduate year 1 or ‘internship’) involves experience in general surgery, plastic surgery, emergency medicine, ITU and anaesthesia amongst others. All training programmes differ slightly in their composition and are essentially locally organized leading to variations in structure and quality of experience. From postgraduate year 2 and above, trainees are supervised by the chief resident. Their training consists of apprentice style learning and the acquisition of manual skills in the emergency room and the operating theatre. All residents prepare formal teaching sessions for medical students and nursing staff. As a chief resident the trainee provides his or her patients with primary orthopaedic care requiring minimal supervision from their attending faculty.
Residents are subject to continuous in-training assessment as well a national examination every November (Orthopaedic In-Training Exam, OITE). Orthopaedic diagnosis and treatment are taught through discussion of specific cases on a daily basis. The majority of residency programmes include exposure to a research project, involving either clinical or laboratory work, to be presented nationally and published at the completion of the training scheme. On completion of the accredited residency, the candidate has the choice of attending an accredited sub-specialty fellowship. This may be a route to an academic career, which is a highly popular choice, or a route to further sub-specialisation, and is undertaken in addition to the core training requirements. Some fellowship programmes (such as Trauma) are starting to move towards a centralised application and appointment process giving all officially recognised fellowships a high status.
The US training schemes have also been susceptible to reductions in working hours and this issue is of equal concern amongst US orthopaedic surgeons. A study published in 2003 reported the mean number of hours worked per week by residents in trauma amounted to over 80 hours, despite the 2003 Accreditation Council on Graduate Medical Education work-hours duty policy limiting resident work hours to 80 hours per week. In the same study, 87% of the surgical faculty felt that reducing resident work-hours would compromise training.
American residents are restricted to 80 hours of duty hours, defined as all clinical and academic activities related to the residency program. Programs interested in extending the duty hours for their chief residents can use the “88 hour exception” to request an increase of up to 10% in duty hours on a programme by programme basis. This is subject to endorsement of the sponsoring institution’s graduate medical education committee (GMEC) and approval of the Review Committee. An increase in duty hours above 80 hours per week can be granted only when there is a very high likelihood that this will improve residents’ educational experiences. A surgical program needs to demonstrate that residents do not attain the required case experiences in some categories. If the program has already made all reasonable efforts to limit activities that do not contribute to enhancing their surgical skills, an increase in hours may be granted.
Following completion of the orthopaedic residency programme, the candidate is eligible to apply for board certification. The American Board of Orthopedic Surgery is the body responsible for the maintenance of educational standards. It is also involved with examinations to acquire board certification, as well as revalidation (mandatory for all surgeons who were board-certified after 1986). Upon completion of an accredited residency, the candidate may sit the Part 1 written examination. To be eligible to sit the Part 2 examination, they must have been practicing for 22 months and have been successful in Part 1. Part 2 consists of oral examinations, in addition to which candidates must submit a list of all their surgical procedures performed during a defined 6-month period. These logbooks must be certified as authentic and the operative cases are stored online as part of a database. Twelve cases are selected for further scrutiny by the examiners. Although board certification is entirely voluntary, 98% of all candidates take the Part 2 examination within 5 years of completing residency programmes. As of 1999, only 74% of all practicing orthopaedic surgeons in the US were board-certified. Teaching and academic appointments are held by 42% of orthopaedic surgeons.
In summary, in the US, the progression from graduation, through training and residency to satisfactory completion of training is achieved by a process of continuous assessment, with a ‘seamless’ approach to the training programme, potentially allowing residents access to more specialist training earlier although variations between programmes do exist.
Training in Australia and New Zealand
In Australia and New Zealand, being Commonwealth countries, the training system has a similar structure to that of the UK. Trainees commence medical school aged 18 after completion of school exams. In New Zealand, there are only two medical schools, Otago and Auckland, although a recent expansion of medical school places may lead to further centres in the future. Medical degrees take five to six years to complete, with many students taking an extra year to complete an intercalated degree. Undergraduate teaching of orthopaedics takes place within the hospital environment, generally by academic orthopaedic surgeons, and occasionally by non-surgical orthopaedic physician practitioners. The last year of medical school is undergone as a ‘trainee intern (TI)’, comprising placement with junior doctors in different hospitals to give the medical student 12 months of clinical experience prior to commencing formal employment.
Following graduation from medical school, all junior doctors complete at least two years of basic training before applying for specialty training programmes. The timing of the first part of the Fellow of the Royal Australasian College of Surgeons (FRACS) examination is currently under review. This is historically similar to the first part of the UK Royal Colleges examinations, consisting of basic medical sciences, anatomy, pathology and physiology. This exam is shared with other surgical specialities, and therefore encompasses general and speciality surgery as well as orthopaedics. At this time the exam cannot be taken until the trainee is accepted onto the training scheme. However, the RACS are currently undertaking a pilot programme to allow junior doctors to take the exam prior to acceptance onto training, possibly with a view to this becoming a mandatory component of the application in the future.
Application for the training scheme can occur after two years in basic training, however, it is unusual to be successful on the first attempt, and usually registrar level orthopaedic experience is required. Most doctors start a post as a ‘junior registrar’ (referring to all doctors working as a non-training registrar) and gain experience for several years in different hospitals, before applying successfully to join a training programme. Application is based on three components: CV, references and interview. Only those candidates who score highly enough based on the CV and references are shortlisted for interview. Interviews take place on one day of the year in a single centre, and are conducted by the NZOA Education Committee.
Once accepted onto the accredited training scheme, the trainee becomes a ‘senior registrar’ (training registrar) and is committed to a five year scheme. During this time the trainee rotates around a mixture of rural and urban centres each year to gain experience of general, trauma and subspecialty orthopaedics. Training posts vary between hospitals and, interestingly, can include posts in private or public hospitals. In the first year of training, the Orthopaedic Principles and Basic Science (OPBS) examination is undertaken. In the fourth year of training, the final fellowship specialty examination is taken, with a pass rate of over 90%. At the end of this time and once the final exams have been successfully passed, trainees embark on one to two years of fellowship training in their chosen sub-speciality.
Surgical training involves a progression in levels of competency from being a doctor with at least two years of postgraduate experience to becoming a practicing specialist. Progressive development occurs through five stages of increasing complexity (pre- vocational, novice, intermediate, competent to proficient). The curriculum is a mixture of practical operating competencies, communication skills and formal theoretical examinations. Progress is reviewed annually by the Australian and New Zealand Orthopaedic Association Education Committee. On successful completion, the applicant will receive a Fellowship with the Royal Australasian College of Surgeons (RACS) and be able to become vocationally registered as an orthopaedic surgeon with the Australian or New Zealand Medical Council. The shortest time possible from graduation to completion of training is 7 years.
An increasing proportion of Australasian orthopaedic registrars undertake a formal clinical and/or research fellowships abroad, typically at year 4 or later. Funding for these posts is a common issue with trainees often out of pocket to receive the training they require.
The future of training
Across all three continents the increasing pressure to deliver service and constraints on working time together with a ‘quality’ agenda will have a profound impact on specialty training. This is perhaps felt most acutely in the UK where the implementation of the working time directive has already changed training.
The changes in the UK system particularly with the use of a national electronic logbook (www.elogbook.org) which allows not only trainees and trainers to monitor their progress, but to compare their operative experience and level to those across the region or country (Fig. 2) is part of a move towards an integrated learning record with competency based assessments. The eLogbook integrates with the intercollegiate surgical curriculum project (www.iscp.ac.uk) which allows a dashboard based view of trainees progress (Fig. 3). The ISCP is designed to integrate a range of clinician and trainee based assessment tools including case by case teaching (case based discussion) core operative and procedural competencies (Procedure Based Assessments and Direct Observations of Procedures). These are recorded by the trainees on a structured form (Fig. 4) and the results of these are available at their annual assessment (ARCP) (Fig. 5).
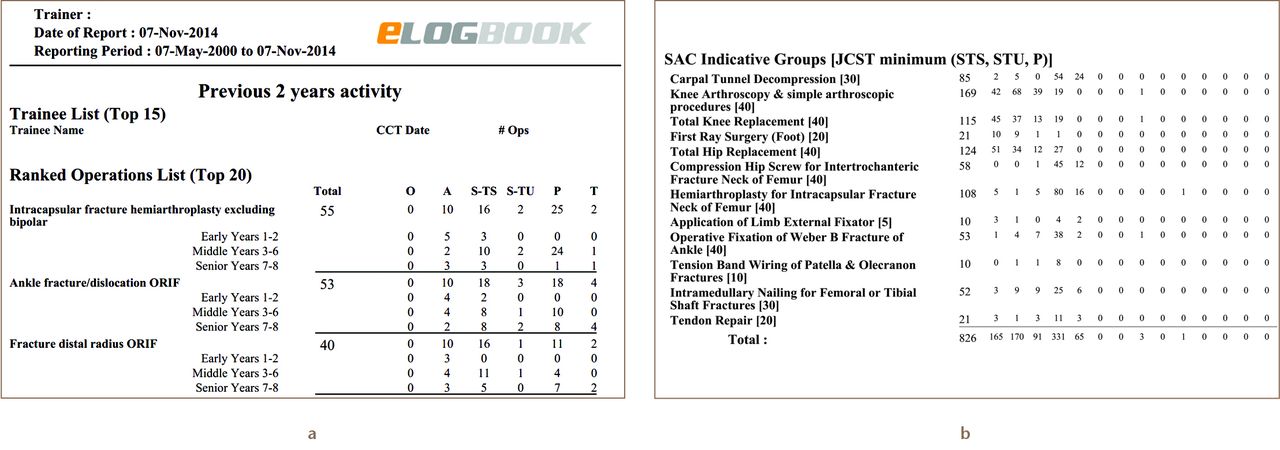
Fig. 2
Trainer (a) and trainee (b) reports.
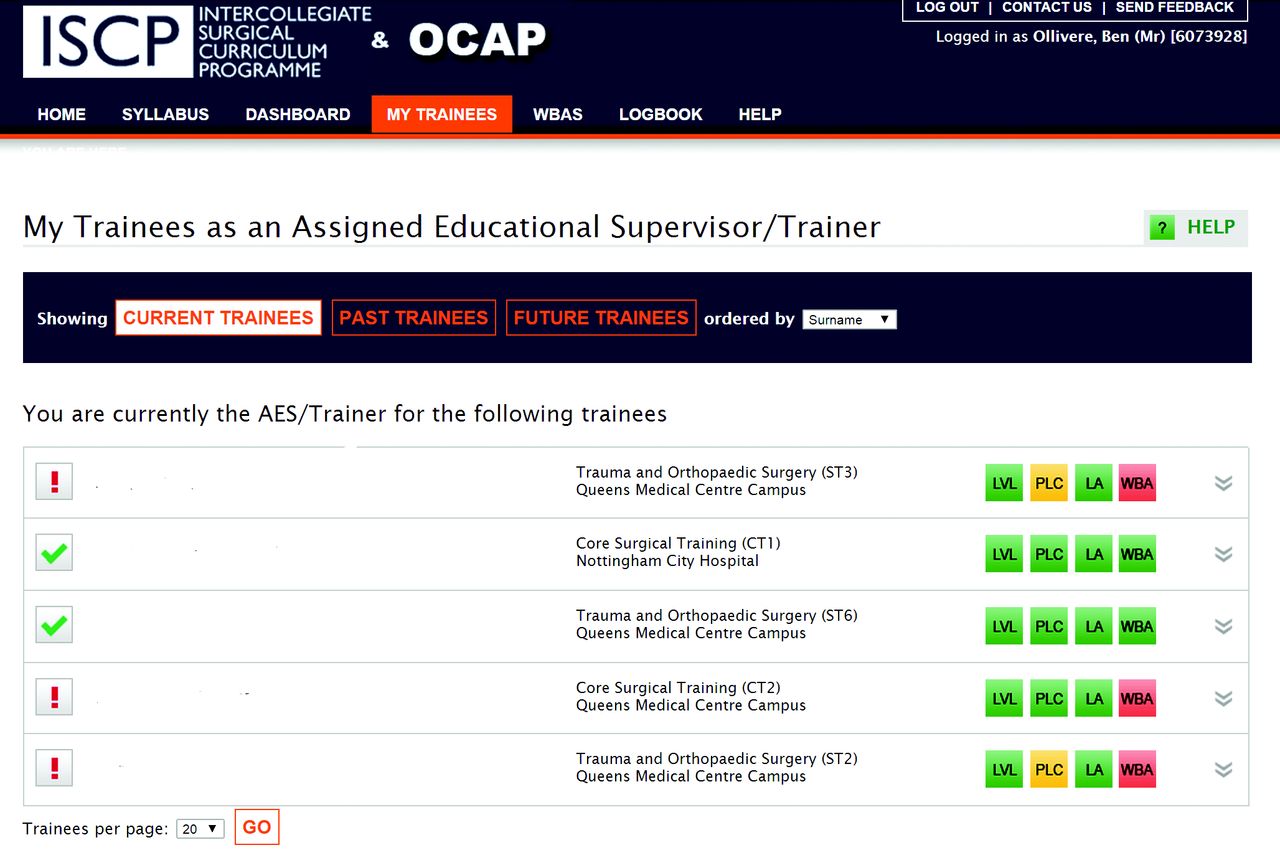
Fig. 3
ISCP overview.
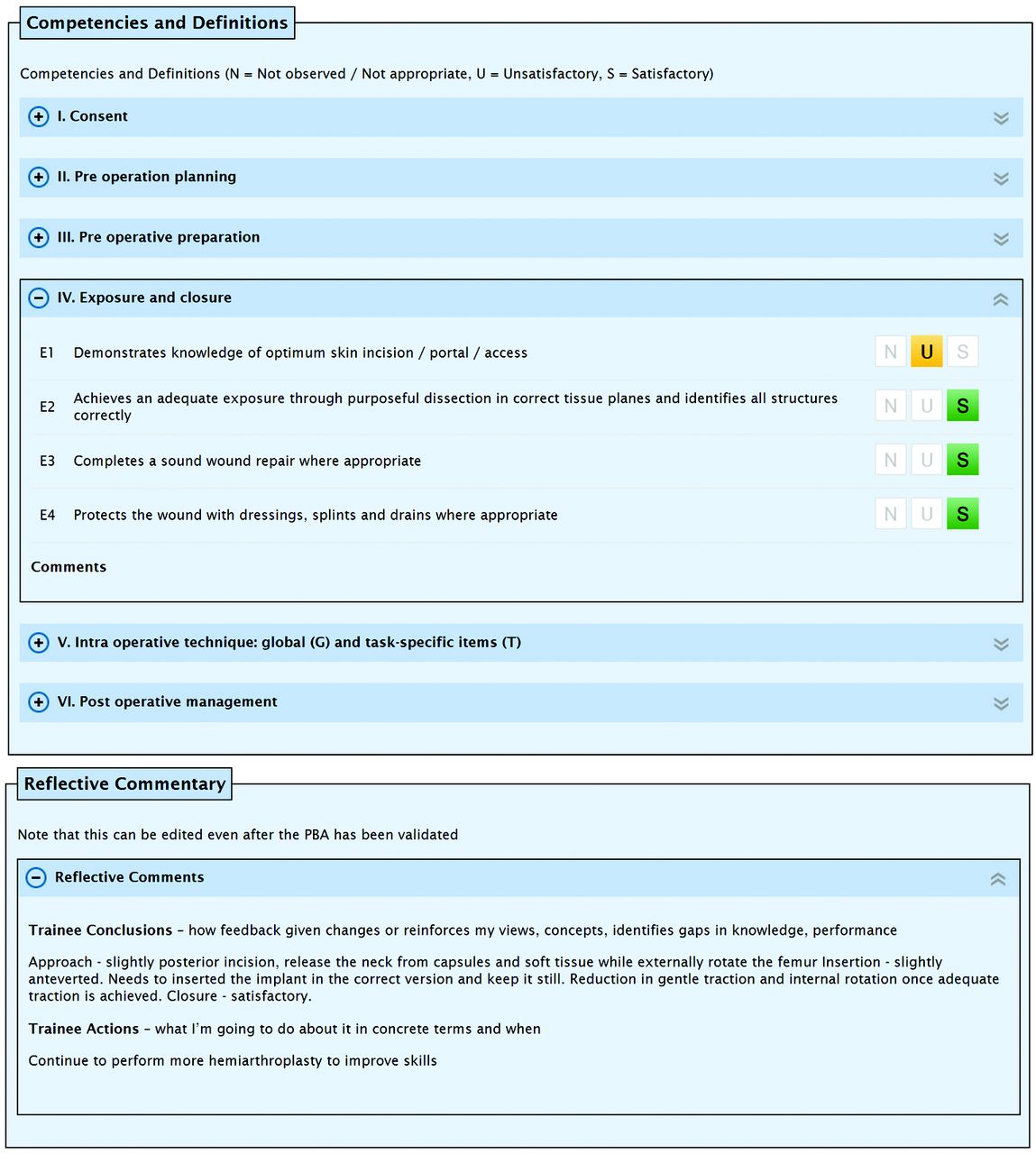
Fig. 4
Procedure based assessment.
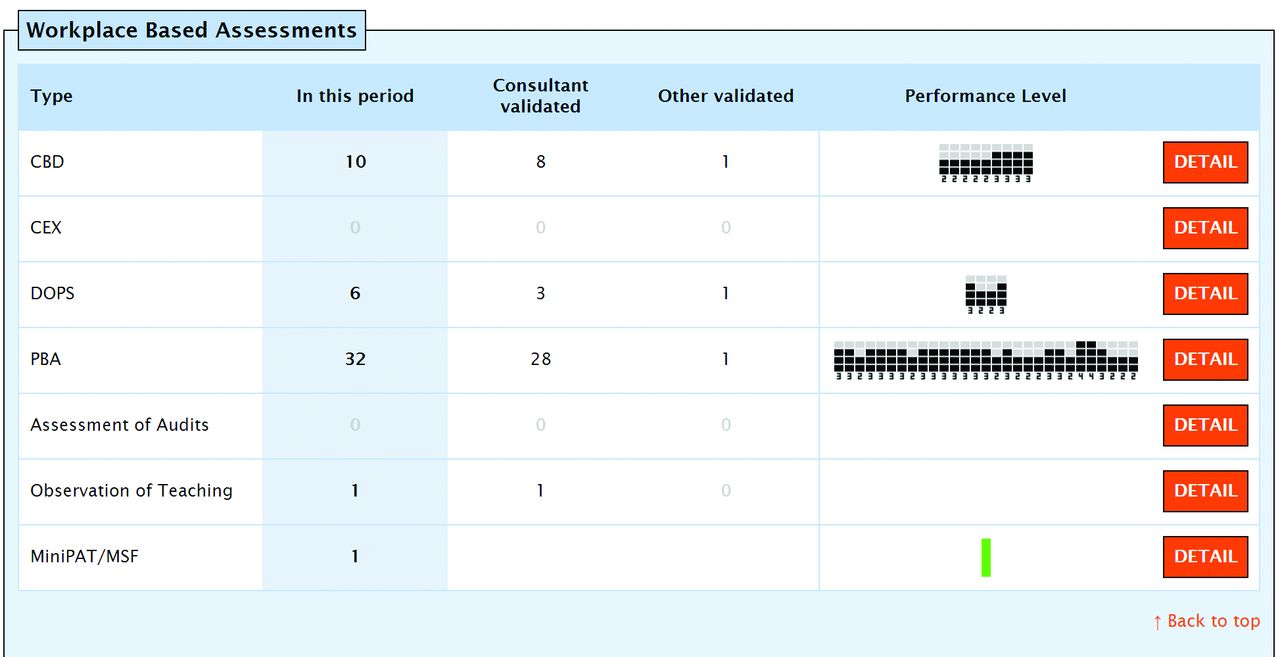
Fig. 5
ARCP WBA overview.
Training programmes up and down the UK have started to become more and more aware of the need to include supplementary training processes and simulation now forms 20% of all orthopaedic higher surgical teaching in the majority of regions. This has been combined with the annual UKITE (UK In Training Exam) which is based on the US OITE and provides training programme directors and their trainees with an objective assessment of their knowledge year on year and in comparison to their peer groups.
The NHS has made great strides in recent years to introduce more modern training with some success despite of the restriction of working hours. The shape of training report (www.shapeoftraining.co.uk) has been controversial, but has at its heart a competency based approach to continuing to provide excellence in medicine within the constraints of the current health care system.
Academic Training
The UK is unique in providing a separate academic pathway ahead of those available in the US or Australiasia. Although UK trainees in regular programmes are expected to be involved in clinical research (and will not pass their annual assessments without publication) there is a separate pathway for clinical academics. Funded through the National Institute for Health Research the academic pathway provides for an eight or nine year programme with dual clinical and academic training.
Trainees begin at the ACF (Academic Clinical Fellow) stage and for their first three years with have around 20% academic and 80% clinical time arranged to allow them to obtain funding for a PhD project which they will then undertake in their 4th and 6th years of training. Following their PhD, academic trainees are then either able to re-enter the training programme as traditional trainees or can opt to continue down the academic route with an ACL (Academic Clinical Lecturer) post which allows for a 50:50 research to clinical split. Clinicians in these posts have four years in which to complete their clinical training and set up a viable academic programme of study prior to starting as a clinical academic.
For those wishing to be a clinical academic the ACL and ACF programmes have provided a unique opportunity to combine clinical and academic training and reach the highest standards in each through a structured integrated programme of study.
Training specialists across the world
The duration of formal orthopaedic training programmes is similar across the US and Australasia, being between four and five years. After the introduction of the UK training grades, orthopaedic training (i.e. from ST3 to ST8) comprises six years. While the UK-trained surgeon will have a basic training in ‘surgery in general’, this is still one year longer than the longest training system elsewhere.
Assessment of trainee progress in the UK and Australasia is similar, all entailing a combination of tools, including operative logbook experience, research experience, and formal competency assessments of various procedures. The US residency programmes employ an annual standardised national examination.
ARCP progression requirements in the UK mean that orthopaedic trainees will have been involved in research of some capacity, however, this is more likely to be clinical in nature, and is certainly not typically a long-term ongoing project across a period of years, as in the US. There are only a small number of UK orthopaedic trainees who complete higher degrees (such as MSc, MD or PhD), although this is changing. Trainees often partake and are encouraged to obtain higher degrees in order to remain competitive when applying for jobs later in their career.
Conclusion
It’s difficult to conclude which is the right or wrong method of training to produce a safe and competent orthopaedic surgeon. The reduction in working hours brought about by the EWTD in the UK, with its inherent concerns regarding quality of training and achievement of competencies versus the potential improvement in quality of life and wellbeing, may have detrimental effects on the quality of newly qualified consultant surgeons. This sits in contrast to the working limit of 80 hours in the US and 72 hours (non-enforced) in Australia and New Zealand (Table I). It may be time in the UK for the pendulum to swing back to longer hours to allow for apprentice style training and increased surgical experience. It may also be feasible to shorten the training programme and allow a more direct route straight into orthopaedics as seen in other training countries.
Table I. Table showing the differences between the three countries
| Location | Length of orthopaedic training | Likely age at end of training | Max hours worked |
|---|---|---|---|
| Australasia | 4/5 | Variable | 72 |
| United Kingdom | 6 | 35 | 48 |
| United States | 4 | 33 | 80 |









