Abstract
Background
Symptoms of obstetric brachial plexus injury (OBPI) vary widely over the course of time and from individual to individual and can include various degrees of denervation, muscle weakness, contractures, bone deformities and functional limitations. To date, no universally accepted overall framework is available to assess the outcome of patients with OBPI. The objective of this paper is to outline the proposed process for the development of International Classification of Functioning, Disability and Health (ICF) Core Sets for patients with an OBPI.
Methods
The first step is to conduct four preparatory studies to identify ICF categories important for OBPI: a) a systematic literature review to identify outcome measures, b) a qualitative study using focus groups, c) an expert survey and d) a cross-sectional, multicentre study. A first version of ICF Core Sets will be defined at a consensus conference, which will integrate the evidence from the preparatory studies. In a second step, field-testing among patients will validate this first version of Core Sets for OBPI.
Discussion
The proposed method to develop ICF Core Sets for OBPI yields a practical tool for multiple purposes: for clinicians to systematically assess and evaluate the individual’s functioning, for researchers to design and compare studies, and for patients to get more insight into their health problems and their management.
Article focus
Developmental process of International Classification of Functioning, Disability and Health (ICF) Core Sets for patients with an obstetric brachial plexus injury (OBPI)
Key messages
A systematic literature review, a qualitative study, an expert survey and a cross-sectional study will be performed to identify ICF categories important for OBPI
The first version of ICF Core Sets will be defined at a consensus conference
Field-testing among patients will validate this first version of Core Sets for OBPI
Strengths and limitations
Universal Core Sets will give the opportunity for clinicians to systematically assess and evaluate the individual’s functioning, for researchers to design and compare studies, and for patients to get more insight into their health problems and their management
Universal Core Sets need to integrate information from different cultural backgrounds, from different countries and from multidisciplinary professionals
Anyone who wishes to actively participate is invited to contact the Leiden ICF brachial plexus team (brachialplexus@lumc.nl) to be formally associated as partners of the project
Introduction
An obstetric brachial plexus injury (OBPI) is caused by traction on the brachial plexus during delivery and can result in severe disabilities in arm function. The incidence varies between 0.4 and 2.9 per 1000 live births.1-3 The severity of the injury may vary from neuropraxia and axonotmesis to neurotmesis and avulsion of rootlets from the spinal cord. The upper part of the brachial plexus is most often affected, resulting in variable weakness of the shoulder and elbow flexion.4 Extension of the elbow and function of the hand and wrist are additionally impaired when the C7, C8, T1, medial trunk and inferior trunk are involved. An isolated injury of the lower brachial plexus (C8-T1) is rare. Depending on the severity and extent of the OBPI, the overall quality of life of patients is very much affected due to impaired upper-limb function. Symptoms of OBPI can vary widely between individuals, and clinical studies have been performed to identify the natural history and to improve treatment.5-13 Several outcome measures are used to evaluate the natural history and the effect of treatment, but there is no consensus on which outcome measures are the most appropriate.14,15
An important base for the optimal management of OBPI is the in-depth understanding, systematic consideration and sound measurement of the impact of OBPI on health and health-related domains. The International Classification of Functioning, Disability and Health (ICF) is a worldwide accepted model of the World Health Organization (WHO) providing a universal language for the description of functioning and includes the domains Body Structures, Body Functions, Activities and Participation as well as Personal and Environmental Factors (Fig. 1).16 These ICF domains, which contain together more than 1400 categories, can serve as a reference for purposes in the clinical practice.17,18 ICF Core Sets are generally agreed on lists of ICF categories and contain as few as possible but as many ICF categories as necessary to describe the typical spectrum of problems of functioning and health of patients with a specific condition. To date, ICF Core Sets have already been or are being developed for more than 20 health conditions, including neurological, musculoskeletal and cardiovascular diseases.19-25 However, ICF Core Sets for OBPI are not available so far. The objective of this paper is to outline the proposed developmental process for internationally accepted, evidence-based, reliable and valid ICF Core Sets for OBPI.

Fig. 1
Diagram showing the International Classification of Functioning, Disability and Health (ICF) model domains. ‘Health condition’ is an umbrella term for disease, disorder, injury or trauma and may also include other circumstances, such as ageing, stress, congenital anomaly or genetic predisposition. It may also include information about pathogeneses and/or aetiology. ‘Body function’ is defined as the physiological functions of body systems, including psychological functions. ‘Body structure’ refers to the anatomical parts of the body, such as organs, limbs and their components. ‘Activity’ is the execution of a task or action by an individual and represents the individual perspective of functioning. ‘Participation’ refers to the involvement of an individual in an everyday situation and represents the societal perspective of functioning. ‘Environmental factors’ make up the physical, social and attitudinal environment in which people live. ‘Personal factors’ are the particular background of an individual’s life and living situation, and comprise features that are not part of a health condition, such as gender, age, race, fitness, lifestyle, habits, and social background. They can be referred to as those factors that define the person as a unique individual.
Materials and Methods
The development of the ICF Core Sets for OBPI is a collaborative project of the Leiden University Medical Center (LUMC) and the ICF Research Branch of the Collaboration Centre of the Family of International Classifications (DIMDI) at the Ludwig-Maximilian University (Munich, Germany). Figure 2 shows the three phases in the development of the ICF Core Sets for OBPI: the preparatory phase with the international consensus conference (phase I) and the testing and implementation phase (phase II). A summary of the methods is shown in Table I. The project will be conducted in conformity with the ethical principles of Declaration of Helsinki. All appropriate study-related documents will be presented to the Medical Ethics Committees for review and approval.
Table I
Summary of the methods for the development of International Classification of Functioning, Disability and Health (ICF) Core Sets for obstetric brachial plexus injury (OBPI)
| Methods | Objectives | Specifics | |||
|---|---|---|---|---|---|
| Systematic review | A systematic review uses explicit methods to systematically search, critically appraise, and synthesise the world literature on OBPI | a) To identify outcome measures cited in published studies with the focus on patients with OBPI; b) To identify and quantify the concepts contained in these measures using the ICF as a reference | To obtain the researchers perspective, electronic databases will be search using keywords including ‘Brachial plexus neuropathies’, ‘Brachial plexus injury’, ‘Erb paralysis’, ‘Klumpke paralysis’ and ‘Obstetric brachial plexus’ | ||
| Qualitative study | Focus group technique is a qualitative method valid to explore the perspective of those who experience OBPI, i.e. the so-called patient perspective | a) To explore and understand the perspective of patients with OBPI on functioning and health; b) To identify and quantify the concepts of functioning and health important to patients with OBPI using the ICF as a reference | To obtain an international perspective, focus groups are conducted with people with OBPI in different countries | ||
| Expert survey | A survey involving experts experienced in the treatment of individuals with OBPI | a) To identify the most relevant problems of patients with OBPI from the perspective of clinical experts; b)Â To identify and quantify the concepts contained in these problems using the ICF as a reference | To obtain a worldwide perspective, experts from all over the world and from different health professions will be included | ||
| Cross-sectional study | A multicentre, cross-sectional study that involves data collection at one time point | a) To describe the prevalence of problems in functioning of patients with OBPI; b) To identify the categories that explain most of the variance of external standards | To obtain an international perspective, centres in different countries will be involved | ||
| Consensus conference | The ‘Nominal-Group Technique’ is a consensus-planning process that helps to prioritise issues during an expert’s conference | To develop ICF Core Sets for OBPI in a formal decision making and consensus process, integrating evidence gathered from preliminary studies and expert opinion | The number of groups is set at four, always including seven experts to address the main interests and to involve the different professions and WHO regions. Each group will consist of different health professionals who work together in a multi-professional and multi-disciplinary approach | ||
| Implementation and testing | Worldwide Empirical studies, including external standards, such as the Short-Form 36 | To study the content validity and feasibility of the Comprehensive and the Brief ICF Core Sets for OBPI | A network of organisations and institutions from all over the world that are interested in the implementation and testing of the pilot ICF Core Sets will be established |
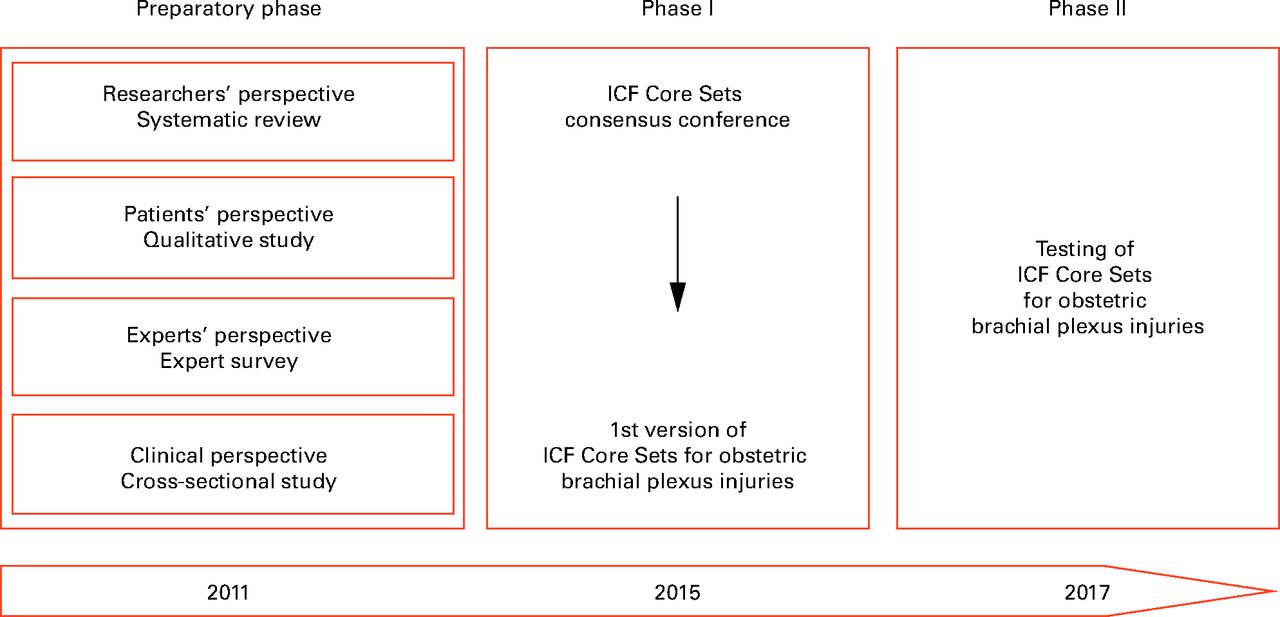
Fig. 2
Time schedule and phases of the project.
Preparatory phase
The preparatory phase aims at identifying concepts relevant to patients with OBPI from four different points of view. Therefore, this phase consists of four different preparatory studies: 1) a systematic review; 2) a qualitative study; 3) an expert survey; and 4) a cross-sectional study.
1. Systematic review
The objective of this study is to capture the researchers’ perspective, a) by identifying outcome measures cited in published studies with the focus on individuals with OBPI; and b) by identifying and quantifying the concepts contained in these measures using the ICF as a reference. Electronic databases regarding the measures used in clinical trials and in observational studies identifying concepts from the researchers’ point of view. The data collection process comprises three steps: i) the parameters used in published studies are identified; ii) the items of all retrieved parameters and their underlying concepts are specified; and iii) finally, these concepts will be linked to the categories of the ICF using standardised linking rules.26,27 Absolute and relative frequencies of the parameters and the linked ICF categories will be reported.
2. Qualitative study
The objectives of this study are: a)Â to explore and understand the perspective of patients with OBPI on functioning and health; and b) to identify and quantify the concepts of functioning and health important to patients with OBPI using the ICF as a reference. It is important to include the patients’ perspective because personal values for outcomes vary between and within patients. In order to identify the prototypical spectrum of problems of patients with OBPI, small groups with ≤ eight individuals between the ages of eight and 18 years are interviewed. These focus groups are likely to generate more concepts than individual interviews, as the interaction and group process can enrich the information generated within a group of patients.28,29 A topic guide based on the components Body Structures, Body Functions, Activities and Participation, Environmental Factors and Personal Factors of the bio-psycho-social model will be applied. All interviews will be digitally recorded, transcribed verbatim and evaluated again by two independent researchers. Participants will be included in the study until saturation is reached, which is defined as the point during data collection when the linking of the retrieved concepts to the second level of the ICF classification is < Â 5% of the number of second-level ICF category nominated so far. The frequencies of the parameters and the linked ICF categories from the focus groups will be reported.
3. Expert survey
An internet-based expert survey will be conducted with the aims of: a) collecting the health professionals’ perspective on relevant problems of patients with OBPI; and b) identifying and quantifying the concepts contained in these problems using the ICF as a reference. As the ICF was developed to facilitate communication between different groups of people and to be used globally, the aim is to include experts from all six WHO regions: Eastern Mediterranean, South-East Asia, Western Pacific, The Americas, Africa and Europe. In order to maximise the number and range of ideas and opinions, the aim is to include experts from different health professions including neurosurgeons, orthopaedic surgeons, plastic surgeons, rehabilitation physicians, neonatologists, neurologists, pediatricians, physical therapists, occupational therapists, nurses and social workers. In order to contribute to the survey, the health professionals must have a minimum of two years’ experience in the treatment of OBPI and must be fluent in English. In the expert survey a five-item open-ended questionnaire is used, which requests that experts list all body structures, functions, activities and participation aspects in which patients with OBPI encounter problems, as well as all contextual factors that have a facilitation and/or hindering influence on the problems of patients with OBPI. The answers of the health professionals are linked to the ICF categories and the frequency of ICF categories are reported.
4. Cross-sectional study
In order to obtain the clinical perspective, a multi-centre cross-sectional study will be conducted. The aims of this study are: a) to describe functioning and health of patients with OBPI; b) to identify the most common problems using the ICF; and c) to identify the categories that explain most of the variance in currently used outcome measures. This multicentre study will be conducted in the different WHO regions and patients with OBPI who are literate in the primary language of the study site will be consecutively included in the study. Data will be collected with a case record form (CRF), which is made up of two parts. The first part is an ICF checklist, which comprises the 31 first-level categories and a selection of 123 from the 362 second-level categories of the whole ICF classification system. It provides a relatively simple questionnaire, which can be filled out by the physician or other health professional. The ICF checklist makes it possible to classify the most important ICF categories in clinical practice. The second part includes the EuroQol (EQ-5D),30 five questions of the WHO Quality of Life Questionnaires (WHOQoL)31 to assess the subjective appraisal of health and well-being, the Short-Form (SF)-36 health survey,32 the Disability of Arm, Shoulder and Hand Questionnaire (DASH),33 and the self-administered Co-morbidity Questionnaire (SCQ).34
Furthermore, sociodemographic variables will be collected. For the ICF components body functions, body structures, activities and participation, absolute frequencies and relative frequencies of impairment will be reported along with their 95% confidence intervals. For environmental factors, absolute frequencies and relative frequencies of persons who regarded a specific category as either barrier or facilitator are reported.
Consensus conference
The results of the preparatory phase will be presented at an international consensus conference. At this conference, experts in the field of OBPI will work actively together to deal with the complex problem of arriving at an international consensus on the most adequate ICF categories to be included on the ICF Core Sets for OBPI. The “Nominal-Group Technique” will be applied to regulate the group dynamic and the teamwork during the conference.35 Since the results of the preliminary studies are all expressed in ICF language, they can be compiled in tables that contain (for each category addressed) the percentage with which the categories were named in the preparatory studies. First, the experts will be asked to select ICF categories for the comprehensive ICF Core Sets, which is a list of ICF categories long enough to describe the prototypical spectrum of functioning and health of patients with OBPI. Secondly, the experts will be asked to select ICF categories from the comprehensive ICF Core Sets lists that are sufficient to describe the prototypical spectrum of functioning of patients with OBPI, with this list being short enough for feasible use in clinical practice. This process will lead to a brief list of ICF Core Sets.
Validation phase
The next step is to test the validity and feasibility of the proposed brief and comprehensive ICF Core Sets for patients with OBPI. This will be conducted in a multicentre cohort study at a network of cooperating organisations. The objectives are to analyse the frequency of patients’ problems in different subsets, including nationality, socioeconomic factors, age, gender, the severity of OBPI and comorbidities. The results will be used to identify the categories that explain most of the variance of external standards, as well as to analyse to what extent the entire severity spectrum of problems in functioning reported by patients with OBPI is represented in the comprehensive ICF Core Sets.
Discussion
In this paper we have described the proposed process to develop ICF Core Sets for OBPI. The ICF has been proposed by the WHO to comprehensively describe limitations in functioning and relevant environmental factors.16 The ICF offers a framework and classification for the patient and clinical perspective both at the individual and the population level. It integrates long known concepts and provides a universal and standardised language. ICF Core Sets are necessary to make the ICF useful to describe functional limitations and disabilities of patients with OBPI.
Currently, ICF Core Sets have been, or are being developed for more than 20 health conditions, including neurological traumas and musculoskeletal diseases such as traumatic brain injuries, spinal cord injuries, osteoarthritis and low back pain.19-25 ICF Core Sets may well serve as the basis for multi-professional patient assessment, goal setting, intervention management and evaluation.36 For a correct interpretation of the patient’s problems, it is important to first describe the concerns of the patient and/or parents in their own words. Physicians can use the ICF Core Sets to describe and classify patients’ symptoms and findings of clinical examinations. Professionals could describe at least all categories from a brief Core Set and use the comprehensive Core Set as a source of additional relevant items. Using the ICF Core Sets supports multidisciplinary and comprehensive assessment of functioning. It helps all team members to consider every potentially relevant aspect of functioning of a patient. The use of ICF Core Sets can assist health care professionals in explaining the necessity of a certain procedure for a patient and for their parents, thereby creating more insight into the health problems and treatment. It is by no means the aim of the ICF to replace validated existing instruments. In contrast, it is likely that they will have an essential role to measure particular parts of the ICF. Most measurement instruments do however cover only a limited number of ICF categories.
Next to the clinical application, ICF Core Sets will be used by researchers and healthcare providers in many ways. ICF Core Sets make it possible to classify and describe an individual’s functioning using widely accepted terminology, which facilitates the comparability of international studies. It can also be used to rate the content validity of health-status measures and to select appropriate instruments for the specific needs for patients with OBPI. In the future, ICF and the ICF Core Sets may become the new basis not only for the further development of such measures, but also for the creation of an item list with parameters relevant to patients with OBPI. Furthermore, ICF facilitates linking medical data across different conditions or interventions for efficient, transparent and cost-effective health care. Other benefits could also rise from compiling a functionality assessment for OBPI from a common set of indicators (a common bio-psycho-social framework) used for all health conditions. For example, a common language would facilitate communication among health professionals and also between health professionals and patients with OBPI, as well as their family or caregivers. In addition, because the ICF is aetiologically neutral, it is easily possible to combine the ICF Core Sets for OBPI with other ICF Core Sets in a non-redundant and useful way when describing and classifying functioning and disability of persons with more than one condition. Worldwide comparisons will also be possible for any health condition, not only for OBPI. This will enable policy makers to make informed decisions with regard to such issues as resource allocation, new legislation and modification of care provision policies.
A few limitations have to be resolved during the developmental process of ICF Core Sets. The assessment of functioning and quality of life data is highly sensitive to ethno-cultural differences.37,38 In order to come up with a first version of ICF Core Sets for OBPI that integrates information from different cultural backgrounds, the preparatory studies will gather data on patients being treated at centres from different countries and from professionals in an international expert survey. Another limitation could be that the preparatory studies collect information only from published papers in English and English-speaking participants. This is done to ease comparability of results from different countries, but on the other hand will contain a structural bias for countries in which English is not the native language. The extent and relevance of this issue will be addressed in the validation phase following the consensus conference. An issue to be addressed is the possible need for stratification by a number of variables including the extent of brachial plexus injury and the age of the growing children. The preliminary studies will provide the necessary information to guide these decisions. It is important to realise that the ICF Core Sets Consensus Conference will provide only a first, best possible version of ICF Core Sets for OBPI, which will then need to be tested worldwide.
In conclusion, this is a big step forward in the development of an internationally acceptable and standardised tool for assessing disability in OBPI. Establishing standardised ICF Core Sets will be useful for research, clinical practice and teaching. The ICF Core Sets will then also form the basis for the development of assessment instruments to quantify the severity of OBPI to measure change over time and the effectiveness of interventions. They could also serve as the basis for setting clinical significance thresholds in diagnostic assessment systems. Finally, it is our hope that such research will lead to interventions and accommodations that improve the restoration and maintenance of functioning and minimise disability among patients with OBPI throughout the world.
Invitation for participation
The development of the ICF core sets is an inclusive and open process. Therefore, the authors of this article encourage clinical experts and patients to actively participate in the process. Anyone who wishes to actively participate is invited to contact the Leiden ICF brachial plexus team (brachialplexus@lumc.nl). Individuals, institutions and associations can be formally associated as partners of the project.
Members of the ICF Brachial Plexus Advisory Board include: J. H. Arendzen (Leiden University Medical Center, the Netherlands), J. Bahm (Franziskushospital, Germany), A. Belzberg (Johns Hopkins Hospital, Maryland), N. C. Budhiparama (Medistra Hospital, Indonesia), H. M. Clarke (Hospital for Sick Children, Canada), J. A. I. Grossman (Miami Children’s Hospital, Florida), C. O. Heise (University of Sao Paolo Medical School, Brazil), H. Kawabata (Osaka Medical Center and Research Institute for Maternal and Child, Japan), S. H. Kozin (Shriners Hospitals for Children, United States), J. Nagels (Leiden University Medical Center, the Netherlands), W. Pondaag (Leiden University Medical Center, the Netherlands), A. E. Price (New York University Tisch Hospital, New York), M. G. Siqueira (University of Sao Paolo Medical School, Brazil), P. M. Waters (Harvard Medical School, Massachusetts), M. S. van Wijlen-Hempel (Dubai Bone and Joint Center, United Arab Emirates), L. Y. S. Yang (University of Michigan Health System, Michigan).
1 Evans-Jones G , KaySP, WeindlingAM, et al.Congenital brachial palsy: incidence, causes, and outcome in the United Kingdom and Republic of Ireland. Arch Dis Child Fetal Neonatal Ed2003;88:F185–F189.CrossrefPubMed Google Scholar
2 Dawodu A , Sankaran-KuttyM, RajanTV. Risk factors and prognosis for brachial plexus injury and clavicular fracture in neonates: a prospective analysis from the United Arab Emirates. Ann Trop Paediatr1997;17:195–200.CrossrefPubMed Google Scholar
3 Bager B . Perinatally acquired brachial plexus palsy: a persisting challenge. Acta Paediatr1997;86:1214–1219. Google Scholar
4 Waters PM . Update on management of pediatric brachial plexus palsy. J Pediatr Orthop B2005;14:233–244.CrossrefPubMed Google Scholar
5 Hoeksma AF , ter SteegAM, DijkstraP, et al.Shoulder contracture and osseous deformity in obstetrical brachial plexus injuries. J Bone Joint Surg [Am]2003;85-A:316–322.CrossrefPubMed Google Scholar
6 van Gelein Vitringa VM , van KootenEO, JaspersRT, et al.An MRI study on the relations between muscle atrophy, shoulder function and glenohumeral deformity in shoulders of children with obstetric brachial plexus injury. J Brachial Plex Peripher Nerve Inj2009;4:9.CrossrefPubMed Google Scholar
7 Malessy MJ , PondaagW. Obstetric brachial plexus injuries. Neurosurg Clin N Am2009;20:1–14.CrossrefPubMed Google Scholar
8 Malessy MJ , de RuiterGC, de BoerKS, ThomeerRT. Evaluation of suprascapular nerve neurotization after nerve graft or transfer in the treatment of brachial plexus traction lesions. J Neurosurg2004;101:377–389.CrossrefPubMed Google Scholar
9 Pondaag W , MalessyMJ. Recovery of hand function following nerve grafting and transfer in obstetric brachial plexus lesions. J Neurosurg2006;105(Suppl):33–40.CrossrefPubMed Google Scholar
10 Pondaag W , MalessyMJ, van DijkJG, ThomeerRT. Natural history of obstetric brachial plexus palsy: a systematic review. Dev Med Child Neurol2004;46:138–144.CrossrefPubMed Google Scholar
11 Pondaag W , de BoerR, van Wijlen-HempelMS, Hofstede-BuitenhuisSM, MalessyMJ. External rotation as a result of suprascapular nerve neurotization in obstetric brachial plexus lesions. Neurosurgery2005;57:530–537.CrossrefPubMed Google Scholar
12 Pondaag W , van der VekenLP, van SomerenPJ, van DijkJG, MalessyMJ. Intraoperative nerve action and compound motor action potential recordings in patients with obstetric brachial plexus lesions. J Neurosurg2008;109:946–954.CrossrefPubMed Google Scholar
13 Hoeksma AF , ter SteegAM, NelissenRG, et al.Neurological recovery in obstetric brachial plexus injuries: an historical cohort study. Dev Med Child Neurol2004;46:76–83.CrossrefPubMed Google Scholar
14 Bae DS , WatersPM, ZurakowskiD. Correlation of pediatric outcomes data collection instrument with measures of active movement in children with brachial plexus birth palsy. J Pediatr Orthop2008;28:584–592.CrossrefPubMed Google Scholar
15 Al-Qattan MM . Assessment of the motor power in older children with obstetric brachial plexus palsy. J Hand Surg Br2003;28:46–49.CrossrefPubMed Google Scholar
16 World Health Organization. International Classification of Functioning, Disability and Health (ICF). http://www.who.int/classifications/icf/en/ (date last accessed 22 May 2013). Google Scholar
17 Stucki G , EwertT, CiezaA. Value and application of the ICF in rehabilitation medicine. Disabil Rehabil2002;24:932–938.CrossrefPubMed Google Scholar
18 Stucki G , CiezaA, EwertT, KostanjsekN, ChatterjiS, UstunTB. Application of the International Classification of Functioning, Disability and Health (ICF) in clinical practice. Disabil Rehabil2002;24:281–282.CrossrefPubMed Google Scholar
19 Cieza A , EwertT, UstünTB, et al.Development of ICF Core Sets for patients with chronic conditions. J Rehabil Med2004;44(Suppl):9–11.CrossrefPubMed Google Scholar
20 Kohler F , CiezaA, StuckiG, et al.Developing Core Sets for persons following amputation based on the International Classification of Functioning, Disability and Health as a way to specify functioning. Prosthet Orthot Int2009;33:117–129.CrossrefPubMed Google Scholar
21 Grill E , ZochlingJ, StuckiG, et al.International Classification of Functioning, Disability and Health (ICF) Core Set for patients with acute arthritis. Clin Exp Rheumatol2007;25:252–258.PubMed Google Scholar
22 Stucki A , CiezaA, MichelF, et al.Developing ICF Core Sets for persons with sleep disorders based on the International Classification of Functioning, Disability and Health. Sleep Med2008;9:191–198.CrossrefPubMed Google Scholar
23 Vieta E , CiezaA, StuckiG, et al.Developing core sets for persons with bipolar disorder based on the International Classification of Functioning, Disability and Health. Bipolar Disord2007;9:16–24.CrossrefPubMed Google Scholar
24 Bernabeu M , LaxeS, LopezR, et al.Developing core sets for persons with traumatic brain injury based on the international classification of functioning, disability, and health. Neurorehabil Neural Repair2009;23:464–467.CrossrefPubMed Google Scholar
25 Grill E , EwertT, ChatterjiS, KostanjsekN, StuckiG. ICF Core Sets development for the acute hospital and early post-acute rehabilitation facilities. Disabil Rehabil2005;27:361–366.CrossrefPubMed Google Scholar
26 Cieza A , BrockowT, EwertT, et al.Linking health-status measurements to the international classification of functioning, disability and health. J Rehabil Med2002;34:205–210.CrossrefPubMed Google Scholar
27 Cieza A , GeyhS, ChatterjiS, et al.ICF linking rules: an update based on lessons learned. J Rehabil Med2005;37:212–218.CrossrefPubMed Google Scholar
28 Thomas L , MacMillanJ, McCollE, HaleC, BondS. Comparison of focus group and individual interview methodology in examining patient satisfaction with nursing care. Social Sciences in Health1995;1:206–220. Google Scholar
29 Coenen M ,  StammTA,  StuckiG,  CiezaA. Individual interviews and focus groups in patients with rheumatoid arthritis: a comparison of two qualitative methods. Qual Life Res  2012;21:359–370.CrossrefPubMed Google Scholar
30 The EuroQol Group. EuroQol: a new facility for the measurement of health-related quality of life Health Policy1990;16:199–208. Google Scholar
31 No authors listed. The World Health Organization Quality of Life Assessment (WHOQOL): development and general psychometric properties Soc Sci Med1998;46:1569–1585. Google Scholar
32 Ware JE , SherbourneCD. The MOS 36-item short-form health survey (SF-36): I: conceptual framework and item selection. Med Care1992;30:473–483. Google Scholar
33 Hudak PL , AmadioPC, BombardierC. Development of an upper extremity outcome measure: the DASH (disabilities of the arm, shoulder and hand) [corrected]: The Upper Extremity Collaborative Group (UECG). Am J Ind Med1996;29:602–608. Google Scholar
34 Sangha O , StuckiG, LiangMH, FosselAH, KatzJN. The Self-Administered Comorbidity Questionnaire: a new method to assess comorbidity for clinical and health services research. Arthritis Rheum2003;49:156–163.CrossrefPubMed Google Scholar
35 Van de Ven AH , DelbecqAL. The nominal group as a research instrument for exploratory health studies. Am J Public Health1972;62:337–342.CrossrefPubMed Google Scholar
36 Rauch A , CiezaA, StuckiG. How to apply the International Classification of Functioning, Disability and Health (ICF) for rehabilitation management in clinical practice. Eur J Phys Rehabil Med2008;44:329–342.PubMed Google Scholar
37 Pasick RJ , StewartSL, BirdJA, D’OnofrioCN. Quality of data in multiethnic health surveys. Public Health Rep2001;116(Suppl 1):223–243.CrossrefPubMed Google Scholar
38 Hahn EA , HolznerB, KemmlerG, et al.Cross-cultural evaluation of health status using item response theory: FACT-B comparisons between Austrian and US patients with breast cancer. Eval Health Prof2005;28:233–259. Google Scholar
Funding statement:
None declared
Author contributions:
B. J. Duijnisveld: Study protocol development, First manuscript draft
Ç. Saraç: Formation of the ICF Brachial Plexus Advisory Board, Critical revision of the manuscript
M. J. A. Malessy: Formation of the ICF Brachial Plexus Advisory Board, Critical revision of the manuscript
The ICF Brachial Plexus Advisory Board: Critical revision of the manuscript
T. P. M. Vliet Vlieland: Study protocol development, Formation of the ICF Brachial Plexus Advisory Board, First manuscript draft
R. G. H. H. Nelissen: Formation of the ICF Brachial Plexus Advisory Board, Critical revision of the manuscript
ICMJE Conflict of Interest:
None declared
©2013 The British Editorial Society of Bone & Joint Surgery. This is an open-access article distributed under the terms of the Creative Commons Attributions licence, which permits unrestricted use, distribution, and reproduction in any medium, but not for commercial gain, provided the original author and source are credited.









