Abstract
Objective
This study compared the primary stability of two commercially available acetabular components from the same manufacturer, which differ only in geometry; a hemispherical and a peripherally enhanced design (peripheral self-locking (PSL)). The objective was to determine whether altered geometry resulted in better primary stability.
Methods
Acetabular components were seated with 0.8 mm to 2 mm interference fits in reamed polyethylene bone substrate of two different densities (0.22 g/cm3 and 0.45 g/cm3). The primary stability of each component design was investigated by measuring the peak failure load during uniaxial pull-out and tangential lever-out tests.
Results
There was no statistically significant difference in seating force (p = 0.104) or primary stability (pull-out p = 0.171, lever-out p = 0.087) of the two components in the low-density substrate. Similarly, in the high-density substrate, there was no statistically significant difference in the peak pull-out force (p = 0.154) or lever-out moment (p = 0.574) between the designs. However, the PSL component required a significantly higher seating force than the hemispherical cup in the high-density bone analogue (p = 0.006).
Conclusions
Higher seating forces associated with the PSL design may result in inadequate seating and increased risk of component malpositioning or acetabular fracture in the intra-operative setting in high-density bone stock. Our results, if translated clinically, suggest that a purely hemispherical geometry may have an advantage over a peripherally enhanced geometry in high density bone stock.
Cite this article: Bone Joint Res 2013;2:264–9.
Article focus
To compare the primary stability of two commercially available acetabular components produced by the same manufacturer, differing only in geometry
It was hypothesised that there would be no differences in primary stability achieved by the two designs in a controlled bench-top model
Key messages
Although the primary stability achieved by both cups was found to be similar, the force required to seat the PSL design in high density substrate was 25% higher than that of the purely hemispherical component
Clinically, higher seating forces are harder to generate and increase the risk of inadequate component seating, malpositioning and acetabular fractures, which may compromise the outcome of the operation
If our results translate clinically, the hemispherical geometry is superior in higher density bone as it achieves the same initial stability but requires a lower insertional force
Strengths and limitations
Strengths: comparison was made between components that only varied in geometry using a controlled reproducible test set-up
Limitations: the use of a dry synthetic bone substrate rather than real bone and not testing torsion stability or combined mechanisms
Introduction
Uncemented and hybrid total hip replacements (THRs) have become increasingly popular over the last decade. Data from the National Joint Registry shows that the use of uncemented THRs overtook cemented arthroplasties in England and Wales for the first time in 2009.1 In 2011, 32.6% of primary hip replacements were cemented, 44.7% uncemented and 17.4% hybrids.1
Uncemented components require excellent primary stability as micromotion at the bone–prosthesis interface inhibits osseointegration and impairs long-term component stability.2-5 Initial primary stability is achieved by the principle of press-fit, where an oversized component is inserted into an undersized reamed cavity. The most common geometric design used to achieve the press-fit effect has been the hemispherical component. However, clinical concerns have arisen over the generation of excessive peri-prosthetic strains, which may be associated with subsequent fractures, and polar gaps, which may serve as route for wear particles or obviate bony ingrowth.6-9 Consequently, other acetabular geometries have been introduced. One of the most widely available is the peripherally enhanced design, which in essence comprises hemispherical geometry with a wider diameter at the peripheral edge. In contrast to the purely hemispherical geometry, the peripherally enhanced design is typically inserted into a cavity reamed to the same diameter as the component’s nominal dimension (‘line-to-line’), meaning that the overall press-fit is provided entirely by the enhanced periphery.
Although several studies have evaluated the primary stability of different acetabular components, these studies have typically compared designs that vary not only in geometry, but also in material properties, wall thickness, and surface finish.10-15 Consequently, any differences in primary stability seen in these studies cannot be attributed solely to differences in the geometry of the components.
The aim of the current study was to compare the primary stability of two commercially-available acetabular components produced by the same manufacturer that differ only in their geometry. It was hypothesised that there would be no differences in the primary stability achieved by the two geometries in a controlled bench-top model.
Materials and Methods
Acetabular components
We evaluated hemispherical and peripheral self-locking (PSL) acetabular component designs of the Trident hip system (Stryker, Newbury, United Kingdom). The PSL component was identical to the hemispherical design, except for a 1.8 mm enhanced peripheral structure. Both components had a core diameter of 52 mm, were manufactured from the same titanium alloy and had the same hydroxyapatite-treated surface. One of each design was used to test each density (0.22 g/cm3 and 0.45 g/cm3) and each mode of failure (pull-out and lever-out), necessitating a total of four of each design.
Synthetic bone substrate
Polyethylene foam (Pedilin Foam; Otto Bock, Bock, Austria) was used as a synthetic bone substrate. Synthetic bone substrate has been shown to lower interspecimen variability compared with post-mortem material, while providing a similar compressive modulus to that of cadaveric bone.10,16,17 Cylindrical blocks (radius 51 mm and height 50 mm) were prepared in densities of 0.22 g/cm3 and 0.45 g/cm3 in an effort to model low- and high-density bone stock, respectively.10 The mean compressive modulus for low- and high-density substrate blocks (77 MPa (sd 12)) and 211 MPa (sd 8), respectively) encompassed the range of values reported for cancellous bone stock (approximately 50 MPa to 450 MPa).18
Test blocks were subsequently mounted on a lathe and reamed 0.5 mm beyond the equator of the acetabular reamer to a depth of 26.5 mm. A standard depth gauge (resolution 0.1 mm) was used to verify the depth of the cavity. Reaming parameters for each acetabular geometry in low and high density substrate are shown in Table I. Consistent with previous studies,10,19 lower press-fit values were used to ensure full seating of the acetabular components in the high density substrate. Our own pilot work also demonstrated that forces in excess of 10 kN were required to insert the PSL component in the high-density substrate when press-fits of 2 mm and 1.8 mm were initially used.20 Such magnitude of force was above the maximum rated capacity of our materials testing machine and would be challenging and potentially damaging to achieve manually in the intra-operative setting. Therefore the chosen press-fit values were modified as described above.
Table I
Reaming parameters used for hemispherical and peripheral self-locking (PSL) acetabular component designs in low- (0.22 g/cm3) and high-density (0.45 g/cm3) substrate
| Hemispherical (52 mm) | PSL (52 mm) | |||
|---|---|---|---|---|
| Low density (0.22 g/cm3) | ||||
| Reaming diameter (mm) | 50 | 52 | ||
| Nominal interference fit (mm) | 2 | 1.8 | ||
| Reaming depth (mm) | 26.5 | 26.5 | ||
| High density (0.45 g/cm3) | ||||
| Reaming diameter (mm) | 51 | 53 | ||
| Nominal interference fit (mm) | 1 | 0.8 | ||
| Reaming depth (mm) | 26.5 | 26.5 |
Seating
Acetabular components were inserted into the reamed test blocks using a custom introducing assembly, which provided a uniformly distributed load to each acetabular component through the original manufacturer’s component-to-inserter locking mechanism (Fig. 1). A uniaxial materials testing machine (Instron 5800R, Instron, High Wycombe, United Kingdom), fitted with a 10 kN load cell (accuracy, 0.1% full scale), was used to seat the two acetabular designs at a linear rate of 2.5 mm/s. Acetabular components were considered to be seated when: 1) the displacement of the component was equivalent to the measured depth of the reamed cavity; and 2) the entire hydroxyapatite-coated area of the component was engaged within the bone substrate, such that only the inner sleeve of the acetabular component was visible.
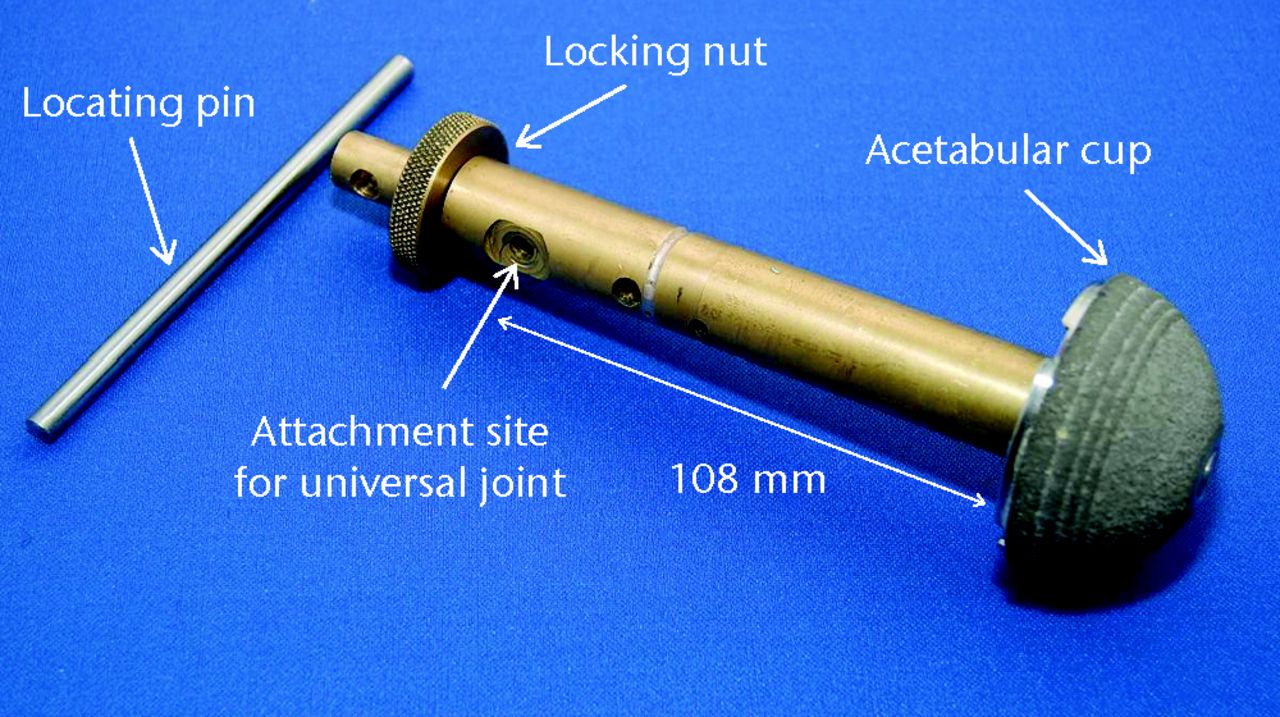
Fig. 1
Photograph showing the peripheral self-locking (PSL) Trident acetabular component (Stryker, Newbury, United Kingdom) mounted on the brass rod connecting assembly used to secure the component to the load cell.
Primary stability
Primary stability of the two geometries was evaluated using two modes of failure: direct distraction (pull-out tests) and sagittal/coronal rotation (lever-out tests). Ten repetitions were performed for each mode of failure, in both high- and low-density bone substrate. One acetabular component was used for each set of ten tests. Therefore a total of 80 tests of primary stability were conducted, 40 each for the hemispherical and PSL designs, using four hemispherical and four PSL components.
Pull-out test
Following seating, the uniaxial materials testing machine was used to distract acetabular components directly from the reamed cavity at a rate of 2 mm/s.
Lever-out test
Following seating, the introducing assembly was disconnected from the load cell and reconnected to a universal attachment via a steel cable and adjustable pulley system. The effective moment arm for the lever-out test was defined as the measured distance from the universal joint to the substrate surface (Fig. 2). Components were subsequently distracted at a rate of 10 mm/s.10

Fig. 2
Diagrammatic illustration of the moment arm determined for ‘lever-out’ testing. A steel cable, low friction pulley and universal connection are used to apply a lever-out moment to the introducing assembly. The moment arm was defined by the distance of the universal joint from the surface of the synthetic block.
Data reduction and statistical analysis
Force and displacement data were sampled at 100 Hz during seating and failure testing. Seating force was defined as the peak force generated during component insertion, while pull-out force was defined as the maximum force during direct distraction. The peak lever-out moment was calculated by multiplying the peak lever-out force by the respective moment arm.
The SPSS statistical package v16.0 for Windows (SPSS Inc., Chicago, Illinois) was used for all statistical procedures. Underlying assumptions of normality and equality of variance were assessed using the Kolmogorov–Smirnoff and Levene’s tests, respectively. As press-fit parameters differed between high- and low-density bone substrate, separate analyses were conducted for each. Between-component differences in peak seating force, pull-out force and lever-out moment for each test were evaluated using independent sample t-tests. An alpha level of 0.05 was used for all tests of significance (significance at p < 0.05).
Results
Seating forces
There was no statistically significant difference in the mean seating force between the hemispherical and PSL components in the low-density substrate (4078 N (2384 to 6743) versus 4649 N (3166 to 6850); p = 0.104). In high density substrate, however, the mean seating force for the PSL geometry was 25% higher compared with the hemispherical design (7858 N (4752 to 13 756) versus 6264 N (3897 to 9200)) (Fig. 3). This difference was statistically significant (p = 0.006).
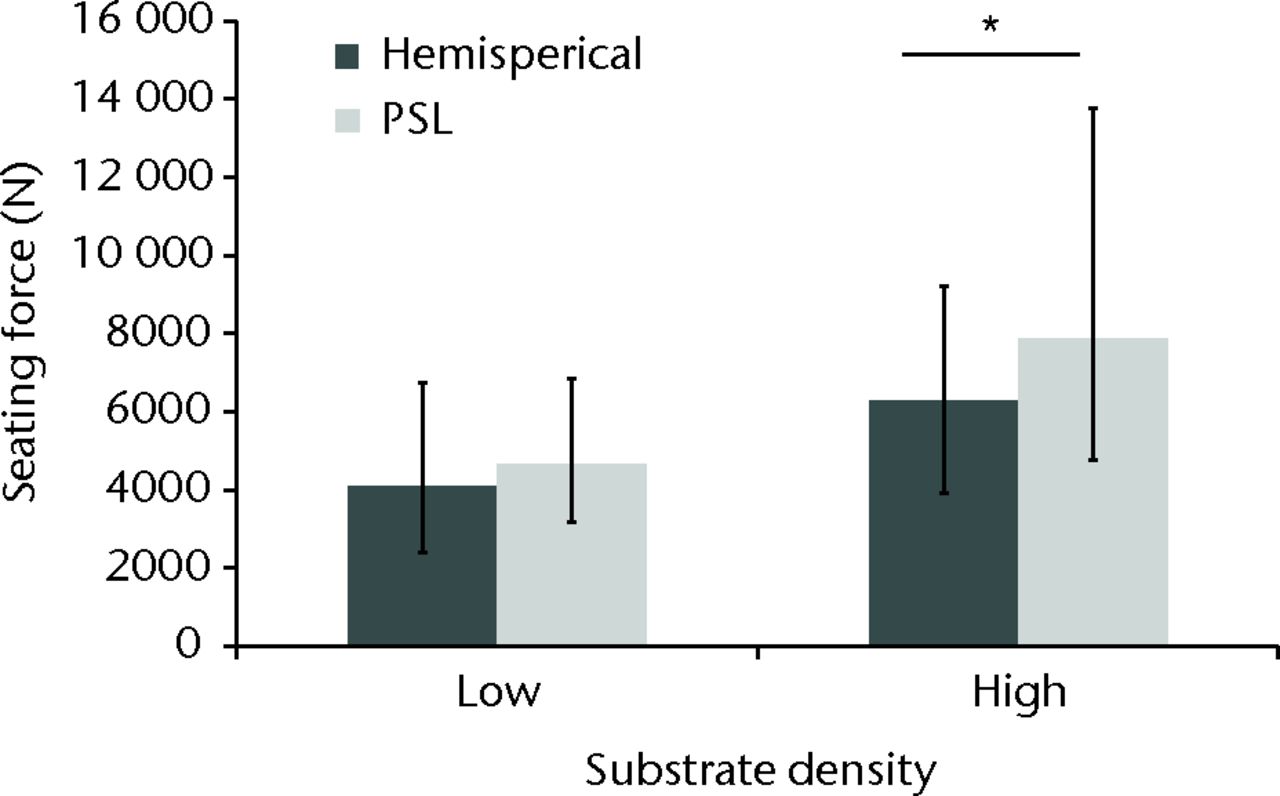
Fig. 3
Seating force for hemispherical and peripheral self-locking (PSL) implant designs in low- (0.22 g/cm3) and high-density (0.45 g/cm3) substrate. The error bars denote the range of values (* p = 0.006).
Primary stability
The primary stability of the two designs is shown in Table II. There were no statistically significant differences in mean pull-out force or lever-out moment between the two geometries in either low- or high-density substrate (all p ≥ 0.087).
Table II
Primary stability of hemispherical and peripheral self-locking (PSL) acetabular component designs in low- (0.22 g/cm3) and high-density (0.45 g/cm3) substrate
| Hemispherical | PSL | p-value* | ||||
|---|---|---|---|---|---|---|
| Low density (0.22 g/cm3) | ||||||
| Mean peak pull-out force (N) (range) | 668 (579 to 820) | 707 (626 to 814) | 0.171 | |||
| Mean peak lever-out moment (Nm) (range) | 14.4 (9.7 to 17.5) | 16.2 (12.2 to 18.3) | 0.087 | |||
| High density (0.45 g/cm3) | ||||||
| Mean peak pull-out force (N) (range) | 1553 (1039 to 2195) | 1424 (962 to 1924) | 0.154 | |||
| Mean peak lever-out moment (Nm) (range) | 37.2 (29.1 to 43.5) | 39.8 (21.7 to 47.3) | 0.574 | |||
-
* independent samples t-test
Discussion
The primary stability of uncemented acetabular components is paramount for biological fixation. While several factors have been suggested to influence this initial stability,11,21 this is the first study, to our knowledge, to directly compare the primary stability of two commercially available acetabular component designs that differ only in geometry. Consistent with our initial hypothesis, we observed that the geometry of the acetabular component had minimal effect on primary stability during pull-out and lever-out testing in both high- and low-density substrates, provided that satisfactory seating had been achieved. However, contrary to our original hypothesis, we also observed that the peripherally enhanced geometry of the PSL component required higher seating forces – approximately 25% higher than those required by the hemispherical design. Thus, in our controlled bench-top model, acetabular geometry appears to have a profound effect on the force required to seat components. This is similar to the senior author’s (MS) intra-operative observations.
From a surgical point of view, it is important that acetabular components can be inserted accurately and without the use of excessive force. The higher force required to seat the PSL component in high-density bone may be difficult to achieve, may lead to incomplete seating and/or and component malpositioning and also may increase the risk of peri-operative fractures. This finding is of particular importance, given that many orthopaedic surgeons prefer to use uncemented arthroplasty in younger patients who are more likely to have higher bone density. Unsatisfactory seating of the acetabular component leads to incomplete engagement and therefore small residual compressive forces that may result in excessive micromotion and adversely affect primary stability.2,4,5 Malpositioning, including lateralisation of the hip’s centre of rotation due to incomplete seating, can lead to impingement and decreased range of movement,22-24 a higher risk of dislocation,25-27 and increased rates of wear.28 Clinical data, however, are paramount. We have highlighted that there are potential difficulties in seating the PSL component in dense bone. This has been observed clinically, with Nunag et al29 reporting 20 of a series of 30 Trident PSL acetabular components (Stryker) having incomplete seating. However, this series showed good clinical outcomes at five years,29 and the Trident acetabular implant has good medium-term registry data,1 although these data do not distinguish between the two variants of the cup.
A limitation of our study is that we quantified the primary stability of the two acetabular geometries using discrete pull-out and lever-out mechanisms in a dry synthetic bone substrate. Although the synthetic material served as a representative model for evaluating the effects of varying bone quality, we recognise that the substrate is unlikely to have the same visco-elastic response as bone, despite possessing a similar compressive modulus. The use of a synthetic substrate, however, gives a consistent set of material properties for all testing, allowing a more accurate comparison of the primary stability of the different component geometries and it has been widely used in previous studies.10,13,14 While we also recognise that torsion stability or combined mechanisms may arguably be more clinically relevant predictors of stability,10,13,30,31 the magnitude of pull-out forces in our series (between 0.7 kN and 1.6 kN) is comparable to the range of failure values reported in the literature (0.7 kN to 2 kN).13,32 Similarly, the magnitude of the lever-out moments resulting in failure in our current study (between 14 Nm and 40 Nm) is within the wide range reported in the literature (5 Nm to 50 Nm).10,12-14,32,33 Due to the availability of implants, each acetabular component was re-used ten times, with a new component for each density of substrate and mode of failure. It was possible that repeated use could cause deformation of the components and therefore changes in the subsequent seating forces and stability. However, we observed no obvious deformation and sequential analysis of the results did not show any trends (either increasing or decreasing) with regards to seating force, pull-out force or lever-out moment.
The exact force needed to seat a component in an appropriately reamed acetabular cavity in vivo is currently unknown. Therefore, the seating forces generated in this study can only be compared with corresponding values estimated from other in vitro studies. Of the few studies that have quantified seating forces with similar press-fit values (0 mm to 2 mm) and substrate densities (0.2 g/cm3 and 0.5 g/cm3), four have reported a range between 1.5 kN and 5 kN with a variety of uncemented implants that included purely hemispherical as well as peripherally enhanced designs.10,11,15,30 The range of seating forces generated in the current study (between 4 kN and 8 kN) is somewhat higher. It should be noted however that while the cited studies have employed similar substrates (polyethylene foam and polyurethane foam) and comparable press-fits, certain implant designs were reported to be incompletely seated.10 In comparison, satisfactory seating was achieved in all the trials of this study and may, in part, explain the relatively high forces required to seat components. It should be also noted that although our method of seating implants does not replicate the method of insertion used in surgery (in which a series of impulsive blows are applied) it is a controlled method of insertion that allows for accurate measurement of the forces involved; it therefore enabled us to compare this important parameter between the cup designs in a standardised fashion.
Conclusions
Although the primary stability achieved by both designs was found to be similar, as assessed by pull-out and lever-out failure, the force required to seat the PSL design in high density substrate was 25% higher than that of the purely hemispherical implant. Clinically, higher seating forces are harder to generate and increase the risk of inadequate component seating, malpositioning and acetabular fractures, which may compromise the outcome of the operation. If our results translate clinically, the hemispherical geometry is superior in higher density bone as it achieves the same initial stability but requires a lower insertional force.
1 No authors listed. National Joint Registry for England and Wales. 9th Annual Report 2011. http://www.njrcentre.org.uk (date last accessed 4 October 2012). Google Scholar
2 Cameron HU , PilliarRM, MacNabJ. The effect of movement on the bonding of porous metal to bone. J Biomed Mater Res1973;7:301–311.CrossrefPubMed Google Scholar
3 Morscher E , MasarZ. Development and first experience with an uncemented press-fit cup. Clin Orthop Relat Res1988;232:96–103.PubMed Google Scholar
4 Pilliar RM , LeeJM, ManiatopoulosC. Observations on the effect of movement on bone ingrowth into porous-surfaced implants. Clin Orthop Relat Res1986;208:108–113.PubMed Google Scholar
5 Søballe K , HansenES, B-RasmussenH, JørgensenPH, BüngerC. Tissue ingrowth into titanium and hydroxyapatite-coated implants during stable and unstable mechanical conditions. J Orthop Res1992;10:285–299.CrossrefPubMed Google Scholar
6 Curtis MJ , JinnahRH, WilsonVD, HungerfordDS. The initial stability of uncemented acetabular components. J Bone Joint Surg [Br]1992;74-B:372–376.CrossrefPubMed Google Scholar
7 Kwong LM , O’ConnorDO, SedlacekRC, et al.A quantitative in vitro assessment of fit and screw fixation on the stability of a cementless hemispherical acetabular component. J Arthroplasty1994;9:163–170.CrossrefPubMed Google Scholar
8 MacKenzie JR , CallaghanJJ, PedersenDR, BrownTD. Areas of contact and extent of gaps with implantation of oversized acetabular components in total hip arthroplasty. Clin Orthop Relat Res1994;298:127–136.PubMed Google Scholar
9 Sharkey PF , HozackWJ, CallaghanJJ, et al.Acetabular fracture associated with cementless acetabular component insertion: a report of 13 cases. J Arthroplasty1999;14:426–431.CrossrefPubMed Google Scholar
10 Adler E , StuchinSA, KummerFJ. Stability of press-fit acetabular cups. J Arthroplasty1992;7:295–301.CrossrefPubMed Google Scholar
11 Saleh KJ , BearB, BostromM, WrightT, SculcoTP. Initial stability of press-fit acetabular components: an in vitro biomechanical study. Am J Orthop2008;37:519–522.PubMed Google Scholar
12 Kuhn A , SchellerG, SchwarzM. Primary stability of cement-free press-fit acetabulum cups: in vitro displacement studies. Biomed Tech1999;44:356–359. Google Scholar
13 Macdonald W , CarlssonLV, CharnleyGJ, JacobssonCM. Press-fit acetabular cup fixation: principles and testing. Proc Inst Mech Eng [H]1999;213:33–39.CrossrefPubMed Google Scholar
14 Olory B , HavetE, GabrionA, VernoisJ, MertlP. Comparative in vitro assessment of the primary stability of cementless press-fit acetabular cups. Acta Orthop Belg2004;70:31–37.PubMed Google Scholar
15 Small SR , BerendME, HowardLA, et al.High initial stability in porous titanium acetabular cups: a biomechanical study. J Arthroplasty2012;28:510–516.CrossrefPubMed Google Scholar
16 Litsky AS , PophalSG. Initial mechanical stability of acetabular prostheses. Orthopedics1994;17:53–57.CrossrefPubMed Google Scholar
17 Pitto RP , BöhnerJ, HofmeisterV. Factors affecting the primary stability of acetabular components: an in vitro study. Biomed Tech1997;42:363–368. Google Scholar
18 Li B , AspdenRM. Composition and mechanical properties of cancellous bone from the femoral head of patients with osteoporosis or osteoarthritis. J Bone Miner Res1997;12:641–651. Google Scholar
19 Fritsche A , BialekK, MittelmeierW, et al.Experimental investigations of the insertion and deformation behaviour of press-fit and threaded acetabular cups for total hip replacement. J Orthop Sci2008;13:240–247. Google Scholar
20 Antoniades G. Primary stability of uncemented cup designs in total hip replacement. Masters of Philosophy Thesis. Glasgow: University of Strathclyde, 2010. Google Scholar
21 Ong KL , SantnerTJ, BartelDL. Robust design for acetabular cup stability accounting for patient and surgical variability. J Biomech Eng2008;130:031001.CrossrefPubMed Google Scholar
22 D’Lima DD , UrquhartAG, BuehlerKO, WalkerRH, ColwellCW. The effect of the conjunction of the acetabular and femoral components on the range of motion of the hip at different head-neck ratios. J Bone Joint Surg [Am]2000;82-A:315–321. Google Scholar
23 Kummer FJ , ShahS, IyerS, DiCesarePE. The effect of acetabular cup orientations on limiting hip rotation. J Arthroplasty1999;14:509–513.CrossrefPubMed Google Scholar
24 Widmer KH , ZurfluhB. Compliant positioning of total hip components for optimal range of motion. J Orthop Res2004;22:815–821.CrossrefPubMed Google Scholar
25 Biederman R , ToninA, KrismerM, et al.Reducing the risk of dislocation after total hip arthroplasty: the effect of orientation of the acetabular component. J Bone Joint Surg [Br]2005;87-B:762–769.CrossrefPubMed Google Scholar
26 Kennedy JG , RogersWB, SoffeKE, et al.Effect of acetabular component orientation on recurrent dislocation, pelvis osteolysis, polyethylene wear and component migration. J Arthroplasty1998;13:530–534. Google Scholar
27 Nishii T , SuganoN, MikiH, et al.Influence of component positions on dislocation: computed tomographic evaluations in a consecutive series of total hip arthroplasty. J Arthroplasty2004;19:162–166.CrossrefPubMed Google Scholar
28 Patil S , BergulaA, ChenPC, ColwellCW, D’LimaDD. Polyethylene wear and acetabular component orientation. J Bone Joint Surg [Br]2003;85-B:56–63.CrossrefPubMed Google Scholar
29 Nunag P , DeakinAH, OburuE, SarungiM. Two-year radiologic assessment of the Trident Peripheral Self-Locking cup using EBRA. Hip Int2012;22:511–515.CrossrefPubMed Google Scholar
30 Baleani M , FognaniR, ToniA. Initial stability of a cementless acetabular cup design: experimental investigation of the effect of adding fins to the rim of the cup. Artif Organs2001;25:664–669. Google Scholar
31 Hadjari MH , HollisJM, HofmannOE, FlahiffCM, NelsonCL. Initial stability of porous coated acetabular implants: the effect of screw placement, screw tightness, defect type, and oversize implants. Clin Orthop Relat Res1994;307:117–123. Google Scholar
32 Ries MD , HarbaughM. Acetabular strains produced by oversized press fit cups. Clin Orthop Relat Res1997;334:276–281.PubMed Google Scholar
33 Wetzel R , SimnacherM, SchellerG. Initial stability of press-fit acetabular cups: an in-vitro study. Biomed Tech2005;50:400–403. Google Scholar
Funding statement:
This work was supported by a research grant from Stryker Ltd. This grant was used by the Golden Jubilee National Hospital to fund the research fellow post and pay tuition fees for the first author. Stryker Ltd provided material support for the study in the form of acetabular components and reamers.This work was presented at Bioengineering 08, at the British Hip Society Annual Scientific Meeting in 2009 and at the International Society of Biomechanics Annual Conference 2009.
Author contributions:
G. Antoniades: First author of original study, Study design, Performing trials, Data collection and analysis, Manuscript review and revision
E. J. Smith: Literature review, Writing paper
A. H. Deakin: Study design, Experimental design, Data collection, Manuscript preparation
S. C. Wearing: Assisted with study design, Data collection and analysis, Manuscript preparation
M. Sarungi: Study concept and design, Gained funding, Overview of study methodology, Reviewing and revising manuscript
ICMJE Conflict of Interest:
None declared. Stryker Ltd were not involved with the experiments, data analysis or reporting of this study.
©2013 The British Editorial Society of Bone & Joint Surgery. This is an open-access article distributed under the terms of the Creative Commons Attributions licence, which permits unrestricted use, distribution, and reproduction in any medium, but not for commercial gain, provided the original author and source are credited.









