Abstract
Aims
The aim of this to study was to compare the previously unreported long-term survival outcome of the Oxford medial unicompartmental knee arthroplasty (UKA) performed by trainee surgeons and consultants.
Patients and Methods
We therefore identified a previously unreported cohort of 1084 knees in 947 patients who had a UKA inserted for anteromedial knee arthritis by consultants and surgeons in training, at a tertiary arthroplasty centre and performed survival analysis on the group with revision as the endpoint.
Results
The ten-year cumulative survival rate for revision or exchange of any part of the prosthetic components was 93.2% (95% confidence interval (CI) 86.1 to 100, number at risk 45). Consultant surgeons had a nine-year cumulative survival rate of 93.9% (95% CI 90.2 to 97.6, number at risk 16). Trainee surgeons had a cumulative nine-year survival rate of 93.0% (95% CI 90.3 to 95.7, number at risk 35). Although there was no differences in implant survival between consultants and trainees (p = 0.30), there was a difference in failure pattern whereby all re-operations performed for bearing dislocation (n = 7), occurred in the trainee group. This accounted for 0.6% of the entire cohort and 15% of the re-operations.
Conclusion
This is the largest single series of the Oxford UKA ever reported and demonstrates that good results can be achieved by a heterogeneous group of surgeons, including trainees, if performed within a high-volume centre with considerable experience with the procedure.
Cite this article: Bone Joint J 2016;(10 Suppl B):22–7.
The Oxford Partial Knee (Zimmer Biomet, Swindon, United Kingdom) is a unicompartmental knee arthroplasty (UKA) with a fully congruent mobile bearing that is designed to reduce wear and was first introduced in 1982. The designer surgeons report cumulative prosthetic survival rates of 98% (95% CI 93 to 100) at ten years in their original series1 and 96% (95% CI 92.5 to 99.5) ten-year survival for all implant related re-operations2 for the third phase of prosthesis. A semi-independent series report similarly good outcomes of up to 95% (95% CI 90.8 to 99.3) at ten years.3,4 However, independent single institution series from non-designer surgeons have produced less impressive results, with survival varying from between 83% to 90% at up to ten years.5-7 In addition, the increasing availability of registry data collected from large numbers of surgeons with wide ranging experience with the prosthesis report results varying from 84.9% to 92% survival at ten years.8-12 This has led to debate into the reasons for the variation in outcomes.13 A number of studies have identified the importance of the numbers of procedures per annum performed by individual surgeons or centres undertaking partial knee arthroplasty, suggesting that centres and surgeons who perform this type of surgery more often have better survival results.14,15 However, no previous study has investigated whether trainee surgeons, who may work in a high-volume centre but perform relatively few procedures themselves, can achieve good results.
The Nuffield Orthopaedic Centre is a high-volume teaching hospital unit performing approximately 300 UKAs each year. Surgeons in training perform a significant number of these procedures and we have never previously investigated the outcome of UKA performed by this group of surgeons and, in fact, the survival outcome of these patients has never been reported in the literature. Therefore, we have identified a cohort of patients with anteromedial knee arthritis16 operated by a cross-section of non-designer surgeons at the Nuffield Orthopaedic Centre. The specific aims of this project were to compare the ten-year survival of the prosthesis when performed by consultants and surgeons in training.
Patients and Methods
We identified 1084 knees in 947 consecutive patients who underwent Oxford UKA for anteromedial knee arthritis between 1998 and 2008 at the Nuffield Orthopaedic Centre. None of these patients had been included in previous survival analyses from our institution.
All patients were selected for surgery using the Oxford indications for this procedure;17 osteoarthritis producing severe or moderate pain that was unresponsive to non-operative care, bone-on-bone medial compartment changes, an intact anterior cruciate ligament and preserved full thickness cartilage in the lateral compartment. Age, obesity, chondrocalcinosis and patellofemoral degenerative changes were not contraindications to surgery.
Details of the operation were obtained from patients’ notes and the hospital electronic records system. We identified those patients who were operated on by surgeons of all grades who were not part of the prosthesis design team. Surgeons were then categorised as consultants or trainees. The trainee group consisted of Specialist Registrars who were undertaking an arthroplasty rotation at our hospital as a part of their Higher Surgical Training and Fellows who were undertaking an arthroplasty fellowship. Although there was wide variation in the level of experience in the trainee group, the Fellows would be expected to have had greater exposure to knee arthroplasty procedures than the Specialist Registrars. However, neither of these groups would have had a significant prior exposure to UKA.
Patients were contacted by post and the status of the UKA was determined. If further surgery had been performed in a hospital other than our centre, that unit was contacted and details of the surgery were requested. A formal review of the electronic operation record was performed for revision surgery at our hospital for each patient. If revision surgery was found to have taken place at the Nuffield Orthopaedic Centre, the notes were obtained and reviewed for the details of the procedure.
Patients who did not respond to the initial postal questionnaire were sent two further questionnaires by post and then were contacted by telephone. If no response regarding the status of the knee was received, their primary care physician was contacted and asked to review the primary care notes for any evidence of further surgery on the knee. If no data were available from the primary care physician, the patient was considered as lost to follow-up and the prosthesis was presumed to fail at either the day after the operation, or the day after the last date when the prosthesis was known to be in situ.18
Statistical analysis
Descriptive statistics were used to explore data. Cross-tabulation and the Pearson chi-squared tests were used for categorical data relating to revision rates between operations performed by consultants and trainees. All cause revision (defined as the removal or exchange of any part of the prosthetic components) was used as the endpoint for best-case survival analysis.19 A life table was constructed for each endpoint definition and survival rates up to ten years were determined. Patients who were lost to follow-up were treated as revisions. Life table survival plots were produced and a log-rank test was used to compare the two groups at nine years post-operatively, so that the number at risk at nine years would be a minimum of ten in each group. Statistical significance was defined as a p-value < 0.05. Statistical analysis was performed using STATA version 12 (Statacorp, College Station, Texas).
Results
Patient demographic details are reported in Table I. The mean patient age at time of surgery was 66.5 years (standard deviation (sd) 9.6). There was an almost equal distribution between male and female patients and side of operation. In all 814 patients had unilateral Oxford UKAs, and in 135 patients there were bilateral Oxford UKAs (although not simultaneously inserted). In total, 77 trainees performed 673 procedures (62.1%), with 13 consultants performing the remaining 411 (37.9%).
Table I
Patient demographic details
| Total number of patients/total number of knee implantations | 949/ 1084 |
|---|---|
| Mean age (yrs) (standard deviation) | 66.5 (9.6) |
| Gender (%) | Male 461 (48.6)/female 488 (51.4) |
| Side (%) | Right 538 (49.5)/left 546 (50.5) |
| Unilateral/bilateral (%) | 814 (85.8)/135 (14.2) |
| Surgeon grade (%) | Consultant 411 (37.9)/Trainee 673 (62.1%) |
| Deceased | 63 patients (79 knees) |
A further breakdown of cases performed by trainees stratified by their experience level and whether or not they were supervised by a consultant who was scrubbed at the time of surgery is presented in Table II. A total of 289 UKAs were performed by 49 Specialist Registrars, 159 (55%) of whom were directly supervised by a consultant. A total of 384 UKAs were performed by 28 Fellows, 162 (42.2%) of whom were directly supervised by a consultant. The median number of UKAs performed by Specialist Registrars was 3 (1 to 41) whilst the median number of procedures performed by Fellows was 7 (1 to 56).
Table II
Number of procedures performed by Fellows and Specialist Registrars with corresponding supervision and failure rate
| Experience level | Total number of UKA procedures performed | Mean number of procedures performed (range) | Number of supervised procedures with consultant scrubbed (%) | Number of failures (% of entire trainee cohort) |
|---|---|---|---|---|
| Specialist Registrar (n = 49) | 289 | 5.9 (1 to 41) | 159 (55) | 14 (2.1) |
| Fellow (n = 28) | 384 | 13.7 (1 to 56) | 162 (42.2) | 17 (2.5) |
| Total trainee cohort (n = 77) | 673 | 8.7 (1 to 56) | 321 (48) | 31 (4.6) |
-
UKA, unicompartmental knee arthroplasty
The mean follow-up was 5.2 years (1 to 12.7, sd 2.2). A total of 79 patients (7.3%) had died. Three patients (0.3%) were unable to be contacted and were therefore declared lost to follow-up. Of the remainder, in 936 (86.3%) the status of the knee was determined from the patient. In 143 (13.2%) the status was determined from the primary care physician.
There were 46 revisions (4.2%), the details of the indication are provided in Table III. A number of UKAs required further surgery without revision of any prosthetic components; 15 underwent exploratory arthroscopy with no further action, three underwent washout of wound and evacuation of haematoma, three manipulation under anaesthetic, one excision of wound neuroma and one open exploration for impingement.
Table III
Summary of revision procedures
| Reason for revision | n (% incidence) | Procedure | n |
|---|---|---|---|
| Aseptic loosening | 12 (1.1) | Revision toTKA/UKA | 10/2 |
| Lateral progression | 13 (1.2) | TKA/Lateral UKA | 8/5 |
| Infection | 7 (0.6) | DAIR with bearing exchange/TKA | 3/4 |
| Unexplained pain | 5 (0.4) | TKA | 5 |
| Bearing dislocation | 7 (0.6) | Bearing exchange only/conversion to TKA/conversion to fixed bearing tibia UKA | 4/2/1 |
| Fracture of tibia | 1 (0.1) | TKA | 1 |
| Unknown* | 1 (0.1) | TKA | 1 |
| Total | 46 (4.2) | 46 | |
-
* Reported by Primary Care Physician TKA, total knee arthroplasty; UKA, unicompartmental knee arthroplasty; DAIR, debridement antibiotics and implant retention
A total of 15 revisions occurred in the consultant group with a revision rate of 3.6%, compared with 31 and 4.7% in the trainee group. There was no significant difference in failure rate between the consultant and trainee group (p = 0.62, Pearson chi-squared). The mean time to revision for the consultant group was 3.8 years and 3.1 years for the trainee series. Comparing the pattern of failure between groups showed that all revisions for dislocation occurred in the trainee group.
Further subanalysis of the trainee group (Table II) showed that there were 14 failures in UKAs performed by Registrars (accounting for 2.1% UKAs performed by trainees) compared with 17 failures in UKAs performed by Fellows (accounting for 2.5% UKAs performed by trainees). There was no significant difference in failure rate between Registrars and Fellows (p = 0.89, Pearson chi-squared).
Analysis of failure rates in the trainee group showed that 17 of the failures occurred in cases where a consultant was scrubbed compared with 14 cases where the trainee was operating independently. This difference was not statistically significant (p = 0.65, Pearson chi-squared). The failure rate within the trainee group was also analysed based on the number of UKAs performed. Trainees who had performed fewer than ten UKAs had a failure rate of 5.1% (9 out of 193 UKAs) compared with a failure rate of 4.7% (22 out of 489 UKAs) in those who had undertaken more than ten UKAs. This difference was not statistically significant (p = 0.51, Pearson chi-squared).
The ten-year cumulative survival rate for revision or exchange of any part of the prosthetic components was 93.2% (95% CI 86.1 to 100, number at risk 45) with the survival table shown in Table IV. Consultant surgeons had a nine-year cumulative survival rate of 93.9% (95% CI 90.2 to 97.6, 3.7, number at risk 16) and trainee surgeons had a cumulative nine-year survival rate of 93.0% (95% CI 90.3 to 95.7, number at risk 35) (Fig. 1). There was no difference in survival between groups (p = 0.30, log rank).
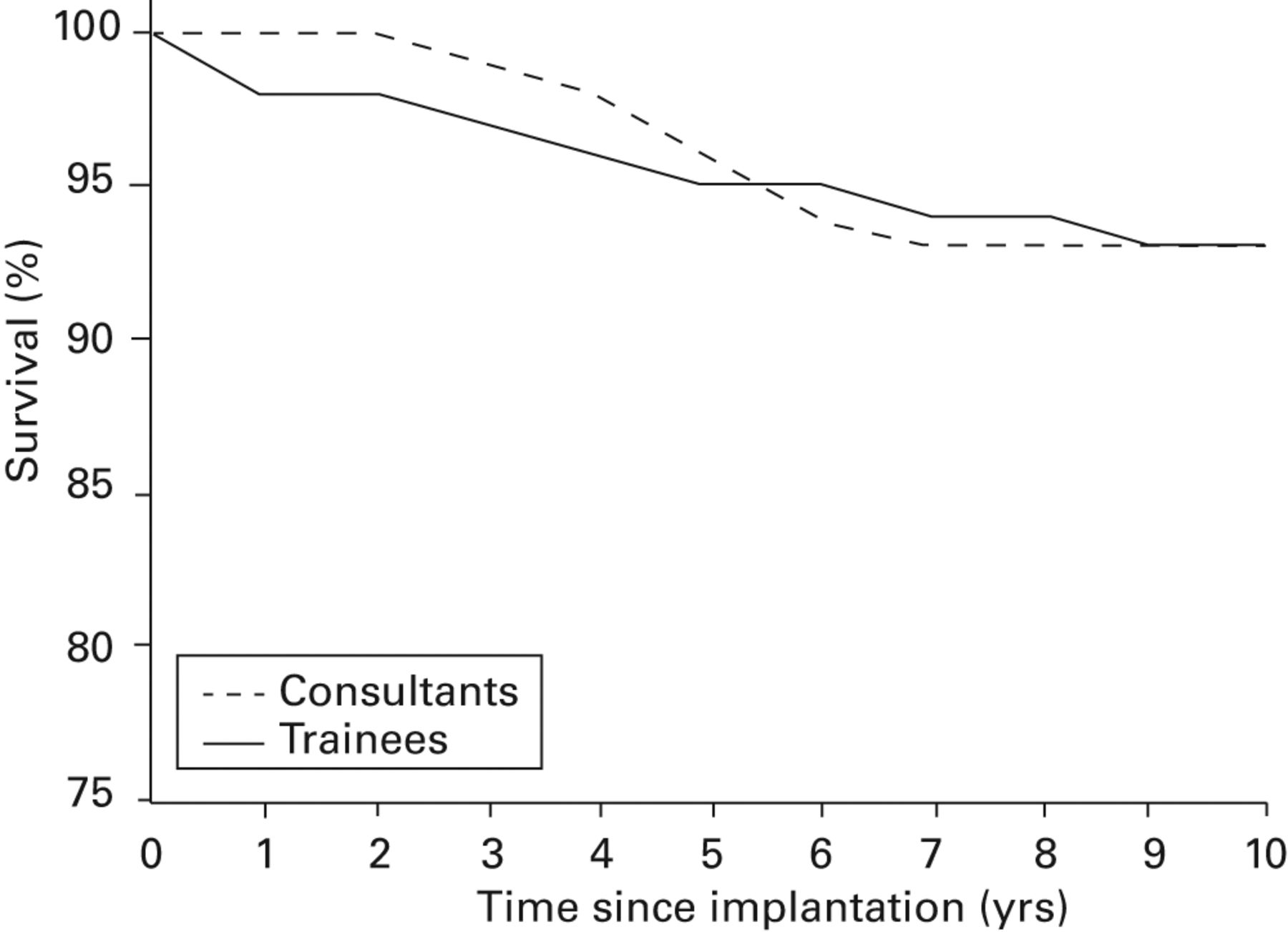
Fig. 1
Graph showing cumulative survival of implants over ten years, comparing consultants and trainees.
Table IV
Life table for whole cohort
| Post-operative yr | n | Failures | Successes | Number at risk | Cumulative survival % | 95% CI |
|---|---|---|---|---|---|---|
| 1 | 1084 | 13 | 4 | 1082.0 | 99.0 | 99.4 to 99.6 |
| 2 | 1067 | 6 | 17 | 1058.5 | 98.2 | 97.4 to 99.0 |
| 3 | 1044 | 8 | 134 | 977.0 | 97.4 | 96.4 to 98.4 |
| 4 | 902 | 6 | 198 | 803.0 | 96.7 | 95.5 to 97.9 |
| 5 | 698 | 8 | 176 | 610.0 | 95.4 | 93.8 to 97.0 |
| 6 | 514 | 3 | 106 | 461.0 | 94.8 | 92.8 to 96.8 |
| 7 | 405 | 4 | 148 | 331 | 93.7 | 91.2 to 96.2 |
| 8 | 253 | 1 | 126 | 190 | 93.2 | 89.7 to 96.7 |
| 9 | 126 | 0 | 59 | 96.5 | 93.2 | 88.3 to 98.1 |
| 10 | 67 | 0 | 44 | 45.0 | 93.2 | 86.1 to 100 |
| 11 | 23 | 0 | 23 | 11.5 | 93.2 | 79.1 to 100 |
-
CI, confidence interval
Discussion
This ten-year survival analysis of 1084 knees from the Nuffield Orthopaedic Centre, but not including procedures performed by the designer surgeons, represents the largest single series of Oxford UKAs in the literature. None of the patients in this series have been included in previous reports of outcome for the Oxford UKA. We report a cohort of 1084 UKAs inserted by 90 different surgeons of different grades. Using revision of any component as failure, we identify a predicted survival of 93.2% (95% CI 86.1 to 100, number at risk 45) at ten years, with 46 requiring revision of one component or more. There was no difference in predicted survival at nine years between those procedures performed by consultants and those performed by trainees.
Although previous studies have evaluated the impact of surgeon grade on the long-term outcome of total hip20,21 and total knee arthroplasty,22 to our knowledge, this is the first study which attempts to evaluate the long-term outcome of UKAs performed by trainees. In keeping with the aforementioned studies, our findings suggest that with appropriate training and supervision, trainee surgeons can achieve similar results to experienced consultants during UKA.
In 1998 Murray, Goodfellow and O’Connor1 reported a cumulative survival rate at ten years of 98% (95% CI 93 to 100) for a cohort of 143 knees undergoing the Oxford UKA. Subsequently, in a cohort of 1000 patients at ten years for the third phase prosthesis, they described a 96% (95% CI 92.5 to 99.5) cumulative survival rate.2 In a series from Skovde, Price, Waite and Svärd3 described ten- and 15-year survival of 95% (95% CI 90.8 to 99.3) and 94% (95% CI 83.1 to 100), respectively, with successful clinical results at ten years. However, these results have not been reproduced in all series and in particular joint registers have shown higher rates of revision.8-10 The Swedish Knee Arthroplasty Registry has previously identified that the numbers performed by a centre can significantly affect the survival of partial knee arthroplasty, with those centres performing over 23 a year outperforming centres undertaking fewer.21 More recently, published data have been identified which reveal for individual surgeons performing more than approximately 15 partial knee arthroplasties a year, the revision rates are improved compared with those undertaking fewer.15 As a result, this has raised issues about the minimum number of procedures that should be performed a year if surgeons undertake partial knee arthroplasty.23,24 In light of this, the training of younger surgeons to undertake partial knee arthroplasty becomes an issue. To our knowledge this is the first study to compare directly the long-term survival results from consultants and trainees within a single unit and we have demonstrated that good results can be achieved from multiple surgeons of differing potential ability and experience. Consistency has been achieved in that all procedures were performed in a recognised centre of excellence for the procedure performing well over 23 UKAs per year. The centre has well-established training, focusing on indications and insertion techniques. This enables trainees to undertake independent UKA procedures with seemingly no detrimental effect on revision rates, as demonstrated by the findings of the current study. In addition, theatre personnel are familiar with the procedure and ward rehabilitation and physiotherapy post-operatively follows a structured and established course. The lack of difference in failure rates between trainees performing fewer than ten UKAs and those performing more than ten UKAs may be explained by the multi-disciplinary expertise of the unit as a whole and the training philosophy. Similarly, as previously suggested,14 indications for revision procedures in this hospital may be different for others, leading to a lower revision of prosthetic components. While trainees are likely to be still on the learning curve of expertise for performing this procedure, the current study indicates that despite this, they can still expect to have good survival.
When analysing prosthetic failure modes within this study, the two most common overall causes of revision, namely aseptic loosening and lateral compartment progression, were similar to those found in the existing literature.25 However, a closer look at the bearing dislocation rate shows that all seven dislocations (15% of all re-operations) occurred following operations performed by trainees. This mode of failure is often regarded as a marker for technical proficiency during the Oxford UKA due to factors such as damage to the medial collateral ligament, impingement from osteophytes, flexion/extension gap imbalance and component malpositioning which results in a wide gap between the tibial and femoral components.26-28 Our teaching philosophy is to emphasise the risk of such errors to our trainees – this is reflected by the very low overall dislocation rate of 0.6% in this series which compares favourably with a pooled dislocation rate of 1.5% reported for the Oxford UKA in a recent systematic review.29 Furthermore, the failures in the current study, which tended to occur within the first two years of surgery, did not adversely affect the long-term survival when comparisons were made between trainees and consultants.
This study has some strengths and weaknesses. This series is the largest series of Phase III Oxford medial UKA to ever be reported from a single centre. Despite being a retrospectively identified cohort, the loss to follow-up in this series is only 0.3%. In 13.2% of all cases, status details were obtained from their primary care physician, however, this is felt to be acceptable given the length of follow-up and volume of cases. It would have been desirable to undertake a similar analysis for total knee arthroplasties performed at our institution for comparison, however, these data were not available and the main focus of the study was to determine outcome and survival in UKAs in a high-volume centre with expertise in UKA training. A major strength of the paper is the collection of data across the full spectrum of surgeons performing Oxford medial UKA at the centre, rather than a few highly selected surgeons. This means the results may represent a truer reflection of the success within the population.
In conclusion, this is the largest ten-year follow up of the Oxford UKA ever reported. Whilst we are aware of the issues of bias given its origin from the inventing centre, this series involves over 90 individual surgeons of varying experience and expertise, with none being part of the designer team. The survival of 93.2% at ten years is likely to result from a standardised approach to surgery with strict indications for the operation and a uniform threshold for revision. Within this framework of care, good results with the Oxford UKA can be achieved by a heterogeneous group of consultant and trainee surgeons.
Take home message: This is the largest ten-year follow up of the Oxford UKA ever reported. Within this framework of care, good results with the Oxford UKA can be achieved by a heterogeneous group of Consultant surgeons and trainees.
1 Murray DW , GoodfellowJW, O’ConnorJJ. The Oxford medial unicompartmental arthroplasty: a ten-year survival study. J Bone Joint Surg [Br]1998;80-B:983–989.CrossrefPubMed Google Scholar
2 Pandit H , JenkinsC, GillHS, et al.Minimally invasive Oxford phase 3 unicompartmental knee replacement: results of 1000 cases. J Bone Joint Surg [Br]2011;93-B:198–204.CrossrefPubMed Google Scholar
3 Price AJ , WaiteJC, SvärdU. Long-term clinical results of the medial Oxford unicompartmental knee arthroplasty. Clin Orthop Relat Res2005;435:171–180.CrossrefPubMed Google Scholar
4 Price AJ , DoddCA, SvärdUG, MurrayDW. Oxford medial unicompartmental knee arthroplasty in patients younger and older than 60 years of age. J Bone Joint Surg [Br]2005;87-B:1488–1492.CrossrefPubMed Google Scholar
5 Kort NP , van RaayJJ, CheungJ, JolinkC, DeutmanR. Analysis of Oxford medial unicompartmental knee replacement using the minimally invasive technique in patients aged 60 and above: an independent prospective series. Knee Surg Sports Traumatol Arthrosc2007;15:1331–1334.CrossrefPubMed Google Scholar
6 Lyons MC , MacDonaldSJ, SomervilleLE, NaudieDD, McCaldenRW. Unicompartmental versus total knee arthroplasty database analysis: is there a winner?Clin Orthop Relat Res2012;470:84–90.CrossrefPubMed Google Scholar
7 Parratte S , PaulyV, AubaniacJM, ArgensonJN. No long-term difference between fixed and mobile medial unicompartmental arthroplasty. Clin Orthop Relat Res2012;470:61–68.CrossrefPubMed Google Scholar
8 Sundberg M , LidgrenL, W-DahlA, RobertssonOThe Swedish Knee Arthroplasty Register. Annual Report, 2011. http://www.myknee.se/pdf/115_SKAR2011_Eng1.0.pdf (date last accessed 1 August 2016). Google Scholar
9 New Zealand Orthopaedic Association. The New Zealand Joint Registry. January 1999 To December 2009. Eleven Year Report, 2009. http://nzoa.org.nz/system/files/NJR%2011%20Year%20Report%20Jan%2099%20-%20Dec%2009.pdf (date last accessed 1 August 2016). Google Scholar
10 Australian Orthopaedic Association. National Joint Replacement Registry. Hip and Knee Arthroplasty Annual Report, 2011. https://aoanjrr.sahmri.com/documents/10180/44800/Annual%20Report%202011?version=1.2& t=1347337258367 (date last accessed 1 August 2016). Google Scholar
11 Vorlat P , PutzeysG, CottenieD, et al.The Oxford unicompartmental knee prosthesis: an independent 10-year survival analysis. Knee Surg Sports Traumatol Arthrosc2006;14:40–45.CrossrefPubMed Google Scholar
12 Baker PN , PetheramT, JamesonSS, et al.Comparison of patient-reported outcome measures following total and unicondylar knee replacement. J Bone Joint Surg [Br]2012;94-B:919–927.CrossrefPubMed Google Scholar
13 Labek G , SekyraK, PawelkaW, JandaW, StöcklB. Outcome and reproducibility of data concerning the Oxford unicompartmental knee arthroplasty: a structured literature review including arthroplasty registry data. Acta Orthop2011;82:131–135.CrossrefPubMed Google Scholar
14 Liddle AD , PanditH, JudgeA, MurrayDW. Effect of Surgical Caseload on Revision Rate Following Total and Unicompartmental Knee Replacement. J Bone Joint Surg [Am]2016;98:1–8.CrossrefPubMed Google Scholar
15 Robertsson O , KnutsonK, LewoldS, LidgrenL. The routine of surgical management reduces failure after unicompartmental knee arthroplasty. J Bone Joint Surg [Br]2001;83-B:45–49.CrossrefPubMed Google Scholar
16 White SH , LudkowskiPF, GoodfellowJW. Anteromedial osteoarthritis of the knee. J Bone Joint Surg [Br]1991;73-B:582–586. Google Scholar
17 Goodfellow J , O’ConnorJ, DoddCAF, MurrayDW Unicompartmental arthroplasty with the Oxford Knee. New York: Oxford University Press, 2006. Google Scholar
18 Murray DW , BrittonAR, BulstrodeCJ. Loss to follow-up matters. J Bone Joint Surg [Br]1997;79-B:254–257.CrossrefPubMed Google Scholar
19 Murray DW , CarrAJ, BulstrodeC. Survival analysis of joint replacements. J Bone Joint Surg [Br]1993;75-B:697–704.PubMed Google Scholar
20 Reidy MJ , FaulknerA, ShitoleB, CliftB. Do trainee surgeons have an adverse effect on the outcome after total hip arthroplasty?: a ten-year review. Bone Joint J2016;98-B:301–306.CrossrefPubMed Google Scholar
21 Palan J , GulatiA, AndrewJG, et al.The trainer, the trainee and the surgeons’ assistant: clinical outcomes following total hip replacement. J Bone Joint Surg [Br]2009;91-B:928–934. Google Scholar
22 Beattie N , MaempelJ, RobertsS, BrownG, WalmsleyP. Supervised registrar-performed surgery does not adversely affect medium-term function outcomes following total knee replacement. Bone Joint J2016;98-B(Supp 12):3. Google Scholar
23 Briggs T Getting it right first time: a national review of adult elective orthopaedic services in England: http://www.boa.ac.uk/pro-practice/getting-it-right-first-time/ (date last accessed 1 August 2016). Google Scholar
24 Liddle AD , PanditH, JudgeA, MurrayDW. Optimal usage of unicompartmental knee arthroplasty: a study of 41,986 cases from the National Joint Registry for England and Wales. Bone Joint J2015;97-B:1506–1511.CrossrefPubMed Google Scholar
25 van der List JP , ZuiderbaanHA, PearleAD. Why Do Medial Unicompartmental Knee Arthroplasties Fail Today?J Arthroplasty2016;31:1016–1021.CrossrefPubMed Google Scholar
26 Song MH , KimBH, AhnSJ, YooSH, LeeMS. Early complications after minimally invasive mobile-bearing medial unicompartmental knee arthroplasty. J Arthroplasty2009;24:1281–1284.CrossrefPubMed Google Scholar
27 Goodfellow JW , O’ConnorJ, DoddCAF, MurrayDW Unicompartmental arthroplasty with the Oxford knee . Oxford: Oxford University Press, 2006:117–128. Google Scholar
28 Bozkurt M , AkmeseR, CayN, et al.Cam impingement of the posterior femoral condyle in unicompartmental knee arthroplasty. Knee Surg Sports Traumatol Arthrosc2013;21:2495–2500.CrossrefPubMed Google Scholar
29 Kim SJ , PostigoR, KooS, KimJH. Causes of revision following Oxford phase 3 unicompartmental knee arthroplasty. Knee Surg Sports Traumatol Arthrosc2014;22:1895–1901.CrossrefPubMed Google Scholar
Author contributions:
N. Bottomley: Study protocol, Data collection, Data analysis, Writing the manuscript.
L. D. Jones: Study protocol, Data collection, Data analysis, Writing the manuscript.
R. Rout: Study protocol, Data collection, Critical appraisal of manuscript.
A. Alvand: Study protocol, Data analysis, Writing the manuscript.
I. Rombach: Data analysis, Critical appraisal of manuscript.
T. Evans: Data collection, Critical appraisal of manuscript.
W. F. M. Jackson: Study protocol, Performing surgeries, Critical appraisal of manuscript.
D. J. Beard: Study protocol, Data analysis, Critical appraisal of manuscript.
A. J. Price: Study protocol, Performing surgeries, Data analysis, Writing the manuscript.
This is an open-access article distributed under the terms of the Creative Commons Attributions licence (CC-BY-NC), which permits unrestricted use, distribution, and reproduction in any medium, but not for commercial gain, provided the original author and source are credited.
The author or one or more of the authors have received or will receive benefits for personal or professional use from a commercial party related directly or indirectly to the subject of this article. In addition, benefits have been or will be directed to a research fund, foundation, educational institution, or other non- profit organisation with which one or more of the authors are associated.
This study has been supported by the NIHR Biomedical Research Unit into Musculoskeletal Disease, Nuffield Orthopaedic Centre and the University of Oxford.
This article was primary edited by G. Scott.









