Abstract
Blast and ballistic weapons used on the battlefield cause devastating injuries rarely seen outside armed conflict. These extremely high-energy injuries predominantly affect the limbs and are usually heavily contaminated with soil, foliage, clothing and even tissue from other casualties. Once life-threatening haemorrhage has been addressed, the military surgeon’s priority is to control infection.
Combining historical knowledge from previous conflicts with more recent experience has resulted in a systematic approach to these injuries. Urgent debridement of necrotic and severely contaminated tissue, irrigation and local and systemic antibiotics are the basis of management. These principles have resulted in successful healing of previously unsurvivable wounds. Healthy tissue must be retained for future reconstruction, vulnerable but viable tissue protected to allow survival and avascular tissue removed with all contamination.
While recent technological and scientific advances have offered some advantages, they must be judged in the context of a hard-won historical knowledge of these wounds. This approach is applicable to comparable civilian injury patterns. One of the few potential benefits of war is the associated improvement in our understanding of treating the severely injured; for this positive effect to be realised these experiences must be shared.
It has been speculated that improvements in body armour during the recent conflicts in the early 21st century have resulted in an increased preponderance of extremity wounds. However, the overall proportion of casualties with limb injuries has remained relatively consistent over the last century of warfare at 50% to 60%.1 One quarter of these extremity injuries are open fractures.2 It is reasonable to anticipate that limb wounds will continue to be the principle burden of injury in future conflicts.
While haemorrhage control and resuscitation is the priority of early treatment of combat injuries, the focus of subsequent surgery evolves to address the prevention and treatment of infection. Wound infection is associated with delayed amputation,3-5 higher amputation levels6 and re-hospitalisation.7,8 Currently infection complicates approximately a quarter of Gustilo and Anderson (GA) grade III9 open tibia fractures in UK and US combat casualties.5,10
This paper examines the current concepts of wound infection as used to guide treatment strategies in the Royal Centre for Defence Medicine and how these have been influenced by the historic experiences from previous conflicts and current experimental data.
Mechanism of Injury
Excluding the initial phases of the war in Iraq, approximately 80% of injuries are due to blast weapons.1,11 These can range from military munitions such as rockets and mortar-bombs to Improvised Explosives Devices (IED), including the buried IED initiated by the victim walking onto the device, which has become ubiquitous in Afghanistan.12
These weapons cause extensive soft-tissue damage, extreme stripping of tissue away from underlying comminuted fractures and driving debris along fascial planes. The extent of contamination is hard to exaggerate with dirt, foliage, clothing and even tissue from other casualties frequently being driven deep into wounds, as shown in figure 1.

Fig. 1
Gross contamination following blast injury immediately prior to debridement. Image shown with permission of patient. © Crown Copyright 2013.
The combat wound
Combat wounds are heterogeneous, irregular and complex, however, certain key characteristics can be effectively modelled using the concept originally proposed in 1953 by Jackson.13 The Jackson wound model describes a wound in terms of three zones: 1) the zone of coagulation-dead, avascular tissue; 2) a zone of stasis–potentially viable tissue that is damaged and vulnerable; and 3) the lightly damaged zone of hyperaemia which is likely to survive unless subject to significant further insult. This is shown schematically in Figure 2. The Jackson wound model is useful for understanding the basis of many treatment strategies and the behaviour of the wound.
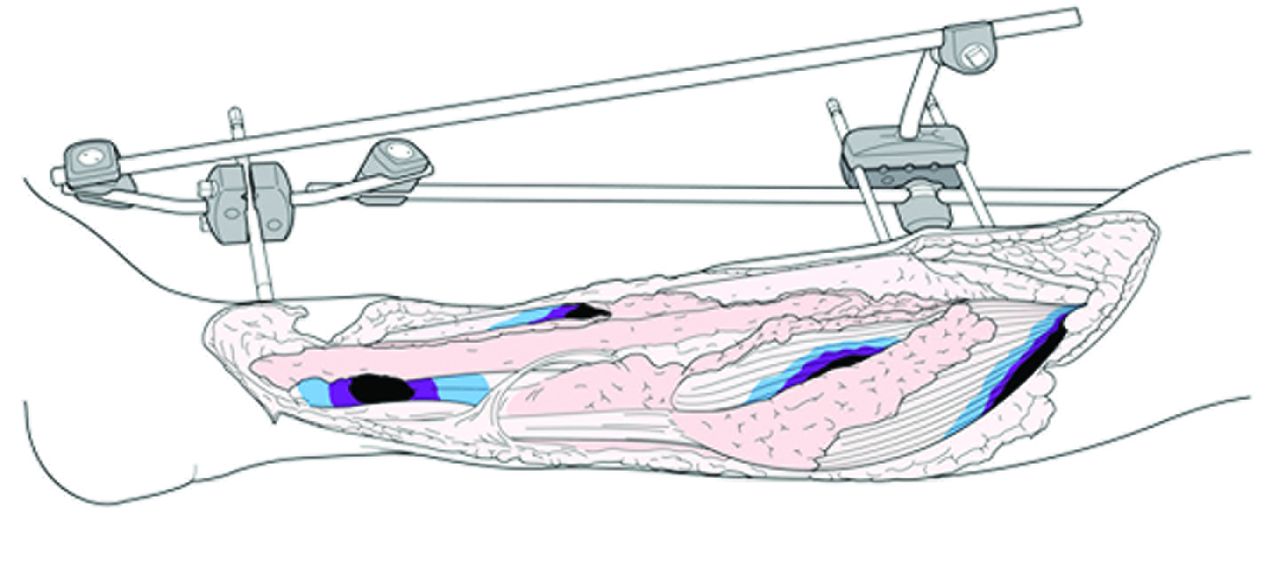
Fig. 2
Diagram of complex open fracture wounds showing zones of necrosis (black), surrounded by vulnerable but potentially viable zones of stasis (purple), surrounded by the zones of hyperaemia (blue). © Crown Copyright 2013
Wounds that have been created by blast weapons have been observed to evolve with tissue in the zone of stasis progressing toward necrosis over several days following initial injury. This progression necessitates delayed primary closure with repeated inspections to ensure that the wound is not closed or covered while it still contains necrotic tissue. Figure 3 shows the appearance of wounds after initial debridement.

Fig. 3
The blast wounds as shown in figure 1 after the initial debridement. Image shown with permission of patient. © Crown Copyright 2013
In 1914, military surgeons were surprised by the aggression of clostridial wound infections in soldiers injured in the heavily manured fields of Flanders.14 Similarly, the wounds of military casualties injured while patrolling on foot in the irrigated agricultural areas alongside the river Helmand, known as ‘the green zone’, have been complicated by infection with unexpected microbes including filamentous fungi15 and the gram-negative Aeromonas hydrophila.6 However, despite the attention focused on atypical infections, the most common organism isolated from infected combat wounds remains un-exotic strains of Staphylococci.10
Treatment timelines
In 1898 Frederich shared his work on the effect of delaying surgical treatment of contaminated soft-tissue wounds in guinea-pig forearms. He showed that when the surgical debridement of contaminated wounds was performed within six hours, no animals developed infection, but when it was delayed beyond this point, they all became infected.
Later animal studies also echoed this finding that delaying surgery allows bacteria to flourish and subsequent infection rates increase16-18 and therefore the ‘six-hour rule’ was widely adopted and enshrined into the 1997 BAPRAS-BOA report on open tibia fractures.19 However, subsequently a large number of observational clinical studies found that the risk of infection or non-union did not increase despite delayed debridement in patients who had received early systemic antibiotics.20-32 A component of the Lower Extremity Assessment Project (LEAP) included a prospective observational study of 315 patients with GA III open fractures of the tibia, foot and ankle. In a multi-variant regression analysis they also found that delay between injury and surgical debridement was not related to infection rate.33 This lead to the current BAPRAS-BOA standards on lower limb open fracture management from explicitly rejecting the six-hour rule in 2009 in favour of surgery within 24 hours by an appropriately senior team.34
The opposing conclusions drawn by the animal studies and the majority of observational case-series can be explained by their respective methodologies. Animal studies examining the timing of surgical debridement do not typically involve systemic antibiotic administration, which may well make delaying surgery ‘safer’ with respect to infection. When this variable has been included in animal studies, the effect of delayed surgery is reduced but not negated.35
For obvious ethical reasons all clinical studies to date have been observational in methodology. The likely tendency of clinicians to prioritise the most heavily contaminated injuries for earlier surgical debridement means that when these injuries unsurprisingly become subsequently infected, the effect is to ‘balance’ delayed and early surgical cohorts with respect to subsequent infection. Another confounder in observational studies is that attempts to treat open fractures surgically, on an emergent basis has traditionally resulted in surgical trainees managing cases overnight. There is a suspicion that this has led in some instances to inadequate debridement and potentially unnecessary infections.
In UK military deployed surgical facilities, consultant surgeons deliver care. In practice this means that casualties with open fractures have their injuries debrided and stabilised by a consultant surgeon, typically within two hours of injury. As the UK trauma networks mature, and management of severe injuries is increasingly concentrated at dedicated centres, the provision of 24-hour consultant surgeon cover may become a reality and reversion to the six-hour rule may warrant consideration.
Damage control orthopaedics
Damage Control is the Naval system by which a ship’s company perform temporary repairs to prolong the ship’s ability to float and fight until definitive repair is possible. The surgical version of this concept of quick, temporary repair was suggested by US trauma surgeons in the 1970s.36 Interestingly, in orthopaedics at the same time, early stabilisation of long bone fractures was becoming the recognised strategy known as ‘Early Total Care’ (ETC).37 Unfortunately, it was a strategy that was often applied without sufficient thought or case selection, and Pape’s seminal paper in 199338 drew the connection between early intramedullary nailing and lung complications. Thus, the orthopaedic community belatedly followed their general surgical colleagues into the era of damage control surgery. The practice of initial surgical treatment of wounds and skeletal stabilisation with internal fixation before definitive treatment some days later is now widely accepted.
The era of ETC was also the time of patients being ‘resuscitated’ according to the then ATLS guidance with excessive crystalloid solutions,39 before the dangers of hypothermia, coagulopathy and hypoperfusion were fully understood. However, resuscitation techniques have evolved: in deployed military medical facilities, casualties with Injury Severity Scores above 40 are regularly physiologically normalised within an hour or two of arrival by a team of two or three anaesthetists. This aggressive resuscitation of patients with large volumes of blood products infused at rates up to 1l/min is tailored to an individual’s coagulopathy as measured by real time thromboelastography.40 Restoration of adequate tissue perfusion as demonstrated by normalised serum lactate is indicative of blood flow restoration to injured tissue and it is reasonable to speculate that this reduces subsequent tissue necrosis and infection in the wound.
With the establishment of Major Trauma Centres, it should be possible for these resuscitation techniques to be adopted in the civilian setting, meaning that fewer patients are so physiologically deranged as to be unfit for anything other than temporary surgical stabilisation.
Irrigation
Lister first described the use of carbolic acid to reduce the bacterial load in open fractures in 1867.41 Although his results were not presented scientifically, his techniques were recognised by his peers as offering an unprecedented improvement in infection rates in open fractures. With hindsight much of his improvement might be attributed to the application of carbolic acid to the surgeon and their instruments rather than directly to the wounds they were treating.
Up to and during the First World War, many surgeons continued to use carbolic acid and experimented with a variety of antiseptic formulations including boric acid, flavine and Bismuth Iodine Paraffin Paste.42 During the First World War Fleming took numerous samples of wound tissue from injured soldiers treated in allied field hospitals and demonstrated that the use of antiseptics in open fracture wounds actually increased bacteria loads. He ascribed this counterintuitive observation to the toxicity of chemical antiseptics to the host immune system, which he thought was the most important factor in wound infection. He summarised this position thus: “it also makes it necessary in the estimation of the value of an antiseptic, to study its effect on the tissue more than its effect on the bacteria”.43
The detrimental effect of seemingly innocuous antiseptics can be understood by evoking the Jackson wound model. Antiseptics kill most, but not all of the bacteria in the wound; they also damage the vulnerable but viable tissue in the zone of stasis, tipping some tissue into non-viability. This necrotic material then acts as an avascular growth media for the remaining bacteria in the wound to ‘rebound’.
This explanation is supported by the experimental findings of Owens, White and Wenke44 who compared disinfectants with saline with respect to lowering bacterial counts in an animal wound model of contaminated open fracture. They found that although immediately after irrigation disinfectants were more effective than saline at reducing levels of bacteria, 48 hours later there was a significant rebound of bacterial growth in the disinfectant groups.44 This is only one of many studies, both animal45-47 and clinical,48,49 that have failed to demonstrate superiority of any irrigation fluid over saline while frequently demonstrating a deleterious effect.
Similarly the use of higher-pressure irrigation systems has been evaluated and found to drive bacteria further into already damaged tissue.50
Currently surgeons should only ever use low-pressure saline to irrigate open fractures. However, we eagerly await the results of the FLOW trial, which is prospectively comparing the efficacy of irrigation with saline and castile soap solution at a variety of pressures at reducing infection following open fracture.
Antibiotics
The first randomised controlled trial to evaluate the efficacy of antibiotics in preventing infection in open fractures was conducted on military patients by Cutler, Morton and Sandusky51 in 1944 and failed to demonstrate a reduction in subsequent infection rate.51 However, with the further refinement of antibiotics, clear beneficial effects of prophylactic antibiotics have subsequently been demonstrated52 and accepted as a fundamental component of preventing infection in open fractures.
While most clinicians would recognise that antibiotics should be administered early34 there is still debate amongst military clinicians as to how urgent this is, and whether antibiotics should be administered by pre-hospital medics.53 This strategy appears to be supported by historical experiences. British servicemen in Borneo between 1963 and 1965 were issued oral oxytetracylcine to take immediately if injured. Wound infection rates were lower in these casualties than those with similar injuries who were not issued antibiotics during the 1982 Falklands conflict. However, this difference was only observed in patients reaching surgery within six hours, and numbers were too small to reach significance.54,55
In the Falklands conflict, seven of the nine cases of wound infection did not have initial antibiotics administered in the first six hours after injury. There was no infection when antibiotics were administered within three hours.
This historical experience was supported by a recent basic science study that demonstrated early antibiotic administration was more important than early surgery, and when antibiotic administration was delayed, postponing surgery dramatically increased infection.35
The duration of antibiotic therapy is also a subject of current debate. Current BAPRAS-BOA standards recommend antibiotic therapy for 72 hours or until wound closure, whichever is sooner.34 However, anecdotally, most surgeons might admit to leaving patients on antibiotics for a longer period. The only randomised control trial looking at the question of the duration of prophylactic antibiotics was published by Dellinger et al32 in 1988. They found no difference in infection rates in patients treated with one or five days of a cephalosporin. Similarly a contemporary observational study of 1492 open fractures found no relation between risk of infection and length of prophylactic antibiotic therapy.56
Current military practice is to treat all open fractures with 1.2 g of intravenous co-amoxiclav every eight hours, and if patients show any signs of wound sepsis, then this is augmented with 1 g of intravenous meropenem every eight hours. Casualties with heavily contaminated wounds who are injured while on foot patrol in agricultural areas have high risk of developing fungal wound infections and are given ambisome 15 mg/kg and posaconazole 200 mg.
Topical negative pressure therapy (TNP)
The large soft-tissue wounds associated with combat injuries are challenging to dress after debridement. Even with adequate haemostasis, there is considerable exudate from the wound, which can readily saturate dressings leading to a wound lying in soggy, potentially contaminated material. This is not only a pro-infective environment, but is rapidly malodorous and can distress a conscious patient. The UK Military practice is to dress significant wounds with TNP between surgical episodes: it is believed that in certain cases this allows a greater delay between surgical debridements than the traditional two to three days, particularly when a patient is physiologically unstable.57 However, it is acknowledged that there is little evidence to support TNP use in preference to traditional dressings.58,59
The only RCT so far on this subject was published by Stannard et al60 in 2009, which found that in civilian open fractures TNP was superior to wet-to-dry gauze dressings in respect to reducing subsequent infection. This study has limited applicability to the military population due to the differences between combat injuries and those encountered in the civilian setting. A further criticism of this study is that the control group of gauze dressings is not a likely current clinical alternative to TNP. The ‘bead-pouch’ technique has been used for 30 years61 and provides a method for sealing a wound while simultaneously creating a very high local concentration of antibiotic.
The compatibility of local antibiotics with TNP has been explored in an animal model of a complex wound. Stinner, Hsu and Wenke62 found that the bacteria load was most effectively reduced by use of a bead pouch alone and the addition of TNP increased the bacteria found in the wound.
The WOLFF study is currently recruiting patients and is comparing TNP with current best practice including the bead-pouch technique. A challenge of a trial of this type is comparing a relatively standardised wound dressing with a variety of alternatives from conventional dressings, to a bead-pouch. However, the results will doubtless increase the evidence for clinicians managing these injuries.
Conclusion
The last ten years of continuous conflict have encouraged military surgeons to examine carefully the experience of their predecessors in previous conflicts. While not wanting to reject the hard-learnt lessons from history, the emergence of new techniques and evidence require clinicians to re-appraise accepted practice.
Wounds sustained on the modern battlefield are typically high energy, involving devastating soft-tissue damage and require extensive debridement. The casualties from the last decade of continuous conflict have all passed through a single UK hospital allowing the accumulation of extensive experience in managing these challenging wounds, which often occur in the context of devastating multi-system trauma.
While injuries as severe as these are rarely encountered in civilian settings, the techniques and strategies outlined in this paper are readily transferable to civilian practice. In our experience, open fracture wounds should be debrided in theatre by a suitably experienced surgical team as soon as possible as delay increases infection; wounds should only be irrigated with saline; systemic antibiotics should be initiated as rapidly as possible and consideration should be given to the use of local antibiotics. TNP is a valuable treatment option, particularly when managing wounds with extensive tissue loss or destruction. In the experience of the military, care that is always consultant-led and -delivered will not only be of a higher standard but will also allow decisions to be made faster.
Experience has shown that consistent application of these basic techniques and strategies can achieve low rates of infection and amputation even in devastated limbs. It is this model that will drive the ethos of our new Major Trauma Networks. This requires extensive (and expensive) re-organisation, and the flexibility and teamwork espoused by the military.
1 Owens BD , Kragh JF Jr, WenkeJC, et al.Combat wounds in operation Iraqi Freedom and operation Enduring Freedom. J Trauma2008;64:295–259.CrossrefPubMed Google Scholar
2 Owens BD , Kragh JF Jr, MacaitisJ, SvobodaSJ, WenkeJC. Characterization of extremity wounds in Operation Iraqi Freedom and Operation Enduring Freedom. J Orthop Trauma2007;21:254–257.CrossrefPubMed Google Scholar
3 Johnson EN , BurnsTC, HaydaRA, HospenthalDR, MurrayCK. Infectious complications of open type III tibial fractures among combat casualties. Clin Infect Dis2007;45:409–415.CrossrefPubMed Google Scholar
4 Huh J , StinnerDJ, BurnsTC, HsuJR. Infectious complications and soft tissue injury contribute to late amputation after severe lower extremity trauma. J Trauma2011;71 Suppl:S47–S51.CrossrefPubMed Google Scholar
5 Penn-Barwell JG , BennettPM, FriesCA, et al.Severe open tibial fractures in combat trauma: Management and preliminary outcomes. Bone Joint J2013;95-B:101–105.CrossrefPubMed Google Scholar
6 Penn-Barwell JG , FriesCA, SargeantID, BennettPM, PorterK. Aggressive soft tissue infections and amputation in military trauma patients. J R Nav Med Serv2012;98:14–18.PubMed Google Scholar
7 MacKenzie EJ , BosseMJ, PollakAN, et al.Long-term persistence of disability following severe lower-limb trauma. Results of a seven-year follow-up. J Bone Joint Surg [Am]2005;87-A:1801–1809.CrossrefPubMed Google Scholar
8 MacKenzie EJ , BosseMJ. Factors influencing outcome following limb-threatening lower limb trauma: lessons learned from the Lower Extremity Assessment Project (LEAP). J Am Acad Orthop Surg2006;14 Spec No:S205–S210.CrossrefPubMed Google Scholar
9 Gustilo RB , AndersonJT. Prevention of infection in the treatment of one thousand and twenty-five open fractures of long bones: retrospective and prospective analyses. J Bone Joint Surg [Am]1976;58-A:453–458.PubMed Google Scholar
10 Burns TC , StinnerDJ, MackAW, et al.Microbiology and injury characteristics in severe open tibia fractures from combat. J Trauma Acute Care Surg2012;72:1062–1067.CrossrefPubMed Google Scholar
11 Bennett PM , SargeantID, MidwinterMJ, Penn-BarwellJG. Unilateral lower limb loss following combat injury: Medium-term outcomes in British military amputees. Bone Joint J2013;95-B:224–229.CrossrefPubMed Google Scholar
12 Ramasamy A , HillAM, HepperAE, BullAM, ClasperJC. Blast mines: physics, injury mechanisms and vehicle protection. J R Army Med Corps2009;155:258–264.CrossrefPubMed Google Scholar
13 Jackson DM . The diagnosis of the depth of burning. Br J Surg1953;40:388–396. Google Scholar
14 Fleming A . On the bacteriology of war wounds. Lancet1915;186:638–643. Google Scholar
15 Warkentien T , RodriguezC, LloydB, et al.Invasive mold infections following combat-related injuries. Clin Infect Dis2012;55:1441–1449.CrossrefPubMed Google Scholar
16 Owen-Smith MS , MathesonJM. Successful prophylaxis of gas gangrene of the high-velocity missile wound in sheep. Br J Surg1968;55:36–39.CrossrefPubMed Google Scholar
17 Brown KV , WalkerJA, CortezDS, MurrayCK, WenkeJC. Earlier debridement and antibiotic administration decrease infection. J Surg Orthop Adv2010;19:18–22.PubMed Google Scholar
18 Dhingra U , SchauerhamerRR, WangensteenOH. Peripheral dissemination of bacteria in contaminated wounds; role of devitalized tissue: evaluation of therapeutic measures. :. Surgery1976;80:535–543. Google Scholar
19 No authors listed. A report by the British Orthopaedic Association/British Association of Plastic Surgeons Working Party on the management of open tibial fractures: September 1997. Br J Plast Surg 1997;50:570-583. Google Scholar
20 Patzakis MJ , Harvey JP Jr, IvlerD. The role of antibiotics in the management of open fractures. J Bone Joint Surg [Am]1974;56-A:532–541.PubMed Google Scholar
21 Bednar DA , ParikhJ. Effect of time delay from injury to primary management on the incidence of deep infection after open fractures of the lower extremities caused by blunt trauma in adults. J Orthop Trauma1993;7:532–525.CrossrefPubMed Google Scholar
22 Harley BJ , BeaupreLA, JonesCA, DulaiSK, WeberDW. The effect of time to definitive treatment on the rate of nonunion and infection in open fractures. J Orthop Trauma2002;16:484–490.CrossrefPubMed Google Scholar
23 Skaggs DL , FriendL, AlmanB, et al.The effect of surgical delay on acute infection following 554 open fractures in children. J Bone Joint Surg [Am]2005;87-A:8–12.CrossrefPubMed Google Scholar
24 Khatod M , BotteMJ, HoytDB, et al.Outcomes in open tibia fractures: relationship between delay in treatment and infection. J Trauma2003;55:949–954.CrossrefPubMed Google Scholar
25 Ashford RU , MehtaJA, CrippsR. Delayed presentation is no barrier to satisfactory outcome in the management of open tibial fractures. Injury2004;35:411–416.CrossrefPubMed Google Scholar
26 Spencer J , SmithA, WoodsD. The effect of time delay on infection in open long-bone fractures: a 5-year prospective audit from a district general hospital. Ann R Coll Surg Engl2004;86:108–112.CrossrefPubMed Google Scholar
27 Charalambous CP , SiddiqueI, ZeniosM, et al.Early versus delayed surgical treatment of open tibial fractures: effect on the rates of infection and need of secondary surgical procedures to promote bone union. Injury2005;36:656–661.CrossrefPubMed Google Scholar
28 Naique SB , PearseM, NanchahalJ. Management of severe open tibial fractures: the need for combined orthopaedic and plastic surgical treatment in specialist centres. J Bone Joint Surg [Br]2006;88-B:351–357.CrossrefPubMed Google Scholar
29 Al-Arabi YB , NaderM, Hamidian-JahromiAR, WoodsDA. The effect of the timing of antibiotics and surgical treatment on infection rates in open long-bone fractures: a 9-year prospective study from a district general hospital. Injury2007;38:900–905.CrossrefPubMed Google Scholar
30 Al-Hilli AB , SalihDS. Early or delayed surgical treatment in compound limb fractures due to high velocity missile injuries: a 5-year retrospective study from Medical City in Baghdad. Iowa Orthop J2010;30:94–98. Google Scholar
31 Reuss BL , ColeJD. Effect of delayed treatment on open tibial shaft fractures. Am J Orthop (Belle Mead NJ)2007;36:215–220.PubMed Google Scholar
32 Dellinger EP , MillerSD, WertzMJ, et al.Risk of infection after open fracture of the arm or leg. Arch Surg1988;123:1320–1327. Google Scholar
33 Pollak AN , JonesAL, CastilloRC, BosseMJ, MacKenzieEJ. The relationship between time to surgical debridement and incidence of infection after open high-energy lower extremity trauma. J Bone Joint Surg [Am]2010;92-A:7–15.CrossrefPubMed Google Scholar
34 Nanchahal J, Nayagam S, Khan U, et al. Standards of the Management of Open Fractures of the Lower Limb, First edition. London: Royal Society of Medicine Press, 2009. Google Scholar
35 Penn-Barwell JG , MurrayCK, WenkeJC. Early antibiotics and debridement independently reduce infection in an open fracture model. J Bone Joint Surg [Br]2012;94-B:107–112.CrossrefPubMed Google Scholar
36 Lucas CE , LedgerwoodAM. Prospective evaluation of hemostatic techniques for liver injuries. J Trauma1976;16:442–451.CrossrefPubMed Google Scholar
37 Riska EB , von BonsdorffH, HakkinenS, et al.Primary operative fixation of long bone fractures in patients with multiple injuries. J Trauma1977;17:111–121.CrossrefPubMed Google Scholar
38 Pape HC , Auf'm'KolkM, PaffrathT, et al.Primary intramedullary femur fixation in multiple trauma patients with associated lung contusion--a cause of posttraumatic ARDS?J Trauma1993;34:540–547.CrossrefPubMed Google Scholar
39 Alexander RH, Proctor HJ, American College of Surgeons. Committee on Trauma. Advanced trauma life support program for physicians: ATLS. fifth edition. Chicago: American College of Surgeons, 1993. Google Scholar
40 Allcock EC , WoolleyT, DoughtyH, et al.The clinical outcome of UK military personnel who received a massive transfusion in Afghanistan during 2009. J R Army Med Corps2011;157:365–369.CrossrefPubMed Google Scholar
41 Lister J . On a new method of treating compound fracture, abscess, and so forth; with observations on the conditions of suppuration. :. Lancet1867;89:326. Google Scholar
42 Browning CH , GulbransenR, KennawayEL, ThorntonLH. Flavine and Brilliant Green, Powerful Antiseptics with Low Toxicity to the Tissues: Their Use in the Treatment of Infected Wounds. Br Med J1917;2925:73–78.CrossrefPubMed Google Scholar
43 Fleming A . Chemical and Physiological Antiseptics: The Action of Chemical and Physiological Antiseptics in a Septic Wound. Br J Surg1919;7:99–129. Google Scholar
44 Owens BD , WhiteDW, WenkeJC. Comparison of irrigation solutions and devices in a contaminated musculoskeletal wound survival model. J Bone Joint Surg [Am]2009;91-A:92–98.CrossrefPubMed Google Scholar
45 Branemark PI , EkholmR. Tissue injury caused by wound disinfectants. J Bone Joint Surg [Am]1967;49-A:48–62.PubMed Google Scholar
46 Penn-Barwell JG , MurrayCK, WenkeJC. Comparison of the antimicrobial effect of chlorhexidine and saline for irrigating a contaminated open fracture model. J Orthop Trauma2012;26:728–732.CrossrefPubMed Google Scholar
47 Brennan SS , LeaperDJ. The effect of antiseptics on the healing wound: a study using the rabbit ear chamber. Br J Surg1985;72:780–782.CrossrefPubMed Google Scholar
48 Anglen JO . Comparison of soap and antibiotic solutions for irrigation of lower-limb open fracture wounds: a prospective, randomized study. J Bone Joint Surg [Am]2005;87-A:1415–1422. Google Scholar
49 Crowley DJ , KanakarisNK, GiannoudisPV. Irrigation of the wounds in open fractures. J Bone Joint Surg [Br]2007;89-B:580–585.CrossrefPubMed Google Scholar
50 Bhandari M , AdiliA, LachowskiRJ. High pressure pulsatile lavage of contaminated human tibiae: an in vitro study. J Orthop Trauma1998;12:479–484.CrossrefPubMed Google Scholar
51 Cutler EC , MortonPC, SanduskyWR. Observations on the Prophylactic Use of Penicillin in the wounds of Aerial Warfare. Br J Surg1944;32:207–211. Google Scholar
52 Patzakis MJ . The use of antibiotics in open fractures. Surg Clin North Am1975;55:1439–1444. Google Scholar
53 Parker PJ . Pre-Hospital antibiotic administration. J R Army Med Corps2008;154:5–6.PubMed Google Scholar
54 Wheatley PR . Research on Missile Wounds: The Borneao Operation Jan. 1933-June 1965. J R Army Med Corps1967;113:18–25. Google Scholar
55 Jackson DS . Sepsis in soft tissue limbs wounds in soldiers injured during the Falklands Campaign 1982. J R Army Med Corps1984;130:97–99.CrossrefPubMed Google Scholar
56 Dunkel N , PittetD, TovmirzaevaL, et al.Short duration of antibiotic prophylaxis in open fractures does not enhance risk of subsequent infection. Bone Joint J2013;95-B:831–837. Google Scholar
57 Penn-Barwell JG , FriesCA, StreetL, JefferyS. Use of topical negative pressure in british servicemen with combat wounds. Eplasty2011;11:35.PubMed Google Scholar
58 Fries CA , JefferySL, KayAR. Topical negative pressure and military wounds--a review of the evidence. Injury2010;41:708–712.CrossrefPubMed Google Scholar
59 Ubbink DT , WesterbosSJ, NelsonEA, VermeulenH. A systematic review of topical negative pressure therapy for acute and chronic wounds. Br J Surg2008;95:685–692.CrossrefPubMed Google Scholar
60 Stannard JP , VolgasDA, StewartR, McGwinG, AlonsoJE. Negative pressure wound therapy after severe open fractures: a prospective randomized study. J Orthop Trauma2009;23:552–557.CrossrefPubMed Google Scholar
61 Henry SL , OstermannPA, SeligsonD. The prophylactic use of antibiotic impregnated beads in open fractures. J Trauma1990;30:1231–1238.CrossrefPubMed Google Scholar
62 Stinner DJ , HsuJR, WenkeJC. Negative pressure wound therapy reduces the effectiveness of traditional local antibiotic depot in a large complex musculoskeletal wound animal model. J Orthop Trauma2012;26:512–518.CrossrefPubMed Google Scholar









