Abstract
Objectives
To assess the effectiveness of a modified tibial tubercle osteotomy as a treatment for arthroscopically diagnosed chondromalacia patellae.
Methods
A total of 47 consecutive patients (51 knees) with arthroscopically proven chondromalacia, who had failed conservative management, underwent a modified Fulkerson tibial tubercle osteotomy. The mean age was 34.4 years (19.6 to 52.2). Pre-operatively, none of the patients exhibited signs of patellar maltracking or instability in association with their anterior knee pain. The minimum follow-up for the study was five years (mean 72.6 months (62 to 118)), with only one patient lost to follow-up.
Results
A total of 50 knees were reviewed. At final follow-up, the Kujala knee score improved from 39.2 (12 to 63) pre-operatively to 57.7 (16 to 89) post-operatively (p < 0.001). The visual analogue pain score improved from 7.8 (4 to 10) pre-operatively to 5.0 (0 to 10) post-operatively. Overall patient satisfaction with good or excellent results was 72%. Patients with the lowest pre-operative Kujala score benefitted the most. Older patients benefited less than younger ones. The outcome was independent of the grade of chondromalacia. Six patients required screw removal. There were no major complications.
Conclusions
We conclude that this modification of the Fulkerson procedure is a safe and useful operation to treat anterior knee pain in well aligned patellofemoral joints due to chondromalacia patellae in adults, when conservative measures have failed.
Article focus
The treatment of recalcitrant anterior knee pain with clinically normal tracking by using the Heatley modified Fulkerson tibial tubercle anteriorisation
Key messages
The Heatley modified Fulkerson anteriorisation of the tibial tubercle has good results with low complication rates
It is a reliable procedure in the appropriate patient with painful chondromalacia patellae
Strengths and limitations
This is a prospective study with only one of 51 knees lost to follow-up at a mean of five years
The cohort lacks a control group
Introduction
The term chondromalacia patellae was defined by Aleman in 1917.1 It means softening of the articular cartilage (Fig. 1) and is not synonymous with anterior knee pain for which there are numerous causes. It remains an enigma regarding both its pathology and symptoms. Pain is often out of proportion with the arthroscopic findings. Despite conservative management of this condition, up to 35% of patients may require operative treatment.2

Fig. 1
Electron microscope image of a section of human patella following freeze fracture processing, showing the structure of the articular cartilage.
The diagnosis of chondromalacia patellae is generally based on arthroscopic findings. Chondromalacia patellae is thought to occur as a result of abnormal stresses deep within the arcades of Benninghoff3 secondary to shear forces. Low impact stressing has been shown to cause vertical splitting of the cartilage in animal experiments.4 Ohno et al5 have demonstrated a loss of proteoglycans near fissures within the matrix of the cartilage in chondromalacia. This leads to a loss of three-dimensional structure and the development of matrix streaks and fissure formation (Fig. 2).

Fig. 2
Electron microscope image showing fissuring in the radial zone below an intact surface layer. The slits marked with * are the result of the freeze fracturing technique.
The idea of advancing the tibial tubercle anteriorly to reduce the load across the patellofemoral joint and improve quadriceps function was first reported by Maquet in 1963.6,7 Ferguson et al8 have reported up to an 80% decrease of the patellofemoral contact pressure after an elevation of the tibial tubercle by 0.5 inches (1.27 cm).
Our study attempts to assess the effectiveness of tibial tubercle osteotomy as a treatment for arthroscopically diagnosed chondromalacia patellae.
Patients and Methods
All patients that presented to one consultant surgeon with anterior knee pain between 1996 and 2001 were assessed and treated according to a strict protocol. The patients who were considered for inclusion in this study all complained of persistent anterior knee pain that was interfering with daily activities e.g. walking, running and climbing stairs. Those patients with anterior knee pain in association with patella maltracking, patellar instability or previous trauma to the patella were excluded from this study. Patellar maltracking was assessed clinically and radiologically. All patients pre-operatively had skyline radiographs of the patella in 30°, 60° and 90° of knee flexion, along with weight-bearing anteroposterior and lateral views of the knee.
All these patients were then enrolled in a physiotherapy rehabilitation programme. Of these patients, those with persistent unremitting anterior knee pain after a period of six months were offered a diagnostic arthroscopy. At arthroscopy, patients with chondromalacia patellae were graded as per the Outerbridge system9 (Table I). Those who received a therapeutic procedure such as a lateral release at the time of arthroscopy were excluded from inclusion in this study.
Table I
The Outerbridge grading system for chondromalacia patellae
| Grade | Description |
|---|---|
| Grade 0 | Normal cartilage |
| Grade I | Cartilage with softening and swelling |
| Grade II | A partial-thickness defect with fissures on the surface that do not reach subchondral bone or exceed 1.5 cm in diameter |
| Grade III | Fissuring to the level of subchondral bone in an area with a diameter more than 1.5 cm |
| Grade IV | Exposed subchondral bone |
Those patients with chondromalacia patellae and persistent anterior knee pain at six weeks after arthroscopy were offered a Heatley modified Fulkerson10,11 tibial tubercle osteotomy. They all provided informed consent for the procedure. In particular, the patients were counselled about scarring (a midline longitudinal scar 7 cm to 10 cm in length) and difficulty kneeling on their operated knee post-operatively due to the anteriorised subcutaneous position of the tibial tubercle. All patients were also informed that the subcutaneous screws might need to be removed at a later date.
A total of 47 patients (51 knees) thus received a tibial tubercle osteotomy between 1996 and 2001 and were the subjects of this study. The tibial tubercle osteotomy was performed by one consultant surgeon (PABM) at a mean of 14 months (9 to 22) after their first presentation in the outpatient clinic. Of the 51 knees studied, 15 had grade I, 17 had grade II, 16 had grade III and three had grade IV at arthroscopy. None had an Outerbridge grading of zero.
The patients were followed-up post-operatively at two weeks, six weeks, three months, six months, one year and annually thereafter. The final review was performed by one of three independent assessors (including one author, CMJ), who had not been involved in the patient’s operation, in a dedicated research clinic. One patient was lost to follow-up at one year and was not included in the study. He was happy with his surgery at last follow up. Therefore, 46 patients (50 knees) were followed for a mean of 72.4 months (62 to 118). There were seven male and 39 female patients with a mean age at the time of surgery of 34.4 years (19.6 to 52.2).
Surgical technique
The Heatley modified Fulkerson technique was used.10,11 The Fulkerson procedure, which was first described using medialisation and anteriorisation of the tibial tubercle without using bone graft. This was a smaller osteotomy than the Macquet. Heatley modified the angle of the osteotomy to achieve anteriorisation with minimal medialisation of the tibial tubercle.
This previously unreported technique involves a 7 cm to 10 cm vertical midline incision from the inferior pole of the patella to the distal end of the tibial tubercle. The patellar tendon is isolated by sharp dissection along its medial and lateral borders. A curved artery forcep is passed from medial to lateral deep to the tendon as it inserts on the tibial tubercle. The jaws of the forceps are opened to allow enough space for a small Langenbeck retractor to be passed deep to the tendon from both the medial and lateral aspects. This allows enough retraction of the patellar tendon to visualise the superior aspect of the tibial tubercle where the superior part of the osteotomy has to be made.
The medial and lateral limbs of the osteotomy are identified by incising the periosteum on the medial and lateral borders of the tibial tubercle. It is helpful to partially release the origin of tibialis anterior to enable good visualisation of the lateral aspect of the tibial tubercle. A series of 2.5 mm drill holes is now made along the medial and lateral limbs of the osteotomy and also on the superior aspect of the tibial tubercle which requires retraction of the patellar tendon insertion first medially, then laterally using a Langenbeck retractor as described above. The osteotomy is then completed by connecting the drill holes with an osteotome. Care is taken to preserve an anterior periosteal bridge at the distal extent of the osteotomy. This is performed by passing a small periosteal elevator under the periosteum from medial to lateral at the distal end of the osteotomy. Elevation of this bridge facilitates positioning of the final drill holes on the medial and lateral sides allowing the osteotomy to be completed deep to this periosteal bridge (Figs 3a and 3b). The osteotomy is started proximally on the superior surface of the tibial tubercle. The osteotome is introduced relatively vertically at the proximal end and relatively horizontally at the distal end. The proximal medial limb of the osteotomy should be at 20° to vertical, gradually flattening out until the most distal part of the osteotomy where the osteotome is almost horizontal (Fig. 3c). The osteotomy is completed deep to the anterior periosteal bridge. Once the osteotomy has been completed the isolated tibial tubercle is freely mobile, attached proximally by the patellar tendon and distally by the anterior periosteal bridge. Because the proximal part of the osteotomy is very steep, a relatively large amount of anteriorisation is achieved with minimal medialisation. Typically the tibial tubercle is anteriorised by approximately 1 cm to 1.5 cm (Fig. 3d). The osteotomy is held in position with a 2 mm Kirschner wire passed through the posterior tibial cortex. The osteotomy is fixed using two 3.5 mm self-tapping cortical screws also passed through the posterior tibial cortex by hand to avoid possible damage to the posterior structures. The wound is closed in layers.
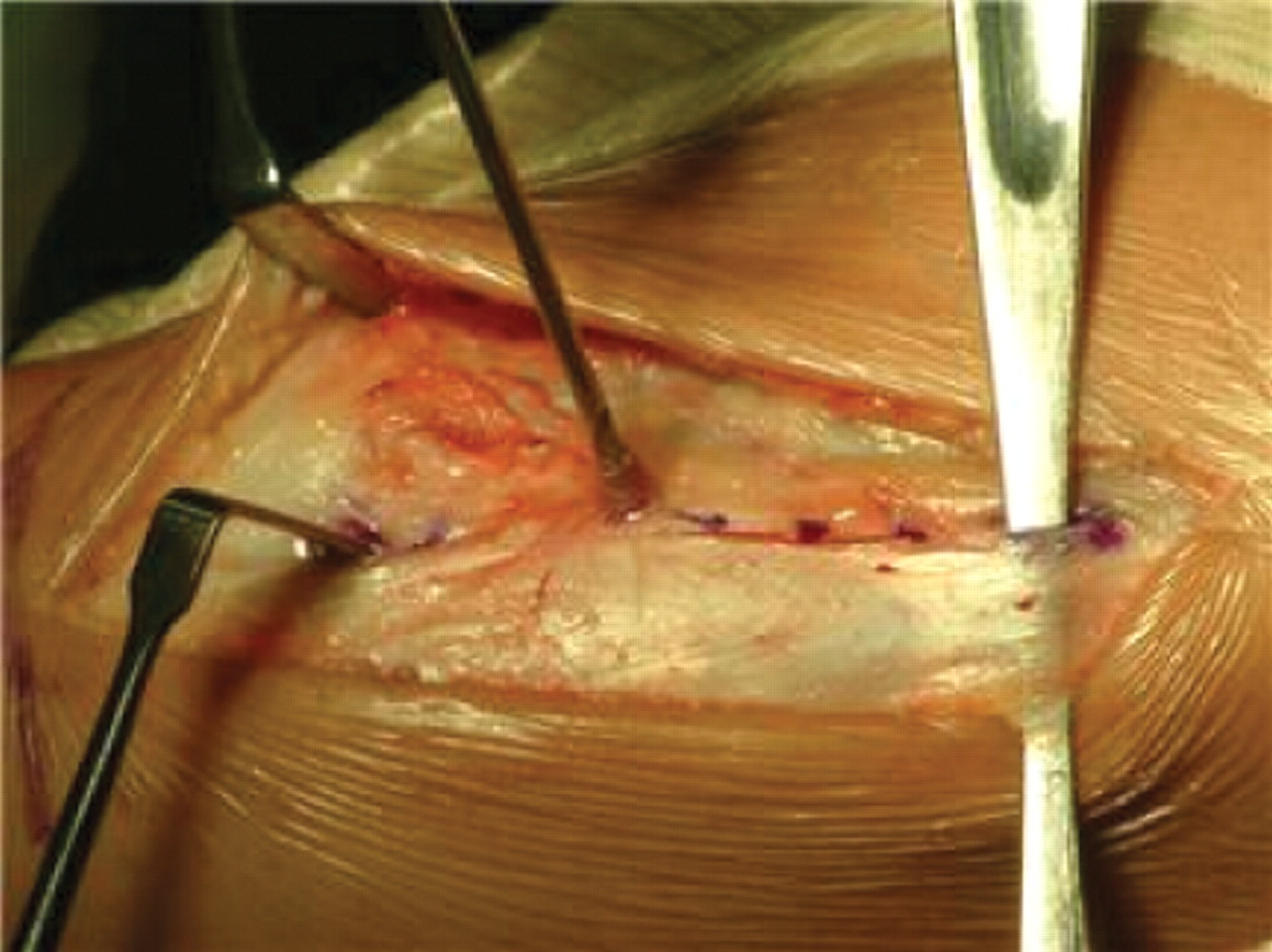

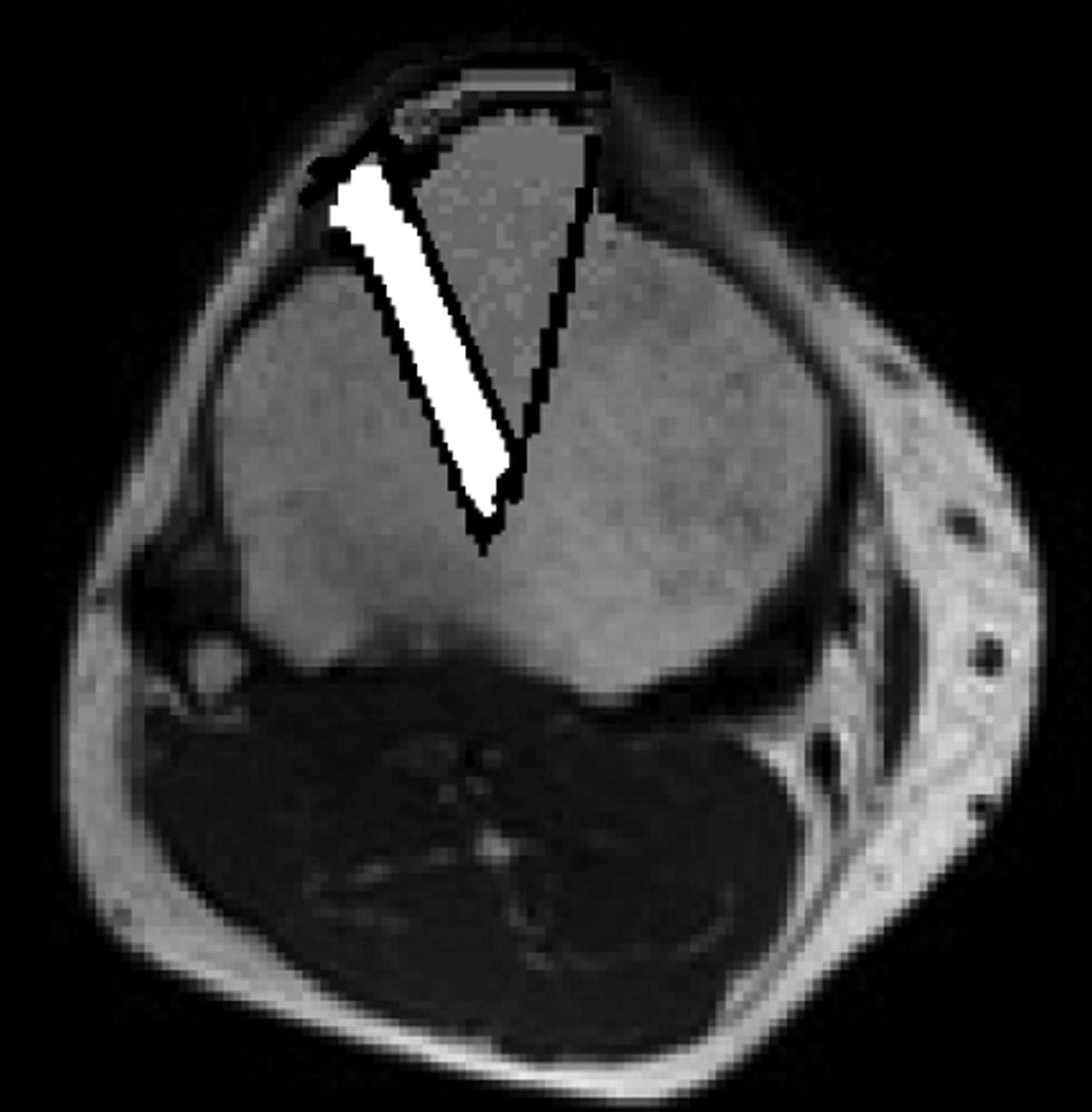
Figs. 3a - 3d
Figures 3a and 3b – intra-operative photographs of the modified tibial tubercle osteotomy: a) drill holes are made on either side of the tibial tubercle and a periosteal bridge is maintained distally. The drill holes are then joined with an osteotome angled to make the triangular osteotomy which is more acute proximally than distally to improve the stability of the construct. b) The osteotomy is anteriorised and held in place with two Kirschner wires before being held definitively with two 3.5 mm self-tapping cortical screws to allow compression. Figures 3c and 3d – diagrams representing the position of the osteotomy, showing c) that the angle of the cut is more acute proximally than distally, and showing d) the position in which the osteotomy is fixed, with the acute angle of the medial limb of the osteotomy meaning that little medialisation occurs for the degree of anteriorisation.
The mean length of stay was 3.2 days(1 to 7). Patients were allowed to fully weight bear post-operatively and were immobilised with a cricket pad splint for a period of two to four weeks. Normal activity was resumed between six and 12 weeks. The mean time off work was three months and mean time off sport 5.3 months.
Objective evaluation was undertaken using the Kujala functional knee scoring system.12 It is used to assess gait, ambulation, support, stair climbing, instability, pain, swelling, squatting flexion deficiency and thigh atrophy. A functional score between 0 and 100 is obtained. The closer the score is to 100, the better the function of the knee.
Patients were also assessed using a visual analogue scale (VAS) for pain from 0 to 10, with 0 equating to no pain and 10 the worst pain imaginable. In addition to this, a patient satisfaction score was used: 1) excellent or much better than before surgery; 2) good or better than before surgery; 3) fair or the same as before surgery; or 4) poor or worse than before surgery). The patients were also asked whether with hindsight they would have the procedure again.
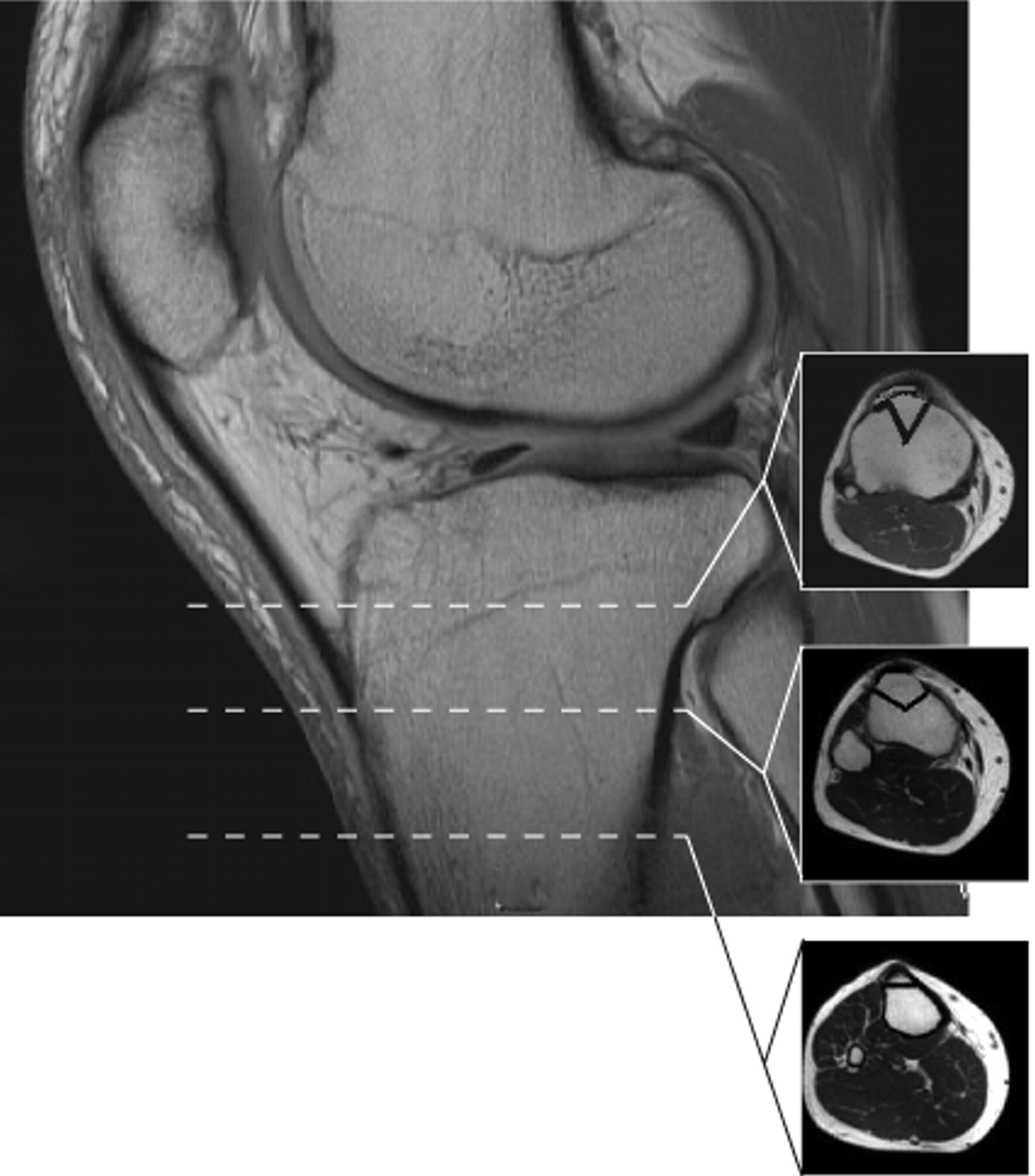
Assessment of union of the osteotomy
Anteroposterior and lateral radiographs were used to assess radiological consolidation of the osteotomy. The patients were also clinically assessed for tenderness and mobility at the osteotomy site at every post-operative visit. When all radiolucencies at the osteotomy site had filled in on serial radiographs, and the osteotomy was both non-tender and immobile, union was deemed to have occurred. Figure 4 shows a typical post-operative radiograph.

Fig. 4
A sample radiograph taken one year post-operatively.
Statistical analysis
This was performed using SPSS software (SPSS Inc., Chicago, Illinois). A Wilcoxon rank-sum test was used to detect difference between pre- and post-operative scores. A Mann-Whitney U test was used to detect any difference between results by gender, and the Kruskal-Wallis rank sum test was used to see if the grade of chondromalacia affected results. Kendall’s rank correlation was used to assess the correlation between pre-operative Kujala score and change in Kujala score, and the difference in Kujala score when considered against age. A p-value < 0.05 was considered significant.
Results
Clinical results
The mean preoperative Kujala score was 39.2 (12 to 63). At final follow up this score had improved to 57.7 (16 to 89) (Table II, Fig. 5). There was a statistically significant difference between the values using the Wilcoxon test with continuity correction (p < 0.001). Of the 50 knees, 46 (92%) showed an improvement in their Kujala scores post-operatively.
Table II
Mean pre-operative and 5-year post-operative scores
| Score | Pre-operative | Post-operative | p-value* | |
|---|---|---|---|---|
| Mean visual analogue scale for pain (range) | 7.8 (4 to 10) | 5.0 (0 to 10) | < 0.001 | |
| Mean Kujala score (range) | 39.2 (12 to 63) | 57.7 (16 to 89) | < 0.001 | |
-
* Wilcoxon rank sum test
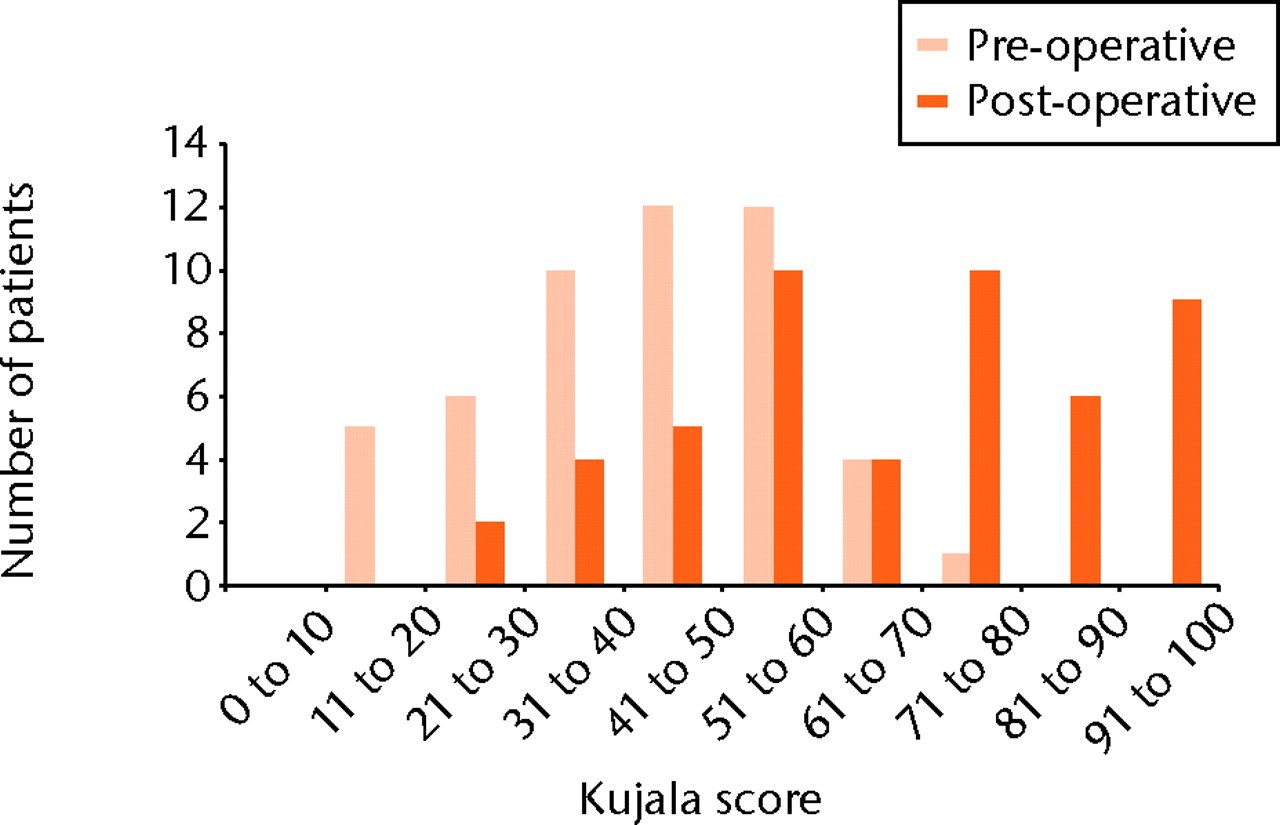
Fig. 5
Bar chart showing the distribution of Kujala scores pre-operatively and at five years post-operatively.
The mean pre-operative VAS for pain was 7.8 (4 to 10), which had decreased by at five years to 5.0 (0 to 10). Of the 50 knees, 37 (74%) had an improvement in the pain score at the latest follow-up. This was again statistically significant using the Wilcoxon test (p < 0.001) (Table II, Fig. 6). Six knees did not change, and seven had a higher score, with a mean increase of 1.3 points (1 to 4) on the VAS.
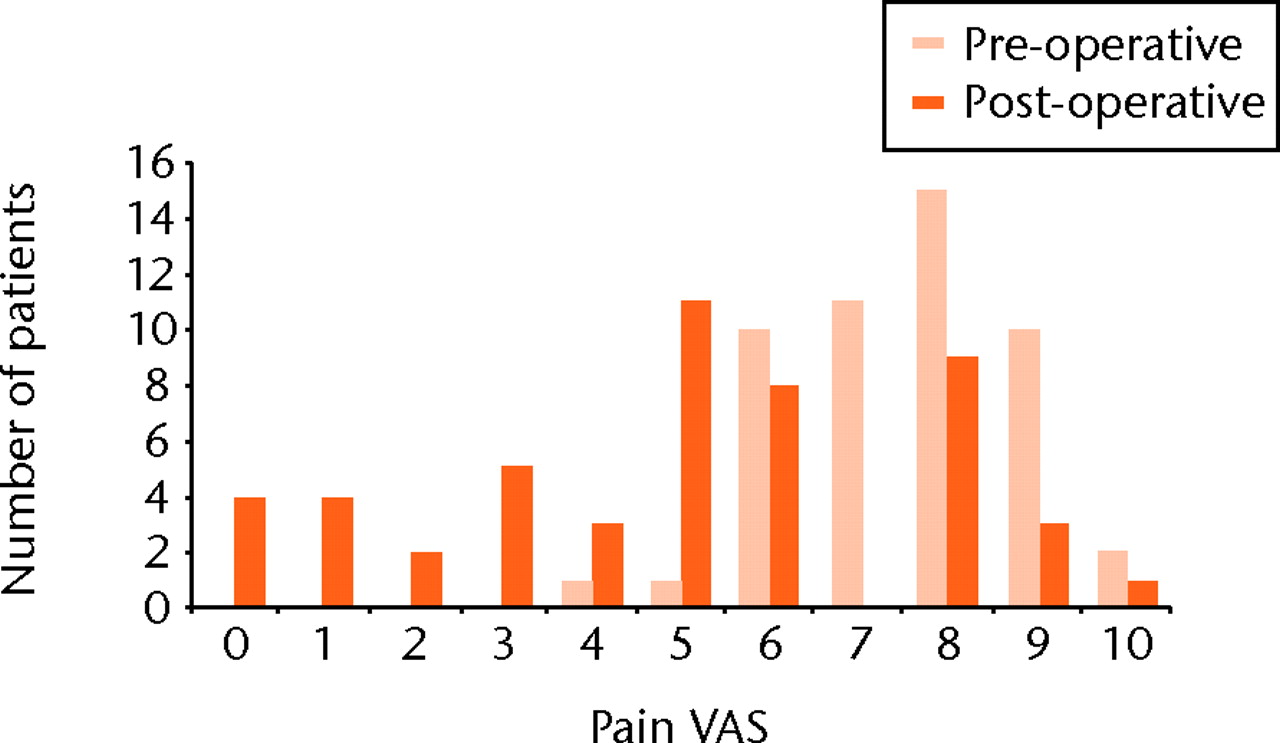
Fig. 6
Bar chart showing the distribution of the visual analogue scale (VAS) for pain pre-operatively and at five years post-operatively.
There was an obvious preponderance of females (39; 43 knees) over males (7; 8 knees) in this study. No significant difference was seen on either the post-operative Kujala scores or VAS for pain when the results of the females were compared with the male patients (p = 0.797 and p = 0.639, respectively; Mann-Whitney test).
The grade of chondromalacia patellae did not make a significant difference to the expected improvement (p = 0.28, Kruskal-Wallis rank sum). Older patients benefited less than younger patients (Kendall's rank correlation τ = 0.201, p = 0.04). Patients with the lowest pre-operative scores had the biggest improvement in Kujala score and therefore appeared to benefit most from surgery (Kendall's rank correlation τ = 0.254, p = 0.01).
Patient satisfaction
In terms of patient satisfaction, eight knees (16%) were rated as excellent, 28 (56%) as good, nine (18%) as the same as before surgery and five (10%) as poor. Furthermore, the patients comprising 43 of the knees (86%) stated that they would have the procedure again. Two patients (two knees) who reported poor results at five years, stated that they would have the operation again, as the result of surgery had been very good for previous years and only recently become worse.
All patients were satisfied with the post-operative cosmetic appearance of their knee after the osteotomy.
A total of 49 knees (98%) achieved bony union at one year. In the remaining knee with delayed radiological evidence of union, the Kujala score was 79 and the patient reported an excellent result at one year.
Complications
There was one undisplaced fracture through the proximal screw hole following a fall. This went on to unite satisfactorily without the need for further surgery. One patient had a superficial infection and was treated with antibiotics successfully for five days by the general practitioner. At the two-week post-operative appointment, all signs of the superficial infection had disappeared.
Only six knees (12%) required removal of screws due to the patient experiencing pain while kneeling. Pain was relieved in four (8%) but two (4%) continued to experience pain when kneeling.
Discussion
Whilst conservative treatment such as physiotherapy can be helpful for patients with anterior knee pain,13,14 there remains a group of patients with persistent debilitating symptoms.
At arthroscopy, experience is required in assessing the degree of softening of the articular surface when the articular surface of the dome is intact. It is always good practice to compare the dome with the concave lateral facet.
Many different procedures have been described to surgically treat chondromalacia patellae, such as drilling, shaving,15 lateral release,16 medial plication17 and patellectomy.18 Interestingly, Hejgaard and Watt-Boolsen19 have demonstrated an advantage in combining anterior displacement of the tibial tubercle to shaving alone.
The patella engages in the trochlear groove in about 30° to 90° of knee flexion, and we believe that surgical anteriorisation of the tibial tubercle will decrease patellofemoral contact pressure in this functional range in particular. The modified Fulkerson procedure seems a logical method of treating this condition, because it adopts the Maquet principle to decrease stress through the patella, and does not alter the articular structure of the knee.
Previously described tibial tubercle osteotomies include the Hauser,20 Roux-Goldthwaite,21 Trillat22 and Bandi23 procedures. These operations were designed to provide medialisation. Since our patient group did not have significant patellar mal-tracking it was not appropriate to alter this by medialisation of the tibial tubercle.
Jenny et al24 reviewed 100 patients who underwent the Maquet procedure for grade IV chondromalacia patellae at a mean follow-up of four years. The pain score improved significantly after the operation and remained unchanged with longer follow-up. The success rate was 62%. The failure rate was about 30% and they reported a 9% rate of serious complications
Lund et al25studied 68 knees in 62 patients with anterior displacement of the tibial tuberosity. Complications were encountered in 22 osteotomies (35%). Hadjipavlou et al26 identified an unacceptable complication rate (8%) in the patients undergoing a Maquet osteotomy for chondromalacia patellae. These included wound breakdown, osteomyelitis and fracture.
While complications have discouraged many from using such techniques,27 good results have been reported previously. Both Heatley, Allen and Patrick28 and Silvello et al29 have reported 65% good or excellent results at 3 years. Buuck and Fulkerson30 demonstrated long-term success and an increase in activity levels at four to 12 years after anterior transfer of the tibial tubercle.
The final result of any elective surgical procedure must also include a cosmetically acceptable post-operative scar. The Heatley modified Fulkerson osteotomy was performed via a relatively small 7 cm to 10 cm skin incision unlike the Maquet osteotomy. Although we accept that no direct comparison of patient satisfaction has been made with a controlled cohort of patients who had other tibial tubercle osteotomies, we believe this smaller osteotomy to be cosmetically superior to the Maquet osteotomy.
We recognise the lack of a control group in this study. We also observe that 43 of the 47 patients had unilateral surgery. Although a number of patients with anterior knee pain due to chondromalacia patellae report bilateral symptoms, the symptoms are frequently not of the same severity. In our experience, once pain relief was achieved in the more severe knee, patients were often able to manage the symptoms in the contralateral knee.
Radiological union can be assessed most accurately using a CT scan, and we accept that we did not perform this to assess union of the osteotomy in our patients. We however believe that the appearance of progressive consolidation of the osteotomy site on plain radiographs, used in conjunction with careful clinical assessment to be suitably accurate in assessing union of the Heatley modified Fulkerson osteotomy.
Our patient selection was based on strict inclusion criteria. Using the Heatley modified Fulkerson technique, we have shown a 92% improvement of their symptoms in the Kujala score and with 86% reporting that they would have the procedure again. The complication rate of 4% (one superficial infection and one un-displaced fracture, both with good functional improvement at one year) for this procedure is lower than reported by other similar cohorts.
The Heatley modified Fulkerson tibial tubercle osteotomy is a safe and useful operation to treat anterior knee pain in well aligned patellofemoral joints due to chondromalacia patellae in adults when conservative measures have failed.
The authors would like to thank K. Miles and D. East at the Research Department of the Conquest Hospital, as well as the East Sussex Healthcare Trust Library.
1 Kipnis J, Scuderi GR. A historic review of patellar pain. In: Scuderi GR, ed. The patella. Springer-Verlag, 1995:1–7. Google Scholar
2 Bentley G . Chondromalacia patellae. J Bone Joint Surg [Am]1970;52-A:221–232.CrossrefPubMed Google Scholar
3 Benninghoff A. Form und Bann der Gelenkknorpel in inhren Beziehungren zur Funktion. Zweiter Teli: Zeitschrift fur Zellforschung und Mikroskopishe Anatromie. Z Zellforsch 1925;2:783 (in German). Google Scholar
4 Tomatsu T , ImaiN, TakeuchiN, TakahashiK, KimuraN. Experimentally produced fractures of articular cartilage and bone: the effects of shear forces on the pig knee. J Bone Joint Surg [Br]1992;74-B:457–462. Google Scholar
5 Ohno O , NaitoJ, IguchiT, et al.An electron microscopic study of early pathology in chondromalacia of the patella. J Bone Joint Surg [Am]1988;70-A:883–899.PubMed Google Scholar
6 Maquet P . A biomechanical treatment of femoro-patellar arthrosis: advancement of the patellar tendon. Rev Rhum Mal Osteoartic1963;30:779–783. Google Scholar
7 Maquet P . Advancement of the tibial tuberosity. Clin Orthop Relat Res1976;115:225–230. Google Scholar
8 Ferguson AB Jr , BrownTD, FuFH, RutkowskiR. Relief of patellofemoral contact stress by anterior displacement of the tibial tubercle. J Bone Joint Surg [Am]1979;61-A:159–166.PubMed Google Scholar
9 Outerbridge RE . The etiology of chondromalacia patellae. J Bone Joint Surg [Br]1961;43-B:752–757.CrossrefPubMed Google Scholar
10 Fulkerson JP , BeckerGJ, MeaneyJA. , .Miranda M, Folcik MA. Anteromedial tibial tubercle transfer without bone graft. Am J Sports Med1990;18:490–497. Google Scholar
11 Fulkerson JP . Anteromedialisation of the tibial tuberosity for patello femoral malalignment. Clin Orthop Relat Res1983;177:176–181. Google Scholar
12 Kujala UM , JaakkolaLH, KoskinsenSK, et al. Scoring of patellofemoral disorders. Arthroscopy1993;9:159–163. Google Scholar
13 Witvrouw E , LysensR, BellemansJ, PeersK, VanderstraetenG. Open versus closed kinetic exercises for patellofemoral pain: a prospective, randomized study. Am J Sports Med2000;28:687–694. Google Scholar
14 Crossley K , BennellK, GreenS, CowanS, McConnellJ. Physical therapy for patellofemoral pain: a randomized, double-blinded, placebo-controlled trial. Am J Sports Med2002;30:857–865.CrossrefPubMed Google Scholar
15 Bentley G . The surgical treatment of chondromalacia patellae. J Bone Joint Surg [Br]1978;60-B:74–81.CrossrefPubMed Google Scholar
16 Väätäinen U , KivirantaI, JaromaH, AiraksinenO. Lateral release in chondromalacia patellae using clinical, radiologic, electromyographic, and muscle force testing evaluation. Arch Phys Med Rehabil1994;75:1127–1131.CrossrefPubMed Google Scholar
17 Huberti HH , HayesWC. Contact pressures in chondromalacia patellae and the effects of capsular reconstructive procedures. J Orthop Res1988;6:499–508.CrossrefPubMed Google Scholar
18 Chakraverty AC . Patellectomy for chondromalacia patellae. Bristol Med Chir J1972;87:60.PubMed Google Scholar
19 Hejgaard N , Watt-BoolsenS. The effect of anterior displacement of the tibial tuberosity in idiopathic chondromalacia patellae: a prospective randomized study. Acta Orthop Scand1982;53:135–139.CrossrefPubMed Google Scholar
20 Hauser ED . Total tendon transplant for slipping patella: a new operation for dislocation of the patella. 1938. Clin Orthop Relat Res2006;452:7–16. Google Scholar
21 Roux C. Luxation habituelle de la rotule: traitment operatoire. Rev Chir Orthop Reparatrice Appar Mot 1888;8:682–689 (in French). Google Scholar
22 Trillat A , DejourH, CouetteA. Diagnosis and treatment of recurrent dislocations of the patella. Rev Chir Orthop Reparatrice Appar Mot1964;50:813–824. Google Scholar
23 Bandi W . Operative treatment of chondromalacia patellae. Zentralbl Chir1977;102:1297–1301. Google Scholar
24 Jenny JY , SaderZ, HenryA, JennyG, JaegerJH. Elevation of the tibial tubercle for patellofemoral pain syndrome: an 8- to 15-year follow-up. Knee Surg Sports Traumatol Arthrosc1996;4:92–96. Google Scholar
25 Lund F , NilssonBE. Anterior displacement of the tibial tuberosity in chondromalacia patellae. Acta Orthop Scand1980;51:679–688.CrossrefPubMed Google Scholar
26 Hadjipavlou A , HelmyH, DubravcikP, HellerL, KernerM. Maquet osteotomy for chondromalacia patellae: avoiding the pitfalls. Can J Surg1982;25:342–345.PubMed Google Scholar
27 Schepsis AA , DeSimoneAA, LeachRE. Anterior tibial tubercle transposition for patellofemoral arthrosis. Am J Knee Surg1994;7:13–20. Google Scholar
28 Heatley FW , AllenPR, PatrickJH. Tibial tubercle advancement for anterior knee pain: a temporary or permanent solution. Clin Orthop Relat Res1986;208:215–224. Google Scholar
29 Silvello L , ScarponiR, GuazzettiR, BianchettiM, FioreAM. Tibial tubercle advancement by the Maquet technique for patellofemoral arthritis or chondromalacia. Ital J Orthop Traumatol1987;13:37–44. Google Scholar
30 Buuck DA , FulkersonJP. Anteromedialisation of the tibial tubercle: a 4- to 12-year follow-up. Oper Tech Sports Med2000;8:131–137. Google Scholar
Funding statement:
None declared
Author contributions:
C. M. Jack: Writing the paper, Data collection
H. O. Khan: Statistical analysis
O. Keast-Butler: Data collection
P. A. Butler-Manuel: Study design, Lead surgeon
F. W. Heatley: Writing the paper, Study design, Invented technique
S. S. Rajaratnam: Writing the paper, Data collection
ICMJE Conflict of Interest:
None declared
©2012 British Editorial Society of Bone and Joint Surgery. This is an open-access article distributed under the terms of the Creative Commons Attributions licence, which permits unrestricted use, distribution, and reproduction in any medium, but not for commercial gain, provided the original author and source are credited.









