Abstract
Aims
Medial unicompartmental knee arthroplasty (UKA) is associated with successful outcomes in carefully selected patient cohorts. We hypothesised that severity and location of patellofemoral cartilage lesions significantly influences functional outcome after Oxford medial compartmental knee arthroplasty.
Patients and Methods
We reviewed 100 consecutive UKAs at minimum eight-year follow-up (96 to 132). A single surgeon performed all procedures. Patients were selected based on clinical and plain radiographic assessment. All patients had end-stage medial compartment osteoarthritis (OA) with sparing of the lateral compartment and intact anterior cruciate ligaments. None of the patients had end-stage patellofemoral OA, but patients with anterior knee pain or partial thickness chondral loss were not excluded. There were 57 male and 43 female patients. The mean age at surgery was 69 years (41 to 82). At surgery the joint was carefully inspected for patellofemoral chondral loss and this was documented based on severity of cartilage loss (0 to 4 Outerbridge grading) and topographic location (medial, lateral, central, and superior or inferior). Functional scores collected included Oxford Knee Score (OKS), patient satisfaction scale and University College Hospital (UCH) knee score. Intraclass correlation was used to compare chondral damage to outcomes.
Results
All patients documented significant improvement in pain and improved functional scores at mid-term follow-up. There were four revisions (mean 2.9 years, 2 to 4; standard deviation (sd) 0.9) in this cohort, three for tibial loosening and one for femoral loosening. There was one infection that was treated with debridement and insert exchange. The mean OKS improved from 23.2 (sd 7.1) to 39.1 (sd 6.9); p < 0.001. The cohort with central and lateral grade 3 patellofemoral OA documented lower mean satisfaction with pain (90, sd 11.8) and function (87.5, sd 10.3) on the patient satisfaction scale. On the UCH scale, patients reported significantly decreased mean overall scores (7.3, sd 1.2 vs 9, sd 2.3) as well as stair climb task (3.5, sd 0.3 vs 5, sd 0.1) when cartilage lesions were located centrally or laterally on the PFJ. Patients with medial chondral PFJ lesions behave similar to patients with no chondral lesions.
Conclusion
Topographical location and severity of cartilage damage of the patella can significantly influence function after successful Oxford medial UKA. Surgeons should factor this in when making their operative decision, and undertake to counsel patients appropriately.
Cite this article: Bone Joint J 2016;98-B(10 Suppl B):11–15.
Unicompartmental knee arthroplasty (UKA) is any accepted surgical option for treating anteromedial osteoarthritis (OA) of the knee with good long-term results and high patient satisfaction.1-4 Patient selection for this procedure continues to be debated.5-8 Recent literature has focused on the role of patellofemoral OA on outcomes after medial OA. Neither anterior knee pain nor radiologically-demonstrated medial patellofemoral joint degeneration is considered a contraindication to Oxford UKA (Biomet, Bridgend, United Kingdom).9 However, management of severe arthritis of the lateral facet of the patella remains controversial and UKA is not considered to be an appropriate choice of surgery in this setting.10,11 Some authors have argued that lateral patellar subluxation12 is a poor predictor of outcome, irrespective of cartilage loss.11,12 The suitability of plain radiographs in identifying patellar cartilage lesions is also debated, with some authors recommending MRI assessment of the patellofemoral joint in the presence of anterior knee pain13 when selecting patients for medial UKA.
We believe that most surgeons offer UKA for predominantly anteromedial OA of the knee based on history, examination and radiographic assessment. We also believe that in the presence of obvious lateral tibiofemoral or lateral patellofemoral OA, surgeons err towards a total knee arthroplasty. There is however, a paucity of literature that will guide the surgeon with intra-operative decision making when faced with patellofemoral cartilage lesions during UKA for carefully selected anteromedial OA.
We hypothesised that the location and severity of the cartilage lesion involving the patellofemoral joint (PFJ) will influence functional outcome and patient satisfaction after medial UKA. Our aim was to investigate any link between medial and lateral PFJ cartilage lesions and its influence on satisfaction and outcome after medial UKA in order to help the surgeon with intra-operative decision making.
Patients and Methods
We prospectively reviewed a cohort of 100 consecutive UKAs in 100 patients (57 men, 43 women; mean age at surgery 69 years; 41 to 82) performed by a single senior surgeon (FSH) between 2002 and 2007. All patients underwent a medial Oxford UKA. Their mean body mass index (BMI) was 27.3kg/m2 (22 to 36.4).
All patients had symptomatic medial knee pain with end stage OA on weight-bearing anteroposterior (AP) and lateral radiographs (Outerbridge grades 3 and 414 – bone-on- bone on standing radiographs). Patients also showed sparing of the lateral compartment on radiographs and this was confirmed on history and examination. None of the patients had radiographic evidence of grade 4 OA (Outerbridge) at the PFJ on the skyline view radiograph. Anterior knee pain in itself was not an exclusion criterion in the absence of grade 3 or 4 changes on plain radiographs.
UKA was not undertaken in the presence of gout or inflammatory arthritis. Pre-operative varus, fixed flexion more than 20° or a fixed varus deformity, were also excluded.
All patients received 1.5 g cefuroxime intravenously at induction and two further doses of 750 mg post-operatively. A tourniquet was inflated only during cementing of the prosthesis. A mini-incision medial-parapatellar approach was used in all cases. The patella was pushed/subluxed laterally, but not everted. Tibial and femoral preparation was undertaken according to the manufacturer’s technical manual. The joint was carefully inspected to confirm a lack of lateral joint OA and to document the cartilage changes at the PFJ. Any cartilage loss at the PFJ was documented using the modified Outerbridge classification (0 to 4). Grade 0 was normal cartilage, grade1 was softening and swelling of the articular cartilage, grade 2 was a partial-thickness cartilage defect with fissures not reaching subchondral bone, grade 3 had fissures and fragmentation to subchondral bone, and grade 4 was exposed subchondral bone. The topographical location of the cartilage loss (trochlea or patella) was documented as medial, central or lateral and superior and inferior.
The mean hospital stay was 3.1 nights (2 to 6). Patients were followed-up at six weeks, six months and then annually. Weight-bearing AP, lateral and skyline radiographs were obtained at each follow-up visit.
Outcome measures
Pre-operatively and at follow-up, the following outcome measures were collected: Oxford Knee Score (OKS),15 patient satisfaction scale,16 anterior knee pain documented on visual analogue scale (VAS) and University College Hospital (UCH) knee score.17 Outcome measures at the latest follow-up were used for analysis in this study. For comparison of outcomes, patients were divided into two groups; group 1 had severe chondral lesions (grade 3, 4) in the central or lateral PFJ; group 2 included all the other patients.
The senior author (FSH) undertook radiographic assessment at follow-up. Images stored on PACS electronically were reviewed and PACS measurement tools were used for all assessments. All patients had standing weight-bearing AP radiographs as well as lateral and skyline views. Alignment and progression of lateral or PFJ OA was documented. Aligment was measured on weight-bearing AP radiographs so as to document overall knee varus or valgus attitude, as well as implant varus or valgus position. Lateral radiographs were used to document tibial slope and femoral flexion. Skyline views were used to document PFJ OA.
Statistical analysis
All values were expressed as means, range and standard deviations (sd). Pre- and post-operative scores were compared using non-parametric (Mann-Whitney U test) measures. Correlation between chondral damage and functional scores were documented using Intraclass correlation coefficient (ICC) with 95% confidence intervals (CI). A p-value < 0.05 was considered to be statistically significant.
Results
The mean follow-up was ten years (8 to 13, median ten years). All patients documented significant improvement in pain and improved functional scores, which was sustained at the minimum eight-year follow-up. The OKS improved from 23.2 (sd 7.1) to 39.1 (sd 6.9); (p < 0.001).
A total of 52 knees had grade 3 or 4 cartilage lesions documented at surgery. In ten patients, no cartilage lesions were found at operation. On the patella there were 12 isolated lateral lesions (18 combined) and ten isolated medial defects (64 combined). On the trochlea, the distribution was as follows: 11 isolated central trochlea (combined 53); 12 isolated lateral lesions (combined 17); 12 isolated medial chondral lesions (combined 53). Table I provides the distribution of cartilage lesions in 100 patients.
Table I
Distribution of cartilage lesions in our study population
| Cartilage grade; location | n | ||
|---|---|---|---|
| Patella | Grade 4 | Grade 3 | Grade 2 |
| Medial | 27 | 21 | 26 |
| Lateral | 4 | 8 | 18 |
| Trochlea | |||
| Central | 11 | 18 | 35 |
| Lateral | 5 | 7 | 17 |
| Medial | 12 | 21 | 32 |
A total of 18 patients reported severe anterior knee pain and persistent anteromedial pain. This resolved completely by 18 months’ follow-up.
There were four revisions in this cohort, three for tibial loosening and one for femoral loosening at a mean of 2.9 years (2 to 4, sd 0.9) from surgery. Radiographs did not show any malalignment of the implants in these four cases. There was one infection at six months that was salvaged with debridement and insert exchange. The revisions were not included in the review of chondral lesions and were excluded from the study.
Table II summarises the OKS, VAS and satisfaction score at minimum eight-year follow-up in those with intra-operative severe PFJ chondral damage (grades 3/4) in central and lateral compartments compared with those with mild or moderate PFJ OA (grades 0/1/2).
Table II
Comparison of mid-term outcomes in Lateral/ Central patellofemoral joint (PFJ) versus Grade 0/1/2 PFJ lesions. Mean values with standard deviations (Mann-Whitney U test)
| Grade 3/4 lateral/central PFJ | Grade 0/1/2 PFJ | p-value | |||||
|---|---|---|---|---|---|---|---|
| Pre-operative | Post-operative | Pre-operative | Post-operative | ||||
| OKS | 23.7 (8.2) | 39.6 (7.5) | 24.2 (8.1) | 40.0 (7.1) | p = 0.21 | ||
| VAS | 8.9 (1.2) | 3.2 (1.1) | 9.0 (1.2) | 1.1 (1.5) | p = 0.42 | ||
| Satisfaction (pain) | - | 90 (11.8) | - | 99 (5.1) | p = 0.01 | ||
| Satisfaction (function) | - | 87.5 (10.3) | - | 99 (4.3) | p = 0.02 | ||
| UCH Knee Score (performance function) | - | 27.5 (5.3) | - | 33 (6.1) | p = 0.01 | ||
| UCH Knee Score (performance pain) | - | 7.3(1.2) | - | 9 (2.3) | p < 0.001 | ||
| Step stair climb (performance function) | - | 3.5 (0.3) | - | 5 (0.1) | p < 0.001 | ||
| Step stair climb (performance pain) | - | 7 (1.1) | - | 10 (1) | p < 0.001 | ||
| Demographics | |||||||
| n | 29 | 58 | |||||
| Mean age (range) yrs | 70 (52 to 80) | 67 (41 to 79) | |||||
| Gender | 18 M/11F | 36 M/22F | |||||
| Mean body mass index (range) kg/m2 | 26 (22 to 35) | 29 (21 to 32) | |||||
-
OKS, Oxford Knee Score; VAS, visual analogue score for anterior knee pain; UCH score, University College Hospital score for anterior knee pain
A statistically significant lower function on the stairs component of UCH score, overall UCH score, and higher pain measured using VAS and UCH knee score (pain component) were noted in those with grade 3/4 lateral PFJ changes (Table II). Figures 1 and 2 illustrate a lateral chondral lesion in the PFJ that was treated with a medial UKA. A high correlation ICC was noted between presence of chondral lesions and OKS (ICC 0.79, 95% CI 0.68 to 0.81), patient satisfaction (ICC 0.8, 95% CI 0.78 to 0.88), UCH knee score (ICC 0.79, 95% CI 0.68 to 0.84) and step stair function of UCH knee score (ICC 0.7, 95% CI 0.69 to 0.89).
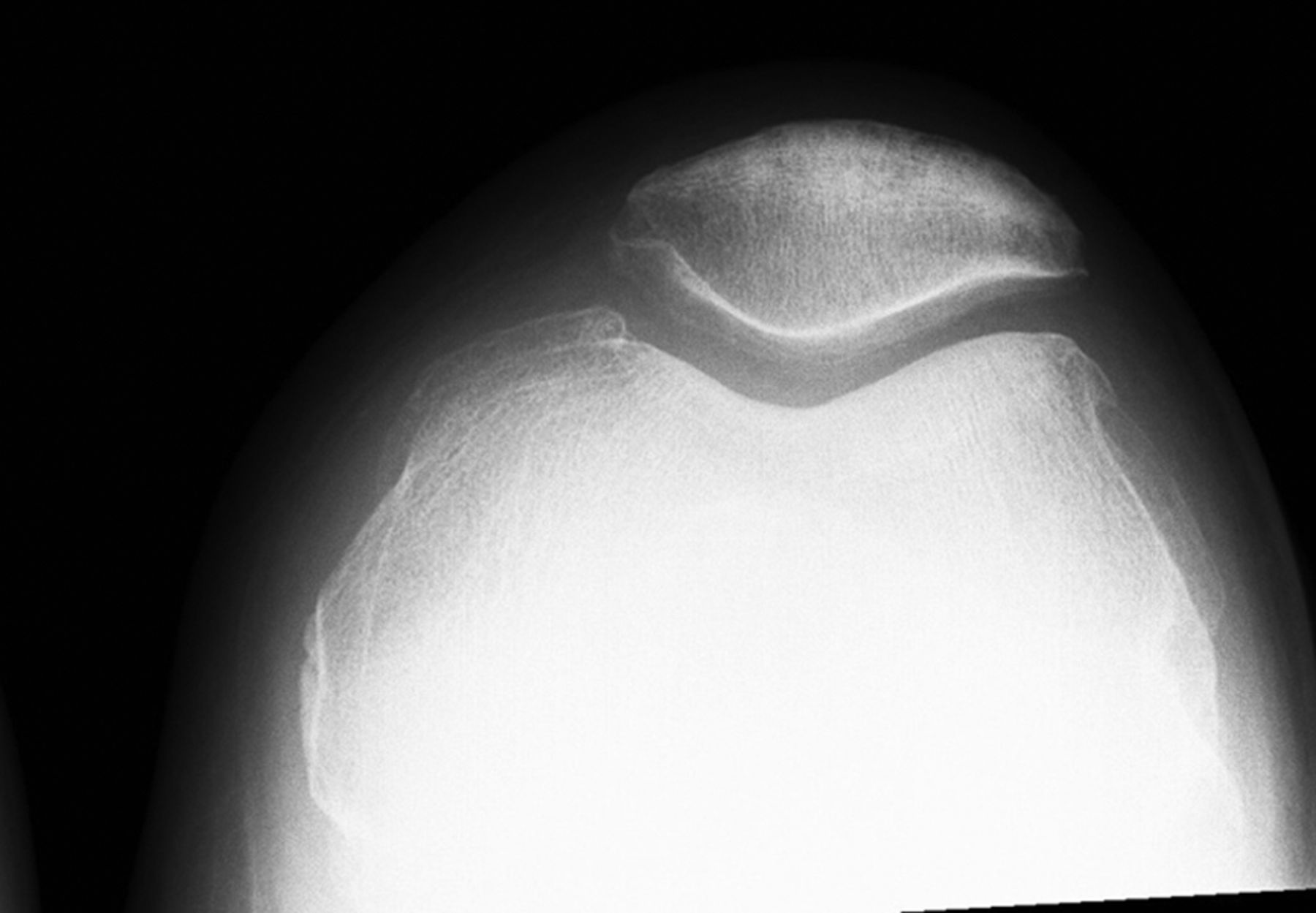
Fig. 1
Pre-operative radiograph of lateral chondral lesion in the patellofemoral joint that was treated with a medial unicompartmental arthroplasty.

Fig. 2
Post-operative radiograph lateral chondral lesion in the patellofemoral joint that was treated with a medial unicompartmental arthroplasty at latest follow-up.
Table III compares the OKS, VAS and satisfaction score at minimum eight-year follow-up in those with medial PFJ chondral damage in the cohort with no or minimal chondral damage documented intra-operatively. No significant difference was noted between patients who had medial lesions and those without any PFJ cartilage lesions or minimal cartilage damage (grade 1) found intra-operatively. Figures 3 and 4 illustrate an example of medial patellar cartilage lesion before and after medial unicompartmental arthroplasty.

Fig. 3
Pre-operative radiograph of medial patellar cartilage lesion that was treated with a medial unicompartmental arthroplasty.

Fig. 4
Post-operative radiograph of medial patellar cartilage lesion treated with medial unicompartmental arthroplasty at latest follow-up.
Table III
Comparison of mid-term outcomes in medial patellofemoral joint (PFJ) versus no or minimal PFJ lesions
| Medial PFJ | Grade 0/1 chondral lesion | p-value | |||
|---|---|---|---|---|---|
| Pre-operative | Post-operative | Pre-operative | Post-operative | ||
| OKS | 23.2 (7.1) | 40.0 (6.6) | 24.0 (5.6) | 40.0 (7.1) | p = 0.3 |
| VAS | 9.0 (1.5) | 1 (0.5) | 9.0 (1.2) | 1.1 (1.4) | p = 0.6 |
| Satisfaction (pain) | - | 98 (10.6) | - | 99 (7.3) | p = 0.5 |
| Satisfaction (function) | - | 99 (8.3) | - | 99 (2.3) | p = 0.21 |
| UCH Knee Score (performance function) | - | 32.9 (7.3) | - | 33.1 (5.1) | p = 0.3 |
| UCH Knee Score (performance pain) | - | 8.9 (1.0) | - | 9 (1.3) | p = 0.4 |
| Step stair climb (performance function) | - | 4.9 (0.5) | - | 5 (0.3) | p = 0.5 |
| Step stair climb (performance pain) | - | 9.1 (1.1) | - | 10 (1) | p = 0.6 |
| Demographics | |||||
| n | 49 | 28 | |||
| Mean age (range) yrs | 68 (48 to 79) | 71 (59 to 80) | |||
| Gender | 28 M/21F | 13M/15F | |||
| Mean body mass index kg/m2 (range) | 30 (27 to 33) | 29 (25 to 35) | |||
-
OKS, Oxford Knee Score; VAS, visual analogue score for anterior knee pain; UCH score, University College Hospital score for anterior knee pain
Radiographic analysis at early follow-up confirmed satisfactory alignment and this was maintained at latest follow-up. Four patients presented after 24 months follow-up with symptomatic restriction of function and pain, and were noted to have implant loosening. None of the patients had pre-operative lateral compartment or PFJ OA and no progression was noted in this series at latest follow-up.
Discussion
In our study of a 100 consecutive UKA for predominantly anteromedial OA of the knee, we have shown improved patient satisfaction and functional outcome with Oxford UKA. We noted a high correlation between decreased patient satisfaction and presence of central or lateral grade 3 cartilage lesions. Presence of medial PFJ chondral lesions did not seem to influence the outcome. Patient-reported outcome measures (OKS), as well as functional task-based scores, confirmed this association.
Our study has several limitations. First it does not compare two cohorts of patients randomised to two groups based on their PFJ cartilage loss. This would require arthroscopic or MRI assessment of all patients and larger numbers. This is not our routine practice and we believe that patient selection for medial UKA should be based on history, examination and radiographic assessment. As shown by this study, arthrotomy and assessment of the knee compartments during surgery provide valuable information and help decision making before proceeding to UKA. Secondly, the patients with more severe lateral cartilage lesions may also differ in demographics and knee biomechanics to the cohort with normal PFJ cartilage. These factors need to be considered when interpreting the results of this study. However, despite these drawbacks, we believe that our study presents a pragmatic view of medial UKA outcomes and helps the surgeon with decision making, as well as pre- and post-operative patient counselling.
Other studies have highlighted the role of PFJ OA on outcome after medial UKA,10,11,18 Our study adds to this knowledge and in addition has looked at the topographical location of the cartilage lesion as well as the grade of cartilage loss in greater detail. We also present the mid-term follow-up results compared with early results presented by most studies.1-3 It is not clear from our study why lateral cartilage lesions are less well tolerated. However, this may be because medial UKA does not adequately address the biomechanics of the lateral patella. It may also be that presence of lateral PFJ lesions is an indicator for more extensive disease.
Our results demonstrated sustained pain relief and excellent knee scores at mid-term follow-up. The presence of patellar chondral lesions was associated with early persistent anterior knee pain, however, this seemed to resolve by the 18-month follow-up. Patients need to be given counselling in this regard. Presence of lateral or central PFJ chondral lesions was associated with decreased knee score and function. Beard et al10 studied the influence of anterior knee pain or radiological evidence of PFJ OA on the patient-reported outcome of Oxford medial UKA. They found that patients with medial patellofemoral degeneration had a similar outcome to those without such degeneration. For some outcome measures patients with lateral patellofemoral degeneration had a worse score than those without, but these patients still had a good outcome. Pongcharoen and Reutiwarangkoon18 compared patients with and without severe arthritis of the lateral facet of the patella following mobile-bearing UKA. They found that anterior knee pain, pain scores, and functional scores were not different between the two groups following a medial Oxford UKA. However, the knee scores of patients with severe arthritis of the lateral facet were worse than those in patients without severe arthritis of the lateral facet of the patella. Song et al11 compared the outcomes of patients with or without PFJ OA who underwent medial UKA. At median follow-up of 5.4 years (3.1 to 10.2), no significant inter-group difference was found in terms of anterior knee pain, Hospital for Special Surgery score, or range of movement. It is possible that their outcome scores were not sufficiently sensitive to demonstrate any difference in PFJ-specific knee pain. In our series, we noticed that the OKS was comparable, but UCH score and stair climb task demonstrated a significant difference. Munk et al12 investigated the importance of PFJ degeneration and the location of pre-operative knee pain for the early favourable outcome of UKA. At one-year follow-up they observed that lateral subluxation of the patella and the pre-operative OKS was a predictor of poor outcome. Full-thickness cartilage loss at any location gave a similar outcome to that with a normal or near-normal joint surface. However, multiple surgeons were involved and routine skyline radiographs were not obtained and severe PFJ OA was not excluded from the series. Our study differs from that of Munk et al12 in that a single surgeon performed all procedures and documented the cartilage lesions. Patients with end-stage PFJ OA were not included in our study group.
In conclusion, topographical location and severity of cartilage damage of the patella can significantly influence function after successful Oxford medial UKA. Surgeons should factor this in their decision making and advise patients appropriately.
Take home message: Lateral PFJ cartilage lesions can negatively influence the outcome of medial UKA, however medial PFJ cartilage lesions are well tolerated.
1 Murray DW , GoodfellowJW, O’ConnorJJ. The Oxford medial unicompartmental arthroplasty: a ten-year survival study. J Bone Joint Surg [Br]1998;80-B:983–989.CrossrefPubMed Google Scholar
2 Berger RA , NedeffDD, BardenRM, et al.Unicompartmental knee arthroplasty. clinical experience at 6- to 10-year followup. Clin Orthop Relat Res1999;367:50–60.PubMed Google Scholar
3 Mercier N , WimseyS, SaragagliaD. Long-term clinical results of the Oxford medial unicompartmental knee arthroplasty. Int Orthop2010;34:1137–1143.CrossrefPubMed Google Scholar
4 Pandit H , HamiltonTW, JenkinsC, et al.The clinical outcome of minimally invasive Phase 3 Oxford unicompartmental knee arthroplasty. Bone Joint J2015;97-B:1493–1500.CrossrefPubMed Google Scholar
5 Liddle AD , PanditH, JudgeA, MurrayDW. Optimal usage of unicompartmental knee arthroplasty. Bone Joint J2015;97-B:1506–1511.CrossrefPubMed Google Scholar
6 Pandit H , JenkinsC, GillHS, et al.Unnecessary contraindications for mobile-bearing unicompartmental knee replacement. . J Bone Joint Surg [Br]2011;93-B:622–628.CrossrefPubMed Google Scholar
7 Kozinn SC , MarxC, ScottRD. Unicompartmental knee arthroplasty. A 4.5-6-year follow-up study with a metal-backed tibial component. J Arthroplasty1989;4(Suppl):S1–S10.CrossrefPubMed Google Scholar
8 Berger RA , MeneghiniRM, SheinkopMB, et al.The progression of patellofemoral arthrosis after medial unicompartmental replacement: Results at 11 to 15 years. Clin Orthop Relat Res2004;428:92–99.CrossrefPubMed Google Scholar
9 Beard DJ , PanditH, GillHS, et al.The influence of the presence and severity of pre-existing patellofemoral degenerative changes on the outcome of the Oxford medial unicompartmental knee replacement. . J Bone Joint Surg [Br]2007;89-B:1597–1601.CrossrefPubMed Google Scholar
10 Beard DJ , PanditH, OstlereS, et al.Pre-operative clinical and radiological assessment of the patellofemoral joint in unicompartmental knee replacement and its influence on outcome. J Bone Joint Surg [Br]2007;89-B:1602–1607.CrossrefPubMed Google Scholar
11 Song EK , ParkJK, ParkCH, et al.No difference in anterior knee pain after medial unicompartmental knee arthroplasty in patients with or without patellofemoral osteoarthritis. Knee Surg Sports Traumatol Arthrosc2016;24:208–213. Google Scholar
12 Munk S , OdgaardA, MadsenF, et al.Preoperative lateral subluxation of the patella is a predictor of poor early outcome of Oxford phase-III medial unicompartmental knee arthroplasty. Acta Orthop2011;82:582–588.CrossrefPubMed Google Scholar
13 Waldstein W , JawetzST, Farshad-AmackerNA, et al.Assessment of the lateral patellar facet in varus arthritis of the knee. Knee2014;21:920–925.CrossrefPubMed Google Scholar
14 Outerbridge HK , OuterbridgeRE, SmithDE. Osteochondral defects in the knee. A treatment using lateral patella autografts. Clin Orthop Relat Res2000;377:145–151.PubMed Google Scholar
15 Judge A , ArdenNK, PriceA, et al.Assessing patients for joint replacement: can pre-operative Oxford hip and knee scores be used to predict patient satisfaction following joint replacement surgery and to guide patient selection?J Bone Joint Surg [Br]2011;93-B:1660–1664.CrossrefPubMed Google Scholar
16 Mahomed N , GandhiR, DaltroyL, KatzJN. The self-administered patient satisfaction scale for primary hip and knee arthroplasty. Arthritis2011;591:253.CrossrefPubMed Google Scholar
17 Hossain FS , PatelS, FernandezMA, KonanS, HaddadFS. A performance based patient outcome score for active patients following total knee arthroplasty. Osteoarthritis Cartilage2013;21:51–59.CrossrefPubMed Google Scholar
18 Pongcharoen B , ReutiwarangkoonC. The comparison of anterior knee pain in severe and non severe arthritis of the lateral facet of the patella following a mobile bearing unicompartmental knee arthroplasty. Springerplus2016;5:202.CrossrefPubMed Google Scholar
Author contributions:
S. Konan: Data analysis, Writing the paper.
F. S. Haddad: Data collection, Data analysis, Editing the paper.
This is an open-access article distributed under the terms of the Creative Commons Attributions licence (CC-BY-NC), which permits unrestricted use, distribution, and reproduction in any medium, but not for commercial gain, provided the original author and source are credited.
This research/study/project was supported by the National Institute for Health Research University College London Hospitals Biomedical Research Centre.
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
This article was primary edited by G. Scott









