Abstract
Objectives
Our aim was to assess the use of intra-operative fluoroscopy in the assessment of the position of the tibial tunnel during reconstruction of the anterior cruciate ligament (ACL).
Methods
Between January and June 2009 a total of 31 arthroscopic hamstring ACL reconstructions were performed. Intra-operative fluoroscopy was introduced (when available) to verify the position of the guidewire before tunnel reaming. It was only available for use in 20 cases, due to other demands on the radiology department. The tourniquet times were compared between the two groups and all cases where radiological images lead to re-positioning of the guide wire were recorded. The secondary outcome involved assessing the tibial interference screw position measured on post-operative radiographs and comparing with the known tunnel position as shown on intra-operative fluoroscopic images.
Results
Of the 20 patients treated with fluoroscopy, the imaging led to repositioning of the tibial guide wire before reaming in three (15%). The mean tourniquet time with intra-operative fluoroscopy was 56 minutes (44 to 70) compared with 51 minutes (42 to 67) for the operations performed without. Six patients (30%) had post-operative screw positions that were > 5% more posterior than the known position of the tibial tunnel.
Conclusion
Intra-operative fluoroscopy can be effectively used to improve the accuracy of tibial tunnel positions with minimal increase in tourniquet time. This study also demonstrates the potential inaccuracy associated with plain radiological assessment of tunnel position.
Article focus
Does the use of intra-operative fluoroscopy increase the accuracy of tibial tunnel positioning?
Key messages
Fluoroscopy is a useful tool to assist with accurate positioning of tunnels intra-operatively
The position of the tibial screw on post-operative radiographs cannot be relied upon to make accurate measurements of tunnel positions
Strengths and limitations
Highlights the potential inaccuracy associated with tunnel assessment on plain radiographs
This is an audit of a change in practice. Assessment of introduction of intra-operative fluoroscopy would be best carried out with a controlled trial
This audit of practice does however identify the potential benefit of using fluoroscopy
Novel finding of difference between true tunnel positions and screw positions
Small numbers were involved in this study
Introduction
The accuracy of bone tunnel placement is crucial for successful outcome in anterior cruciate ligament (ACL) reconstruction surgery. Isometric positioning of the tunnels minimises graft stretching, improves rotational control, decreases the risk of notch impingement and reduces the risk of re-rupture.1-3 Reports have confirmed significant variation in tunnel placement,4 even in the hands of experts,5 and is associated with worse outcome.6
Intra-operative fluoroscopy has been used in order to better identify bony landmarks and therefore improve the accuracy of tunnel positions.7 It has been shown that the radiation exposure required is safe and not a contraindication to its use in ACL reconstruction.8
A routine unpublished audit of femoral and tibial tunnel positions following single bundle hamstring arthroscopic ACL reconstruction by the senior author (BL) identified inconsistencies in tibial tunnel positions in the sagittal plane. The tunnels were assessed according to the method of Pinczewski et al,2 which is for a single-bundle technique. In their review of femoral and tibial tunnels they found that the only significant difference between those who suffered rupture and those with an intact graft at seven years was the position of the tibial tunnel in the sagittal plane.2 The incidence of rupture increased if the tunnel was placed > 50% posteriorly along the length of the anterior tibial plateau. Loss of knee flexion was significantly associated with more posterior placement of the tibial tunnel. Based on this evidence and the results of the audit, we introduced intra-operative fluoroscopy and audited this change in practice.
When assessing the position of the tunnels, difficulties associated with accurately identifying the tunnels on early post-operative radiographs became apparent. The tunnel positions on these radiographs are normally inferred by the position of the metal interference screw, whereas on later radiographs the sclerotic margins of the tunnels allows more accurate interpretation.2,4 A secondary outcome of this study was to compare the true tunnel position as assessed by intra-operative fluoroscopy with the post-operative early radiological assessment of tunnel position.
Patients and Methods
Between January and June 2009 it became routine practice for the senior author (BL) to include (when available) the use of intra-operative sagittal plane fluoroscopy to aid tunnel placement. In the study period, a total of 31 ACL reconstructions were undertaken on 31 patients. Intra-operative fluoroscopy was available in 20 of these procedures, forming the group for this study.
ACL reconstruction was performed under tourniquet control using a standard arthroscopic technique, with a four-strand hamstring graft, femoral tunnel drilling via the anteromedial portal, endobutton femoral fixation, and a tibial RCI interference screw (Smith and Nephew, Andover, Massachusetts) that was usually 35 mm long within a 40 mm tunnel. When available, the fluoroscope was positioned to allow lateral imaging of the flexed knee, allowing a check on the entry point of the femoral tunnel and the exit point of the tibial tunnel. The guide wire was re-positioned before tunnel reaming if indicated. Images were retained both of the guide wire position and the tibial tunnel reamer within the tunnel.
Patients were discharged the day after surgery and were enrolled in a standard accelerated rehabilitation programme. Patients were seen at two weeks for a post-operative clinical check and routine anteroposterior (AP) and lateral radiographs were performed to record the position of the metalwork. Patients were reviewed to assess subsequent progress at six weeks and again at eight months when the International Knee Documentation Committee (IKDC) subjective knee evaluation score9 and Tegner activity score10 were recorded.
The positions of the tibial tunnel reamer on lateral intra-operative fluoroscopic images and of the interference screw on post-operative lateral radiographs were measured independently by three of the authors (AWH, BL and RG). Standard measurement tools available on the Picture Archiving and Communications System (PACS) were used and placement of the tibial tunnel was assessed as follows (Figs 1 and 2): the length of the tibial plateau was determined and the positions of the anterior and posterior borders of the tibial tunnel were identified relative to the anterior edge of the plateau. This allowed the centre of the tunnel to be calculated and then expressed as a proportion of the total length of the tibial plateau.2,4,11
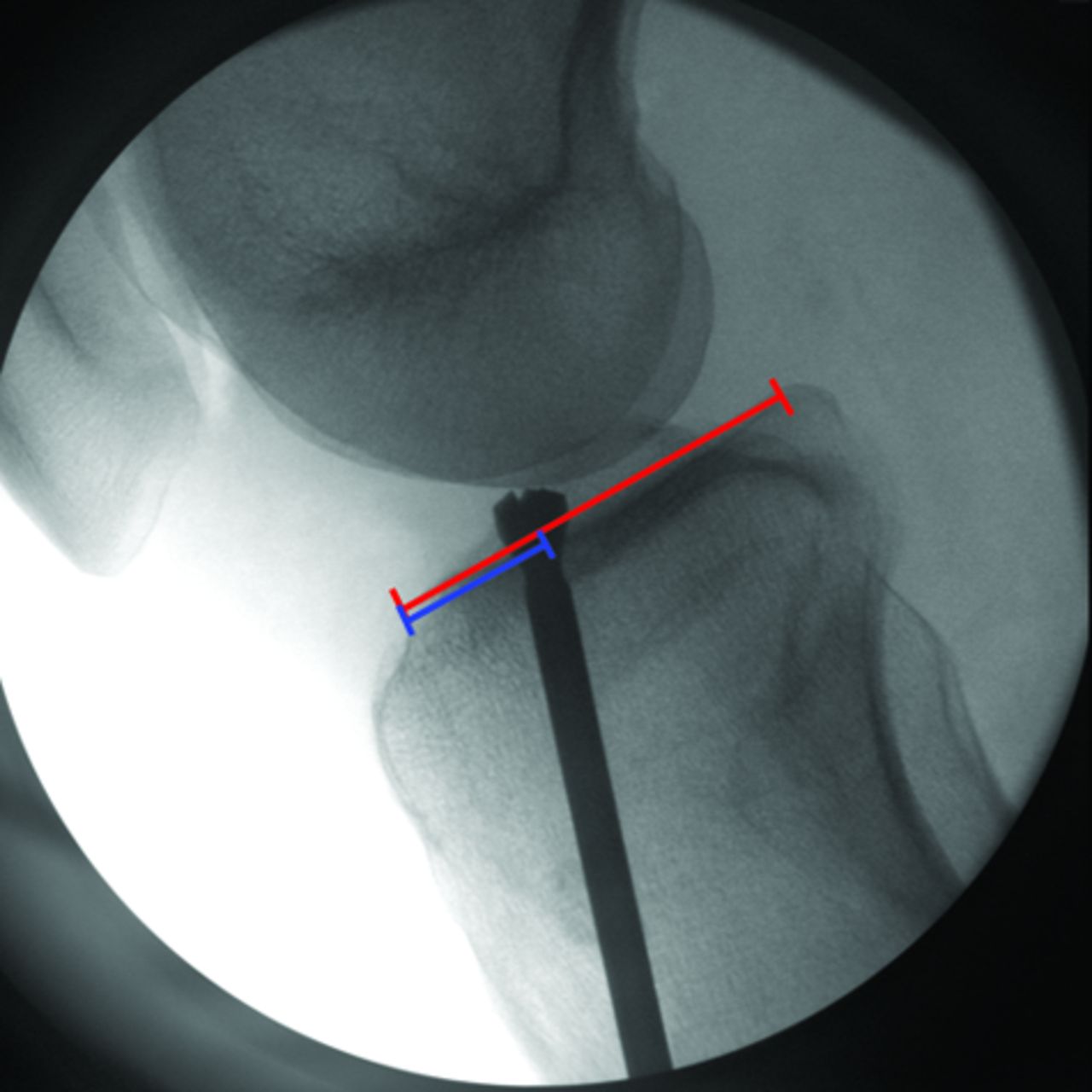

Figs. 1a - 1b
Intra-operative fluoroscopic image (a) and post-operative radiograph (b) showing the interference screw following the position of the reamer.
Statistical analysis
Results are expressed as mean and standard deviation (sd) of the measurements taken by the three authors. Mean intra-operative and post-operative measurements were compared using a Wilcoxon matched-pairs signed-ranks test. A p-value < 0.05 was considered to denote statistical significance.
Results
The fluoroscopy group comprised 20 patients (12 men and eight women) with a mean age of 31 years (16 to 50), and the non-fluoroscopy group comprised 11 patients (seven men and four women) with a mean age of 33 years (18 to 44). The mean tourniquet time for the 20 operations with fluoroscopy was 56 minutes (44 to 70), compared with 51 minutes (42 to 67) for those operations performed without fluoroscopic guidance. Other intra-articular procedures such as partial meniscectomy or meniscal repair were undertaken in eight patients in the fluoroscopy group and in three patients in the non-fluoroscopy group.
Intra-operative fluoroscopy revealed the position of the tibial guide wire to be unsatisfactory in three patients (15%), and the wire was therefore re-positioned before tunnel reaming.
The interobserver reliability of tunnel position was assessed graphically and using analysis of variance (ANOVA). The results indicated that assessment of fluoroscopic and post-operative radiographs were similar between the three clinicians (p = 0.903 and p = 0.961, respectively). The mean tibial tunnel position as indicated by the tunnel reamer was 41% (sd 2.7; 37% to 47%) of the total plateau depth (Figs 1a and 2a). The mean position of the tibial screw on post-operative radiographs was 46% (sd 9.2; 38% to 76%) of the total plateau depth (Figs 1b and 2b). A total of six patients (30%) had post-operative screw positions that were > 5% more posterior than the known intra-operative position of the tibial tunnel. A Wilcoxon matched-pairs signed-ranks test shows that the difference between true tunnel position and interference screw position is significant (p = 0.022).
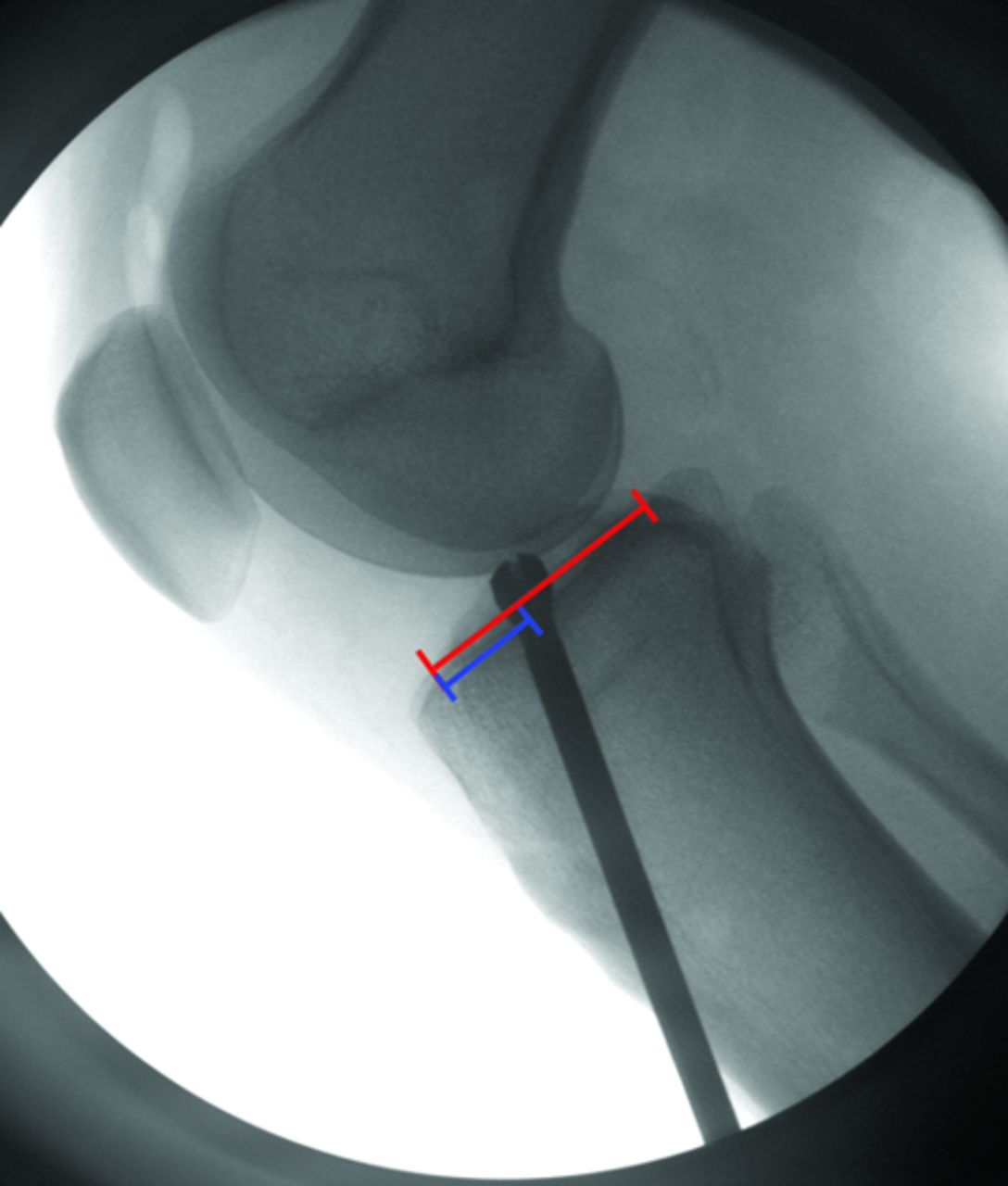

Figs. 2a - 2b
Intra-operative fluoroscopic image (a) and post-operative radiograph (b) showing the interference screw not following the position of the reamer.
Although the long-term outcome of these operations is not yet known, all patients have been seen and assessed at a minimum of eight months follow-up. One patient sustained a re-rupture at four months when he fell awkwardly off a step and has undergone revision reconstruction. The remaining 19 patients of the fluoroscopy group are all doing well, with a mean IKDC score of 83.6 (67 to 95) and mean Tegner activity score 6.1 (4 to 9). The results for the six patients with posterior screw positions are also good, with similar results to those seen in the remaining 13 patients (IKDC: 85 (76 to 90) versus 82.1 (67 to 95); Tegner: 5.8 (4 to 9) versus 6 (4 to 9)).
Discussion
This study shows that accurate placement of the tibial bone tunnel can be achieved with use of intra-operative image intensification and with minimal time added to the procedure (approximately five minutes), adding to the body of evidence to support the use of intra-operative fluoroscopy for hamstring ACL reconstruction.11,12 This is also the first study to quantify the relationship between the positions of the interference screw and the true tunnel position based on intra-operative fluoroscopic images.
It is accepted that bone tunnels should be positioned as anatomically as possible to prevent impingement, graft stretching, over constraint or restriction of motion of the knee.1,2 Pinczewski et al2 related tunnel position to outcome at seven years in 200 patients. A tibial tunnel placed > 50% posteriorly from the anterior tibial plateau was associated with loss of knee flexion and a higher incidence of graft rupture. Behrend et al12 studied tunnel positioning in 50 patients operated on by surgeons with varying degrees of expertise, and reported correct placement of the tibial tunnels in only 64% of knees, and that there was no significant correlation between tunnel placement and surgical expertise. There was a highly significant correlation between an anterior femoral tunnel and worse outcome.12 Ahn et al13 identified sagittal tunnel position as one of the risk factors associated with the onset of medial-compartment osteoarthritis. This was thought to be related to anterior position of the graft causing impingement to the notch, possibly leading to graft failure, anterior instability and eventually osteoarthritis. There is still some debate as to where the optimum position should be for tibial and femoral tunnels,14-16 but any intervention that allows more accurate placement intra-operatively has to be beneficial to outcome in the long-term.
Mehta et al17 examined whether the use of intra-operative fluoroscopy influenced surgical decision-making. Using a trans-tibial technique in 407 procedures, the position of the femoral tunnel entry point was altered in 62 (15%), usually more posteriorly. Although they were assessing femoral and not tibial tunnels, their rate of re-positioning was the same as this study.
The discrepancy between tunnel position and screw position may be explained by the soft cancellous metaphyseal bone. Although the intended technique is to insert the screw between the four strands of the hamstring graft over a flexible guide wire, the interference screw can meet with resistance from the graft and may adopt the path of least resistance posteriorly through the tunnel wall. This could be overcome by using a more rigid guide wire with the tip arthroscopically visualised in the tunnel before screw placement. Although some deviation between measurements taken from intra- and post-operative films can be expected due to minor differences in rotation, this error should be minimised by expressing the position as a percentage of the total plateau depth, suggesting that the differences observed in this study are genuine. Patients in this study with screws positioned posteriorly still achieved good outcome, suggesting that a screw that deviates from the centre of the tunnel gives satisfactory graft fixation. The long-term outcome is still uncertain and there may be problems with tunnel enlargement related to posterior screw positions.
1 Khalfayan EE , SharkeyPF, AlexanderAH, BrucknerJD, BynumEB. The relationship between tunnel placement and clinical results after anterior cruciate ligament reconstruction. Am J Sports Med1996;24:335–341.CrossrefPubMed Google Scholar
2 Pinczewski LA , SalmonLJ, JacksonWF, et al.Radiological landmarks for placement of the tunnels in single-bundle reconstruction of the anterior cruciate ligament. J Bone Joint Surg [Br]2008;90-B:172–179.CrossrefPubMed Google Scholar
3 Barrett GR , TreacySH. The effect of intraoperative isometric measurement on the outcome of anterior cruciate ligament reconstruction: a clinical analysis. Arthroscopy1996;12:645–651.CrossrefPubMed Google Scholar
4 Topliss C , WebbJ. An audit of tunnel position in anterior cruciate ligament reconstruction. Knee2001;8:59–63.CrossrefPubMed Google Scholar
5 Kohn D , BeuscheT, CarisJ. Drill hole position in endoscopic anterior cruciate ligament reconstruction: results on an advanced arthroscopy course. Knee Surg Sports Traumatol Arthrosc1998;6(Suppl):13–15. Google Scholar
6 Allen CR , GriffinJR, HarnerCD. Revision anterior cruciate ligament reconstruction. Orthop Clin North Am2003;34:79–98.CrossrefPubMed Google Scholar
7 Goble EM . Fluoroscopic allograft anterior cruciate reconstruction. Tech Orthop1988;2:65–73. Google Scholar
8 Chitnavis JP , KarthikesalingamA, MacdonaldA, BrownC. Radiation risk from fluoroscopically-assisted anterior cruciate ligament reconstruction. Ann R Coll Surg Engl2010;92:330–334.CrossrefPubMed Google Scholar
9 Anderson AF , IrrgangJJ, KocherMS, MannBJ, HarrastJJ. The International Knee Documentation Committee Subjective Knee Evaluation Form: normative data. Am J Sports Med2006;34:128–135.CrossrefPubMed Google Scholar
10 Tegner Y , LysholmJ. Rating systems in the evaluation of knee ligament injuries. Clin Orthop Relat Res1985;198:43–49.PubMed Google Scholar
11 Howell SM , HullML. Checkpoints for judging tunnel and anterior cruciate ligament graft placement. J Knee Surg2009;22:161–170.CrossrefPubMed Google Scholar
12 Behrend H , StutzG, KesslerMA, et al.Tunnel placement in anterior cruciate ligament (ACL) reconstruction: quality control in a teaching hospital. Knee Surg Sports Traumatol Arthrosc2006;14:1159–1165.CrossrefPubMed Google Scholar
13 Ahn JH, Kim JG, Wang JH, Jung CH, Lim HC. Long-term results of anterior cruciate ligament reconstruction using bone–patellar tendon–bone: an analysis of the factors affecting the development of osteoarthritis. Arthroscopy 2012:Epub. Google Scholar
14 Yasuda K , van EckCF, HoshinoY, FuFH, TashmanS. Anatomic single- and double-bundle anterior cruciate ligament reconstruction, part 1: Basic science. Am J Sports Med2011;39:1789–1799.CrossrefPubMed Google Scholar
15 Hensler D , Van EckCF, FuFH, IrrgangJJ. Anatomic anterior cruciate ligament reconstruction utilizing the double-bundle technique. J Orthop Sports Phys Ther2012;42:184–195.CrossrefPubMed Google Scholar
16 Alentorn-Geli E , LajaraF, SamitierG, CugatR. The transtibial versus the anteromedial portal technique in the arthroscopic bone-patellar tendon-bone anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc2010;188:1013–1037.CrossrefPubMed Google Scholar
17 Mehta VM , PaxtonEW, FithianDC. Does the use of fluoroscopic and isometry during anterior cruciate ligament reconstruction affect surgical decision making?Clin J Sport Med2009;19:46–48. Google Scholar
Funding statement:
None declared
Author contributions:
A. W. Hughes: Writing the paper, Data collection and analysis, Statistical analysis
A. J. Dwyer: Data collection and analysis
R. Govindaswamy: Data collection, Writing the paper
B. Lankester: Performing surgery, Writing the paper
ICMJE Conflict of Interest:
None declared
©2012 British Editorial Society of Bone and Joint Surgery. This is an open-access article distributed under the terms of the Creative Commons Attributions licence, which permits unrestricted use, distribution, and reproduction in any medium, but not for commercial gain, provided the original author and source are credited.









