Abstract
Not all questions can be answered by prospective randomised controlled trials. Registries were introduced as a way of collecting information on joint replacements at a population level. They have helped to identify failing implants and the data have also been used to monitor the performance of individual surgeons. This review aims to look at some of the less well known registries that are currently being used worldwide, including those kept on knee ligaments, ankle arthroplasty, fractures and trauma.
Not all questions can be answered by prospective randomised controlled trials. Questions such as which is the best hip replacement, or at what age do patients cease to benefit from a ceramic bearing, require far too many patients for a conventional study. Registries are, in essence, large cohort studies and are therefore (by conventional evidence levels) at best Level III evidence. If one were to think, however, at a population level, and capture all the patients with a disease or intervention, they become Level I epidemiological studies.
The first and most venerable of the registries started life in 1979. With the stated aim of assessing the outcome of joint replacements, the Swedish Hip Registry started prospectively collecting information on all joint replacements throughout Sweden (Fig. 1).1 This ‘register’ would collect data on joint replacements, using re-operation and revision as failure parameters. Through high compliance and large case numbers with lengthy follow-up, the life-span of implants could be accurately measured. Other countries have since followed suit, the largest of which is the UK’s National Joint Registry (NJR) for England and Wales,2 with 1.2 million index procedures registered by March 2012, with up to eight years’ follow-up. Comparatively, the Swedish registry is smaller, but has up to 31 years’ follow-up. These arthroplasty registers represent a new way of studying the outcomes of disease and interventions: a broad brush ‘top down’ approach.
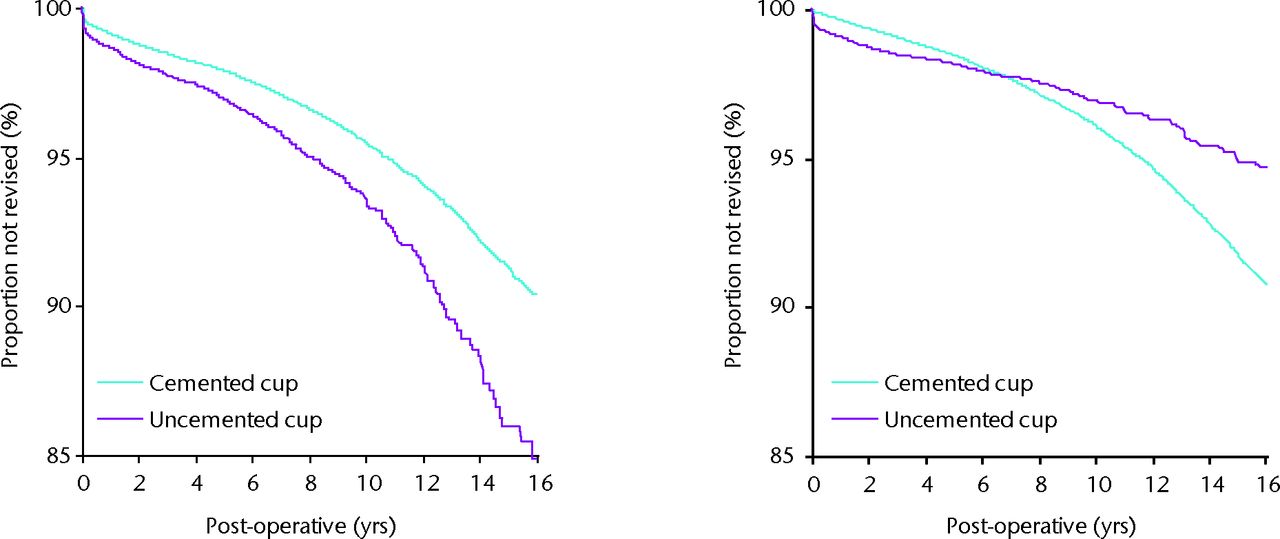
Fig. 1
Survival analysis of cementedversus uncemented stems and cups. Permission granted from the Swedish Hip Arthroplasty Register, 2011 (Garellick G, et al.The Swedish Hip Arthroplasty Register Annual Report, 2011.)
Registries like these have have proved successful in a number of ways. They have identified, and continue to identify, implants with high early failure rates, leading to implants being withdrawn from the market. They provide information that can help the surgeon decide the most appropriate implant and operative technique for their patients, and are able to tease out subtle questions such as which cement is best? Does canal lavage reduce loosening rates? Does surgical volume affect outcome? They can also be used to monitor the performance of surgical techniques, units and even individual surgeons.
However, registries are only as good as their design and management. Registries with low capture rates may lead to inaccurate data. The ideal situation is one where the whole population is included, and all operations and re-operations are registered. To do this well can be expensive.
The vast amounts of data they provide lead to lengthy reports, often with interesting findings hidden away. This article aims to draw together some of the most interesting findings from registry data around the world.
The initial orthopaedic registries were of hip and knee replacements. More recently, registry data have been collected on many other orthopaedic specialty areas, including knee ligament surgery, hip fractures and trauma.
Knee ligament registries
The Scandinavian countries have been trailblazers with registries of all types. Following hot on the heels of their comprehensive arthroplasty registries were the first national knee ligament registries. The Norwegian3 registry was started in 2004, followed by the Swedish1 and Danish versions in 2005.4-7 The Kaiser Permanente (KP) health organisation Anterior Cruciate Ligament (ACL) reconstruction registry5 was also started in 2005 in the USA and Norway. The KP organisation is a large private healthcare provider in the USA, and it invites its own surgeons to input data into the registry. It is therefore a voluntary large cohort study, not a national registry.
Data collected by these registries include epidemiological and aetiological information, pre- and post-operative Knee Injury and Osteoarthritis Outcome Score (KOOS),8 the type of grafts and implants used, and the presence of meniscal, cartilage and other injuries identified at the time of surgery. Revision rates are also recorded.6 The majority of data are collected on anterior cruciate ligament reconstruction (ACLR) but other ligaments are also included.
The latest published data from these registries (data from up to 2010), include over 10 000 patients in the Norwegian, Danish and KP registries, and over
17 000 patients in the Swedish registry. All quote compliance rates in their populations of over 85%.
These registries report that the median age for ACLR surgery is approximately 27 years, the majority of which occur in males. Soccer injuries appear to be the most implicated sport (even in the US registry).9 Clinically, KOOS scores improve post-operatively, and continue do so for up to five years (Swedish).10 Improvements after revision surgery are less than after primary surgery. Both pre-operatively and post-operatively, decreased improvement is seen after ACLR in smokers than non-smokers (Swedish).10 No significant improvement in KOOS scores has been identified in double-bundle ACLRs when compared with single-bundle ACLRs (Swedish).10
Geographical variations in graft selection have also been identified. The KP registry reports a low usage of autografts (only used in 61%) in all primary ACLRs in the USA (allografts were used in 37% of cases). Comparatively, by 2010, 96% of all primary ACLRs in Sweden were performed using hamstring autograft. The Swedish and Norwegian registries have identified an increase in the use of hamstring autograft and a corresponding reduction in the use of patellar tendon autograft since 2005. The Scandinavian registries have also revealed a shift towards a consensus of fixation methods. The vast majority of surgeons now use cortical buttons to achieve graft fixation on the femoral side and interference screw fixation on the tibial side (Swedish and Norwegian).
The registries highlight the importance of meniscal pathology, occurring in between 48% and 61% of cases requiring ligament reconstruction (the medial meniscus is injured in between 30% and 40%). The Norwegian registry has shown an increased trend in the suturing of meniscal injuries compared with resection since 2004. Synchronous articular cartilage injuries are found to occur in approximately 24% of cases. The incidence of meniscal damage and cartilage lesions identified at ACLR increases with increasing time from injury to surgery.4,6
Failure rates of ACLR are difficult to interpret due to the short follow-up period (only up to five years). The revision rate adjusted for person-years at risk has been identified globally as being extremely low (estimated at between 0.9% and 1.5%). Rates of PE, DVT and deep infection have been found to be extremely rare, at around 0.1%.
Unlike their arthroplasty counterparts, which focus mainly on comparative revision rates of differing prostheses, no figures in any registry have been published suggesting that any particular technique or implant have higher failure rates. This is partly due to the many different graft types and combinations (e.g. single/double bundle), and the many types of fixations available (the Norwegian registry contains 39 femoral fixation implants and 44 tibial fixation implants). Given time, more enrolled cases and higher consensus on surgical techniques differences are bound to emerge between techniques and implants in revision rates and outcomes.
The Swedish registry found that the rate of contralateral ACLR or revision ACLR of the index knee was 5% and 4.1%, respectively, at five years.11 The rate of revision in the Danish registry is very similar at five years (4.1%), and revision occurred most frequently after one to two years.10 The corresponding figure for 15- to 18-year-old female soccer players was 22%, making this the most clearly identified high-risk group. Once again, soccer is implicated as being the sport most likely to lead to ACLR rupture (Norwegian).
The Danish registry has published results that reveal a higher failure rate of allograft tissue when compared with autograft in revision surgery (RR 2.1 (95% CI 1.5 to 2.4); p < 0.01).10 The Danish registry identifies similar re-revision rates to primary ACLR of 5.4% at five years.
The findings from these registries are only as good as the data that are collected. While compliance rates are > 85%, the loss to follow-up (post-operative KOOS score), for example in the Swedish registry, was 60% at five-year follow-up. This therefore leads to concerns that reported failure rates of ACLR may not be entirely accurate. However, as national registries include the whole population, patients whose ACLRs fail (and require revision surgery) are more likely to be captured by the national registry, when compared with individual hospital or organisation registries such as the KP registry in the USA, where patients may undergo ACLR at one healthcare provider, and may then have their revision surgery at a different healthcare provider.
In summary, the knee ligament registries have been able to provide a large amount of information on the epidemiology and aetiology of ACL rupture and their associated injuries.12 Follow-up times are still relatively short, and it is hopeful that with time, further analysis may be performed that will identify superior methods of graft fixation and implants, with the aim of improving patient outcomes and reducing failure rates. Compliance and capture rates must remain high, and accurate recording of failures must be maintained.
Fracture registries
Once again the Scandinavian countries led the way with collection of registry data in fracture care. The Norwegian registry3 started to collect data on hip fracture patients in 2005, and the latest published report in 2010 had over 43 000 operations recorded. The Swedish Arthroplasty register13 only collects data on patients treated with arthroplasty while KP have kept a registry on their hip fracture patients in the US since 2009,14 and recently a hip fracture registry has been set up in Australia15 and New Zealand.16
The UK launched its own hip fracture registry in 2007 and it currently has over 200 000 cases of hip fracture in its National Hip Fracture Database (NHFD).17 This is now by far the largest fracture registry. All UK hospitals are registered and 97% regularly upload cases. The NHFD was introduced as part of a drive to improve the quality of care of hip fracture treatment in the UK. Uniquely, the NHFD monitors compliance, care quality and performance outcomes. This is ultimately linked to financial incentives. Six clear standards were set, and it monitors its performances against these standards. These include prompt admission to an orthopaedic ward from the Emergency Department (within four hours), surgery within 48 hours of admission, nursing care suitable to prevent pressure sore incidence, routine access to ortho-geriatric medical care pre- and post-operatively, assessment and application of bone health treatment and falls assessments. The UK government then set financial incentives for hospitals to achieve high quality care to treat this frail group of patients.
Huge amounts of epidemiological data have been identified on hip fracture patients, who have been termed ‘the frailest of the frail’.18 The displaced intracapsular fracture is the most common presentation (47%), with intertrochanteric and subtrochanteric fractures making up 34% and 5% of cases (NHFD), respectively. Total hip replacements (THR) now make up 16% of treatments for displaced intracapsular fracture in the UK, compared with 22% in Sweden (although there are significant geographical variations in Sweden with rates of THR of between 2% and 63%). The treatment types vary within the Scandinavian countries; in Norway 91% of all patients treated with arthroplasty receive a bipolar prosthesis, and unipolar implants are only used in 2% of cases (THR is used in 7%), compared with Sweden where THR rates are higher, and when a hemiarthroplasty is used a unipolar prosthesis is used approximately 66% of the time.
The NHFD has provided information that the mean combined length of stay of acute and post-acute care is improving in the UK, and is currently 21 days, leading to significant cost savings. A total of 9.1% of patients in the UK died in hospital after sustaining their hip fracture. Improvements in the UK have been made when compared with the standards mentioned previously with 83% undergoing surgery within 48 hours, and over 40% are reviewed by a specialist ortho-geriatrician pre-operatively.
The Swedish registry has also recently published information based on their data on rates of re-operation. They report that re-operation rates are higher after bipolar (when compared with unipolar) and uncemented hemiarthroplasty, although clearly, like all registry data, this may be subject to selection bias. The Swedes are also keen advocates of THR to treat hip fractures in active patients, providing data that THR leads to less pain and high satisfaction levels in patients both older and younger than 70 years.
There are no national registries on fracture care other than those for hip fractures. Is this an area that requires improvement to monitor the vast array of implants available in fracture treatment?
The hip fracture registries have provided large amounts of demographic data. A registry for hip fracture patients can help to identify appropriate treatments that are associated with lower failure and re-operation rates. Uniquely, when a national registry is associated with a package to drive quality improvement (such as in the NHFD) and the funding link to achieve these outcomes, this can have a real impact on patient outcomes.
Trauma registries
There are a number of large trauma registries worldwide, the largest of which is the National Trauma Data Bank (NTDB),19 a trauma registry based in the US that was established in 1989 and now contains more than five million records. It has collected a vast amount of information, and it uses this data to evaluate trauma trends, improve the quality of care, and aims to modify existing injury prevention and education programmes.
Information from the NTDB has shown that in the US in 2012, the largest number of accidents were caused by fall-related injuries (40%; 309 543 cases leading to 10 162 deaths), followed by motor-vehicle incidents (28%; 216 787 cases leading to 9425 deaths), although motor-vehicle incidents occur more frequently in younger individuals, while falls are more common over 40 years of age (Fig. 2). Firearm incidents make up 4% of all incidents, but 16% involved in firearm-related incidents die as a result.
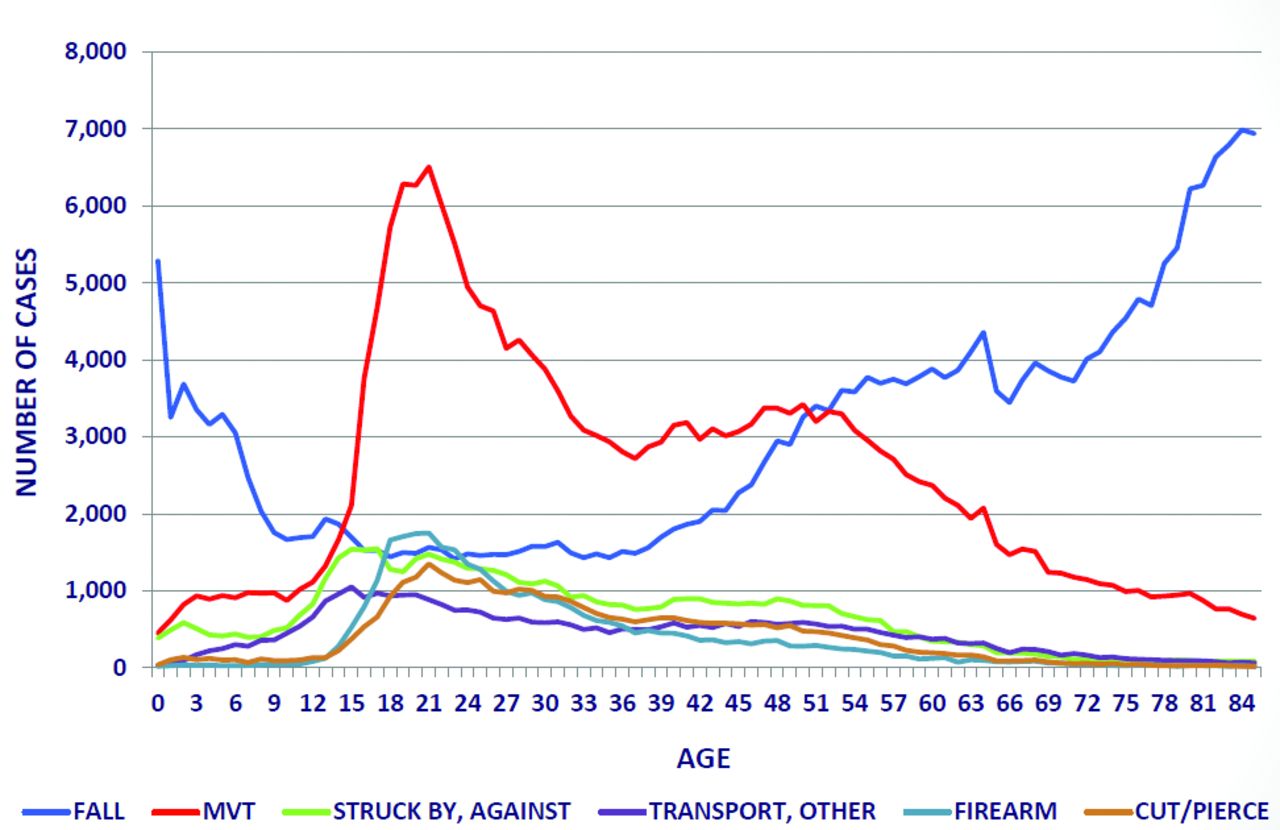
Fig. 2
Incidence of mechanism of injury related to age in the United States. Reproduced from National Trauma Data Bank 2012 Annual Report (American College of Surgeons. National Trauma Data Bank 2012 Annual Report.)
Up to the age of 70 years, men account for the majority of incidents, but after 70 years, most patients are women.
The NTDB uses the Injury Severity Score (ISS)20 to stratify injury severity. Mortality in the most severe group (ISS > 24) is 28%, and mortality rates in all ISS groups are higher in patients over 75 years.
Many other trauma registries exist worldwide, including the Japanese Trauma Data Bank,21 with almost 80 000 cases, and the Malaysian National Trauma Database (MNTD)22 with over 166 000 cases. In Japan, similar percentages of falls and motor-vehicle incidences occur, however, gunshot wounds only make up 0.06% of the trauma (compared with 4% in the USA). The MNTD analyses its data differently, looking only at the ‘major’ trauma cases (e.g. ISS > 15); in Malaysia, 77% of major trauma cases occur from motor-vehicle accidents, and only 7% from falls. Gunshot wounds only make up 0.2% of their major trauma cases. The UK Trauma Audit and Research Network (TARN)23 has collected data since 2008 and seeks to improve acute trauma care in the UK. In a similar manner to the NHFD, the UK Department of Health has started a system of ‘performance related pay’ for patients suffering major trauma and is managed within the new UK major trauma system. Although only implemented within the last year, the newest TARN reports demonstrate a huge increase in unexpected survivors as a result of this.
Large trauma databases such as these form an invaluable role in the identification and deliverance not only of trauma care, but also injury prevention. Countries without such trauma databases may use the data obtained from the sources such as the NTDB, however, local factors strongly influence injury presentations. Strong local trauma databases can therefore be advantageous and target resources to the areas of most need.
Ankle arthroplasty
Data on ankle arthroplasty are now regularly collected. Numbers are small, and length of follow-up is limited in many registries, lagging behind total hip and knee registries in terms of compliance, however, most ankle arthroplasty registries contain more complete data. Figure 3 demonstrates a typical data collection form, used by the Australian registry at times of primary surgery as well as at re-operation.
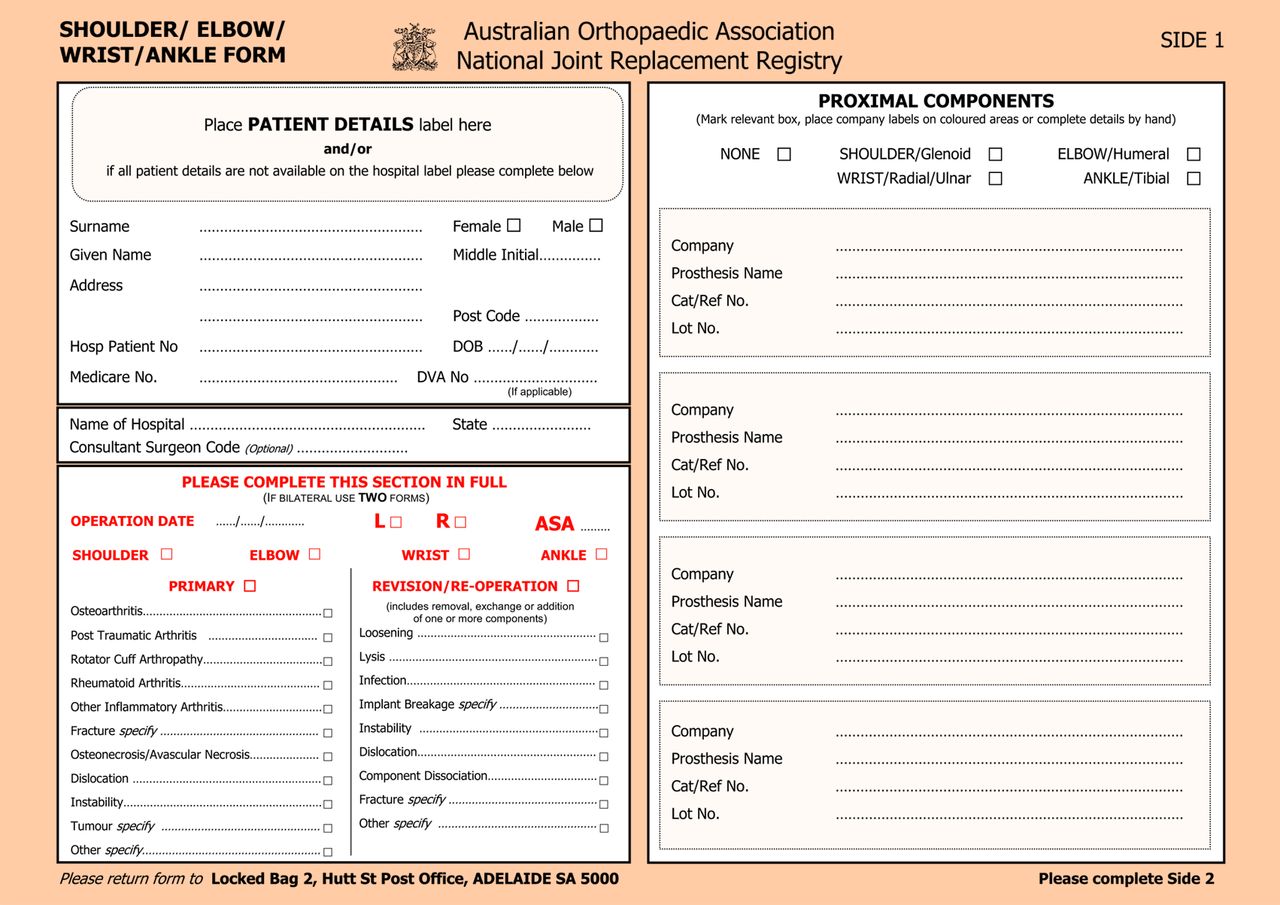
Fig. 3
FigCapA typical data collection form, taken from the Australian Joint registry: used for both primary surgery as well as re-operation for ankle, shoulder, wrist and elbow replacement.27
The New Zealand registry16 has up to 12 years of follow-up, although only 837 operations have been registered. Their latest report quotes revision rates of 1.4 per 100-component-years, while the Swedish registry24,25 has up to 18 years of follow-up (although with only 780 registrations) and reports an estimated ten-year survival at 69% (95% CI 67 to 71), although when the poorly performing STAR prosthesis was excluded from analysis, the ten-year survival was 78% (72% to 83%). It identified a 4% deep infection rate after ankle arthroplasty.
The Australian registry15 has larger numbers (1051 operations), but with shorter follow-up (four years), and found a cumulative failure rate of 10.1%. Again, the STAR prosthesis had the highest failure rate (5.39 per 100-component years; 95% CI 0.14 to 30.01). For all prostheses, loosening and lysis are the main reasons for revision (41%), followed by infection (11.5%). Insert revision was performed in 44.6% of cases, with only 12% having both implants exchanged, and 9.5% having implants removed.
The New Zealand registry also sent out Oxford-12 questionnaires26 to their patients at six months and five years post-surgery. At six months, 56% had a good or excellent score, and at five years, 64% achieved a good or excellent score. After revision surgery, this changed to 38%.
The National Joint Registry2 for England and Wales has recently started to collect data on ankle arthroplasty, however, data collection only started in April 2010. A total of 471 procedures have been recorded, however, limited analysis has been performed.
When compared with the hip and knee registries, the amount of data collected is tiny. However, ankle arthroplasty is on the increase, and the information gained from registry data is extremely valuable to monitor for failing implants.
Conclusion
Registry data is becoming a more and more familiar part of day-to-day life in orthopaedics, and there is valuable information contained in their reports, and not just concerning joint replacements. The data used in registries inform healthcare decisions at every level from government to individual surgical prosthesis selection and is much more wide ranging than one might think at first glance. The link of funding to registry data has been demonstrated to improve and push forward health care and outcomes effectively in two areas of trauma. Registries are, however, not a panacea; they are simply an audit of outcomes and are limited by their very nature. All registries suffer from profound selection bias and many use coarse outcome measures, meaning only large differences (death rates, revision rates) are likely to be reported. With the advent in the UK of ‘surgeon level’ data and the ability of patients to access a league table not just of hospitals but individual surgeons, registries are becoming more and more important in daily life.
1 Karholm J . The Swedish Hip Arthroplasty Register. Acta Orthop2010;81:3–4. Google Scholar
2 No authors listed. National Joint Registry for England and Wales. www.njrcentre.org.uk (date last accessed 29 August 2013). Google Scholar
3 No authors listed The Norwegian Arthroplasty Register; The Norwegian Cruciate Ligament Register; The Norwegian Hip Fracture Register.http://nrlweb.ihelse.net/eng/default.htm#Publications (date last accessed 29 August 2013). Google Scholar
4 Granan L , FrossbladM, LindM, EngebretsenL. The Scandinavian ACL registries 2004-2007: baseline epidemiology. Acta Orthop2009;80:563–567.CrossrefPubMed Google Scholar
5 Maletis G , GrnanaL, InacioM, FunahashiT, EngebretsenL. Comparison of community-based ACL reconstruction registries in the US and Norway. J Bone Joint Surg [Am]2011;93-A (Suppl):31–36. Google Scholar
6 Granan L , BahrR, LieS, EngebretsenL. Timing of anterior cruciate ligament reconstructive surgery and risk of cartilage lesions and meniscal tears: a cohort based on the Norwegian National Knee Ligament Registry. Am J Sports Med2009;37:955–961. Google Scholar
7 Lind M , MenhertF, PedersenA. The first results from the Danish ACL reconstruction registry: epidemiologic and 2 year follow-up results from 5,818 knee ligament reconstructions. Knee Surg Sports Traumatol Arthrosc2009;17:117–124.CrossrefPubMed Google Scholar
8 Roos EM , LohmanderLS. Knee injury and Osteoarthritis Outcome Score (KOOS): from joint injury to osteoarthritis. Health Qual Life Outcomes2003;1:64. Google Scholar
9 Paxton EW , NambaRS, MaletisGB, et al.A prospective study of 80,000 total joint and 5000 anterior cruciate ligament reconstruction procedures in a community-based registry in the United States. J Bone Joint Surg [Am]2010;92-A (Suppl):117–132.CrossrefPubMed Google Scholar
10 Lind M , MenhertF, PedersenA. Incidence and outcome after revision anterior cruciate ligament reconstruction: results from the Danish register for knee ligament reconstructions. Am J Sports Med2012;40:1551–1557. Google Scholar
11 No authors listed. Swedish ACL Register. Annual Report 2011. www.aclregister.nu (date last accessed 29 August 2013). Google Scholar
12 Engebretsen L , ForssbladM. Why knee ligament registries are important. Knee Surg Sports Traumatol Arthrosc2009;17:115–116.CrossrefPubMed Google Scholar
13 Garellick G, Kärrholm J, Rogmark C, Rolfson O, Herberts P. The Swedish Hip Arthroplasty Register Annual Report 2011. http://www.shpr.se (date last accessed 29 August 2013). Google Scholar
14 No authors listed. Kaiser Permanente. Registries: Hip Fracture. http://kpimplantregistries.org/Registries/Hip_Fracture.htm (date last accessed 29 August 2013). Google Scholar
15 No authors listed. Australian Orthopaedic Association: demographics and outcome of ankle arthroplasty: supplementary report to the Annual Report 2012. https://aoanjrr.dmac.adelaide.edu.au/ (date last accessed 29 August 2013). Google Scholar
16 No authors listed. The New Zealand Joint Registry. http://www.nzoa.org.nz/nz-joint-registry (date last accessed 29 August 2013). Google Scholar
17 No authors listed. The National Hip Fracture Database. http://www.nhfd.co.uk/ (date last accessed 29 August 2013). Google Scholar
18 No authors listed. BOA welcomes latest hip fracture report. http://www.boa.ac.uk/About/CEOBlog/Lists/Posts/Post.aspx?ID=174 (date last accessed 29 August 2013). Google Scholar
19 No authors listed. National Trauma Data Bank 2012 Annual Report. http://www.facs.org/trauma/ntdb/pdf/ntdb-annual-report-2012.pdf (date last accessed 29 August 2013). Google Scholar
20 Baker SP , O'NeillB, Haddon JrW, LongWB. The injury severity score: a method for describing patients with multiple injuries and evaluating emergency care. J Trauma1974;14:187–196.PubMed Google Scholar
21 No authors listed. Japan Trauma Data Bank Report 2012 (2007-2012). http://www.jtcr-jatec.org/ (date last accessed 29 August 2013). Google Scholar
22 No authors listed. National Trauma Database. http://www.acrm.org.my/ntrd/publication.html (date last accessed 29 August 2013). Google Scholar
23 23. No authors listed. Trauma Audit and Research Network. www.tarn.ac.uk (date last accessed 29 August 2013). Google Scholar
24 Henricson A , NilssonJA, CarlssonA. 10-year survival of total ankle arthroplasties: a report on 780 cases from the Swedish Ankle Register. Acta Orthop2011;82;655-9.:.CrossrefPubMed Google Scholar
25 25. No authors listed. The Swedish Ankle Register. www.swedankle.se (date last accessed 29 August 2013). Google Scholar
26 Dawson J , FitzpatrickR, CarrA, MurrayD. Questionnaire on the perceptions of patients about total hip replacement. J Bone Joint Surg [Br]1996;78-B:185–190.PubMed Google Scholar
27 No authors listed. National Joint Replacement Registry: multijoint form. https://aoanjrr.dmac.adelaide.edu.au/data-collection (date last accessed 29 August 2013). Google Scholar









